Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Q45.1 What is the procedure for performing the Stoughton vasoconstriction assay, and how does this assay assess the potency of topical corticosteroid (TCS) molecules? (Pg. 512)
Q45.2 How does the vehicle affect the potency of TCS? What are the pros and cons of including propylene glycol in the vehicle? (Pgs. 514, 522)
Q45.3 At the molecular level, how does TCS induce production of various proteins that mediate the clinical effects of TCS? (Pg. 514)
Q45.4 What are the most important anti-inflammatory effects of TCS in the skin? (Pg. 514)
Q45.5 What are the most important antiproliferative and atrophogenic effects of TCS? (Pg. 515)
Q45.6 Concerning local adverse effects of TCS, (1) which is most common, (2) what are the clinical features, and (3) which clinical feature is irreversible? (Pg. 520, Box 45.7 )
Q45.7 What are several of the most important factors leading to the development of the addiction/rebound syndrome (including patients with perioral dermatitis)? (Pg. 520)
Q45.8 What are some of the ocular complications from TCS applied in a periorbital distribution (intentionally or inadvertently)? (Pg. 520)
Q45.9 Concerning allergic contact dermatitis to the actual TCS molecule, (1) what are the four groups of TCS (including two subgroups), (2) what are one to two representative TCS molecules in each of these groups? (Pg. 521x2, Box 45.8 )
Q45.10 What is meant by tachyphylaxis when treating with TCS, and which TCS potency groups are at particular risk for this complication of therapy? (Pg. 521)
Q45.11 What is a rare, yet noteworthy, complication of using potent TCS for diaper dermatitis? (Pg. 521)
Q45.12 What are the two most common allergens found in TCS vehicles? (Pg. 522)
Allergic contact dermatitis
Atopic dermatitis
Adverse effects (events)
Betamethasone diproprionate in optimized vehicle
Bullous pemphigoid
Cutaneous T-cell lymphoma
Fingertip unit
Glycosaminoglycan
Glucocorticoid receptor
Hypothalamic–pituitary–adrenal
Interferon
Immunoglobulin E
Interleukin
Liquor carbonis detergens
Lichen planus
Lichen sclerosus atrophicus
Platelet-activating factor
Pyoderma gangrenosum
Psoralen and ultraviolet A
Pemphigus vulgaris
Salicylic acid
Topical corticosteroid
Ultraviolet A
Ultraviolet B
The authors would like to thank Michael R. Warner for his contribution to previous editions of this chapter.
The human body regulates inflammatory immune reactions via endogenous glucocorticoids such as cortisol (hydrocortisone). In the early 1950s, physicians began using systemically administered cortisol to treat inflammatory dermatoses. Unfortunately, corticosteroids (CS) with a ketone group at the C11 position (cortisone) must be reduced to their corresponding 11-hydroxyl analogs (hydrocortisone = cortisol) to be active, a reduction that does not occur effectively in the skin. Thus, early attempts to use topical cortisone failed until 1952, when Sulzberger and Witten successfully treated eczematous dermatitis with topical hydrocortisone. Their success marked a cornerstone in the history of dermatology and the birth of a major new market for pharmaceutical companies. The next six decades of research, experience, and marketing led to the development of an ever-growing list of TCS preparations and an array of interrelated facts attempting to explain their clinical effects. The pertinent points of TCS pharmacology and the appropriate clinical use of TCS in dermatology are summarized in this chapter.
To understand the pharmacology and pharmacokinetics of TCS, clinicians must first understand how their clinical effect is measured and compared.
The term ‘potency’ is used to describe the intensity of a TCS clinical effect. To estimate clinical effect, assays measure aspects of the anti-inflammatory and/or the antiproliferative properties of TCS (see Mechanism of Action section) using laboratory animals or human volunteers ( Box 45.1 ). Q45.1 The Stoughton Vasoconstriction Assay is the most commonly used test of TCS ‘potency’. In fact, the term potency is often misused to describe the vasoconstriction rating of a TCS, which does not always correlate with clinical efficacy.
Studies Using Laboratory Animals
Mitotic index suppression—hairless mouse
Antigranuloma assay—rat
Croton oil inflammation assay—rat
6-chloro-2-4-dinitrobenzene inflammation—guinea pig
Studies Using Human Volunteers
Vasoconstrictor assay
Artificially induced inflammation
Tape stripping
Ultraviolet light
Mustard oil
Nitric acid
Tetrahydrofurfuryl alcohol
Nickel-induced positive patch tests
Dimethylsulfoxide
Sodium hydroxide
Spontaneously occurring skin disease (psoriasis)
Inhibition of fibroblast growth in vitro
Neutral red release assay
Mouse tail epidermis
Transgenic mouse model expressing human elastin promoter/chloramphenicol acetyltransferase
Guinea pig epidermis
Micrometer calipers
Histopathologic examination of skin biopsies
X-ray radiography
Pulsed ultrasound
Optical coherence tomography
The actual vasoconstriction assay usually involves the following:
Preparing the test CS in 95% alcohol.
Applying it to the volar surface of a normal volunteer’s forearm.
Allowing the alcohol to evaporate, then covering the test area with an occlusive dressing for 16 hours.
Washing off the area.
Assessment of vasoconstriction 2 hours later on a blind basis by an experienced investigator using a multiple unit scale (0–3 or 0–4).
Statistical analysis.
The vasoconstriction assay is the assay of choice because it usually correlates well with clinical efficacy and is reproducible. In patients with psoriasis, for example, the vasoconstriction assay demonstrated excellent correlation in bilateral, symmetrically paired comparisons of psoriatic target lesions treated 1 to 3 times daily, for 2 to 3 weeks with 30 of 32 different TCS compounds. The two exceptions were aclometasone ointment and hydrocortisone valerate cream, which both demonstrated greater vasoconstrictive activities than clinical efficacy. The vasoconstriction assay proved to be reproducible by the same and other observers in completely different settings, locations, climates, and subjects. The disadvantages are that the test is subjective, only measures one aspect of TCS effects, and produces no ‘hard copy’ (such as with an electrocardiogram or chest x-ray) for subsequent comparison, analysis, and validation. TCS preparations are best evaluated with the vasoconstriction assay and a second assay on spontaneously occurring skin diseases in human volunteers (psoriasis).
The pharmacokinetics and resultant clinical potency of a TCS preparation depend on four interrelated factors: (1) the structure of the CS molecule, (2) the vehicle, (3) the concentration of the CS molecule in the vehicle, and (4) the characteristics of the skin onto which the TCS is applied. The exact relationship between these factors is neither clear nor predictable; however, certain aspects have been elucidated.
Hydrocortisone is considered the backbone of most TCS molecules ( Fig. 45.1 and Table 45.1 ). These molecules are formed by placing hydroxyl groups into the 11-β, 17-α, and 21 positions; ketone groups into the 3 and 20 positions; and a double bond into the 4 position of the glucocorticoid nucleus. The further addition or alteration of functional groups (hydroxy, hydrocarbon, ester, fluoro, chloro, acetonide, ketone) at certain positions can greatly affect the molecule’s pharmacokinetics (see Table 45.1 ).
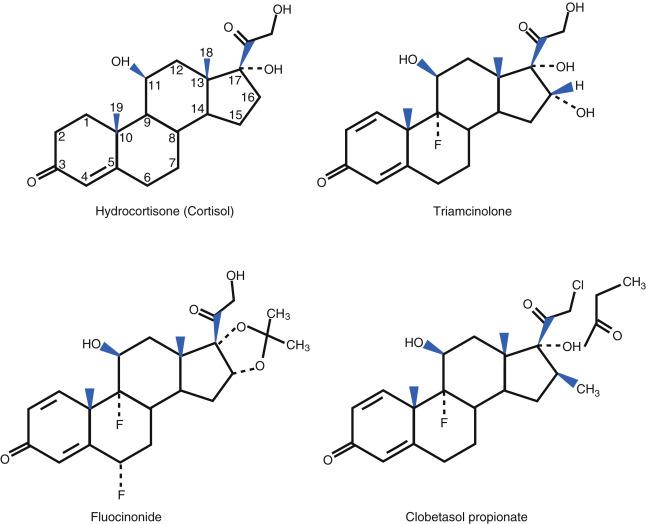
| Name | Structure | Relevant Functional Groups | Vasoconstrictor Potency Rating a |
|---|---|---|---|
| Hydrocortisone | [Hydrocortisone structure] | C11: β-hydroxyl C17: hydroxyl C20: ketone C21: hydroxyl |
Class VII Low potency (1.0%, 2.5%) Generic ointment |
| Triamcinolone acetonide | [Triamcinolone acetonide structure] | C1,2: double bond C9: fluorine C11: hydroxyl C16: hydroxyl |
Class V Moderate (0.1%) Generic ointment |
| Fluocinolone acetonide acetate (fluocinonide) | [Fluocinonide structure] | C1,2: double bond C6: fluorine C9: fluorine C16,17: acetonide C21: ester (acetate) |
Class II High potency (0.05%) Generic ointment |
| Clobetasol propionate | [Clobetasol propionate structure] | C1, 2: double bond C9: fluorine C16: methyl C17: ester C21: chlorine |
Class I Superpotent (0.05%) Generic ointment |
a Vasoconstrictor potency of selected ointment for the topical corticosteroids listed.
The removal, replacement, or masking of hydroxyl groups changes a given molecule’s lipophilicity, solubility, percutaneous absorption, and glucocorticoid receptor (GCR)-binding activity. Replacement of the 21-hydroxy group in betamethasone with a chloro moiety creates clobetasol, which binds much more tightly to the GCR. Esterification or addition of acetonide groups masks hydroxyl groups. Esterification at the 17 position of betamethasone creates betamethasone-17-valerate, which binds much more tightly to GCR and is approximately 125 times more potent than betamethasone in the vasoconstriction assay. Esterification at the 21 position of betamethasone creates betamethasone-21-valerate, which binds less tightly to the GCR but significantly increases percutaneous absorption (and potency) by increasing the molecule’s lipophilicity. Acetonide groups are formed from the 16-α, 17-α dihydroxy groups of triamcinolone and fluocinolone. Triamcinolone acetonide binds much more tightly to GCR than triamcinolone, and fluocinolone acetonide penetrates human skin and hairless mouse skin 14 to 23 times faster than fluocinolone. Fluocinolone acetonide can be further esterified at the 21 position to create fluocinolone acetonide acetate (fluocinonide), which is even more potent.
A double bond in the 1 position increases glucocorticoid activity. Halogenation at the 6-α, 9-α, or 21 position increases potency according to the position and nature of the halogen atom. An additional fluorination (difluorasone diacetate-6-α) or chlorination further enhances the potency. Addition of a 16-α methyl, 16-β methyl, or 16-α hydroxy group reduces mineralocorticoid activity; thus, these functional groups are often incorporated into molecules containing 9-α or 6-α halogens such as dexamethasone, betamethasone, and triamcinolone.
Structural modifications also affect biotransformation. Enzymes in the epidermis cause de-esterification of TCS into inactive metabolites. Halogenation at the 21 position (clobetasol propionate) inhibits de-esterification at the 17 position and significantly increases potency. Halogenation at the 9-α position also reduces biotransformation.
The vehicle is a highly engineered balance of numerous chemicals, each serving a separate or overlapping purpose. Emollients are incorporated to retard transepidermal water loss, occlude the CS molecule, and increase the flexibility of the skin. Emulsifying agents are required to create oil-in-water preparations such as creams and lotions. Other chemicals act to stabilize emulsions and thicken the final preparation. Solvents are used in lotions, solutions, gels, and sprays to create a less viscous product. Humectants are necessary in all oil-in-water preparations to maintain the required water content.
The vehicle can indirectly alter a given preparation’s therapeutic and adverse actions by altering the pharmacokinetics of the TCS molecule. Q45.2 Solvents such as propylene glycol and ethanol, for example, affect the TCS molecule’s solubility in the vehicle and skin by affecting its percutaneous absorption. The net effect of the propylene glycol is to enhance potency through increasing the percutaneous absorption. Very occlusive vehicles also enhance a TCS molecule’s percutaneous absorption, probably by increasing the hydration of the stratum corneum. For this reason, a TCS molecule in an ointment vehicle tends to be more potent than the same concentration of the molecule in a cream or lotion. Emulsifiers help to distribute the drug evenly on the skin surface. The vehicle can also directly contribute to a TCS preparation’s therapeutic effects and adverse effects (AE) (see Adverse Effects and Therapeutic Guidelines sections) and ultimately determine a given TCS preparation’s acceptance by the patient. Foams are well accepted by patients, for example, but are more costly to produce because propellant technology is relatively complex and more expensive to manufacture.
The condition of the skin also affects bioavailability. Penetration of the applied drug correlates inversely with the thickness of the stratum corneum. Penetration increases with inflamed or diseased skin, and with increased hydration of the stratum corneum, relative humidity, and temperature. The stratum corneum may also act as a reservoir for TCS for up to 5 days; this retention is TCS concentration and formulation dependent.
The list of available TCS preparations can only be matched by the list of possible mechanisms of action. An understanding of the mechanisms helps direct research toward more effective TCS derivatives.
TCS elicit their effects via binding to and activating GCR as follows: Q45.3
The CS diffuses into the target cell and binds to the GCR in the cytoplasm.
The CS–GCR complex undergoes necessary conformational changes.
The resulting active complex traverses the nuclear envelope and directly or indirectly binds to deoxyribonucleic acid (DNA).
Gene regulation and transcription of various specific messenger ribonucleic acid (mRNA) occur.
GCR are nearly ubiquitously expressed in human cells; therefore, TCS produces a myriad of actions ( Boxes 45.2 and 45.3 ). Negative gene regulation has been associated with anti-inflammatory action, whereas positive gene regulation has been associated with some AE. Research is now focused on more-selective molecules with improved therapeutic indices, accounting for the long list of GCR-mediated effects, both desirable (therapeutic benefits) and undesirable (AE).
Stabilize cell and lysosomal membranes: prevent release of lysosomal contents and phospholipid precursors for synthesis of prostaglandins and platelet-activating factor (PAF)
Potentiate vascular response to catecholamines
Reduce vascular smooth muscle sensitivity to histamine and bradykinin
Inhibit mast cell sensitization induced by immunoglobulin (Ig)E
Inhibit release of histamine and other mast cell mediators
Induction of anti-inflammatory proteins—lipocortins, vasocortin, and vasoregulin
Lipocortins inhibit phospholipase A 2 and block release of arachidonic acid and PAF from cell membranes; therefore, prevent formation of potent inflammatory mediators including prostaglandins, leukotrienes, 12-hydroxyeicosatetraenoic acid (12-HETE), and 15-HETE
Lipocortins also prevent PAF-induced wheal and flare reactions and leukocyte chemotaxis
Vasocortin and vasoregulin decrease vascular permeability
Reduce ability to adhere to vascular endothelium
Reduce migration to sites of inflammation
Reduce number at sites of inflammation
Reduce phagocytosis, bactericidal activity, release of acid hydrolases and pyrogens
Cause abnormal nitroblue tetrazolium test in vitro
Reduce number at sites of inflammation
Reduce fungicidal activity and clearance of opsonized particles
Reduce response to macrophage activating factor and decreased chemotaxis
Reduce response to mixed leukocyte reaction
Reduce response to concanavalin A-induced T-cell blastogenesis
Reduce response to tetanus toxoid and streptodornase-streptokinase
Suppress response to mixed lymphocyte reaction
Reduce antibody-dependent cell-mediated cytotoxicity
Reduce natural killer cell activity
Moderate-potency topical corticosteroid (TCS) causes decreased expression of Fc receptor, C3b receptor, and HLA-DR (Human Leukocyte Antigen – DR isotype) positivity, but no alteration in CD1a antigen expression
Superpotent TCS cause loss of cells expressing Langerhans’ cell markers
Reduce production of interleukin-1 (both IL-1α and IL-1β), interferon-γ, tumor necrosis factor, IL-2, and granulocyte–monocyte colony-stimulating factor
The following are probably both direct and glucocorticoid receptor-mediated effects
Number of keratinocyte mitoses seen diminished
Stratum corneum thickness reduced
Granular layer reduced or absent
Basal layer of keratinocytes flattened
Keratinocyte growth factors suppressed
Keratinocyte ultrastructure (keratin filaments, keratohyalin granules, membrane-coating granules) normal
Basement membrane unaffected
Melanocytes pigment production inhibited
Early Atrophy
Dermal volume reduced—decreased water content, loss of glycosaminoglycans
Hypoactive fibroblasts: suppression of procollagen I messenger ribonucleic acid transcription, reduced activity of prolyl 4-hydroxylase and lysyl oxidase, collagenase activity reduced, hyaluronate synthetase activity suppressed
Collagen and elastic fibers unchanged
Dermal volume reduced
Collagen and elastic fibers diminished and abnormally aggregated
Hypoactive fibroblasts (as above)
Dermal vessels fragile, attributed to loss of fibrous and ground substance support
TCS seems to affect every aspect of cutaneous inflammation, including inflammatory cells, chemical mediators, and tissue responses. All cells involved with inflammation are affected. Q45.4 Epidermal Langerhans cells, the antigen-presenting cell responsible for initiation of both nonspecific and acquired immune responses, are reduced in number and demonstrate decreased cellular receptors, indicating decreased antigen-presenting function. Polymorphonuclear leukocytes have less ability to adhere to vascular endothelium and are reduced in number at sites of inflammation. Their phagocytic and antibacterial capabilities are diminished. Monocytes are also decreased in number at sites of inflammation and show decreased fungicidal activity and clearance of opsonized particles. Lymphocytes demonstrate decreased antibody-dependent cellular cytotoxicity and decreased natural killer cell activity. Mast cell sensitization and mediator release induced by immunoglobulin E (IgE) are inhibited. TCS also reduces the synthesis and secretion of cytokines and inflammatory proteins necessary to initiate and sustain an immune response. Production of interleukin (IL)-1, IL-2, interferon (IFN)-γ, tumor necrosis factor, and granulocyte–monocyte-stimulating factor is reduced. TCS induces lipocortins, which inhibit phospholipase A 2 and subsequent cell surface liberation of platelet-activating factor and arachidonic acid, as well as associated potent inflammatory mediators. TCS even affects the vascular component of inflammation by augmenting the vasoconstrictive response to epinephrine and norepinephrine, and by reducing the responses to histamine and bradykinin.
Together, the anti-inflammatory properties of TCS are useful for dermatoses in which inflammation is a problem, such as atopic dermatitis (AD) and contact dermatitis, but can be deleterious for dermatoses in which inflammation is a useful host response, for example dermatophyte infections.
Q45.5 TCS reduces mitotic activity in the epidermis, leading to flattening of the basal cell layer and thinning of the stratum corneum and stratum granulosum. Levels of opioid peptides (enkephalins), which modulate epidermal differentiation and inflammatory processes, are reduced by TCS. Keratinocyte ultrastructure and the basement membrane are not affected. TCS promote atrophy of the dermis, mostly through inhibition of fibroblast proliferation, migration, chemotaxis, and protein synthesis. Fibroblast synthesis of both glycosaminoglycans (GAG) and collagen is inhibited. The loss of GAG occurs early because their normal turnover rate in the skin is 2 to 18 days. Their loss, combined with TCS-induced vasoconstriction, leads to the reduced dermal volume (water) observed after just 3 weeks of superpotent (also called ‘ultrapotent’ or ‘megapotent’) TCS application. Late dermal atrophy results from continuation of the early processes and reduction of elastin and collagen fibers, which also become abnormally aggregated. Together, the antiproliferative and atrophogenic effects of TCS are helpful in proliferative dermatoses such as psoriasis; however, these effects are injurious when TCS is used in the wrong disease, location, or potency, or in excessive quantities.
The mechanisms of systemic actions of percutaneously absorbed TCS are the same as those of systemically administered CS (see Chapter 13 ).
Box 45.4 lists the indications and contraindications for TCS, some of which are discussed here.
Dermatitis/Papulosquamous
Atopic dermatitis a
a Conditions typically very sensitive to topical corticosteroids.
FLOAT NOT FOUND
Diaper dermatitis a
Dyshidrotic eczema
Erythroderma
Lichen planus
Lichen simplex chronicus
Nummular dermatitis a
Pityriasis rosea
Psoriasis—intertriginous a
Psoriasis—plaque or palmoplantar
Seborrheic dermatitis a
Bullous pemphigoid
Cicatricial pemphigoid
Epidermolysis bullosa acquisita
Herpes gestationis (pemphigoid gestationis)
Pemphigus foliaceus
Dermatomyositis
Lupus
Behçet disease
Pyoderma gangrenosum
Alopecia areata
Acne keloidalis nuchae
Chondrodermatitis nodularis helicis
Cutaneous T-cell lymphoma, patch-stage
Granuloma annulare
Jessner lymphocytic infiltrate
Lichen planopilaris
Lichen sclerosis et atrophicus
Morphea
Pruritic urticarial papules and plaques of pregnancy
Pruritus—perianal, vulvar, scrotal
Sarcoidosis
Vitiligo
Well syndrome
Absolute
Known hypersensitivity to the topical corticosteroid
Known hypersensitivity to a component of the vehicle
Relative
Bacterial, mycobacterial, fungal, viral infection
Infestation
Ulceration
Only when potential benefits justify possible risk to the fetus
Used with caution at sites other than the breast or nipple (not known if topical corticosteroid is distributed into the breast milk).
TCS are first-line treatments for AD in all age groups; their efficacy is well established in randomized, controlled clinical trials. For adults, moderate-potency TCS is used for flares on the trunk and extremities; typically, control of the disease occurs after 2 to 3 weeks of twice-daily therapy. To finish treatment or to treat early recurrences, a lower potency of the TCS can be used twice daily (see Therapeutic Guidelines section). Fluticasone propionate 0.05% cream applied once daily was as effective as twice-daily treatment in a multicenter, randomized study. Prophylactic treatment with mometasone furoate cream twice weekly for 6 months was effective (90% disease free) in an open-label study of 68 patients; however, one patient developed skin atrophy. Desoximetasone 0.25% spray has been shown to be an effective treatment option for adults with AD, especially with itch being a major symptom. Within 1 week of starting treatment there was a significant reduction in pruritus after twice daily application. Throughout the study period of 4 weeks the reduction in pruritus was sustained and no AE occurred. Quality of life was also improved with use of desoximetasone 0.25% spray.
For children with AD, lower-potency TCS are recommended (see Therapeutic Guidelines section). Twice-daily desonide hydrogel 0.05%, flucocinolone acetonide 0.01% in peanut oil, hydrocortisone butyrate 0.1% lipocream, and once-daily fluticasone proprionate 0.05% lotion have been shown to be effective and safe for up to 1 month in children down to 3 months of age. Occasionally, intermediate-potency TCS are necessary for reasonably short courses. Betamethasone valerate 0.1% ointment applied for 3 days followed by vehicle for 4 days was as effective as hydrocortisone 1% cream applied for 7 days in an 18-week randomized, double-blinded, parallel-group study of 174 children. Mometasone furoate 0.1% cream once daily was significantly more effective than twice-daily hydrocortisone valerate 0.2% cream in a 3-week multicenter, randomized, evaluator-blinded, parallel-group study with 219 children aged 2 to 12 years. These children had failed to respond to at least 7 consecutive days of a topical hydrocortisone preparation. No treatment-related atrophy was noted in either group.
Compliance with TCS may be a very significant issue in AD patients. Adherence to regimens varies significantly, although patients may report near perfect usage.
Ceramide-based barrier creams, pimecrolimus cream, and tacrolimus ointment can augment the benefit of TCS therapy of AD in both adults and children. (see Chapter 48 .)
Fluocinonide 0.05% cream and topical tacrolimus 0.3% in clobetasol propionate 0.05% ointment have been shown to be effective in treating individuals with discoid lupus erythematosus.
Superpotent TCS alone or high-potency TCS under occlusion are effective treatments for localized granuloma annulare. Occlusive TCS preparations (such as flurandrenolide tape) and intralesional TCS treatment (such as 5–10 mg/mL triamcinolone acetonide) are also effective.
Localized cutaneous lichen planus (LP) generally responds to TCS. Fluocinonide in an adhesive base produced good to partial responses in 16 of 20 cutaneous LP patients treated in a randomized, double-blind, placebo-controlled study. TCS are also useful in the treatment of lichen planopilaris.
Oral erosive LP can be effectively treated with TCS in gels, ointments, inhalers, and rinses. Dexamethasone elixir or solution and prednisolone oral solution to be used as rinses are currently available. Mometasone furoate 1% microemulsion mouthwash three times daily over 30 days significantly reduced pain and lesion surface area in a phase II clinical trial with 49 patients. Fluticasone propionate spray four times daily and betamethasone sodium phosphate mouth rinse four times daily were both effective in a 6-week randomized, cross-over study of 48 patients. A comparative study suggested that clobetasol ointment in an adhesive base, plus antimycotics, was as effective as oral prednisone 50 mg daily. Clobetasol propionate 0.05% ointment was superior to fluocinonide 0.05% ointment in a placebo-controlled, comparative study for treatment of atrophic–erosive oral lichen planus.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here