Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic venous insufficiency (CVI) refers to clinical conditions of varying severity, from varicose veins at one end of the spectrum to venous ulceration. Advanced chronic venous disease (CVD) has a more severe clinical presentation than simple varicose veins, reticular veins, or telangiectasia but may be part of the clinical syndrome of CVI that typically presents with swelling, skin changes, and/or leg ulcers. The prevalence of varicose veins has been estimated to be 25% to 33% of the general population. The progression of isolated varicose veins to CVI is rare and noted to be approximately 2% per year. The prevalence of skin changes and ulceration is thought to be approximately 2% to 5% of the general population, whereas the prevalence of venous ulcers alone is approximately 1%. Although the direct costs associated with the treatment of CVI have historically been estimated to be 1 billion dollars/year, the actual number is likely much higher. There are additional indirect costs due to impairment of quality of life (QOL) and consequent societal impact. The management of simple varicose veins are considered in Chapter 53 .
The CEAP (Clinical, Etiologic, Anatomic, and Pathophysiologic) classification groups chronic venous disorders on the basis of clinical presentation, etiology, anatomy, and pathophysiology and is denoted in the basic and full forms. This classification, considered in Box 54.1 , was first described in 1995 and revised in 2004. Although C1 clinical presentation is considered a chronic disorder, patients with C2 to C6 clinical presentation have CVD and the term CVI applies to those patients who have a clinical presentation of C3 to C6. The group of CVI patients with a history of deep vein thrombosis are described as having postthrombotic syndrome (PTS).
C0No visible or palpable signs of venous disease
C1Telangiectases or reticular veins
C2Varicose veins
C3Edema
C4aPigmentation and/or eczema
C4bLipodermatosclerosis and/or atrophie blanche
C5Healed venous ulcer
C6Active venous ulcer
SSymptoms including ache, pain, tightness, skin irritation, heaviness, and muscle cramps, as well as other complaints attributable to venous dysfunction
AAsymptomatic
EcCongenital
EpPrimary
EsSecondary (postthrombotic)
EnNo venous etiology identified
AsSuperficial veins
ApPerforator veins
AdDeep veins
AnNo venous location identified
PrReflux
PoObstruction
Pr,oReflux and obstruction
PnNo venous pathophysiology identifiable
Modified from Eklöf B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg . 2004;40:1248–1252, used with permission.
The veins in the lower extremity can broadly be grouped into three categories: superficial, perforator, and deep. Superficial veins are those that run superficial to the muscle fascia and include the great saphenous, small saphenous, and accessory veins ( Fig. 54.1 ). There exist multiple connections between these veins. Deep veins run deep to the muscle fascia and are axial veins that parallel the course of the arteries. Perforating veins are those that connect the superficial system to the deep veins in the process traversing the fascia (see Fig. 54.1 ). The veins that connect the superficial veins among themselves and which stay above the fascia are termed connecting veins. The great saphenous vein (GSV) starts at the medial end of the dorsal venous arch, runs anterior to the medial malleolus, rising up the medial leg and thigh, and empties into the common femoral vein (CFV) after piercing the fascia approximately 4 cm lateral and inferior to the pubic tubercle. The small saphenous vein (SSV) starts at the lateral end of the dorsal venous arch, courses behind the lateral malleolus, and ascends along the lateral leg before emptying into the popliteal vein approximately 60% of the time. The outflow is into the femoral, profunda femoral, or internal iliac veins, and the GSV the reminder of the time. The two saphenous veins can be connected by a communicating vein, the intersaphenous vein (Giacomini vein). The deep veins originate in the foot as the continuation of the dorsalis pedis vein (anterior tibial) and from the plantar aspect as the continuation of the deep venous plantar arch in the form of the lateral and medial plantar veins and then the posterior tibial veins. Continuation in the leg and the thigh is through accompaniment of corresponding arteries. There is often duplication of the deep veins, especially in the calf where the posterior tibial, anterior tibial, and peroneal veins accompany the corresponding artery as venae comitantes. The incidence of duplication of the femoral vein, popliteal vein, common femoral, or the iliac veins is much lower. The profunda femoris vein communicates directly with the popliteal vein in 38% of limbs and communicates via a tributary in a further 48% of limbs. The direct perforator veins can be divided into those of the foot, ankle, calf, and thigh. The foot perforators are grouped into medial, lateral, dorsal, and plantar, but unlike the perforating veins elsewhere the flow is from the deep veins into the superficial veins. The calf has three main group of perforating veins, including medial (paratibial and posterior tibial), lateral, and anterior perforating veins. Although the upper, middle, and lower posterior tibial perforators connect the posterior accessory GSV to the posterior tibial veins, the paratibial perforators connect the GSV to the posterior tibial veins. Four to five paraperoneal perforators typically exist along the lateral calf. In the thigh, the femoral canal perforators connect the GSV with the femoral or cranial popliteal vein approximately 10 to 15 cm proximal to the knee.

The veins in the lower extremities serve the dual purpose of being a conduit to conduct blood back to the heart and also as a reservoir. They are aided in these functions by two aspects unique to the venous system—the presence of unidirectional bicuspid valves in the veins and the calf pump. There is variation in the number and location of valves in the superficial, perforator, and deep venous systems. The GSV typically has at least six valves, with varicosity decreasing this number. The most constant valve is usually the one within 2 to 3 cm of the saphenofemoral junction, present in more than 94% of the population. The mean number valves in the SSV is quite variable, 1.8 to 13. The perforator veins have valves that normally allow blood flow from superficial to the deep systems. The deep system has a valve pattern that decreases in number with cranial progression. The inferior vena cava (IVC) does not have any valves, and the common iliac vein (CIV) valve is seen in only 1.2%. Valves are present in the external iliac vein (EIV; right more often than left) in 27% of veins and in the internal iliac in 10%. The CFV above the SFJ usually has a valve, and there are approximately five valves between the SFJ and the knee joint. The deep veins of the calf typically have valves every 2 cm. The mean distance between valves in the GSV has been estimated to be 3.8 ± 0.4 cm and in the femoral vein was 4.6 ± 0.3 cm. This study found that the valve cusps were at a minimum angle of 60% to one another and that the angle between the valves correlated with the distance between the valves. However, no relation was noted between the diameter of the normal vein and the angle between the valves. Four stages of valve function have been defined—opening, equilibrium, closing, and closed. Although it was originally believed that valve closure was related to the reversal of flow, contemporary thinking is that it is due to the vortex generated by the part of the flow that goes into the valve sinus. This vortex, while keeping the valve leaflets away from the vein wall, forces the closure of the valve by virtue of pressure exerted once the flow through the valve itself slows.
The calf pump or peripheral heart is akin to a peripheral pump whose role is to store and subsequently “pump” blood back into the central circulation through muscle contraction that occurs with lower extremity activity. This pump is composed of venous sinusoids that constitute the reservoir of the pump embedded in skeletal muscle which provided the contractile effect. These sinusoids lie within the gastrocnemius and soleus muscles, with those in the latter being more developed. The inflow for the sinusoids is the superficial veins, reticular veins, and from the muscle itself via muscular veins and postcapillary venules. The outflow for the soleal sinusoids is constituted by the posterior tibial and peroneal veins via indirect perforators, while that for the gastrocnemius sinusoids is the popliteal vein via the gastrocnemius veins. Although thigh and foot pumps also exist, they play a secondary role to the calf pump. Valves exist in the network of veins that constitute the inflow and outflow but are absent in the sinusoids themselves. The presence of proximal deep venous obstruction or reflux from incompetent valves can lead to calf pump dysfunction and manifestation of CVI.
The CEAP classification defines etiology in chronic venous disorders as being congenital, primary, or secondary. Congenital etiology primarily involves venous and arteriovenous (AV) malformations and, to a very limited extent, iliac vein compression because some cases of such compression occur at embryological fusion sites. Congenital absence or anomalies of veins or venous valves and persistent embryonic veins also belong to this group. Primary etiology refers to degenerative changes in the vein wall and valves leading to reflux and varicosity. Most patients with nonthrombotic iliac vein lesions have primary etiology. Secondary refers to an acquired origin could be due to a variety of causes, including postthrombotic changes, extrinsic compression of the deep veins from fibrosis or tumor, and iatrogenic from placement of IVC filters. Of these the postthrombotic changes are the predominant secondary etiology. Although Bauer noted that most of the advanced cases of CVI were due to primary etiology, more recent data from increasing use of duplex ultrasound (DUS) and intravascular ultrasound (IVUS) support PTS as the most common etiology for CVI.
The primary driver for CVI is reflux involving the superficial and/or deep veins, obstruction involving the deep veins, or a combination of the same. The common pathway that leads to clinical manifestations is venous hypertension.
Venous reflux can arise as discussed previously by failure of valves either from primary or secondary etiology. In the superficial veins, such reflux can arise by primary degeneration of the vein valve leaflets, dilation of the vein wall, or secondary etiology, including superficial thrombophlebitis, trauma, or hormonal effects. Primary etiology has been found to be responsible for 11% to 75% of deep venous reflux (DVR). Primary DVR arises due to stretching/elongation of the valve cusps or dilation of the affected venous segment. A developmental etiology has also been recognized due to symptoms predating the age of actual presentation, often as early as teenage years. Trauma has also been presented as a cause. Degeneration of the fibroelastic tissue of the valve that gradually develops over time is deemed the most plausible cause in a majority of patients. Secondary DVR usually results from DVT. With regard to progression of DVR, it has been postulated that an initial incompetent valve high in the femoral vein creates an excess stress on the valve below and leads to it becoming incompetent. For clinical manifestations, the reflux must involve multiple venous segments in the thigh and calf (axial reflux) as opposed to segmental reflux. A functioning, competent popliteal valve has been considered a barrier to development of severe symptoms, even in the presence of reflux involving the entire femoral vein because it protects the calf pump from the deleterious effect of reflux. This is particularly true for patients with venous ulcer (C6 disease) in whom Danielsson et al. noted axial distribution of reflux in a majority of patients (79%). In their series, no patient had isolated DVR below the knee with primary etiology as the predominant cause. However, the role of the competent popliteal valve is still debated. More recent work by Neglen et al. has shown the popliteal valve not to be an important determinant of venous hemodynamics or clinical severity by itself. The authors note that reflux in additional segments must also be considered. Secondary DVR resulting from DVT often involves not only the thrombosed segment but also the adjacent segment(s). As Caps et al. have pointed out, permanent valvular damage can occur even in the absence of thrombosis of the deep venous segment. Although the precise mechanism has not been identified, release of inflammatory mediators and localized vein dilation have been proposed as potential contributing factors. The most frequent pathophysiology in secondary DVR is direct damage to the vein valve cusps by the thrombus. Dysfunction of the valves of the deep veins has been shown to increase the rate of progression of venous disease with a higher rate of ulcer formation. Failure of the valves can also occur in the perforator system with resultant blood flow from deep to the superficial system. The resultant impact on the latter is dilation and secondary failure of the vein valves. Reflux may also occur in the venous tributaries without concomitant reflux in the superficial/deep or perforator system, leading to localized symptoms. Clinical severity increases with an increase in DVR (higher CEAP clinical class correlates with worsening axial reflux). This has been supported by other studies. The prevalence of both superficial and deep reflux is very common in patients with venous ulceration. In 264 patients with venous ulceration the anatomic distribution of reflux was noted as follows: deep reflux (71%), superficial reflux (57%), and perforator reflux (17%). This relative distribution varies according to the practice setting. In one series, up to 80% had superficial reflux alone or in combination with perforator and/or deep insufficiency. Occurrence of reflux in more than one venous compartment is extremely common, occurring in up to two-thirds of patients with healed or active ulceration. Isolated perforator insufficiency is extremely rare as a basis of venous leg ulcers because most are associated with reflux in other territories.
Obstruction of the deep veins leads to limitation of limb blood outflow leading to development of elevated venous pressure in addition to calf pump dysfunction. The etiology of such obstruction can be primary due to extrinsic compression (e.g., nonocclusive iliac vein lesions, such as May-Thurner syndrome [MTS]) or secondary due to extrinsic compression (retroperitoneal fibrosis, pelvic masses or tumors) or intrinsic, such as PTS. With increasing use of IVUS the increasing incidence of PTS in causing venous obstruction has come to the fore. Also important is the presence of combined venous obstruction and reflux. Coexistence of deep venous obstruction with DVR reinforces the pathology with earlier occurrence of symptoms than would be the case if obstruction did not exist. Most postthrombotic reflux is associated with obstruction. Furthermore, the prevalence of having combined reflux and obstruction significantly increases in patients with skin changes constituting CEAP clinical class 4, 5, and 6 disease when compared with those without skin damage. In one study of patients with venous leg ulcers, only 1% was found to be due to obstruction alone without reflux.
Although calf pump dysfunction can occur due to primary causes such as muscular or neuromuscular disorders, it is more commonly due to severe reflux or obstruction. The overwhelming of the calf pump renders it less efficient in the process, leading to venous hypertension and sequelae thereof. Calf pump dysfunction appears to be a noteworthy mechanism responsible for development of more advanced stages of clinical disease, including venous ulcers.
The final pathway for reflux, obstruction, and/or calf pump dysfunction to exert its impact is through venous hypertension. The hemodynamic changes resulting from changes in the macrovenous milieu reflect on to the microcirculation, leading to a constellation of findings collectively termed venous microangiopathy. Activation of inflammatory pathways and dysfunction of microvenous valves can also contribute to the development of such microangiopathy (elongation, dilation and tortuosity of capillary beds, endothelial damage, and thickening of basement membrane). Although the precise mechanism is not known for the development of venous microangiopathy, white blood cell and growth factor trapping, in addition to fibrin cuff formation, have been hypothesized as potential mechanisms.
The history should focus on establishing the etiology—congenital versus primary versus secondary or a combination thereof—by focusing on personal or family history of venous thromboembolic episodes (VTEs) or thrombophilia, medication history (hormone replacement therapy, oral contraceptive pills, or use of testosterone), obstetric history, and smoking. Risk factors for CVI include age, positive family history, and obesity. Examination should always be performed with the patient in the standing position in a warm room with good light and should establish the size, location, and distribution of varicose veins and also focus on other signs of venous disease such as edema (partially pitting or nonpitting), skin changes (induration, pigmentation, lipodermatosclerosis, atrophie blanche, eczema, dermatitis, skin discoloration, increased skin temperature), and ulceration (healed or active). Inspection and palpation are essential parts of the examination, and auscultation (bruit) is particularly helpful in those with vascular malformation and AV fistula. Varicose dilations or venous aneurysms, palpable cord in the vein, tenderness, thrill, bruit, or pulsatility should be recorded. Ankle mobility should also be examined because patients with advanced venous disease frequently have decreased mobility in the ankle joints. Sensory and motor functions of the limb and foot are assessed to help differentiate from diabetic neuropathy or any underlying neurologic problem. An abdominal mass or lymphadenopathy can provide a clue to venous compression and outflow obstruction. Corona phlebectatica (ankle flare or malleolar flare) is a fan-shaped pattern of small intradermal veins located around the ankle or the dorsum of the foot. This is considered to be an early sign of advanced venous disease. Inspection of the abdominal wall and perineal and inguinal region should be routinely performed. Perineal, vulvar, or groin varicosities can be seen in iliac vein obstruction or internal iliac vein or gonadal vein incompetence causing pelvic congestion syndrome (PCS). Scrotal varicosity may be a sign of gonadal vein incompetence, left renal vein compression between the superior mesenteric artery and the aorta (Nutcracker syndrome), or occasionally even IVC lesions or renal carcinoma. Skin lesions, other than those listed previously, such as capillary malformations, tumors, onychomycosis, or excoriations, should be noted. An aneurysmal saphenous vein can be misdiagnosed as a femoral hernia or vice versa. The presence of a longer limb, lateral varicosity noted soon after birth, and associated capillary malformations are tip-offs for congenital venous-lymphatic malformation (Klippel-Trénaunay syndrome). A complete pulse examination is performed to exclude underlying peripheral artery disease. The physical examination can be complemented by a handheld Doppler ultrasound examination, although the latter does not replace evaluation of the venous circulation with color duplex scanning. The aim of the clinical evaluation is not only to determine the presenting signs and symptoms and the type of venous disease (primary, secondary, congenital) but also to exclude other etiologies (peripheral artery disease, rheumatoid disease, infection, tumor, or allergies). The physician should also establish the degree of disability caused by the venous disease and its impact on the patient’s QOL. The American Venous Forum recommends using the revised Venous Clinical Severity Score (VCSS) to grade and document the presenting symptoms of patients with CVD ( Table 54.1 ).
| Pain | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
|---|---|---|---|---|
| Or other discomfort (i.e., aching, heaviness, fatigue, soreness, burning); presumes venous origin | Occasional pain or other discomfort (i.e., not restricting regular daily activity) | Daily pain or other discomfort (i.e., interfering with but not preventing regular daily activities) | Daily pain or discomfort (i.e., limits most regular daily activities) | |
| Varicose Veins | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
| “Varicose” veins must be ≥ 3 mm in diameter in the standing position to qualify | Few: scattered (i.e., isolated branch varicosities or clusters); also includes corona phlebectatica (ankle flare) | Confined to calf or thigh | Involves calf and thigh | |
| Venous Edema | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
| Presumes venous origin | Limited to foot and ankle area | Extends above ankle but below knee | Extends to knee and above | |
| Skin Pigmentation | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
| Presumes venous origin; does not include focal pigmentation over varicose veins or pigmentation due to other chronic diseases (i.e., vasculitis purpura) | None or focal | Limited to perimalleolar area | Diffuse over lower third of calf | Wider distribution above lower third of calf |
| Inflammation | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
| More than just recent pigmentation (i.e., erythema, cellulitis, venous eczema, dermatitis) | Limited to perimalleolar area | Diffuse over lower third of calf | Wider distribution above lower third of calf | |
| Induration | None: 0 | Mild: 1 | Moderate: 2 | Severe: 3 |
| Presumes venous origin of secondary skin and subcutaneous changes (i.e., chronic edema with fibrosis, hypodermitis); includes white atrophy and lipodermatosclerosis | Limited to perimalleolar area | Diffuse over lower third of calf | Wider distribution above lower third of calf | |
| No. of Active Ulcers | 0 | 1 | 2 | ≥ 3 |
| Active ulcer duration (longest active) | N/A | < 3 months | > 3 months but < 1 year | Not healed for > 1 year |
| Active ulcer size (largest active) | N/A | Diameter < 2 cm | Diameter 2–6 cm | Diameter > 6 cm |
| Use of Compression Therapy | None: 0 | Occasional: 1 | Frequent: 2 | Always: 3 |
| Not used | Intermittent use of stockings | Wears stockings most days | Full compliance: stockings |
Patients with CVI can present with a variety of symptoms and signs. Such manifestations can overlap for PTS and nonthrombotic iliac vein lesions including MTS. In fact, MTS can be identified in 18% to 49% of patients presenting with left lower limb DVT. MTS can affect any age group. It is more commonly seen in women and usually involves the left side. Another aspect previously noted is the worsened clinical manifestation in patients with combined deep venous obstruction and reflux. Patients may present with one or more of the following—limb swelling; pain; venous claudication (pelvic, thigh, or hip pain that develops after exercise); venous varicosities; hyperpigmentation; skin and subcutaneous inflammatory changes (eczema, lipodermatosclerosis, induration, and venous ulcerations). One review noted swelling followed by venous claudication as the most common symptoms at presentation in patients undergoing intervention for nonmalignant obstruction of the iliocaval system. This study also observed the incidence of active ulcers as approximately 19%.
DVR and obstruction can both cause limb swelling, although swelling from reflux is usually less severe and more intermittent than that caused by obstruction. Such limb swelling in the presence of skin damage can lead to recurrent bouts of cellulitis, which is not uncommon in patients presenting with massive limb edema. Patients presenting with limb swelling that is more diffuse than just overlying varicose veins should undergo careful interrogation for deep venous obstruction/reflux.
Patients with CVI can experience pain that is focal in nature involving the thigh, calf, or shin, or be more diffuse involving the entire extremity. Such pain can be of varying quality—achiness, heaviness, shooting, or bursting. Relief from such pain is usually by measures which reduce limb venous pressure, including elevation and ambulation. It is also possible for CVI patients with deep venous obstruction to experience venous claudication, pain that arises with exercise. Arterial pathology can be ruled out in such patients with pulse exam and exercise ankle-brachial index. Hyperesthesia can also be the presenting symptom at times. Atypical pain that occurs when a patient is recumbent and relieved with ambulation is also seen. Another condition is venous hypertension syndrome where patients complain of severe pain in an otherwise normal- appearing limb and is seen in approximately 10% of patients. Iliac vein obstruction usually presents with pain out of proportion to signs.
Hyperpigmentation and lipodermatosclerosis include skin manifestations in patients presenting with CVI. They represent the final end points of venous hypertension that leads to skin damage. Obstructive venous pathology or combined obstruction/reflux is generally more responsible for this as opposed to isolated DVR. Reflux leading to such skin changes can occur with substantial reflux that requires either axial DVR or a refluxing large-caliber saphenous vein (usually > 10 mm). The prevalence of having combined reflux and obstruction significantly increases in patients with skin changes constituting CEAP clinical class 4, 5, and 6 disease when compared with those with a lack of substantial skin damage. In patients with venous leg ulcers, only 1% was found to be due to obstruction alone without reflux.
Patients with CVI can also have restless legs at night waking them from sleep or causing them to remain awake at night. These can also be a manifestation of CVI, especially obstructive deep venous lesions. Relief of the obstruction leads to respite from the symptom or even complete resolution.
Limb swelling due to CVI can mimic that from lymphedema, and such patients can present with humping of dorsum of foot, squaring of toes, and inability to pinch the skin off the second toe (Stemmer sign). Secondary lymphedema from overloading of the lymphatic system from venous obstruction/reflux is more common than previously thought and responds to correction of relevant venous pathology including obstruction. It is essential to evaluate patients presenting with lymphedema for possible venous obstruction/reflux.
PCS denotes a collection of symptoms and signs in women arising from incompetence of the pelvic veins and accounts for up to 20% of outpatient gynecological consultations. Patients with PCS can present with pain (pelvic, lower abdominal, lower back, hip, and/or dyspareunia), urinary frequency, dysmenorrhea, and/or varicose veins of the vulva, perineum, buttocks, and lower extremity, in addition to ovarian point tenderness.
A variety of studies are used to screen and confirm diagnosis in patients with CVI.
Venous DUS is the most commonly used tool given its noninvasive nature and cost effectiveness. DUS can be used to evaluate the superficial, deep, and perforator systems, and ascertain pathology: reflux versus obstruction versus combination. A 5-MHz linear array pulsed wave Doppler transducer is used most frequently for the deeper veins, with the higher-frequency probe (up to 18 MHz) for detailed assessment of the superficial veins. Evaluation of reflux should be performed with the patient in the upright position, with the leg rotated outward, heel on the ground, and weight taken on the opposite limb. The veins below the knee can also be assessed in the sitting position. Using the supine position for reflux gives both false-positive and false-negative results. All deep veins of the leg are evaluated followed by the superficial veins, including the GSV, SSV, accessory saphenous veins, and perforating veins, for a complete examination. The four components that are essential in a complete duplex scanning examination for CVI are visibility, compressibility, venous flow, and augmentation. Asymmetry in flow velocity, lack of respiratory variations in venous flow, and waveform patterns at rest and during flow augmentation in the CFVs indicate proximal obstruction. Reflux in the superficial system is elicited by increased intraabdominal pressure using a Valsalva maneuver followed by manual compression of the calf/foot. Reflux in the deep veins of the lower extremity is typically evaluated in the standing position using the cuff deflation technique put forth by van Bemmelen et al. Based on studies by Masuda et al. and Araki et al. the standing cuff deflation technique appears to be a superior method when compared with other techniques, including the Valsalva maneuver. Four stages of the venous valve cycle—opening, equilibrium, closing, and closed phases—have been described. The ability of the valve to maintain the closed phase determines occurrence of reflux. Although metrics such as valve closure time/reflux time (VCT/RT) have been postulated and used to grade reflux, these represent more qualitative than quantitative indices. The latter include peak reflux velocity (PRV) and time-averaged flow (TAF), which have demonstrated good correlation with both hemodynamic parameters and clinical severity in multiple studies. The most common criteria used for defining reflux is derived from data published by multiple groups, including Labropoulus et al., and have since been incorporated into the clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. Per the guidelines, DVR is defined as reflux lasting for 500 ms or more in the deep veins below the knee and the deep femoral vein (DFV) and lasting for 1000 ms or more in the femoral and popliteal veins. For the superficial truncal veins in the lower extremity, reflux is pathologic if it lasts longer than 500 ms. The perforator veins are noted to have pathologic reflux if they have a diameter > 3.5 mm and outward flow of > 500 ms, located beneath a healed or open venous ulcer. Duplex scanning also ascertains location and extent of the obstructive pathology, besides providing inflow and outflow data. Normal luminal diameter cutoffs used for the CFV, EIV, and CIV are 12, 14, and 16 mm, respectively ( Table 54.2 ). The corresponding areas used for the three segments are 125, 150, and 200 mm 2 , respectively. Luminal diameter/areas less than these cutoffs in the symptomatic patient require further investigation in the form of IVUS.
| Vein | Luminal Area (mm 2 ) | Diameter (mm) |
|---|---|---|
| CFV | 125 | 12 |
| EIV | 150 | 14 |
| CIV | 200 | 16 |
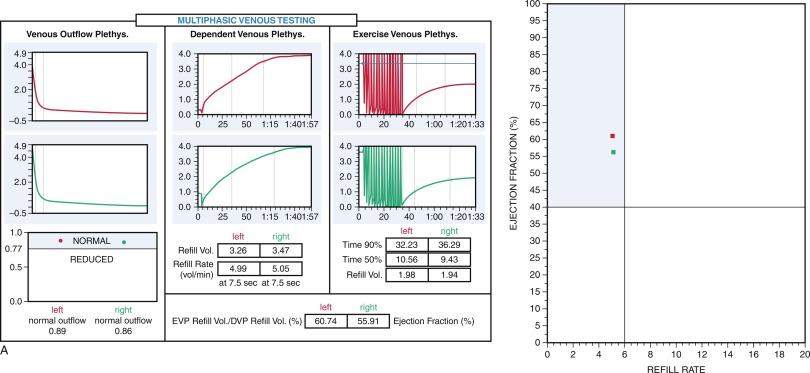
Air plethysmography (APG) is a noninvasive technique of evaluating lower extremity reflux, obstruction, and calf pump function using calf volumetric changes ( Fig. 54.2 ). Other forms of plethysmography have fallen out of favor due to a variety of shortcomings. APG is performed using the technique described by Christopoulos et al. where a tubular bag is placed around the leg of the patient in the supine position. The leg is subsequently elevated to 45 degrees, emptying the veins and allowing the calibration of the device. The patient then stands up quickly, holding onto a frame with the body weight on the contralateral limb. The increase in the calf volume that results is known as the functional venous volume (VV), and the time taken to achieve 90% of this volume is known as the venous filling time (VFT). The venous filling index (VFI), which is a comprehensive measure of reflux, is computed by dividing 90% of VV by VFT. The subject is then asked to take one tiptoe and with weight on both legs and return to the baseline position. Contraction of the calf muscles during this action ejects venous blood with resultant reduction in calf volume. The volume forced out is the ejection volume (EV), and (EV/VV) × 100 is the ejection fraction. The subject is then asked to perform 10 tiptoes and return to baseline. The calf volume at the end of the 10 tiptoes is the residual volume (RV). The residual volume fraction (RVF) is represented by (RV/VV) × 100. EV, EF, RV, and RVF all represent calf pump metrics. A recent study has suggested a body weight transfer maneuver (subject rocks forward shifting most of his or her weight onto the leading foot and then back again onto the rear foot) as being better than the tiptoe maneuver in evaluating calf pump function given a 40% relative increase in EF. Venous obstruction is evaluated by the venous occlusion method, in which patients are placed in a supine position with the leg elevated to empty the veins. A 14-cm thigh tourniquet is placed close to the groin and inflated to 80 mm Hg with resultant increase in the VV (beyond the original value previously noted). Following attainment of a steady state (arterial inflow equals venous outflow), the thigh tourniquet is deflated rapidly leading to a rapid decrease in calf volume. The amount of venous blood that leaves the leg in the first second is calculated (V1). Outflow fraction (OF) is computed as (V1/VV) × 100. Repetition of the process with digital occlusion of the long saphenous and small saphenous veins at the level of the knee gives the OF with superficial occlusion. Venous outflow resistance (VOR) is another metric that can be used to determine outflow obstruction and is computed by simultaneous recording of the volume and pressure outflow curves. The resistance is estimated by dividing the pressure on the curve by the flow. OF and VOR are plethysmographically calculated measures of outflow obstruction. Kurstjens et al. compared OF, ejection fraction, and RVF as a quantitative metric of outflow obstruction with DUS and magnetic resonance venography (MRV). They found poor correlation between OF, EF, and RVF and presence of deep venous obstruction. The same group in a separate study using receiver operator curves demonstrated that venous occlusion APG could not be used to identify obstruction proximal to the femoral venous confluence or those who would benefit from femoroiliocaval stenting. Lattimer et al. have put forth venous drainage index (VDI) as a metric for quantitative assessment of venous obstruction based on the inverse relation between the rate of reduction of calf volume on leg elevation with the degree of proximal venous obstruction. Further study is required to elucidate the usefulness of this metric.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here