Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nonsurgical skin tightening is a popular concept, with novel devices continually entering the market.
The main types of nonsurgical skin-tightening technologies include radiofrequency, infrared light, ultrasound, microneedling with radiofrequency, and subdermal minimally-invasive radiofrequency.
Treatment protocols have evolved over the years to focus on reduced energy settings and multipass techniques, making the procedures safer and more comfortable for patients.
All skin-tightening devices work by the introduction of energy to create heat within the skin or underlying structures. These devices elicit mechanical and biochemical effects that lead to both immediate contraction of collagen fibers, and delayed remodeling and neocollagenesis via wound healing.
Patient selection is key for best results and overall patient satisfaction.
Ideal candidates for nonablative approaches include those patients concerned with risks and recovery of more invasive procedures, and those willing to accept lesser efficacy in exchange for improved side effect and healing time profiles.
Noninvasive and minimally invasive skin-tightening devices are capable of improving both skin laxity and facial contours. The physician must analyze the patient's three-dimensional facial and neck structures, dynamically and at rest, to determine the regions most amenable to therapy, which typically include the upper face/brow and the lower face/jawline.
Skin-tightening procedures can be performed along with fillers, neurotoxins, or other laser- or light-based devices to address multiple issues and achieve a more global improvement: synergy amongst these modalities leads to enhanced patient satisfaction.
Very rarely patients may experience side effects related to overly-aggressive treatment, such as burns, indentations, scars, or changes in pigmentation. The overall incidence of such problems is extremely low with all current devices, owing to updated and improved protocol trends, the use of lower energies, and regular patient feedback as a guide to safe energy delivery.
The appearance of rhytides and skin laxity are near certainties during the aging process. A number of modalities have been used to reduce these phenomena, including laser, mechanical, and surgical techniques. In the mid to late 1990, ablative resurfacing lasers were deemed the gold standard for facial skin tightening. Despite substantial clinical benefits, the technology was beset with significant downtime, and an increased risk of side effects, including erythema, permanent pigmentary changes, infection, and scarring. Patients are now more accustomed to procedures with both reduced downtime and sufficient clinical improvement. This has led to a burgeoning number of nonablative technologies with little to no recovery time and a more favorable risk–reward profile. Unlike ablative lasers, nonablative technologies induce thermal injury to the dermis or subcutaneous tissues, without epidermal vaporization. Epidermal protection is customarily achieved through the use of adjunctive surface cooling.
In terms of skin laxity, specifically, the benchmark remains rhytidectomy or surgical redraping. The goal of this chapter is to review the major types of minimally invasive or nonablative, tissue-tightening techniques, including radiofrequency-, light-, and ultrasound-based devices ( Table 7.1 ). These options are not a replacement for surgical procedures, and appropriate patient selection remains key to overall satisfaction.
| Skin-Tightening Technology | Device |
|---|---|
| Monopolar radiofrequency |
|
| Bipolar radiofrequency with light energy | Elos Plus, Galaxy, Aurora, Polaris, ReFirme (Syneron-Candela) |
| Bipolar radiofrequency with vacuum | Aluma (Lumenis) |
| Bipolar radiofrequency delivered via a microneedle electrode array |
|
| Broadband infrared light |
|
| Unipolar and bipolar radiofrequency |
|
| Bipolar radiofrequency |
|
| Ultrasound technology |
|
| Ultrasound with radiofrequency | Exilis (BTL Aesthetics) |
All skin-tightening devices work by delivering energy to create heat within the skin or underlying structures. This elicits mechanical and biochemical effects that lead to both immediate contraction of collagen fibers and delayed remodeling and neocollagenesis via a wound-healing response ( Box 7.1 ).
Immediate collagen contraction by direct heating of collagen fibers
Delayed remodeling and neocollagenesis via a wound-healing response
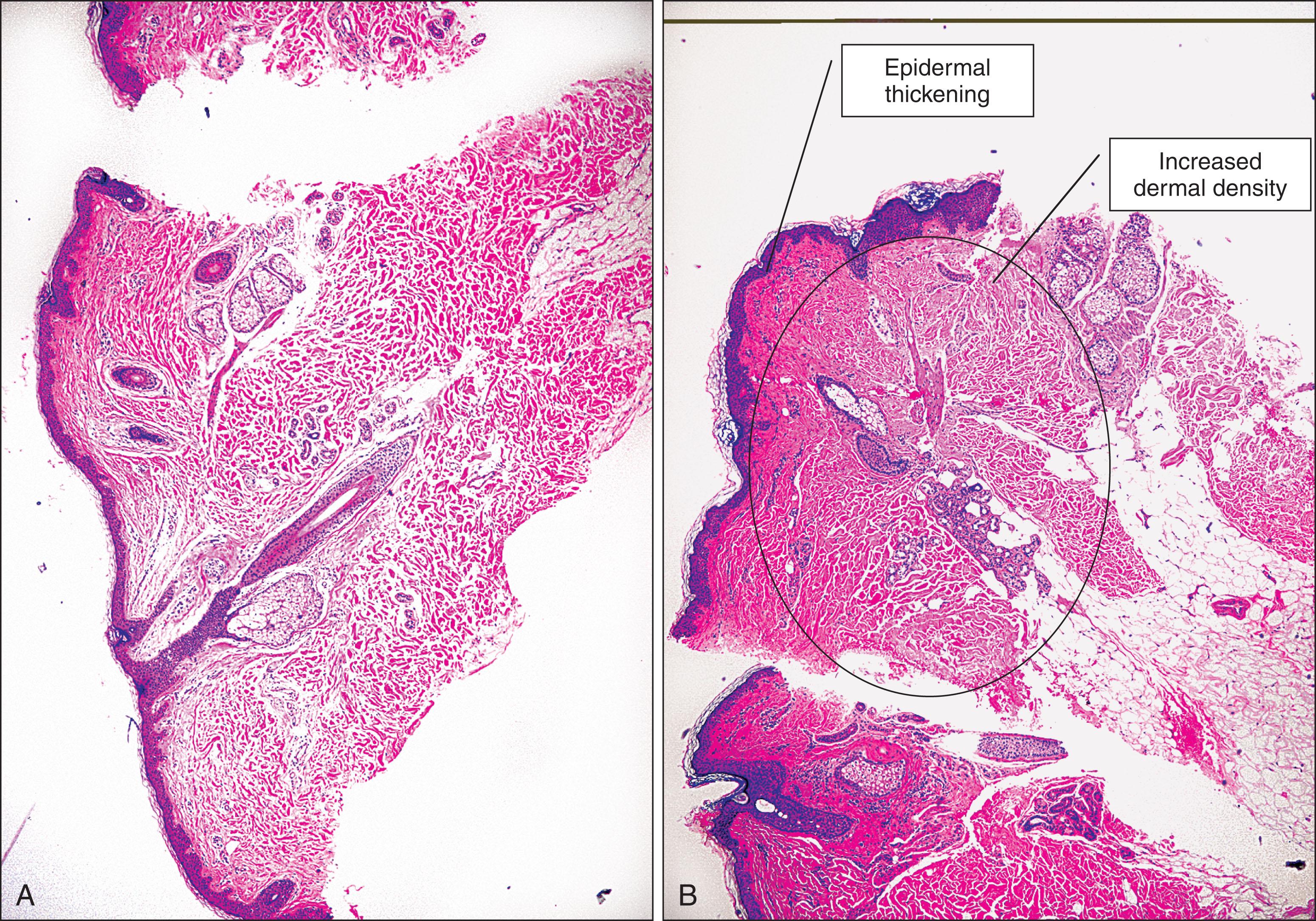
Collagen fibers are composed of a triple helix of protein chains linked with interchain bonds into a crystalline structure. When collagen fibers are heated to specific temperatures, they contract due to breakage of intramolecular hydrogen bonds. This contraction causes the crystalline triple helix structure to fold, creating thicker and shorter collagen fibers. This is thought to be the mechanism of action of immediate tissue tightening seen after skin-tightening procedures. Studies have also found selective contraction of fibrous septae in the subcutaneous fat, which is thought to be responsible for the inward (Z dimension) tightening ( Fig. 7.1 ). It is also believed that fibroblasts, upon heating, stimulate neocollagenesis. Increased production of type I collagen with reorganization in parallel arrays of compact fibrils then leads to delayed dermal remodeling.
Problems arise if too much heat is delivered, as collagen fibrils denature completely above a critical heat threshold, leading to cell death, and scar formation. If too little heat is delivered, there can be an inadequate tissue response, although it appears mild thermal injury, in the sub-coagulative range, does give rise to new dermal ground substance and tissue remodeling of photodamaged skin over time. The optimal shrinkage temperature of collagen has been cited as 58°C–65°C, with initial onset of fibril shrinkage at 58°C, and the main transition to denaturation occurring at approximately 65°C; however, contraction is, in actuality, determined by a combination of temperature and exposure time. For every 5°C decrease in temperature, a tenfold increase in exposure time is required to achieve an equivalent amount of collagen contraction. Studies demonstrate with exposure times in the millisecond domain, the shrinkage temperature is greater than 85°C, whereas for exposure times over several seconds, the shrinkage temperature is at the lower range of 60°C–65°C. In conclusion, both temperature and exposure time must be considered.
The other main mechanism in skin rejuvenation is a secondary wound-healing response that produces dermal remodeling over time, which entails activation of fibroblasts to increase deposition of type I collagen and encourages collagen reorganization into parallel arrays of compact fibrils.
Radiofrequency (RF) devices are indispensable for hemostasis, electrocoagulation, and endovenous closure in medical dermatology. In the esthetic arena, the technology has been used for skin resurfacing and noninvasive tissue tightening.
Radiofrequency is energy in the electromagnetic spectrum, ranging from 300 MHz to 3 kHz. Unlike most lasers, which target specific absorption bands of chromophores, heat is generated from the natural resistance of tissue to the movement of electrons within the radiofrequency field, as governed by Ohm's law ( Box 7.2 ): of fundamental importance, it is a formula which calculates the relationship between voltage, current and resistance in an electrical circuit (V = IR). This resistance, called impedance, generates heat relative to the amount of current and time by converting electrical current to thermal energy. Consequently, energy is dispersed to three-dimensional tissue volumes at targeted and controlled depths.
Impedance ( Z ) to the movement of electrons creates heat relative to the amount of current ( I ) and time ( t ):
Energy (Joules) = I 2 x Z x t
The configuration of electrodes in a noninvasive RF device can be monopolar, unipolar, bipolar, multipolar or fractional. Minimally-invasive platforms include fractional (insulated or noninsulated microneedles) or subcutaneous probes. The main differences are the configuration of electrodes and the type of electromagnetic field that are generated. In a monopolar system, the electrical current passes through a single electrode in the handpiece to a grounding pad ( Box 7.3 ). This type of electrode configuration is common in surgical radiofrequency devices, because there is a high density of power close to the electrode surface, with the potential for deep penetration of tissue heating. In tissue-tightening applications, surface cooling is used to protect the outer layers of the skin and heat only the deeper targets. In a bipolar system, the electrical current passes between two electrodes at a fixed distance ( Box 7.4 ). This type of electrode configuration has a more controlled current distribution; however, the depth of penetration is limited to approximately one-half the distance between the electrodes and will vary with frequency. Unipolar radiofrequency transfers RF energy as electromagnetic radiation rather than as a current, leading to resistive heating requiring no ground. In fractional RF, multiple electrode arrays, or microneedles, are utilized to induce fractional thermal injury. RF microneedling devices can have either insulated or noninsulated needles; insulated needles only heat the area surrounding the sphere at the uninsulated tip whereas noninsulated needles create thermal columns of injury in both the epidermis and dermis relying on the high impedance of the epidermis for epidermal protection. Despite this high impedance, the epidermis is not entirely spared from thermal injury with noninsulated needles. Subdermal, minimally-invasive RF devices utilize a subdermal probe (accessing the dermis through focal skin punctures) to deliver energy in a monopolar or bipolar fashion, heating the dermis to a desired, predictable temperature (55°C–65°C for dermis, 70°C for fat).
The electrical current passes through a single electrode in the handpiece to a grounding pad
There is a high density of power close to the electrode's surface, with the potential for deep penetration of tissue heating
The electrical current passes between two electrodes at a fixed distance
The depth of penetration of the current is limited to approximately one-half the distance between the electrodes
With radiofrequency technologies, the depth of energy penetration depends upon the following factors: (1) the configuration of the electrodes (i.e., either monopolar or bipolar), (2) the mode of delivery (i.e., skin surface, needle-based, or probe-based), (3) the type and composition of tissue serving as the conduction medium (i.e., fat, blood, skin), (4) temperature, and (5) the frequency of the electrical current applied ( Box 7.5 ). Tissue is made up of multiple layers, including dermis, fat, muscle, and fibrous tissue, all of which have a different resistance to the movement of radiofrequency energy ( Table 7.2 ). Structures with higher impedance are more susceptible to heating. In general, fat, bone, and dry skin tend to have low conductivities, such that current tends to flow around these structures rather than through them. Wet skin has a higher electrical conductivity, allowing greater penetration of current. For this reason, in certain radiofrequency procedures, improved results can be seen with generous amounts of coupling fluid and increased hydration of the skin. The structure of an individual's tissue (dermal thickness, fat thickness, fibrous septae, number and size of adnexal structures) plays a role in determining impedance, heat perception, and, ultimately, total deposited energy, despite otherwise comparable parameters.
Frequency of the electrical current
Electrode configuration (i.e., monopolar or bipolar)
Type of tissue serving as the conduction medium
Temperature
| Type of Tissue | Electrical Conductivity (siemens/m) |
|---|---|
| Bone | 0.02 |
| Fat | 0.03 |
| Dry skin | 0.03 |
| Nerve | 0.13 |
| Cartilage | 0.23 |
| Wet skin | 0.22 |
| Muscle | 0.50 |
| Thyroid | 0.60 |
Temperature also influences tissue conductivity and the distribution of electrical current. In general, every 1°C increase in temperature lowers the skin impedance by 2%. Surface cooling will increase resistance to the electrical field near the epidermis, driving the radiofrequency current into the tissue, and increasing the penetration depth. Conversely, target structures that have been prewarmed with optical energy will, in theory, have greater conductivity, less resistance, and greater selective heating by the radiofrequency current. This is the theoretical advantage touted by hybrid, skin-tightening devices, that use a combined approach of light and radiofrequency energy to provide synergistic results.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here