Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The mediastinum is bounded laterally by the two lungs, anteriorly by the sternum, posteriorly by the vertebrae, superiorly by the thoracic inlet and inferiorly by the diaphragm.
The true prevalence of mediastinal masses is unknown as most surgical series are biased towards patients requiring surgery and do not include all aneurysms, intrathoracic goitres or lymph node masses in patients with established diagnoses such as lymphoma or sarcoidosis. In adult surgical series, the most frequent tumours are of neurogenic (17%–23%), thymic (20%–25%) or lymph node (10%–20%) origin (usually neoplastic). Developmental cysts, thyroid masses and germ-cell tumours constitute the next most frequent group (approximately 10% each). In children, neuroblastoma/ganglioneuroma, foregut cysts and germ-cell tumours account for over three-quarters of cases, whereas thymoma and thyroid masses are rare.
The mediastinum is divided into compartments to aid in developing a differential diagnosis and planning a surgical procedure or biopsy. There are no physical boundaries between the mediastinal compartments, and disease process can spread from one compartment to another. The mediastinum is divided into three parts: anterior, middle and posterior. A line that extends from the thoracic inlet to the diaphragm along the anterior pericardial surface and anterior to the trachea separates the anterior from middle compartments. The middle and posterior compartments of the mediastinum are separated by a line that runs 1 cm behind the anterior margins of the vertebral bodies. A new classification system divides the mediastinum into prevascular, visceral and paravertebral compartments based on anatomical structures seen on cross-sectional imaging such as multidetector computed tomography (CT). All three compartments are superiorly bound by the thoracic inlet and inferiorly by the diaphragm. The anterior compartment is bound anteriorly by the posterior cortex of the sternum and posteriorly by the anterior pericardium. The prevascular compartment contains the thymus, lymph nodes, fat and the left brachiocephalic vein. The visceral compartment is bound anteriorly by the anterior pericardium and posteriorly by a vertical line connecting a point 1 cm posterior to the anterior margin of the thoracic vertebral bodies. The visceral compartment contains most of the vascular structures. Those not contained within the visceral compartment include the left brachiocephalic vein, lymph nodes, trachea, carina, oesophagus and the thoracic duct. The extrapericardial pulmonary arteries and veins are considered pulmonary structures and not part of the visceral mediastinum. The paravertebral compartment is bound anteriorly by a vertical line connecting a point 1 cm posterior to the anterior margin of the thoracic vertebral bodies and posteriorly by a vertical line against the posterior margin of the chest wall at the lateral margin of the transverse processes of the thoracic spine. The paravertebral compartment contains the paravertebral soft tissues and the thoracic spine. Most of the abnormalities in the paravertebral compartment are neurogenic neoplasms.
Mediastinal masses are often incidentally detected on chest radiograph (CXR). Despite diagnostic limitations, the CXR is important for detecting and localising mediastinal masses when suspected clinically. The interfaces between the mediastinum and the lung parenchyma are represented as mediastinal lines visible on the CXR. Thickening, obliteration and distortion of these lines are useful signs in detecting mediastinal abnormalities on the CXR.
CT is the most useful technique for localising, characterising and demonstrating the extent of a mediastinal mass and its relationship to other structures. CT is also useful in delineating calcification and different attenuation such as fat, which can help generate a more refined differential diagnosis. CT following intravenous (IV) contrast medium with multiplanar reformats provides an excellent assessment of mediastinal structures, including vessels in the coronal and sagittal planes ( Fig. 4.1 ), and the presence or absence of enhancement in the mediastinal mass. CT can guide biopsy, plan resection and follow response to therapy.

Magnetic Resonance Imaging (MRI) is very useful in differentiating cystic from solid lesions (e.g. thymic cyst from solid neoplasms), identifying septations and solid components in cystic neoplasms and differentiating benign cysts from cystic neoplasms. MRI remains useful for imaging suspected neurogenic tumours, demonstrating intraspinal extension of a mediastinal mass and further evaluating the relationship of a mass adjacent to the heart, pericardium and larger intrathoracic vessels. MRI may have advantages over contrast media-enhanced CT for distinguishing between solid tissue and adjacent vessels (fast-flowing blood in vessels results in a signal void on spin-echo sequences) and may be useful for confirming that a mass is cystic. Unlike CT, MRI is not as sensitive to the presence of calcification.
Ultrasound (US) of the mediastinum, including echocardiography and endoscopic US, may be of use in selected patients, in particular for distinguishing cystic from solid mediastinal masses and for distinguishing cardiac from paracardiac masses. US is increasingly being used to guide mediastinal biopsy.
Radionuclide examinations have a limited role in assessing mediastinal masses. Positron emission tomography (PET) and PET/CT using [F-18]2-deoxy- d -glucose ( 18 F-FDG) have proven useful in evaluating mediastinal lymph node involvement in lung cancer and lymphoma. One of the limiting factors of PET/CT in characterising mediastinal masses is the presence of both false positives and false negatives. Thymic hyperplasia can have a variable fluorodeoxyglucose (FDG) uptake and may be as high to overlap with malignant lesions in the mediastinum. Fibrosing mediastinitis can also have high FDG uptake and thus confound with malignant lesions. Radionuclide examinations may also be useful in imaging thyroid masses, neuroendocrine tumours and phaeochromocytomas.
Localise to the mediastinum
Localise within the mediastinum
Characterise on CT or MRI
The CXR is the first step in evaluating mediastinal diseases. Findings that help in localising the lesion to the mediastinum include:
No air bronchogram
Obtuse margins with the lung
Distortion, obliteration or thickening of mediastinal lines
Abnormalities of spine, rib and sternum
The information obtained from the relationship of the normal anatomical structures representing the ‘mediastinal lines and stripes’ on CXR aid in localising the lesion within the mediastinum to the anterior, middle or posterior mediastinum and generating a differential diagnosis before proceeding to a chest CT examination.
Anterior mediastinal masses can be identified when both the hilum overlay sign and preservation of the posterior mediastinal lines are present. Widening of the right paratracheal stripe and convexity relative to the anteroposterior (AP) window reflection both indicate abnormality in the middle mediastinum. Disruption of the azygo-oesophageal recess can be caused by disease in either the middle or posterior mediastinum. Paravertebral masses disrupt the paraspinal lines, and the region of masses above the level clavicles can be inferred by their lateral margins. Posterior masses have sharp margins caused by their interface with lung, whereas anterior masses do not.
Although there is no tissue plane separating the divisions of the mediastinum, attempting to localise an abnormality within the mediastinum helps in narrowing the differential diagnosis and determining appropriate further imaging.
Localisation of the mediastinal lesion on CT is based on which compartment of the mediastinum is the centre of the lesion on the axial CT image with the largest size of the lesion and/or which mediastinal structures are displaced by the lesion (typically those that abut the compartment from which the lesion arises). The Japanese Association for Research on the Thymus (JART) study demonstrated that utilising the centre of the lesion to localise the mediastinal compartment resulted in classification of all 445 mediastinal masses to specific compartments.
Mediastinal masses can be further characterised by CT or MRI, depending on whether they contain fat, fluid or are vascular ( Table 4.1 ). An alternative, the new International Thymic Malignancy Interest Group (ITMIG) classification, is shown in Table 4.2 .
| Lesions | Fluid | Fat | Vascular | |
|---|---|---|---|---|
| Anterior | Thymoma Lymphoma Germ-cell tumour Goitre |
Thymic cyst Thymoma Pericardial cyst Germ-cell tumour Lymphoma |
Germ-cell tumour Thymolipoma Fat pad Morgagni hernia |
Thyroid Cardiac coronary aneurysm Ascending aortic aneurysm |
| Middle | Lymph nodes Duplication cyst Arch anomaly Oesophageal mass |
Duplication cyst Necrotic nodes Pericardial recess |
Lipoma Oesophageal fibrovascular polyp |
Arch anomaly Azygos vein Vascular node |
| Posterior | Neurogenic Bone and marrow |
Neuroenteric cyst Schwannoma Meningocele |
Extramedullary haematopoiesis | Descending aorta |
| More than one lesion | Infection Haemorrhage Lung Cancer |
Lymphangioma Mediastinitis |
Liposarcoma | Haemangioma |
| Lesions | Fluid | Fat | Vascular | |
|---|---|---|---|---|
| Prevascular | Thymoma Lymphoma Germ-cell tumour Goitre |
Thymic cyst Thymoma Pericardial cyst Germ-cell tumour Lymphoma |
Germ-cell tumour Thymolipoma Fat pad Morgagni hernia |
Intrathoracic goitre |
| Visceral | Lymph nodes Duplication cyst Arch anomaly Oesophageal mass |
Duplication cyst Necrotic nodes Pericardial recess |
Lipoma Oesophageal fibrovascular polyp |
Cardiac coronary aneurysm Ascending aortic aneurysm Arch anomaly Azygos vein Vascular node Descending aorta |
| Paravertebral | Neurogenic Bone and marrow |
Neuroenteric cyst Schwannoma Meningocele |
Extramedullary haematopoiesis | |
| More than one lesion | Infection Haemorrhage Lung Cancer |
Lymphangioma Mediastinitis |
Liposarcoma | Haemangioma |
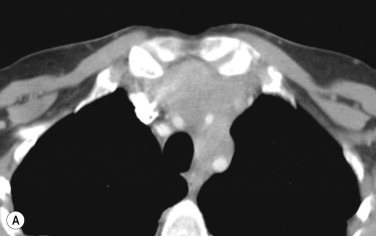
Most thyroid masses in the mediastinum represent downward extensions of either a multinodular colloid goitre or, occasionally, an adenoma or carcinoma. Approximately 3% to 17% of goitres extend into the thorax from the neck. Intrathoracic thyroid masses usually have a well-defined spherical or lobular outline (see Fig. 4.1 ). Rounded or irregular, well-defined areas of calcification may be seen in benign areas, whereas amorphous cloud-like calcification is occasionally seen within carcinomas.
Almost all intrathoracic thyroid masses displace the trachea and may cause tracheal narrowing. The direction of displacement depends on the location of the mass. Thyroid masses are most commonly anterior and lateral to the trachea. Posteriorly masses often separate the trachea and the oesophagus.
CT imaging features of mediastinal thyroid goitres include continuity of the mediastinal mass with the thyroid gland in the neck, foci of calcifications and cystic areas, high attenuation (higher than muscle) on unenhanced CT reflecting high iodine content and intense and prolonged enhancement following IV injection of iodinated contrast medium administration.
The most important of these features is to demonstrate continuity of the mass with the cervical thyroid. It is usually possible to diagnose a thyroid origin by noting a well-defined mass in the paratracheal, or sometimes retrotracheal, region, almost invariably being continuous with the thyroid gland in the neck. It is not possible to distinguish between a benign and malignant mass on CT unless the tumour has clearly spread beyond the thyroid gland. It should, however, be noted that multiple masses are a feature of benign multinodular goitre, though carcinoma can develop in multinodular goitre. MRI of intrathoracic goitre, like CT, can identify cystic and solid components, and in addition can demonstrate haemorrhage. In most practices, evaluation of the abnormal thyroid usually relies on US with biopsy.
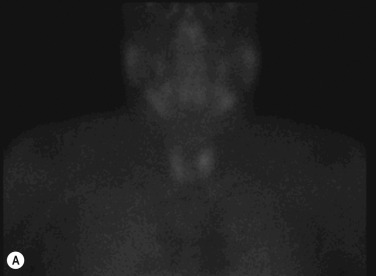
Radionuclide imaging with 123 I or 131 I demonstrates the presence of thyroid tissue within the mediastinum in almost all intrathoracic goitres. Although radionuclide imaging is a sensitive and specific method of determining the thyroid nature of an intrathoracic mass, CT is more useful as the initial technique because it provides more information should the mass prove to be something other than a thyroid lesion and is almost as specific as nuclear medicine in diagnosing a thyroid origin. CT optimally demonstrates the shape, size and position of the mass ( Fig. 4.2 ).

A parathyroid tumour is a rare cause of an anterior mediastinal mass. The parathyroid glands may migrate into the chest during fetal development. Mediastinal parathyroid tumours causing hyperparathyroidism are most commonly located in or around the thymus. In most patients with hyperparathyroidism, the aetiology lies within the parathyroid gland (either hyperplasia or a small adenoma) and escapes visualisation on CT. The role of CT or MRI is for detection of ectopic adenoma, which is suspected when no lesion is detected by US, or the hyperparathyroidism persists despite parathyroidectomy. The adenomas tend to be small and enhance homogeneously. Often, the CT is used in conjunction with 99m Tc-sestamibi imaging ( Fig. 4.3 ).
The thymus is a bilobed, triangular-shaped organ that occupies the retrosternal space and varies widely in size and shape depending on the age. After 25 years of age, the thymus is no longer discretely recognised but seen as islands of soft-tissue attenuation within a background of fat. Although the thymus may still be seen as a discrete structure in adulthood, it usually involutes and is completely replaced by fat. Anterior mediastinal masses of thymic origin include thymomas, thymic carcinoma, thymolipoma, thymic lymphoma, thymic carcinoid and thymic hyperplasia. Thymic cysts may be simple cysts and occur in an otherwise normal gland, may lie within a thymoma or may follow thymic irradiation for Hodgkin disease.
Thymomas are the most common tumour of the thymus in adults, and the most common primary tumour of the anterior mediastinum in adults. Thymomas are usually benign or low-grade malignant tumours of thymic epithelium. The average age at diagnosis is approximately 50 years, earlier in those who present with myasthenia gravis. Thymomas are extremely unusual below the age of 15 and rare under 20. Up to 50% of patients with thymoma have myasthenia gravis, and approximately 10%–20% of patients with myasthenia gravis have a thymoma. Thymomas may be encapsulated (non-invasive) or may extend beyond their capsule (invasive). A variety of other syndromes are seen in patients with thymoma, including hypogammaglobulinaemia and pure red cell aplasia.
Most thymomas (90%) arise in the superior aspect of the anterior mediastinum. A few are situated more inferiorly, projecting from the left or right heart border, or lying close to the cardiophrenic angles ( Fig. 4.4 ). They are usually spherical or oval in shape and may show lobulated borders. Thymomas may demonstrate cystic changes, haemorrhage or necrosis. A few thymomas are predominantly cystic and some thymomas may demonstrate punctate or curvilinear calcifications. CT is the most sensitive technique to detect all of these features and to help detect a thymoma in patients with myasthenia gravis. Thymomas as small as 1.5–2.0 cm in diameter are readily identified in men and women over the age of 40, largely because the rest of the thymus is atrophic. Diagnosing a small thymoma in those patients younger than age 40, and particularly younger than 30, can be difficult because the normal gland is variable in size and in myasthenia gravis the associated hyperplasia may cause a bulky gland. Fortunately, thymoma is so infrequent in children that the potentially difficult problem of finding a thymoma in a child with myasthenia gravis rarely arises.
Thymomas usually show homogeneous density and uniform enhancement after contrast media injection and may occasionally be cystic. Most thymomas are completely encapsulated but approximately 30%–60% show degrees of invasion of the tumour capsule. Invasion of the mediastinal fat and adjacent pleura may be identified with invasive thymomas, and while CT shows such invasion, it cannot reliably diagnose invasive thymoma if the tumour is still confined to the thymus. Pleural metastases resulting from transpleural spread are a feature of invasive thymomas, and therefore the whole of the pleural cavity should be carefully examined. On MRI, the normal thymus in children and young adults characteristically demonstrates homogeneous and intermediate T 1 and T 2 weighted signal intensity, less intense than mediastinal fat but greater than muscle. In older patients after puberty, the T 1 and T 2 signals increase with age because the thymus begins to involute and is replaced by fat. Thymomas typically demonstrate low T 1 signal intensity similar to muscle and relatively high T 2 signal intensity. MRI can be useful for showing mediastinal involvement when CT is not definitive. T 2 weighted images occasionally show lobulated internal architecture and scattered areas of high intensity that correspond to fibrous septa and cystic areas (see Fig. 4.4 ). Heterogeneity of signal intensity caused by septation, cystic change and haemorrhage is common.
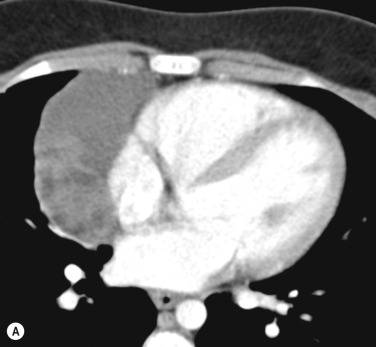
Invasive thymomas invade beyond the capsule into the mediastinum and can involve the pleura and pericardium. Complete obliteration of the adjacent fat planes suggests mediastinal invasion ( Fig. 4.5 ). Complete preservation of the adjacent fat planes excludes extensive invasive disease but does not rule out minimal capsular invasion. Certain findings such as encasement of mediastinal structures, infiltration of fat planes and an irregular surface between the mass and lung parenchyma are highly suggestive of invasion by the tumour. Pleural thickening, nodularity and the presence of an effusion generally indicates invasion by the thymoma. MRI is superior to CT for defining the invasion of contiguous structures such as the pleura and pericardium in patients with invasive thymoma but is not used in most cases.
Most common thymic tumour in adults
Usually benign or low-grade malignant thymic epithelial tumours
Average age of diagnosis is age 50
Myasthenia gravis develops in up to 50%
Less commonly develop hypogammaglobulinaemia and pure red cell aplasia
Absence of, or extension into, the capsule indicates an invasive nature
Complete obliteration of the adjacent fat planes suggestive of mediastinal invasion
Absence of obliteration of adjacent fat does not exclude capsular invasion
MRI more sensitive than CT in showing mediastinal involvement when CT is not definitive
Pleural thickening, nodularity or the presence of an effusion generally indicates invasion
CT , Computed tomography; MRI , magnetic resonance.

Thymic carcinoma is a thymic epithelial tumour with a high degree of anaplasia, cell atypia and increased proliferation. It accounts for about 20% of thymic epithelial tumours and predominantly occurs in adults. Thymic carcinomas have a poor prognosis despite treatment with surgery and radiotherapy. Thymic carcinomas are aggressive, locally invasive malignancies that have frequently metastasised to regional lymph nodes and distant sites at presentation. Although only about 5% of patients with invasive thymomas have distant metastasis at diagnosis, 50%–65% of patients with thymic carcinomas have distant metastases at diagnosis. They are typically large, heterogeneous masses, containing areas of necrosis and calcification, often demonstrating evidence of invasion of adjacent structures, in particular the mediastinum, pericardium and pleura ( Fig. 4.6 ). Thymic carcinomas lack a well-defined capsule, whereas two-thirds of thymomas are encapsulated. On MRI, thymic carcinoma demonstrates intermediate signal intensity, slightly higher than muscle on T 1 weighted sequence, and high signal intensity on T 2 weighted sequence. Thymic carcinomas are more commonly associated with mediastinal node and extrathoracic metastasis, but less commonly associated with pleural implants compared with invasive thymomas. In general, before considering a diagnosis of thymic carcinoma on imaging, more common metastatic carcinomas should be considered.

Primary neuroendocrine tumours (carcinoids) of the thymus are rare, well-differentiated neuroendocrine tumours and account for less than 5% of anterior mediastinal tumours. Unlike pulmonary carcinoids, these tumours are aggressive and at least 20% of patients have distant metastasis at presentation to the liver, lung, bone, pleura and pancreas. Approximately 40% of patients have Cushing syndrome because of adrenocorticotrophic hormone secretion by the tumour, and up to 20% have multiple endocrine neoplasia (MEN) syndromes I and II.
Thymic carcinoid is histologically distinct from thymoma, although their imaging features overlap. On CT or MRI, the tumours appear as a lobulated thymic mass with heterogeneous enhancement ( Fig. 4.7 ) and central areas of low attenuation secondary to necrosis or haemorrhage; local invasion may also be seen. Bone metastasis is typically osteoblastic. Thymic carcinoids are more aggressive than thymomas and cause more frequent superior vena cava (SVC) obstruction.
Thymolipomas are rare, benign, well-encapsulated tumours composed of a mixture of mature fat and normal-looking or involuted thymic tissue that account for about 5% of thymic neoplasms. The reported age range is 3–60 years. The average age of the patient is 22–26 years and most patients are asymptomatic. These tumours occur low in the anterior mediastinum, and often extend to the cardiophrenic angle as their pliability allows them to conform to adjacent structures. Thymolipomas can grow to a very large size before discovery and, being soft, mould themselves to the adjacent mediastinum and diaphragm, and may mimic cardiomegaly or lobar collapse. Individual cases have been reported in association with a variety of conditions, including myasthenia gravis, aplastic anaemia, Graves disease and hypogammaglobulinaemia. CT shows the fatty nature of the mass, with islands of thymus and fibrous septa running through the lesion. On MRI, fat within the tumour appears as high signal intensity and soft tissue appears as low signal intensity bands coursing through the mass. CT and MRI generally reveal a connection between the tumour and the thymus.
The most common association of lymphofollicular thymic hyperplasia is myasthenia gravis (seen in 50% of patients with myasthenia gravis), but lymphofollicular thymic hyperplasia is also seen in other conditions, such as thyrotoxicosis, systemic lupus erythematosus (SLE), Hashimoto thyroiditis and Addison disease. Thymic hyperplasia is rarely severe enough to cause visible enlargement of the thymus. When it does enlarge the thymus, both lobes are enlarged, usually uniformly ( Fig. 4.8 ). Only rarely, hyperplasia may mimic a thymic mass.
The thymus may atrophy because of stress or as a consequence of steroid or chemotherapy. The gland usually returns to its original size on recovery or cessation of treatment, but it may become larger than its original size (rebound thymic hyperplasia). Among patients who undergo chemotherapy, approximately 10%–25% may develop rebound hyperplasia, which occurs usually within 2 years of chemotherapy. Such rebound hyperplasia may be difficult to distinguish from neoplastic involvement. The diagnosis depends on a known reason for thymic rebound, the absence of clinical features to indicate tumour recurrence and the presence of an enlarged, normally shaped thymus. Thymic rebound hyperplasia typically shows diffuse enlargement, a smooth contour, a mixture of fat and lymphoid tissue, and normal vessels; whereas, thymic neoplasia is usually associated with a nodular contour and frequently contains necrotic or calcified foci. In patients over 15 years with an enlarged thymus, chemical shift MR and fat-suppressed T 2 weighted or short tau inversion recovery (STIR) imaging can diagnose thymic hyperplasia by detecting fatty infiltration or fat in the thymus, helping to differentiate from a neoplastic process. In thymic hyperplasia there is a drop in signal intensity at opposed phase images, while in thymic tumours there is no such reduction in signal. Chemical-shift MRI can depict physiological fatty infiltration of the thymus in 50% of persons aged between 11 and 15 years old, in 100% of those older than 15 years old, but in none of those under 15 years old.
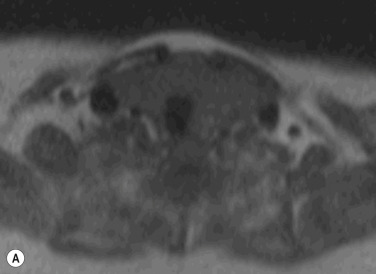
Thymic cysts are uncommon, representing 1% of all mediastinal masses. They can be congenital or acquired. Congenital thymic cysts are derived from a patent thymopharyngeal duct and are usually unilocular. Approximately 50% of thymic cysts are discovered in those under 20 years old. Acquired thymic cysts are multilocular and occur in association with thymic tumours, Langerhans cell histiocytosis or radiation therapy for Hodgkin disease. On CXRs, thymic cysts are indistinguishable from other thymic masses. On CT, simple congenital thymic cysts are seen as well-defined water attenuation masses with imperceptible walls. Multilocular thymic cysts appear as well-defined heterogeneous masses with imperceptible walls. On MRI, thymic cysts demonstrate typical characteristics of fluid with low T 1 and high T 2 signal intensity ( Fig. 4.9 ). If haemorrhage or infection occurs, then the cysts can demonstrate high signal on both T 1 and T 2 weighted images.

Germ-cell tumours account for 10%–15% of anterior mediastinal masses in adults and approximately 25% in children. Germ-cell tumours of the mediastinum are believed to be derived from primitive germ-cell elements left behind after embryonal cell migration. The mediastinum is the most common extragonadal site for these tumours, approximately 60% of which arise in the anterior mediastinum. Most germ-cell tumours present during the second to fourth decades of life. Mediastinal germ-cell tumours include teratoma and a number of malignant forms, chiefly seminoma and non-seminomatous germ-cell tumours such as embryonal carcinoma, choriocarcinoma, endodermal sinus tumour and tumours with mixtures of these cell types. Malignant germ-cell tumours secrete human chorionic gonadotrophin and α-fetoprotein, which can be used as markers to diagnose and monitor the tumour. Malignant germ-cell tumours are almost always seen in male patients.
Teratomas contain elements of all three germinal layers: ectoderm (skin, teeth, hair), mesoderm (bone, cartilage, muscle) and endoderm (bronchial or gastrointestinal epithelium). Teratomas are the most common mediastinal germ-cell tumour and most are cystic. Teratomas are found at all ages, particularly in adolescents and young adults, with women slightly outnumbering men. They are usually asymptomatic and diagnosed incidentally on chest radiography or CT, but may give rise to cough, dyspnoea or chest pain if they compress the bronchial tree or SVC, or if they rupture into the mediastinum or lung. Teratomas are usually stable, but haemorrhage or infection may lead to a rapid increase in size. Teratomas are classified as mature, immature and malignant. Mature teratomas represent approximately 60%–70% of all mediastinal germ-cell tumours. They are composed of well-differentiated benign tissues with a predominant ectodermal element and often referred to as dermoid cysts. Immature teratomas contain various adult tissues, but also contain foci of primitive, less well-organised tissue. Teratoma with malignant transformation contains frankly malignant tissues. Teratomas usually have a benign course and surgical resection is the treatment of choice on the small chance that few malignant elements are present. Malignant teratomas have a poor prognosis.
On CXR or CT most teratomas present as a well-defined, rounded or lobulated mass, localised to the anterior mediastinum. Fat and calcification may rarely be identified on CXR. Teratomas may have variable appearances on CT. Combinations of fat, fluid, soft-tissue components and calcification may be seen in teratomas ( Fig. 4.10 ).

MRI is useful in differentiating teratoma from thymoma and lymphoma. Soft-tissue elements in the teratoma are isointense to muscle, cystic elements demonstrate low T 1 intensity and high T 2 intensity, and fat appears as high T 1 intensity with signal loss on fat-saturation sequence. Fat is virtually diagnostic of teratoma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here