Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Define the pathologies discussed in this chapter and describe their causes, clinical signs, and sonographic findings
Explain sonohysterography and the indications for performing the procedure
Identify the role of Doppler in evaluating pelvic pathology
Differentiate among the types of intrauterine contraceptive devices and describe the sonographic appearance of each
Sonography is traditionally applied in the female pelvis to delineate the size, texture, vascularity, and structure of pelvic anatomy. The examination may also supply information on the morphology of malfunctioning organs that seem normal on pelvic examination. Small, nonpalpable submucosal myomas or polyps may cause abnormal bleeding. The localization of intrauterine contraceptive devices (IUCDs) may be assessed by pelvic ultrasound examination. The homogeneity of the myometrium is assessed, and the thickness of the endometrial cavity is measured, in addition to the length and width of the uterus and cervix. Both transabdominal and transvaginal sonography are important in these evaluations. Transabdominal imaging furnishes a survey of anatomy, whereas transvaginal imaging provides better characterization of internal architecture of the vagina, cervix, and uterus. Color and spectral Doppler sonography can also play a role in assessing normal and pathologic blood flow, as well as identify vessels separate from fluid-filled structures. Newer techniques include sonohysterography, a process in which a small catheter, placed under ultrasound guidance, introduces sterile saline into the endometrial canal to provide a detailed evaluation of an intracavitary, endometrial, or submucosal lesion. Additionally, three-dimensional (3D) ultrasound now provides us with coronal representation of the uterus. Other imaging modalities used to evaluate pelvic anatomy and pathology include magnetic resonance imaging (MRI) and computed tomography (CT). These two modalities are particularly useful in the staging of malignant disease.
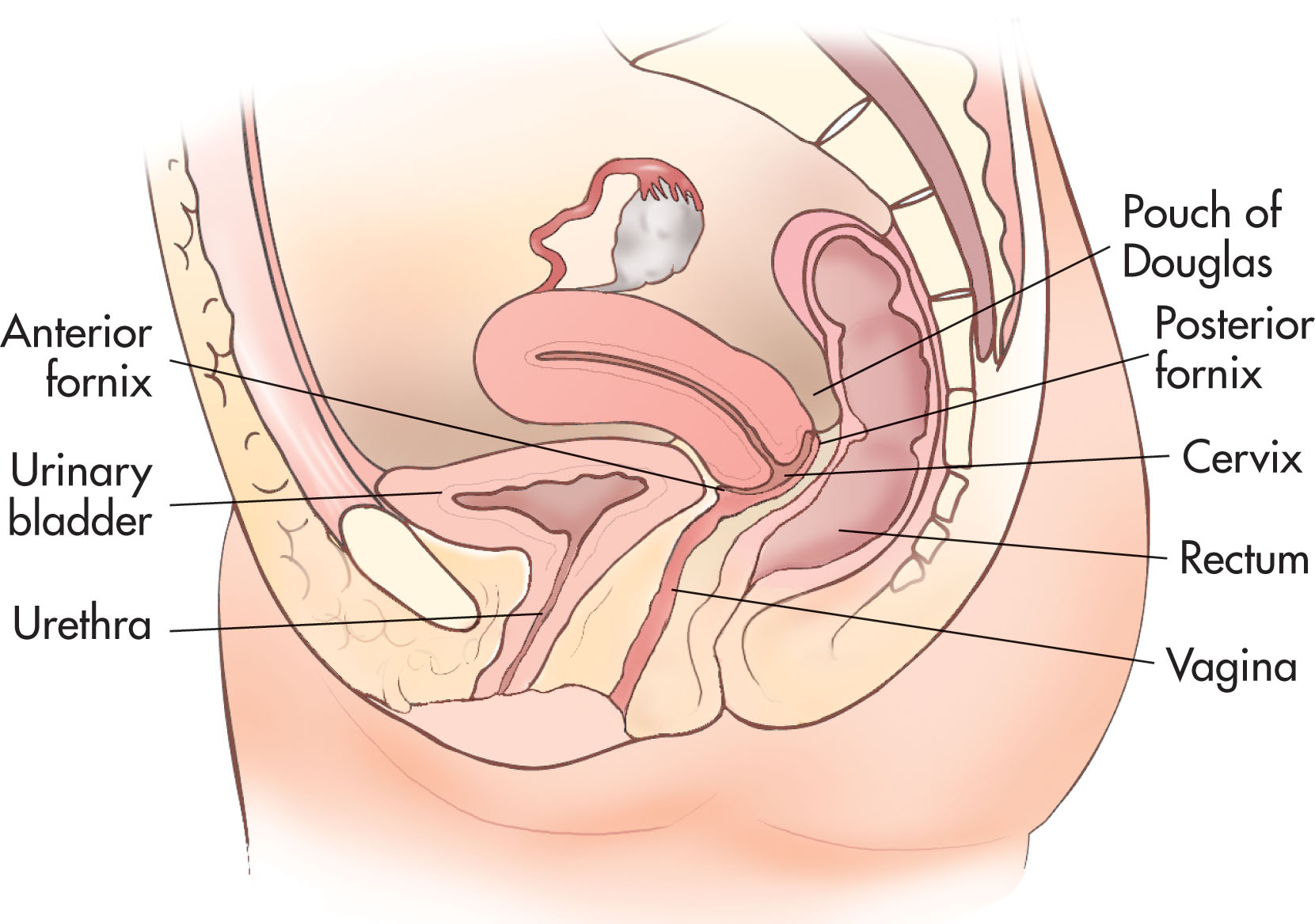
The vagina runs anterior and caudal from the cervix, between the bladder and rectum ( Fig. 43.1 ). Occasionally, sonography is used to characterize a vaginal mass, such as a Gartner duct cyst . These are the most common cystic lesions of the vagina and usually are found incidentally during sonographic examination ( Fig. 43.2 ). The most common congenital abnormality of the female genital tract is an imperforate hymen that results in obstruction. Obstruction of the uterus or the vagina may result in an accumulation of fluid (hydrometra), blood (hematometra), or pus (pyometra).
Solid masses of the vagina are rare. As with carcinoma of the cervix, sonography is not used for diagnosis of carcinoma of the vagina, but it may play a role in staging. When found, the lesion is usually vaginal adenocarcinoma or rhabdomyosarcoma. The lesions appear as a solid mass, occasionally with areas of necrosis. Translabial scanning may be used to best evaluate the vaginal area (see Chapter 42 ).
A vaginal cuff is seen in hysterectomy patients after surgery. The upper size limit of a normal vaginal cuff is 2.1 cm. If the cuff is larger than this or contains a well-defined mass or areas of high echogenicity, it should be regarded with suspicion for malignancy, especially in the patient who has a previous history of cancer. Nodular areas in the vaginal cuff may be due to post-irradiation fibrosis.
The rectouterine recess (posterior cul-de-sac) is the most posterior and inferior reflection of the peritoneal cavity (see Fig. 43.1 ). It is located between the rectum and uterus and is also called the pouch of Douglas. Because of its location, it is frequently the site of intraperitoneal fluid collections. As little as 5 mL of fluid has been detected by transvaginal sonography. Fluid in the cul-de-sac is a normal finding in asymptomatic women and can be seen during all phases of the menstrual cycle. Pathologic fluid collections may be associated with ascites, blood resulting from a ruptured ectopic pregnancy, hemorrhagic cyst, or pus resulting from an infection. Pelvic abscesses and hematomas can also occur in the cul-de-sac. Sonographic characteristics help to differentiate these findings ( Fig. 43.3 ).

Transvaginal sonography should be utilized to obtain high-quality images of the cervical area. The cervix lies posterior to the bladder between the lower uterine segment and the vaginal canal (see Fig. 43.1 ). The cervical canal extends from the internal os where it joins the uterine cavity, to the external os, which projects into the vaginal vault. It is a cylindrical portion of the uterus that enters the vagina and measures 2 to 4 cm in length. Transvaginal scanning of the cervix is performed after the patient empties her bladder. The transducer is inserted into the vagina with the patient supine, knees gently flexed, and hips elevated on a pillow. After the uterine cavity has been examined, the probe should be slowly pulled back slightly to image the internal and external cervical os. In the sagittal view, the handle of the transducer is slowly moved upward or back to better image the cervix (see Chapter 42 ). With gentle rotation and angulation of the transducer, coronal images are also obtained.
The most common finding is the presence of nabothian cysts ( Box 43.1 ), which result from chronic cervicitis and are seen frequently in middle-aged women. This cyst results from an obstructed dilated transcervical gland and is also called epithelial inclusion cyst.
Benign cysts in cervix
Chronic inflammatory retention cysts
Asymptomatic
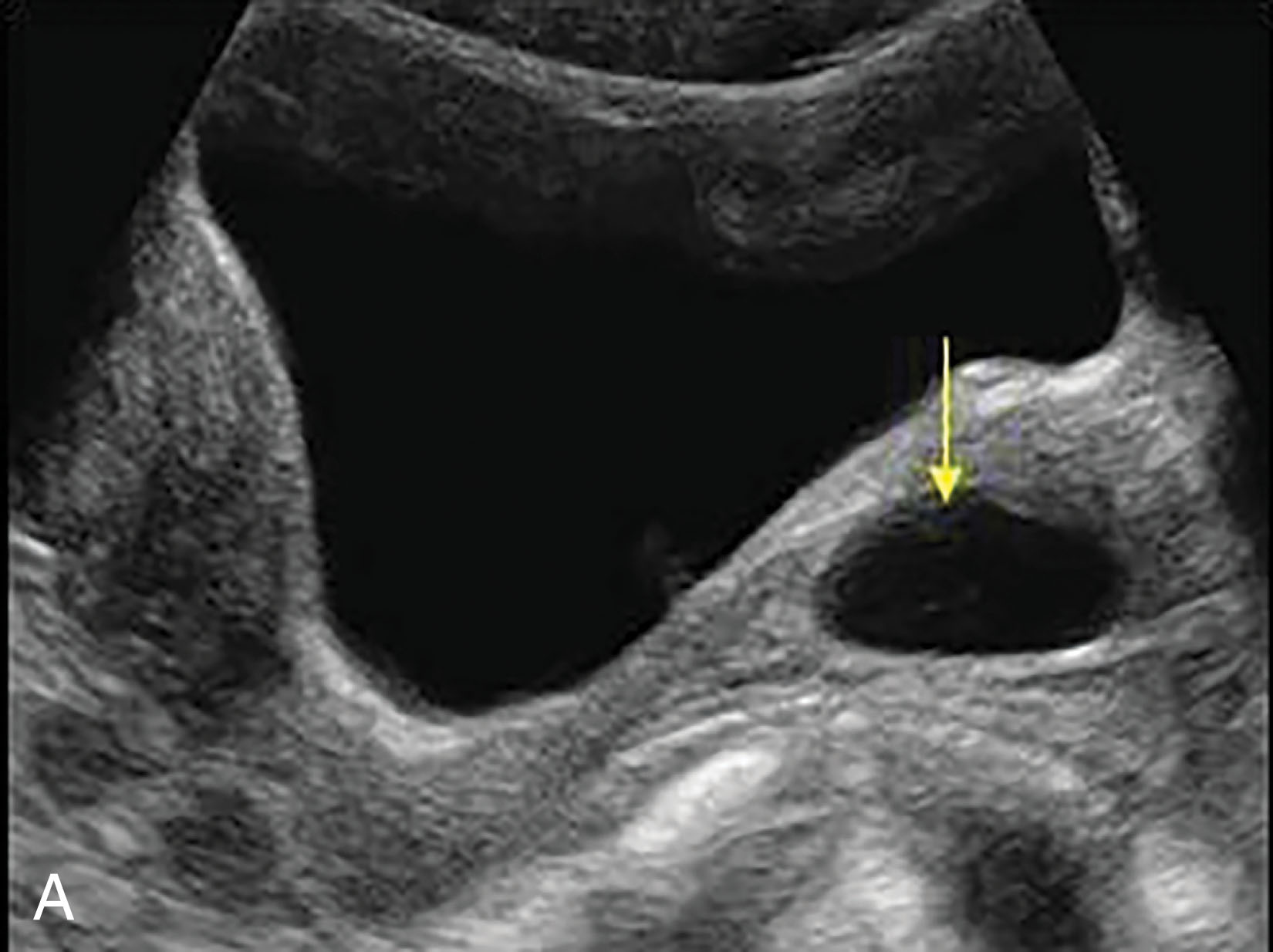
On sonographic evaluation, these lesions appear along the cervical canal as discrete, round, fluid-filled anechoic structures, usually measuring less than 2 cm; they may be multiple ( Fig. 43.4 ). Occasionally, nabothian cysts may have internal echoes that may be caused by hemorrhage or infection.
Cervical polyps may present clinically with irregular bleeding. This benign condition arises from the hyperplastic protrusion of the epithelium of the endocervix or ectocervix . Chronic inflammation is the most likely factor. The polyps may be pedunculated, projecting out of the cervix, or broad-based, and ultrasound may or may not see cervical polyps, depending on their location ( Fig. 43.5 ). Women in their late middle age are more likely to develop polyps.
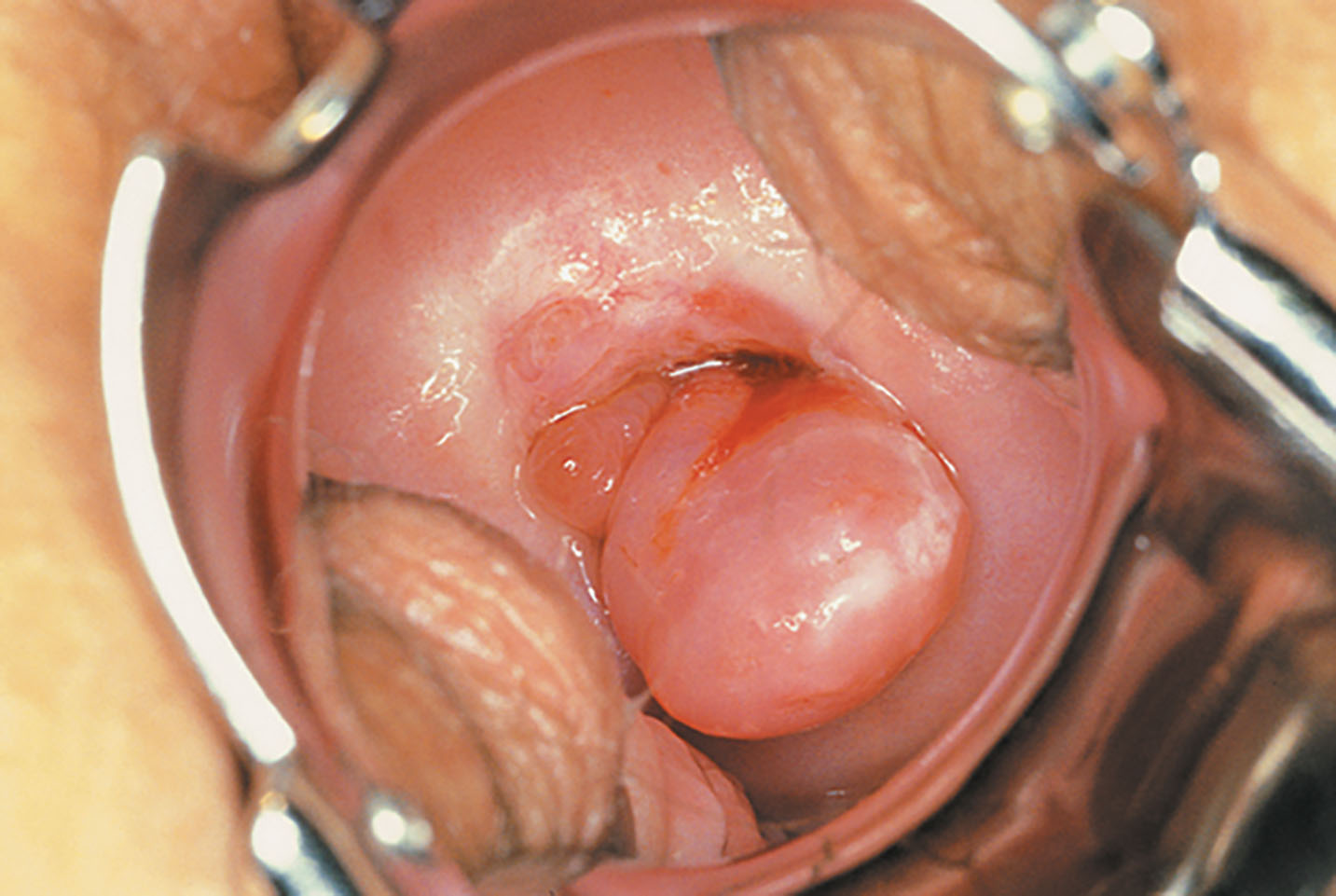
A small percentage of leiomyomas (myoma tumors) occur in the cervix ( Fig. 43.6 ). When the myomas are small, the patient is asymptomatic, but as the mass enlarges, bladder or bowel obstruction may result. The myoma may be pedunculated and prolapse into the vaginal canal. Sonography may assist in determining the location of the stalk and the thickness of the stalk. Fluid infusion with sonohysterography enhances this visualization.
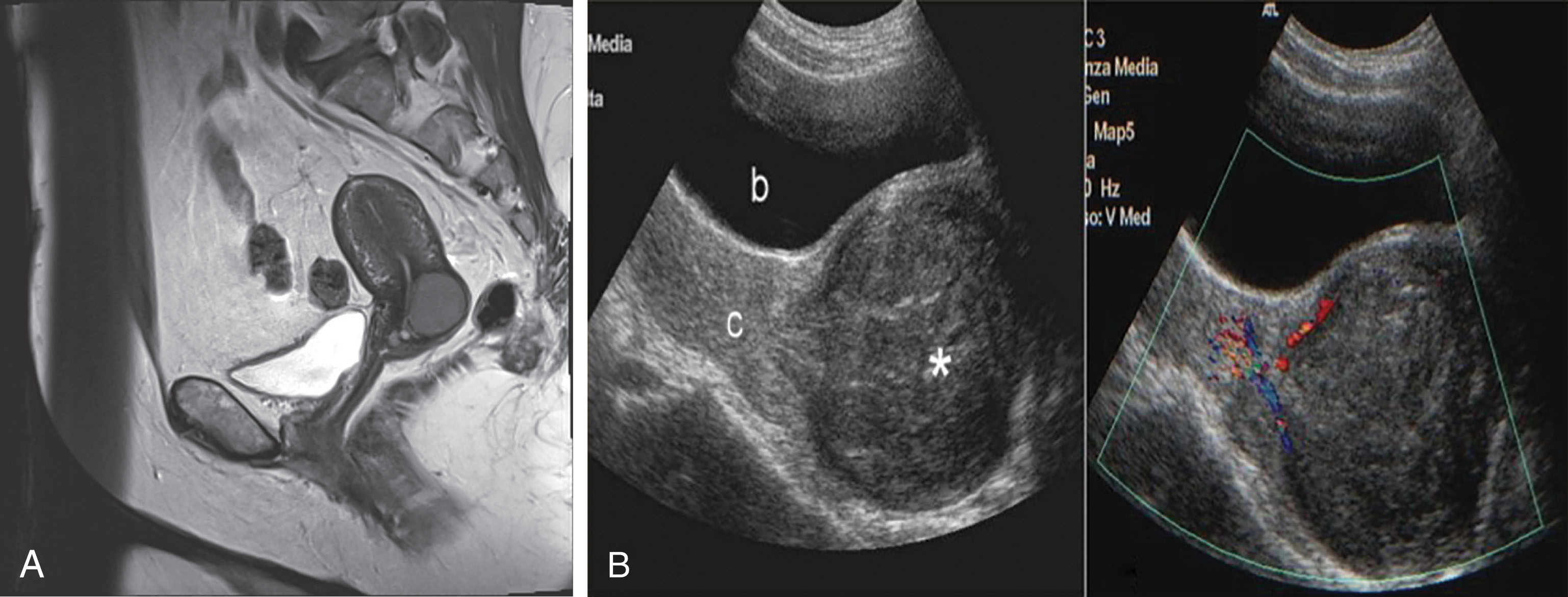
Cervical stenosis is an acquired condition with obstruction of the cervical canal at the internal or external os, resulting from radiation therapy, previous cone biopsy, postmenopausal cervical atrophy, chronic infection, laser or cryosurgery, or cervical carcinoma. The menopausal patient may be asymptomatic even though the stenosis can produce a distended, fluid-filled uterus ( Fig. 43.7 ), the result of an accumulation of uterine secretions, fluid (hydrometra), pus (pyometra), or blood (hematometra). Intracavitary fluid collections can be readily seen on ultrasound and may be an indirect indicator of cervical stenosis. Premenopausal patients may experience abnormal bleeding, oligomenorrhea or amenorrhea, cramping, dysmenorrhea , or infertility.
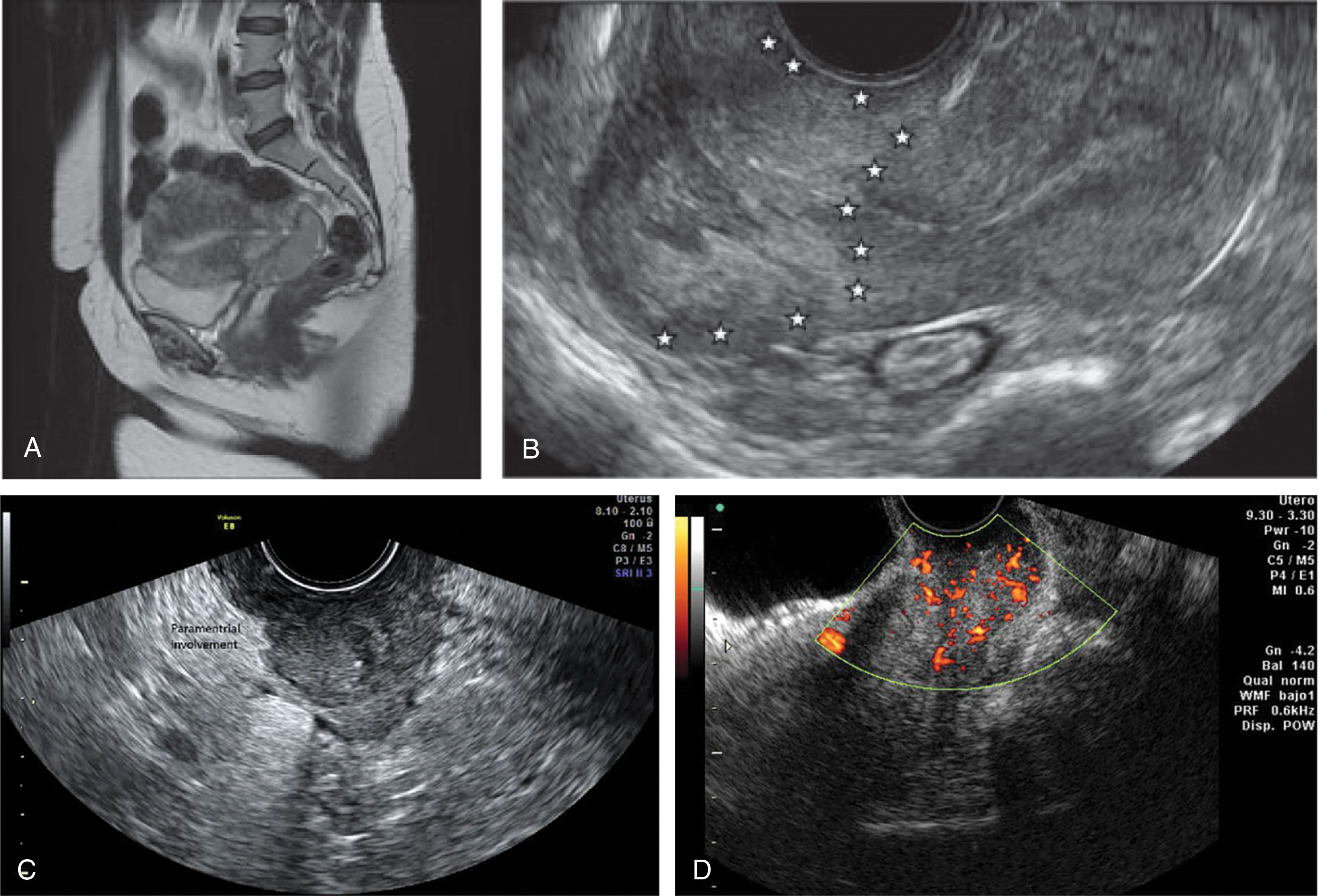
Squamous cell carcinoma is the most common type of cervical cancer. Precursors to this disease are the cervical dysplasias classified as mild, moderate, or severe. When the full thickness of the epithelium is composed of undifferentiated neoplastic cells, the lesion is referred to as carcinoma in situ. The detection of these abnormalities is attributed to screening with Papanicolaou (Pap) smears because most of the early lesions are asymptomatic. Advanced cervical cancer is usually evident clinically ( Box 43.2 and Fig. 43.8 ). Sonography may demonstrate a solid retrovesical mass, which may be indistinguishable from a cervical myoma. Transvaginal and translabial ultrasound may demonstrate bladder, ureteral, vaginal, or rectal involvement and may be used in staging cervical cancer. CT and MRI are preferable, however, because they are superior methods for staging and evaluating lymphatic spread. Areas of increased echogenicity or hypoechoic areas with an irregular outline signify changes compatible with cervical carcinoma ( Fig. 43.9 ). Multiple cystic areas within a solid cervical mass are a rare cervical neoplasm arising from the endocervical glands termed adenoma malignum or minimal deviation adenocarcinoma . Ultrasound is also helpful in guiding biopsies of the cervix and vagina.
Affects women of menstrual age
Clinical findings: Vaginal discharge or bleeding
Sonographic findings: Retrovesical mass, obstruction of ureters, invasion of bladder
Translabial or transperineal sonography may be used instead of or with the transvaginal approach to help define the cervical area. A 5.0 to 7.5 MHz sector or curvilinear transducer is covered with a sterile probe cover and applied to the vestibule of the vagina in the sagittal plane. Partial bladder filling may assist visualization of the cervical area. Rotation of the transducer obliquely in a counterclockwise direction shows the coronal images and defines the second plane for visualization. Positioning the patient with the hips elevated, as in the transvaginal approach, helps to displace pelvic gas and identify anatomy. Limitations can be overcome by elevation of the hips, better application of the transducer to the perineum, or changes in the orientation of the probe.
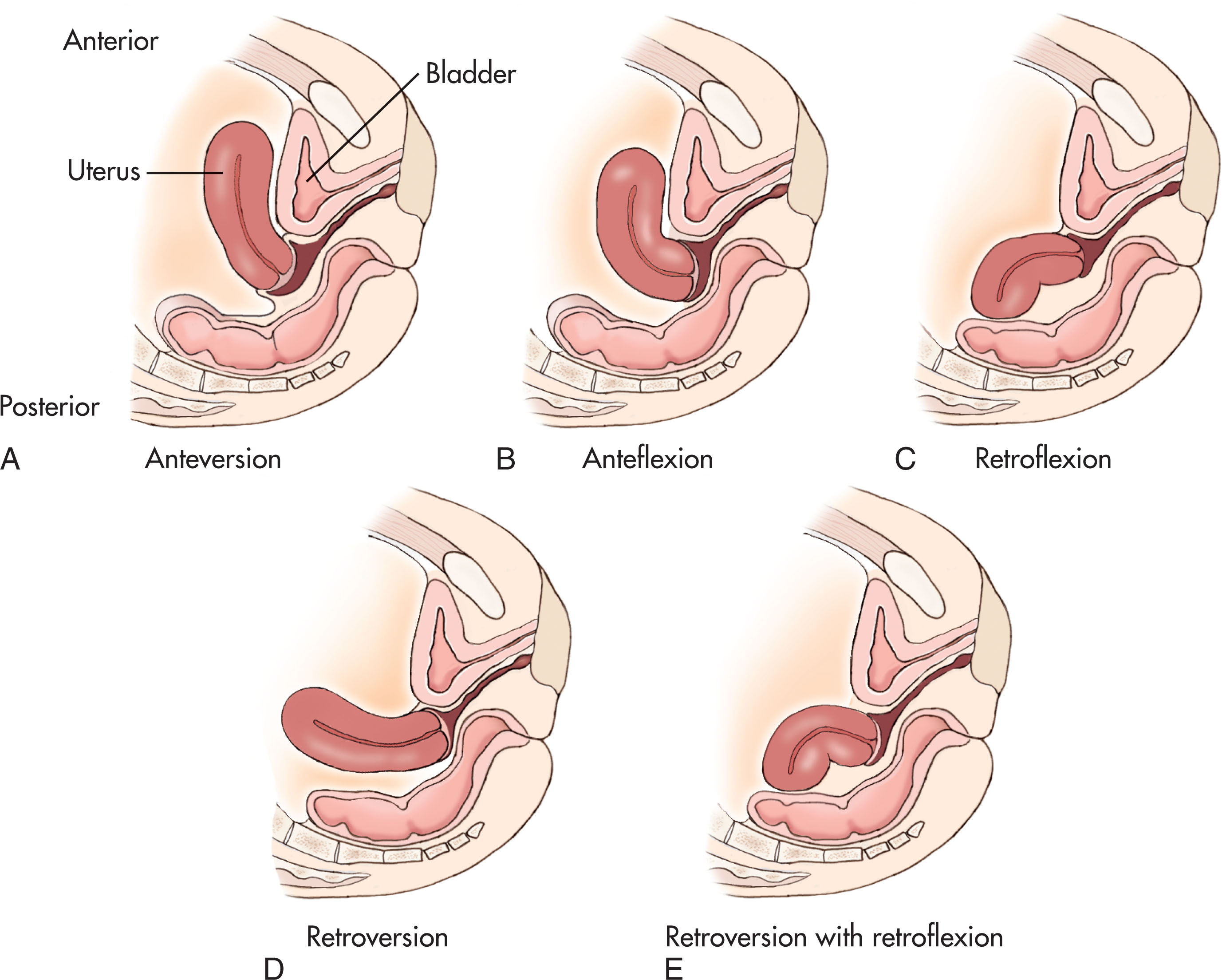
The uterus lies in the true pelvis between the urinary bladder anteriorly and the rectosigmoid colon posteriorly (see Fig. 43.1 ). Uterine position is variable and changes with the degrees of bladder and rectal distention. The body of the uterus may lie obliquely on either side of the midline, which may mimic a mass on physical examination. Flexion refers to the axis of the uterine body relative to the cervix. Version refers to the axis of the cervix relative to the vagina. The uterus is usually anteverted and anteflexed. It may also be retroflexed (when the body tilts posteriorly) or retroverted (when the uterine fundus tilts backward) ( Fig. 43.10 ). Transvaginal sonography has proven to be excellent for assessing the retroverted or retroflexed uterus because the transducer is close to the posteriorly located fundus. The size and shape of the normal uterus are related to age, hormonal status, and parity.
Common differential considerations for pathology of the uterus are seen in Box 43.3 .
Pregnancy
Postpartum
Leiomyoma
Adenomyosis
Bicornuate or didelphic uterus
Leiomyoma
Carcinoma
Early intrauterine pregnancy
Endometrial hyperplasia
Retained products of conception or incomplete abortion
Trophoblastic disease
Endometritis
Adhesions
Polyps
Inflammatory disease
Endometrial carcinoma
Endometritis
Retained products of conception
Pelvic inflammatory disease
Cervical obstruction
Gas (abscess)
Intrauterine device
Calcified myomas or vessels
Retained products of conception
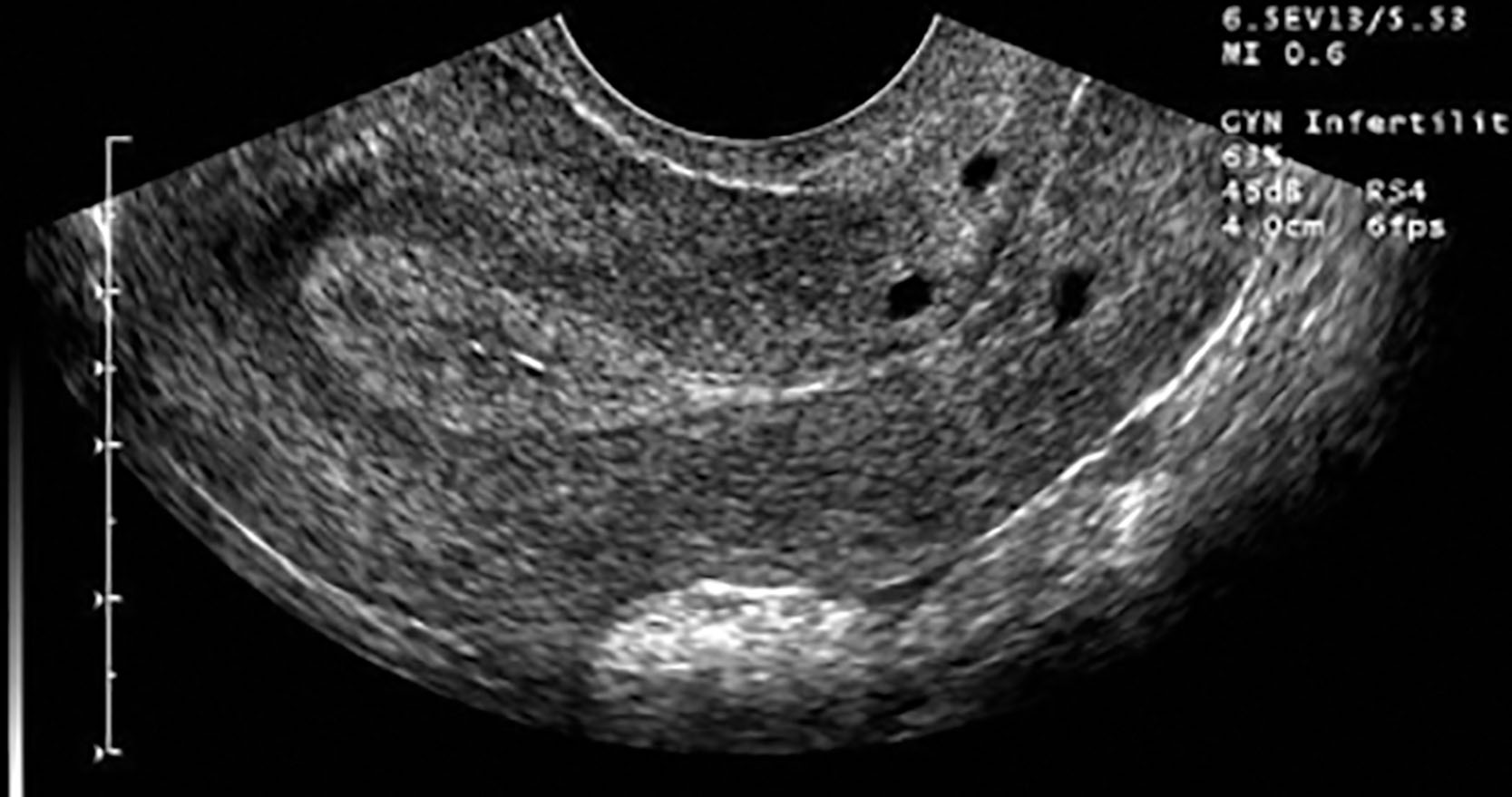
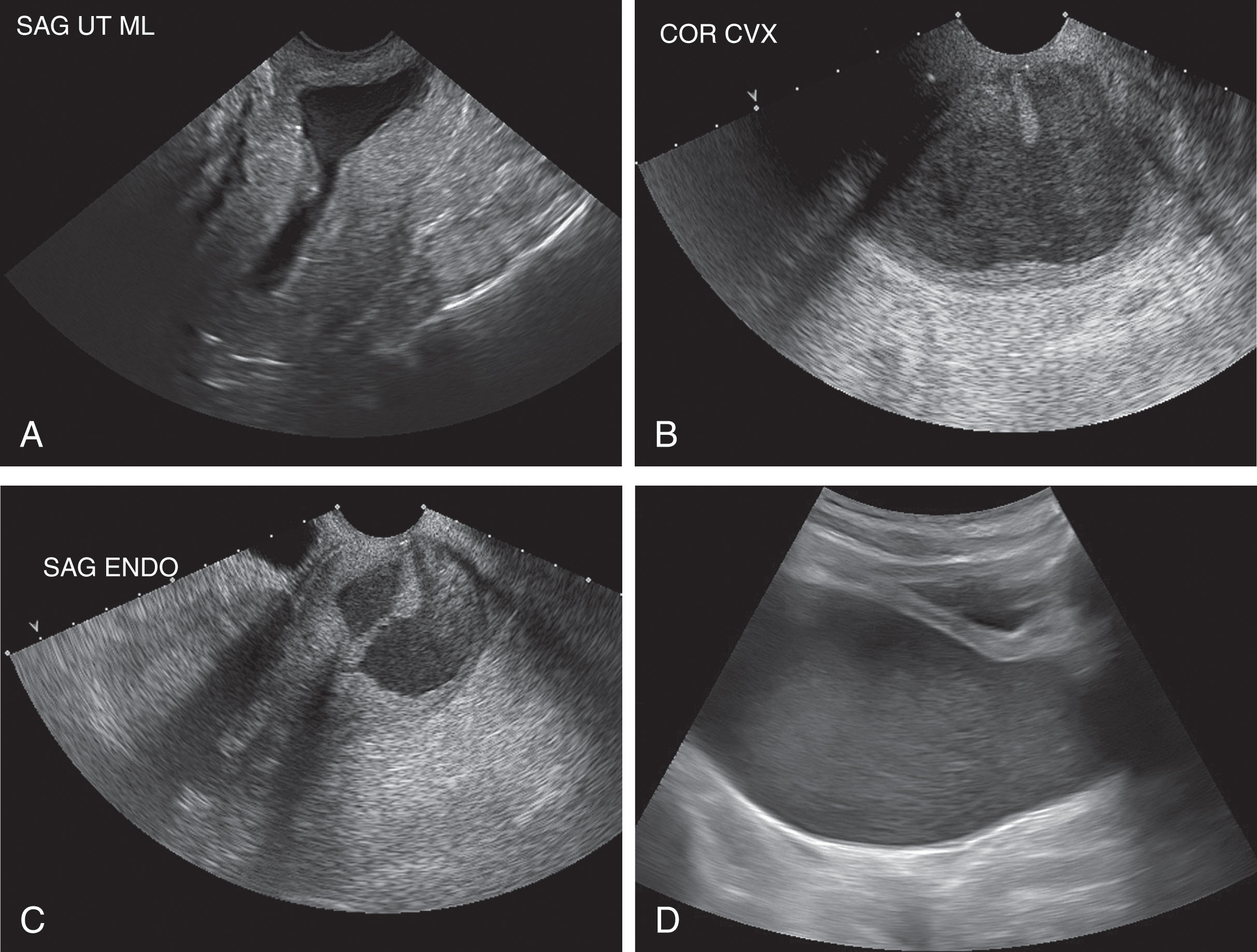
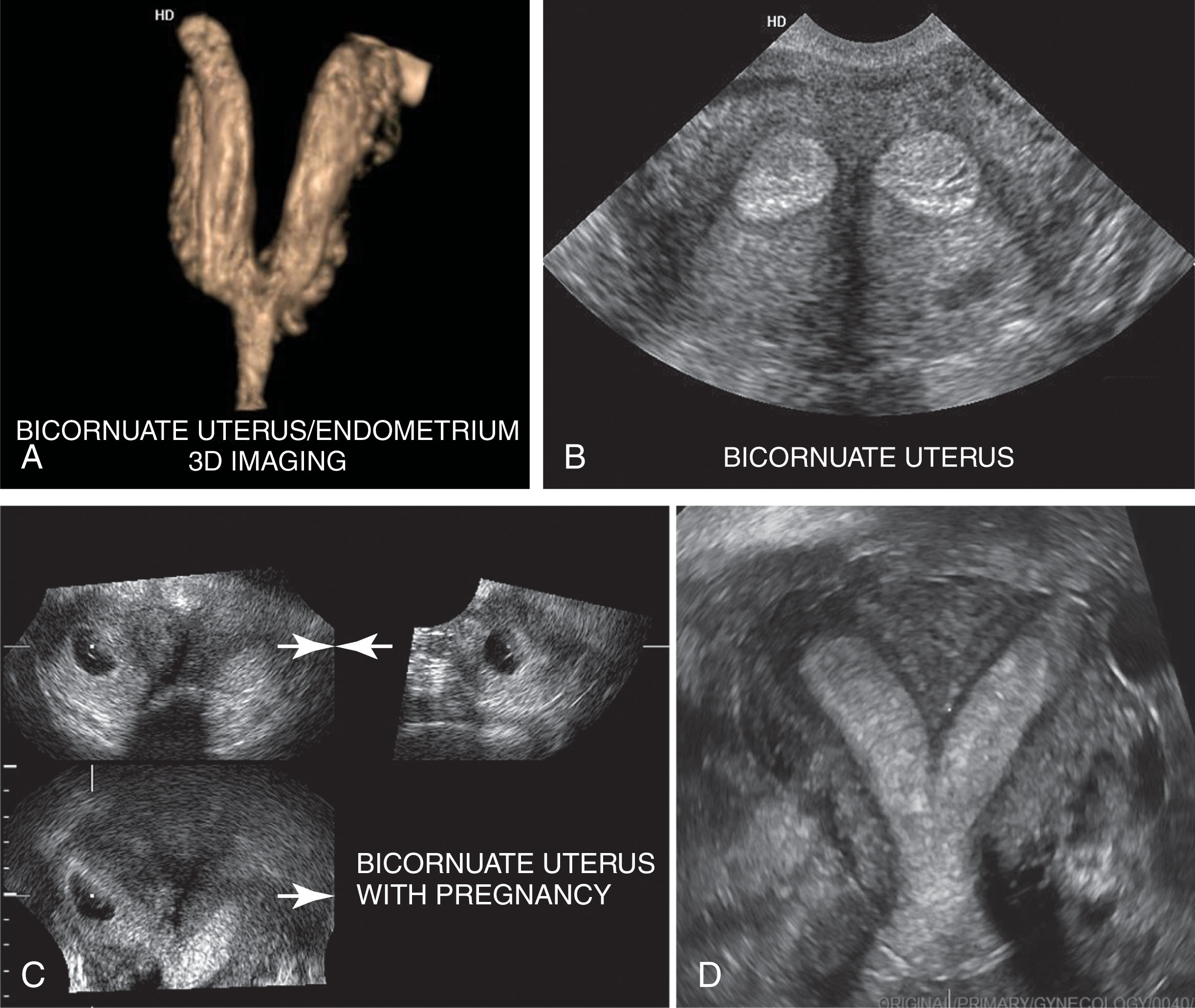
Ultrasound is the first clinical examination ordered to evaluate the enlarged uterus. There are common variations of uterine morphology, the bicornuate—or “two-horned uterus”—and the didelphic uterus, that can be visualized with great specificity with sonography. These developmental variations are discussed in detail in the pediatric chapter. A detailed examination can reveal the endometrium in each horn, identify pathology, or document pregnancy ( Fig. 43.11 ).
Leiomyomas , commonly called myomas, are the most common gynecologic tumors, occurring in approximately 20% to 30% (or greater depending on the reference source) of women over 30 years old. They are more common in African American women.
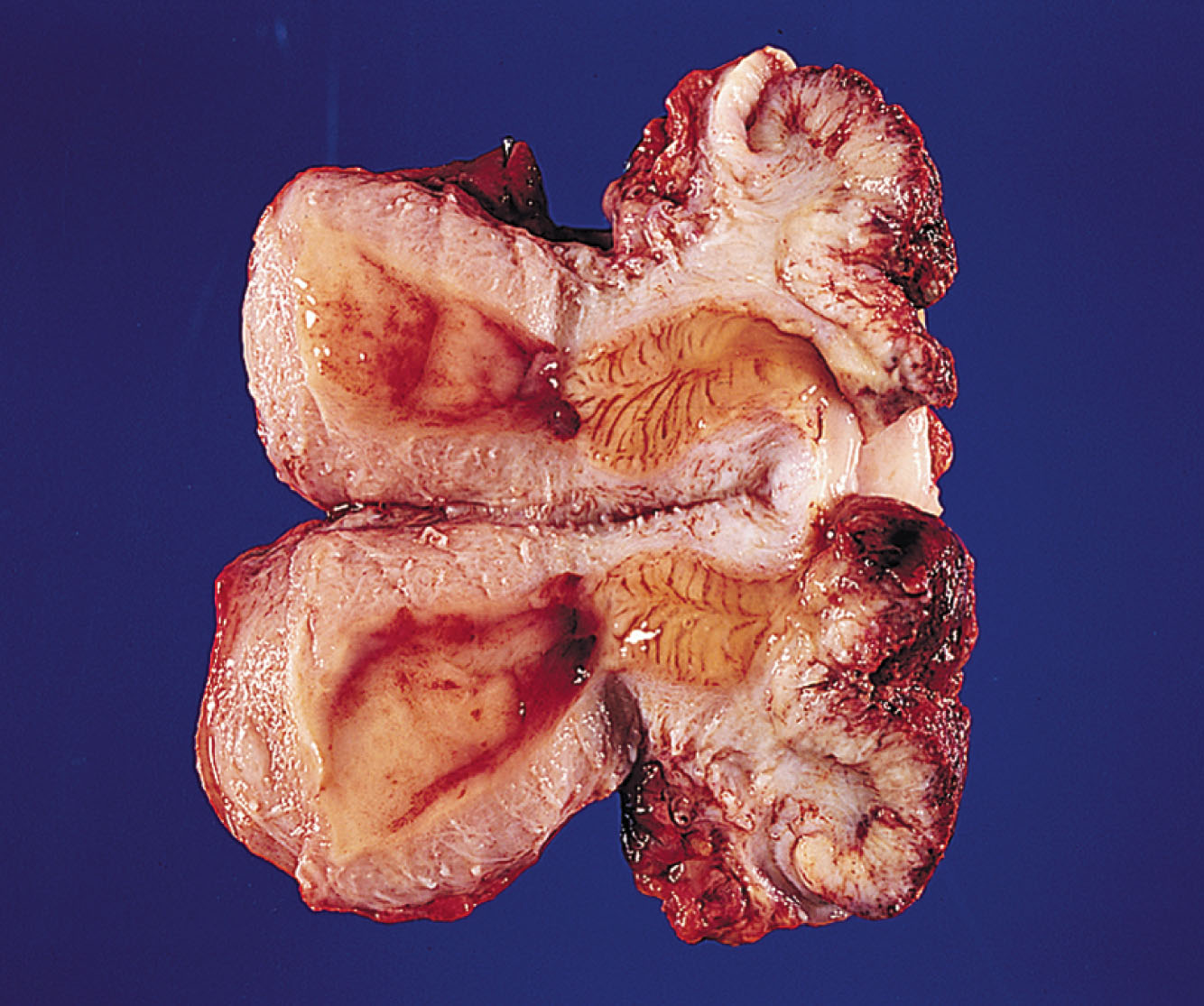
Myoma tumors are composed of spindle-shaped, smooth muscle cells arranged in a whorl-like pattern with variable amounts of fibrous connective tissue, which can degenerate into a number of different histologic subtypes ( Fig. 43.12 ). The tumors consist of nodules of myometrial tissue and are usually multiple. The myoma is encapsulated with a pseudocapsule and separates easily from the surrounding myometrium. With atrophy and vascular compromise as a result of outgrowing their blood supply, fibrotic changes and degeneration of the myomas can occur. Liquefaction, necrosis, hemorrhage, and ultimate calcification may take place. Hyalinization (development of an albuminoid mass in a cell or tissue) occurs most often, making the myomas appear more lucent or hypoechoic than the myometrium. Ten percent of myomas contain calcification, and a similar number have areas of hemorrhage. Other myomas contain tissue that has undergone necrosis and liquefaction and become myxoid in texture.

Myomas are estrogen dependent and may increase in size during pregnancy, although about half of all myomas show little change during pregnancy. Myomas identified in the first trimester are associated with an elevated risk of pregnancy loss, and this risk is higher in patients with multiple myomas. They rarely develop in postmenopausal women, and most stabilize or decrease in size following menopause because of a lack of estrogen stimulation. They may increase in size in postmenopausal patients who are undergoing hormone replacement therapy. Tamoxifen has also been reported to cause growth in leiomyomas. A rapid increase in myoma size, especially in a postmenopausal patient, should raise the level of concern for a neoplasm.
Clinically, myomas cause uterine irregularity and enlargement with the sensation of pelvic pressure and sometimes pain. Patterns of irregular bleeding, menometrorrhagia, or heavy menstrual bleeding (menorrhagia) are the primary clinical problems. Myomas may contribute to infertility by distorting the fallopian tube or endometrial cavity; if located in the lower uterine segment or cervix, the tumor may interfere with normal vaginal delivery. Because of the increased estrogen during pregnancy, the tumor may grow and bleed within, causing pain. Box 43.4 summarizes the characteristics of leiomyomas.
Most common pelvic tumor
Smooth muscle cell composition
Fibrosis occurs after atrophic or degenerative changes
Degeneration occurs when myomas outgrow their blood supply; calcification
May be pedunculated
Clinical findings: enlarged uterus, profuse and prolonged bleeding, pain
Leiomyomas can affect any portion of the uterine wall; however, the tumor may also be uncommonly found in the lower uterine segment, the cervix, and in the broad ligament. Leiomyomas are either submucosal leiomyomas (displacing or distorting the endometrial cavity with subsequent irregular or heavy menstrual bleeding), intramural leiomyomas (confined to the myometrium, the most common type), or subserosal leiomyomas (projecting from the peritoneal surface of the uterus). Sometimes, subserosal leiomyomas become pedunculated and appear as extrauterine masses ( Box 43.5 ).
The signs and symptoms of leiomyomas depend on their size and location ( Fig. 43.13 ). Submucosal myomas may erode into the endometrial cavity and cause irregular or heavy bleeding, which may lead to anemia. Fertility may be affected by submucosal or intramural myomas, which may impede sperm flow, prevent adequate implantation, or cause recurrent miscarriages. It is particularly important to diagnose submucosal leiomyomas because they are a well-established cause of dysfunctional uterine bleeding, infertility, and spontaneous abortion. Small submucosal leiomyomas may be removed hysteroscopically.
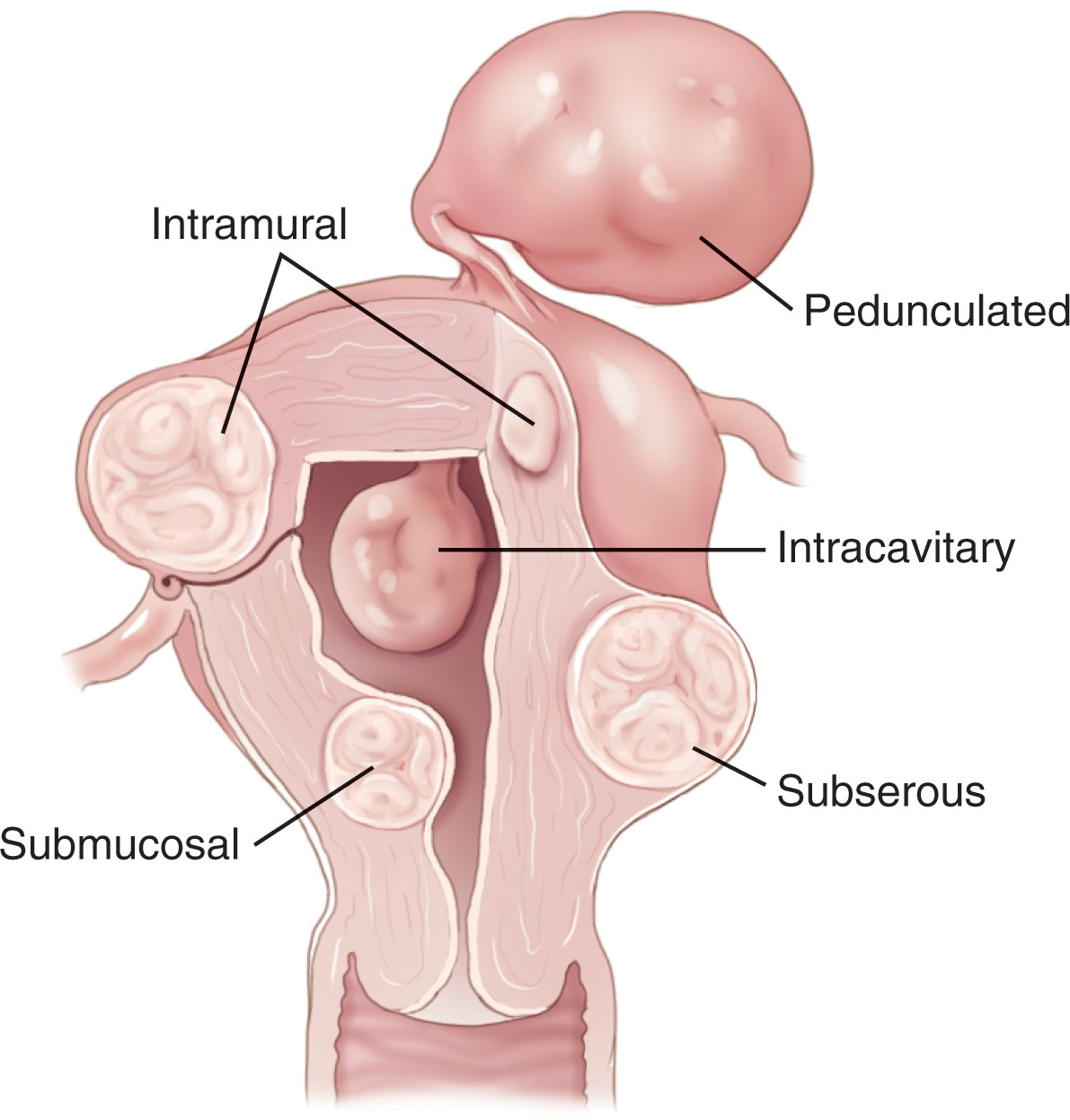
Uncommonly, a pedunculated subserosal lesion develops a long stalk and is migratory; it can implant into the blood supply of the broad ligament, omentum, or the bowel mesentery. Transvaginal sonography is often helpful in showing the uterine origin of the mass and identifying the stalk. Occasionally, a pedunculated myoma becomes adherent to surrounding structures and develops an auxiliary blood supply.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here