Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
5-fluorouracil angiotensin-converting enzyme inhibitors Crohn’s disease cytomegalovirus cyclooxygenase anticytotoxic T-lymphocyte-association protein-4 gastrointestinal inflammatory bowel disease immune checkpoint inhibitors mycophenolate mofetil nonsteroidal antiinflammatory drugs olmesartan-associated enteropathy programmed cell death protein-1 pancreatic enzyme replacement therapy sodium polystyrene sulfonate 5-FU
ACEIs
CD
CMV
COX
CTLA-4
GI
IBD
ICIs
MMF
NSAIDs
OAE
PD-1
PERT
SPS
Many conditions may share the clinical and endoscopic features of inflammatory bowel disease (IBD), and it is, therefore, essential to make differential differentiate and initiate the appropriate management plan. An important condition to recognize is drug-induced enteropathy as it is ubiquitous. A multitude of medications have been associated with the development of gastrointestinal (GI) lesions with ulcerative or nonulcerative inflammation and strictures, nonsteroidal antiinflammatory drugs (NSAIDs) being the most common ones. Indeed, more than 700 medications are found to be associated with enterocolitis . Clinical manifestations of drug-induced enteropathy or colopathy resemble those of IBD and may include nausea, vomiting, abdominal pain, diarrhea, or rectal bleeding.
Drug-induced GI injury may occur through topical or systemic mechanisms. Physiologically or pathologically narrowed lumens of the GI tract, particularly the esophagus pylorus, and terminal ileum, are at risk. Commonly reported agents causing esophageal injury include NSAIDs, tetracycline, emepronium, potassium chloride, and quinidine sulfate . In addition to causing mucosal damage through a variety of pathways, drugs may also lead to vascular and ischemic complications, impact microbiota, or disrupt mechanisms regulating electrolyte and fluid balance .
Drug-induced GI complications not only include mucosal injury, inflammation, strictures, or perforation but can also lead to other disease entities such as microscopic colitis (further discussed in Chapter 26 : Inflammatory bowel disease–like conditions: other immune-mediated gastrointestinal disorders) or exacerbation of underlying IBD. A classic example is the use of NSAIDs. It is also important to note that medications may induce other conditions mimicking IBD through complications from their underlying mechanism of action. This is, for example, the case with antibiotics allowing Clostridium difficile infection, or immunosuppressants leading to infectious enterocolitis from cytomegalovirus (CMV) .
Drug-induced enteropathy remains a diagnosis of exclusion, and care has to be taken to rule out any other contributing conditions. Conditions that mimic IBD are extensively described in this book, such as immune-mediated conditions, immune deficiency–associated GI disorders, malignancies, infectious etiologies (such as tuberculosis), or radiation-induced GI injury. They may share common clinical, endoscopic, histologic, and imaging features. This chapter is to describe common drug-induced GI complications for their clinical, endoscopic, and histologic features as well as a brief guide to management.
NSAIDs are widely used in the management of pain and inflammatory conditions. These molecules work by inhibiting cyclooxygenase (COX) activity with subsequent downstream effects. Through inhibiting COX activity, NSAIDs inhibit the production of prostaglandins, which play an important role in mucosal healing and repair .
NSAIDs have been associated with a variety of GI lesions. Although peptic ulcer disease is the most widely described complication initially, the advent of small bowel imaging and endoscopy i.e.balloon-assisted enteroscopy and video capsule endoscopy has demonstrated that small bowel lesions are frequently found in patients on NSAID therapy .
NSAIDs inhibit the two isoforms of the COX enzyme, namely, COX-1 and COX-2 . Selective COX-2 inhibitors have been developed in the hope of reduced GI damage. Although this category of medications have similar therapeutic effects to nonselective NSAIDs, they initially did appear to lead to less GI injury . However, recent data have shown COX-2 inhibitors to be associated with GI lesions similarly to nonselective NSAIDs .
NSAID-induced GI lesions are common. In a prospective cohort, small bowel mucosal breaks were found in 55% of patients receiving naproxen along with a proton-pump inhibitor for 2 weeks . NSAIDs may cause a variety of GI complications ranging from erosions, ulcers, strictures, friability, or perforation, which may manifest by different clinical presentations.
Risk factors for NSAID-induced gastroduodenal injury include history of peptic ulcer disease, advanced age, combination of NSAIDs and corticosteroids or anticoagulants, comorbidities, and Helicobacter pylori infection . Risk factors for NSAID-related small bowel injury are different and include the use of “oxicam” type of NSAIDs (such as meloxicam), diclofenac, the presence of comorbidities, and the combination of NSAIDs and aspirin . In a retrospective study assessing NSAID-related small bowel lesions with video capsule endoscopy, most lesions were found in the jejunum (52.8%), followed by the ileum (27.9%) . In a retrospective analysis of NSAID-associated GI injury, most patients had ulcers in the ileocecal location. The ulcers were semicircumferential or circumferential with sharp demarcation .
In addition to causing inflammation in the GI tract, the use of NSAIDs contributes to worsening or exacerbation of underlying Crohn’s disease (CD), ulcerative colitis , or pouchitis . Commonly over-the-counter or prescribed NSAIDs are used to treat IBD-associated arthralgia or arthropathy. The use of NSAIDs can also cause microscopic colitis or diverticular complications such as perforation and fistula . Furthermore, chronic use of NSAIDs can lead to diaphragm disease in the lumen of GI tract with formation of short intestinal strictures. These strictures occur most commonly in the small bowel and right colon. Patients with diaphragm disease frequently present with GI bleeding or obstructive symptoms, anywhere from 2 months to more than 20 years into NSAID therapy .
The clinical presentation of NSAID-induced GI lesions varies according to disease type and location. NSAID-induced lesions may be asymptomatic or present as iron deficiency anemia or hypoalbuminemia . Obscure or overt GI bleeding is common presentation . Other clinical manifestations include abdominal pain, diarrhea, nausea, and vomiting. Obstructive symptoms may also occur . Symptoms may arise anytime while on NSAIDs but tend to occur in a median time of 3 months after the start of therapy .
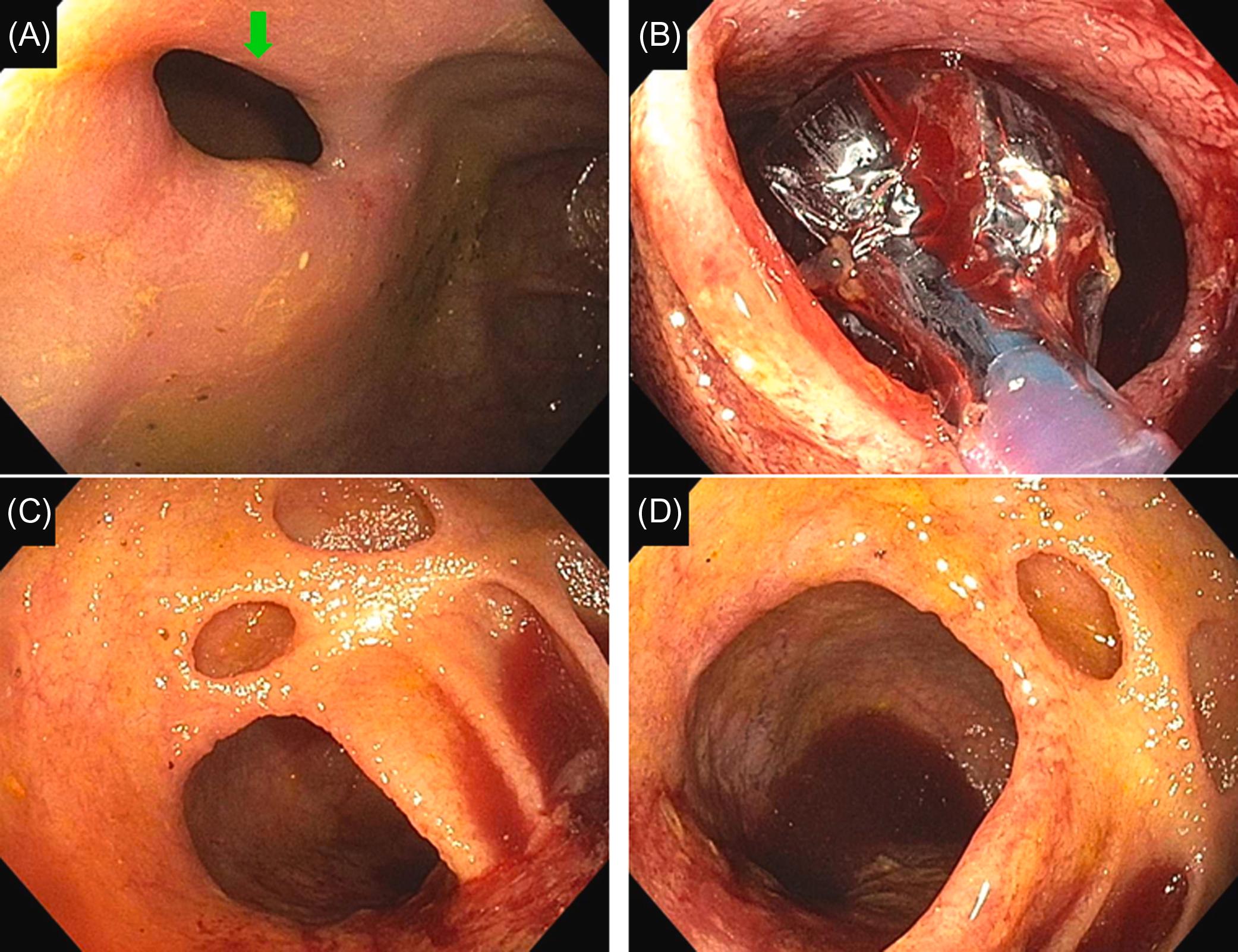
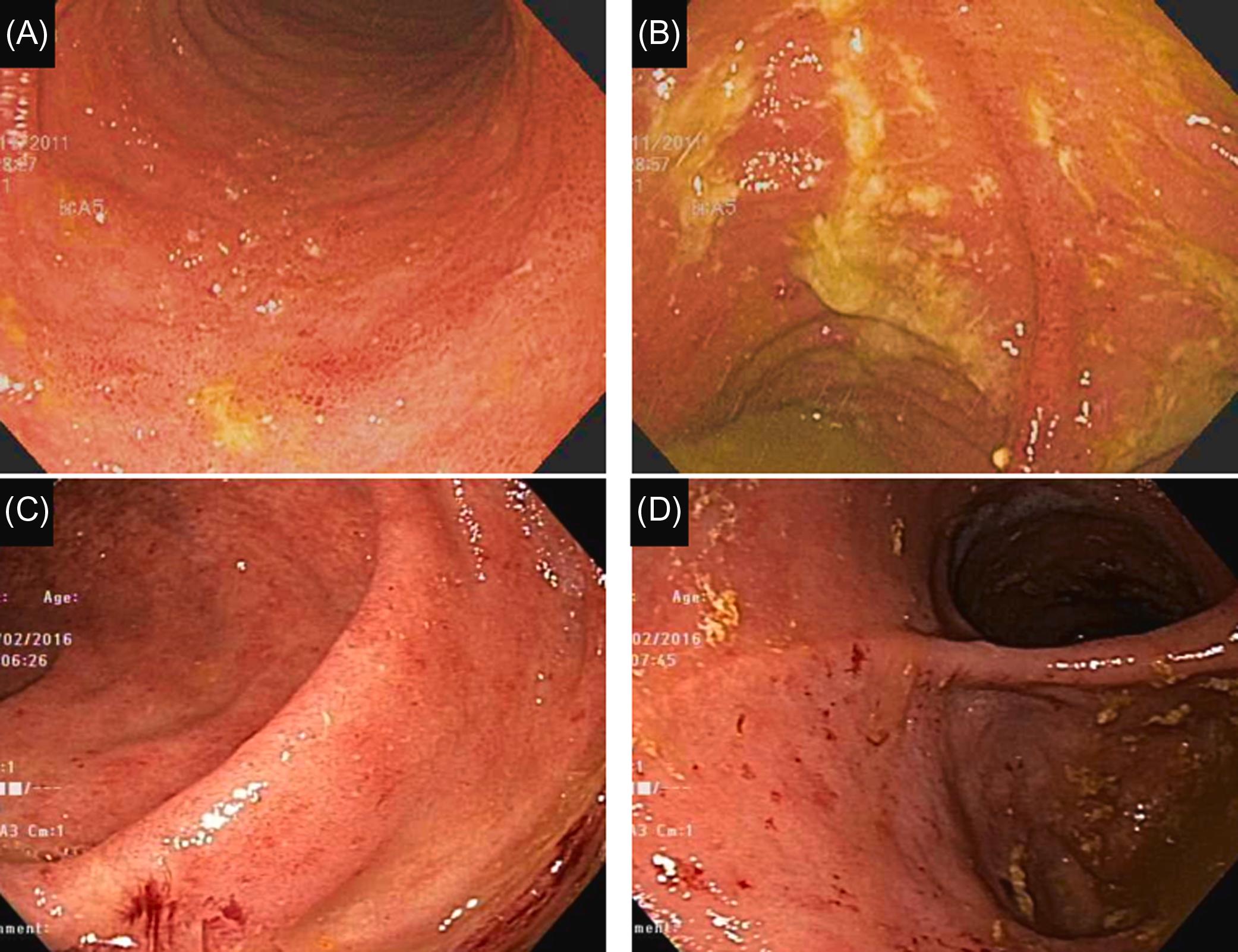
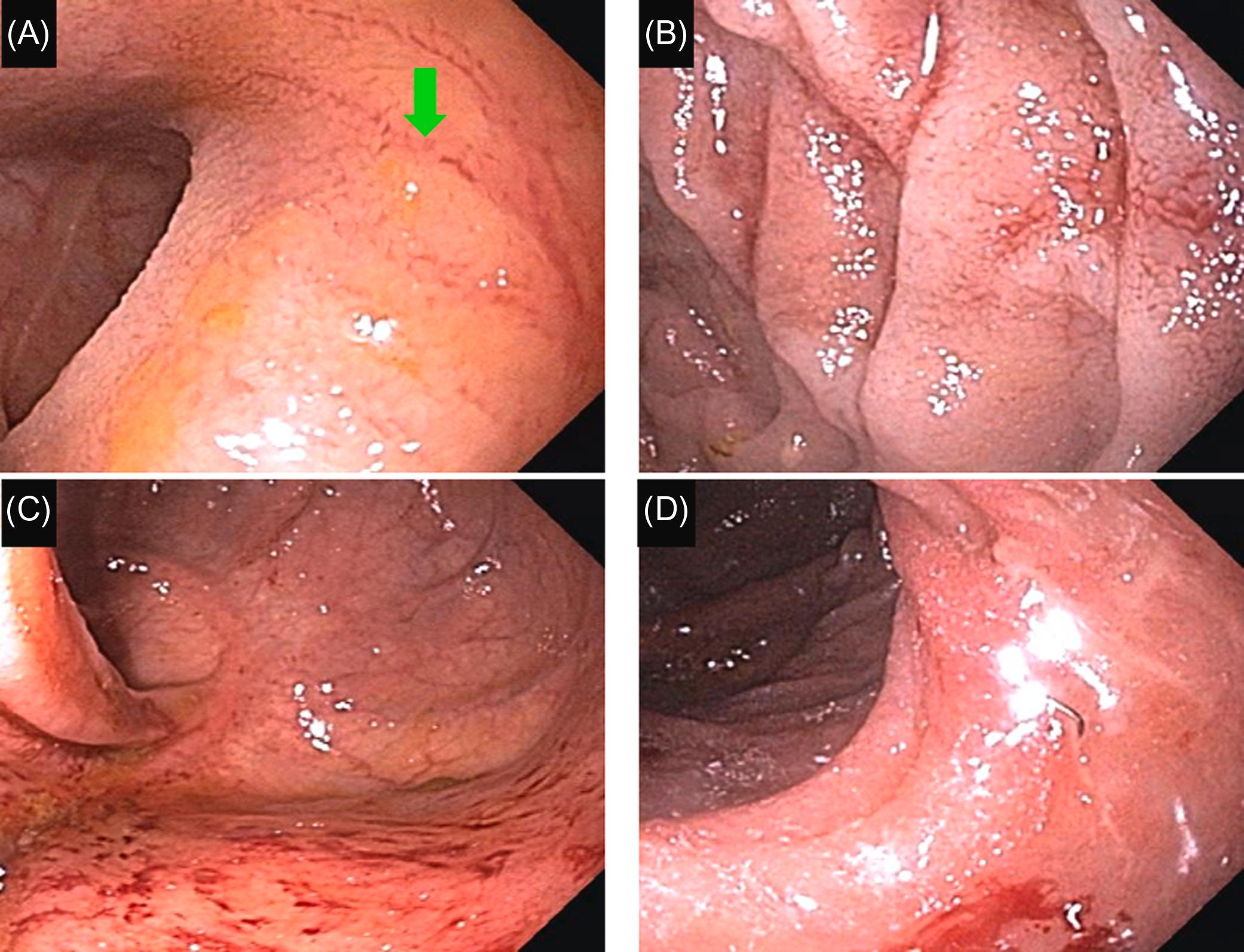
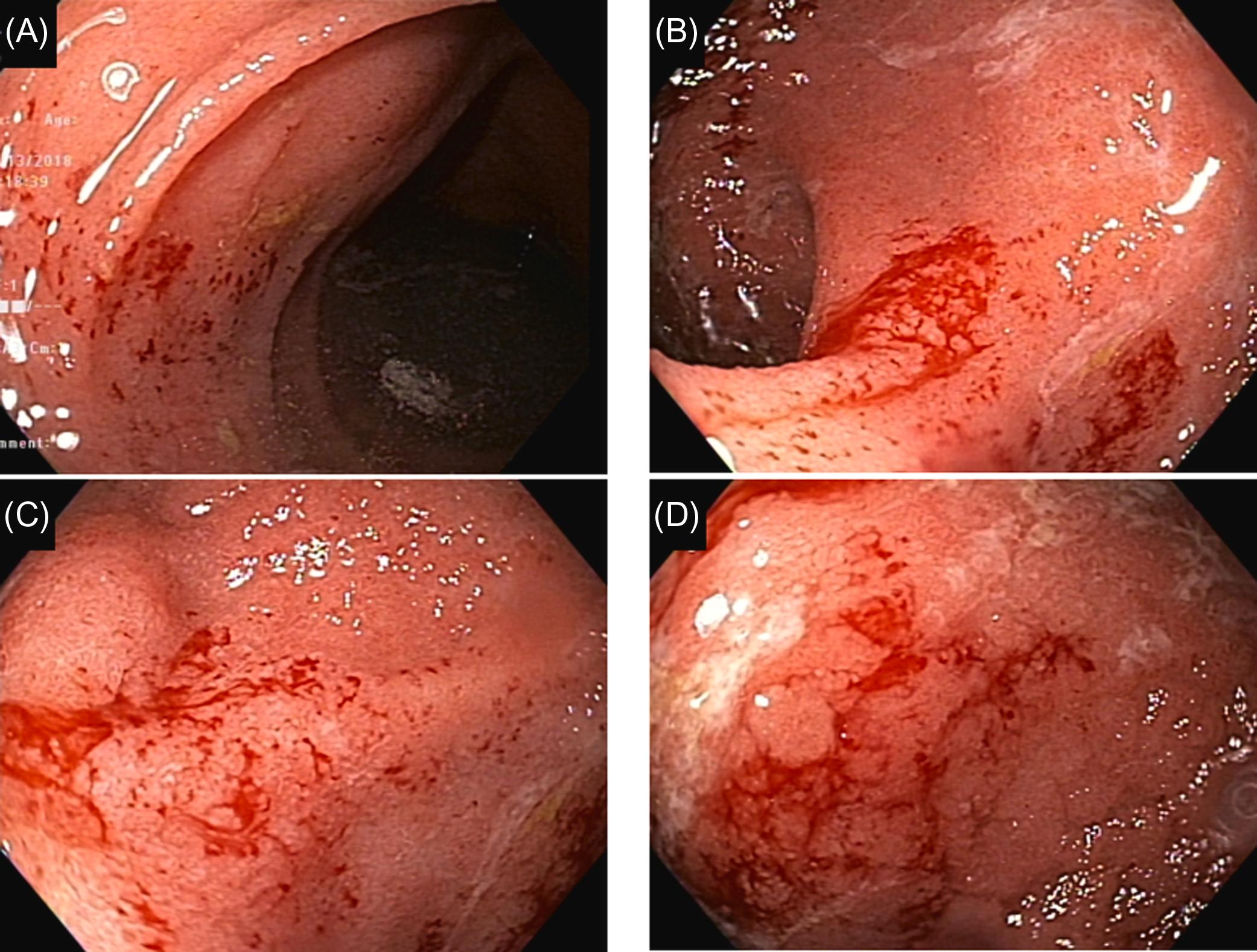
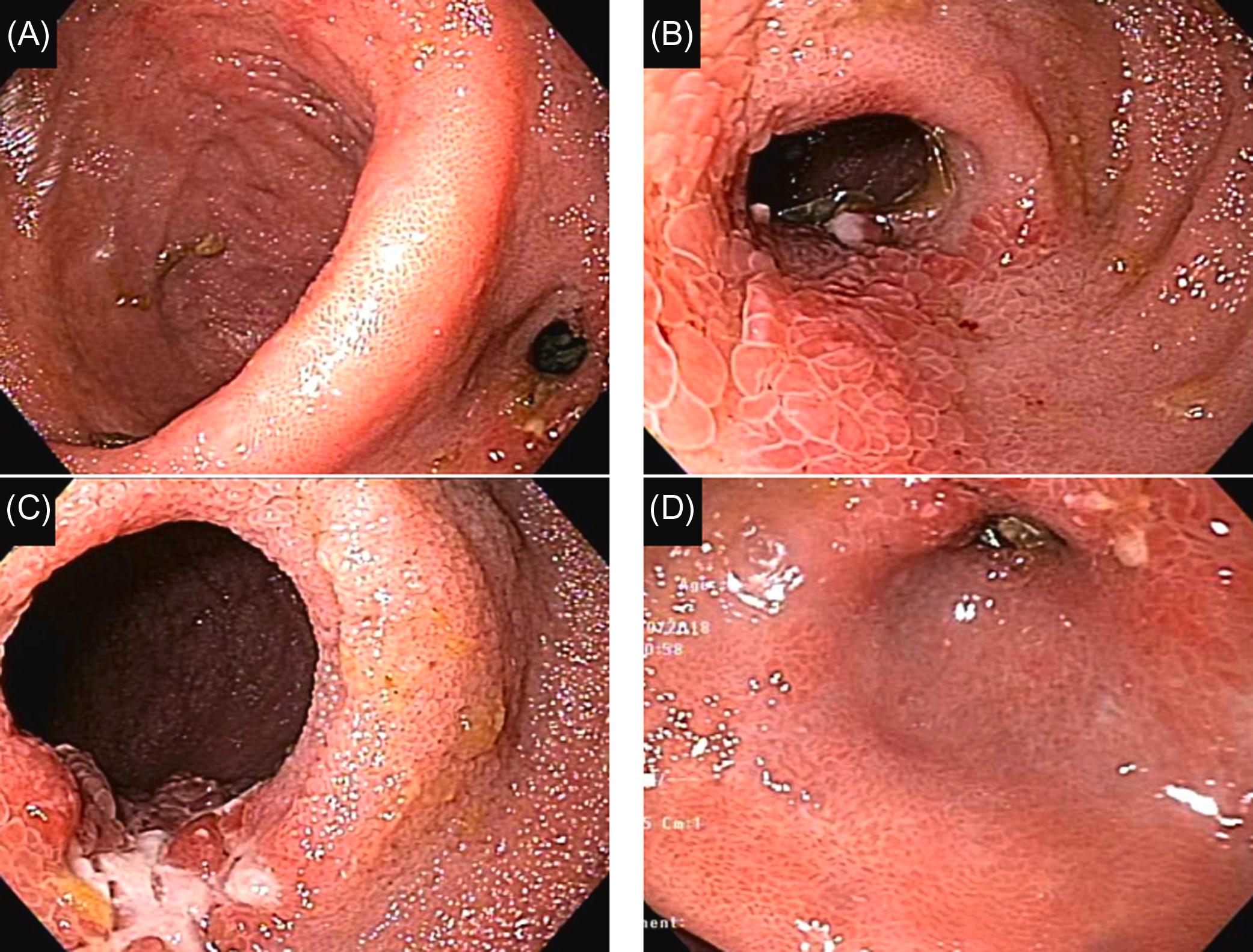
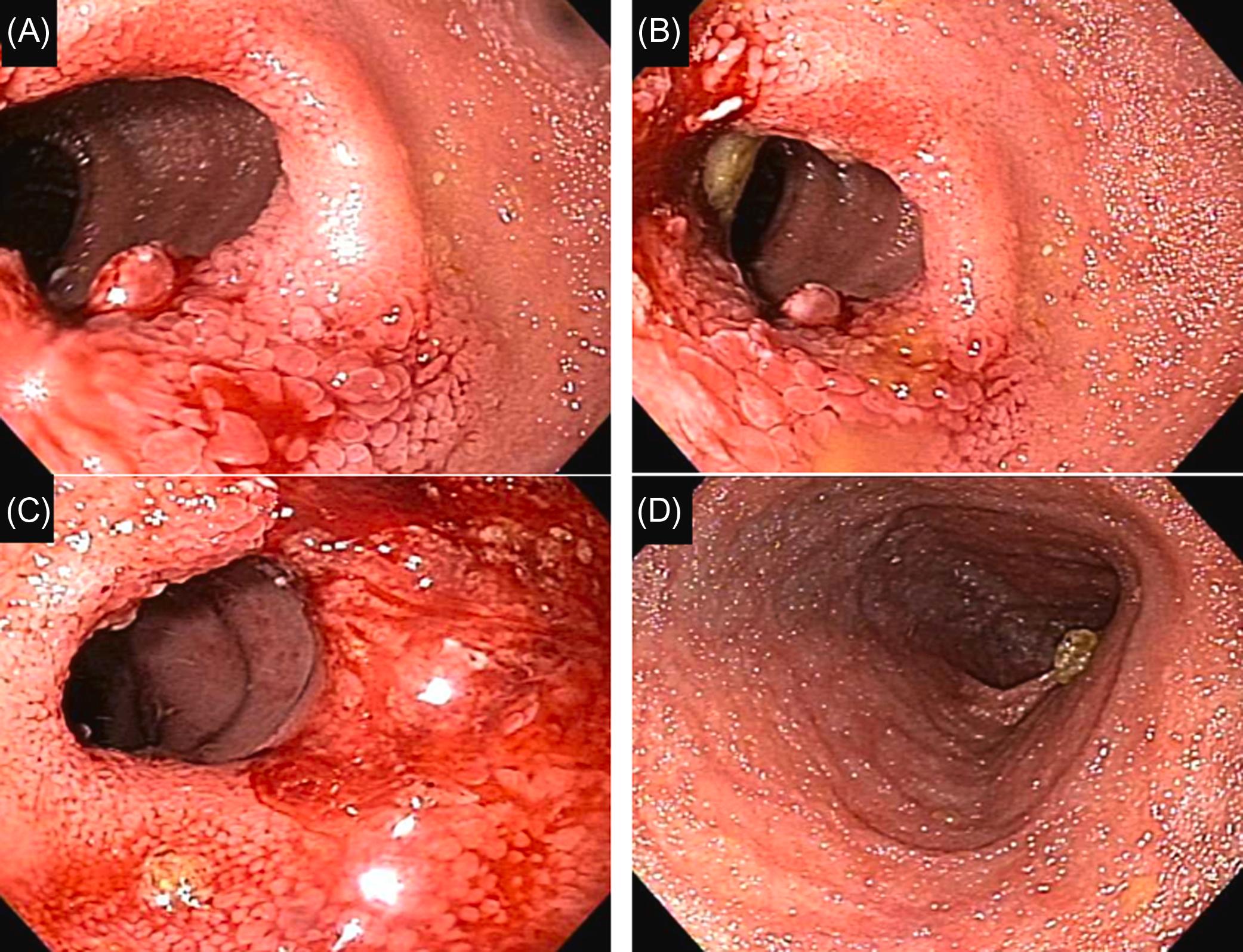
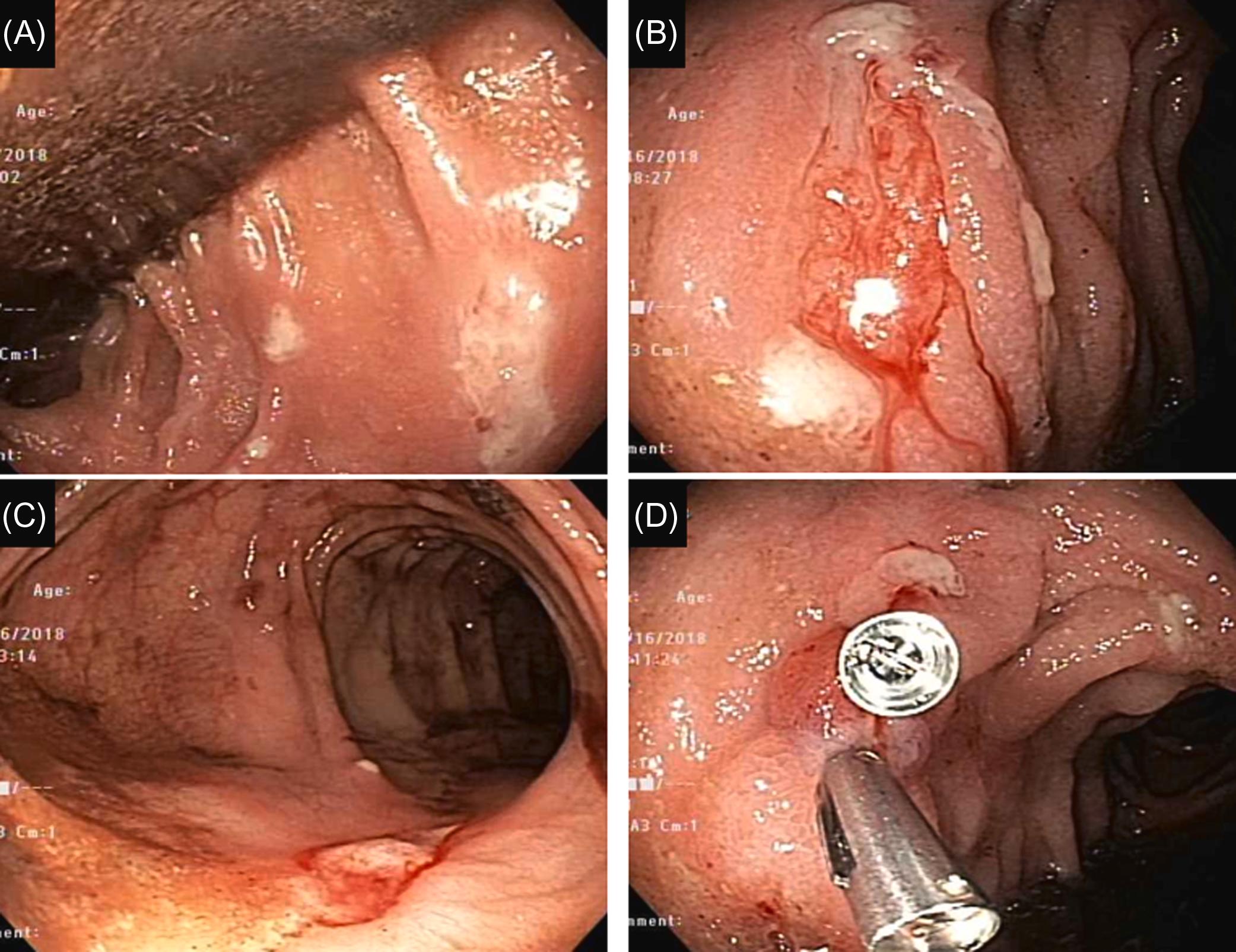
Endoscopic features vary, depending on the location of GI jury, duration and dosage of NSAIDs, concurrent use of ulcer-prone medications, and comorbidities. Differential diagnosis should be made between NSAID-induced GI tract injury, IBD, and NSAID-associated IBD flare-up. Although commonly seen in the stomach and duodenum, the endoscopic lesions are also found in the esophagus, small bowel, and colon . Petechiae, erythema, erosions, and ulcerations are common. Erosions and ulcers can be small or large, and round, linear or irregular ( Figs. 29.1–29.8A and B ) . Active ulcer bleeding may be seen, as well as perforation . Other endoscopic features include mucosal scars ( Fig. 29.8C ), strictures ( Figs. 29.8D–29.10A and B ), diverticuli ( Fig. 29.10C and D ), and diaphragms ( Fig. 29.11 ). The latter is characterized by the presence of thin membranous strictures in the small bowel and colon .
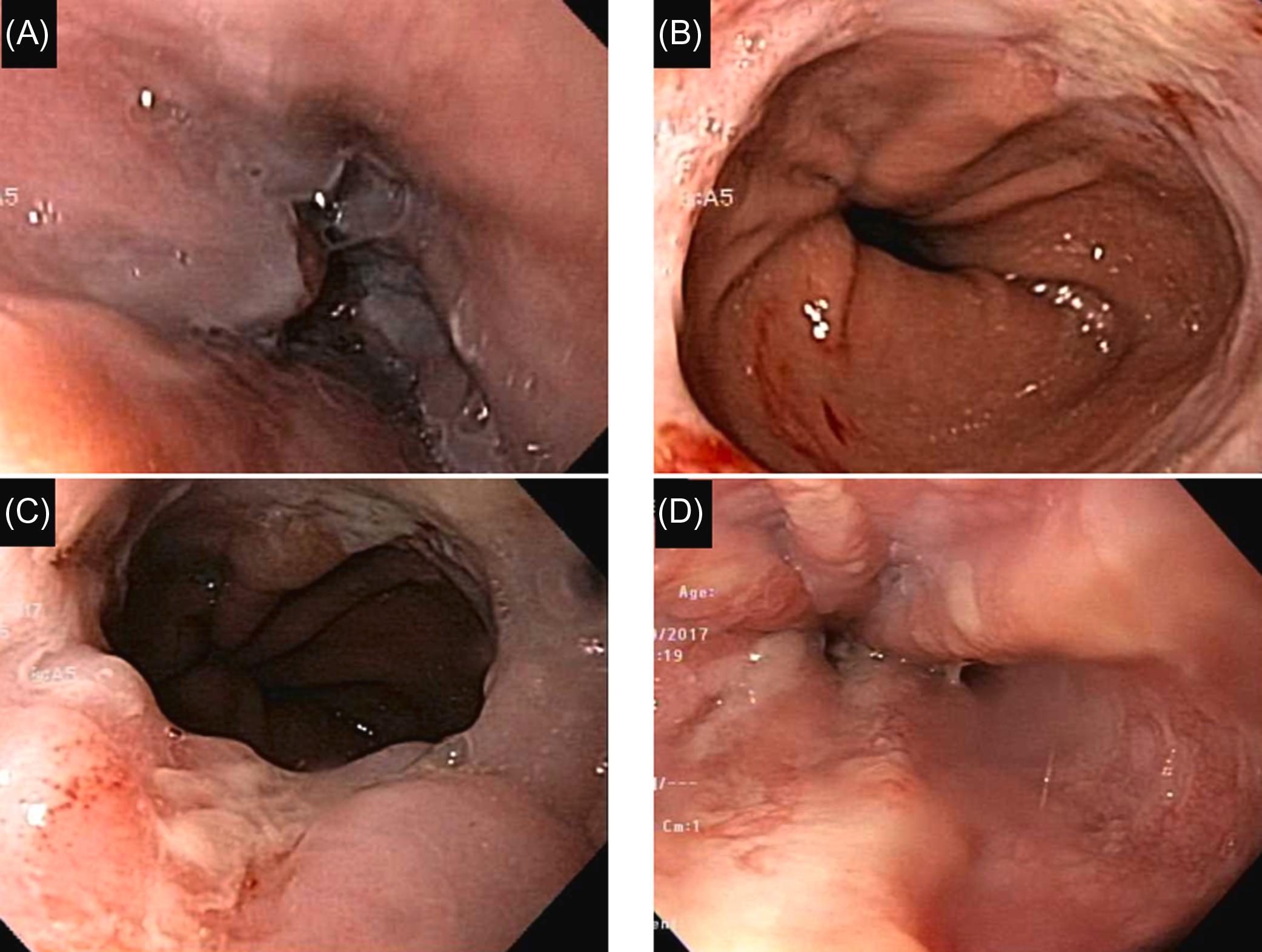
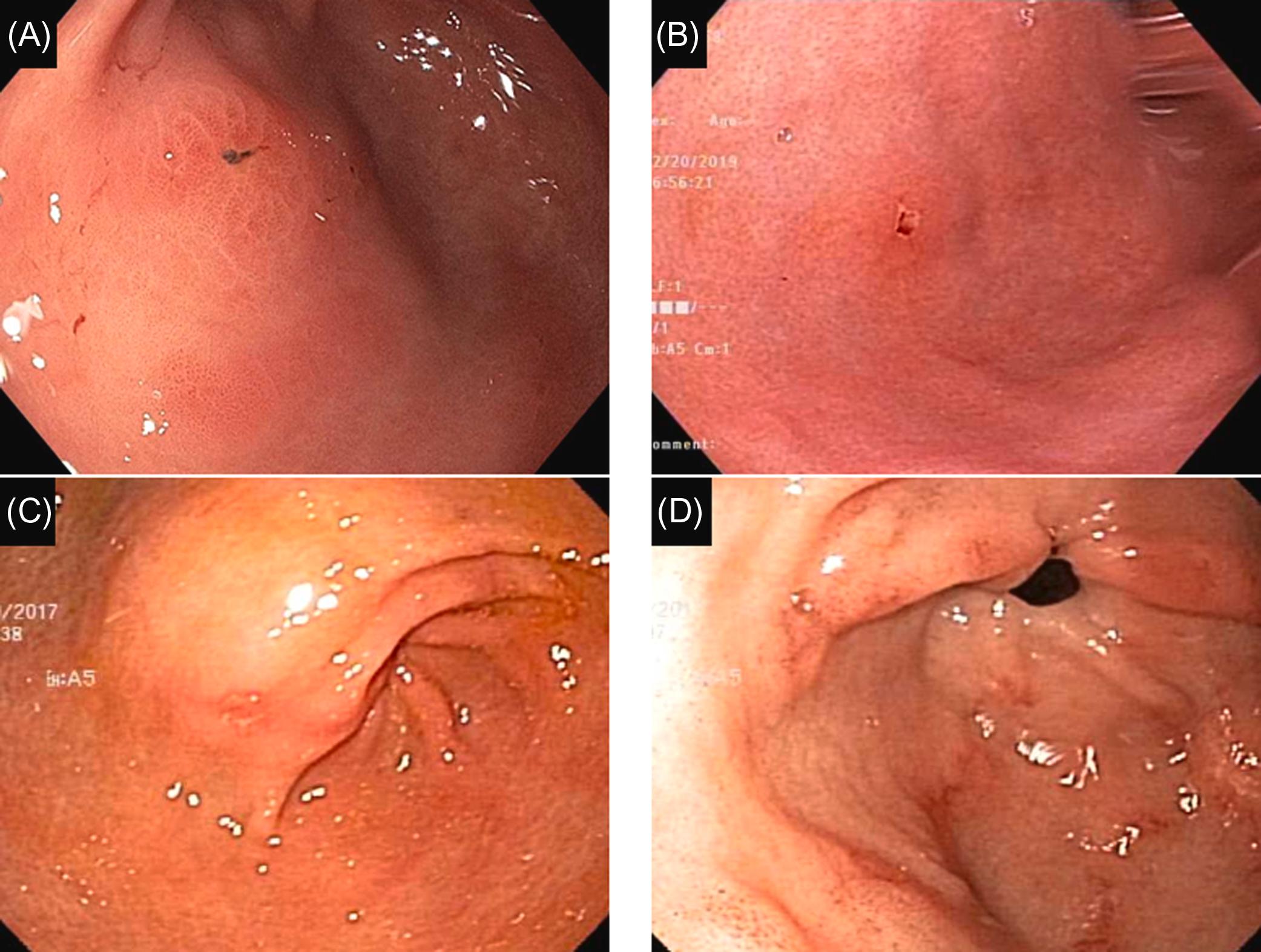
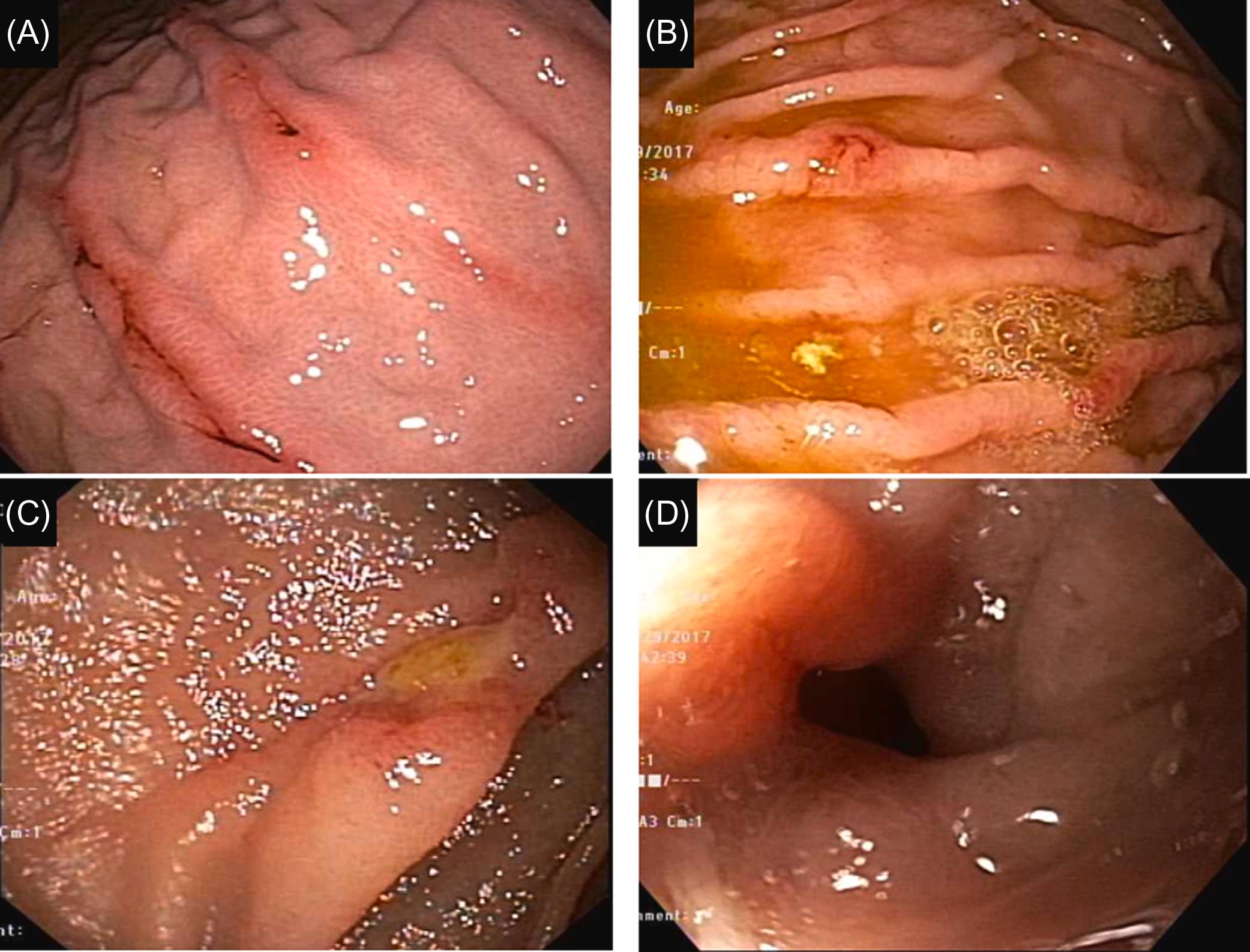
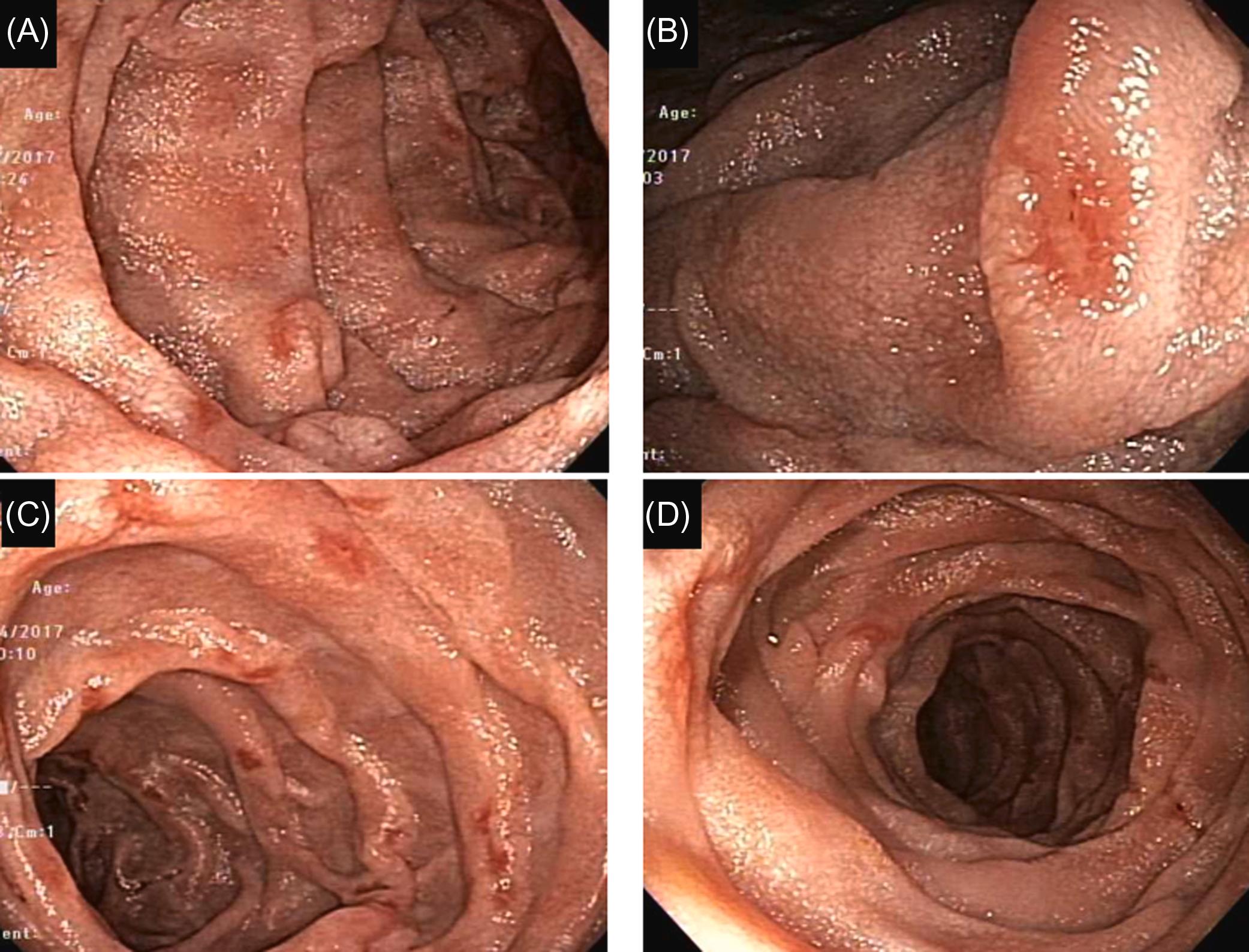
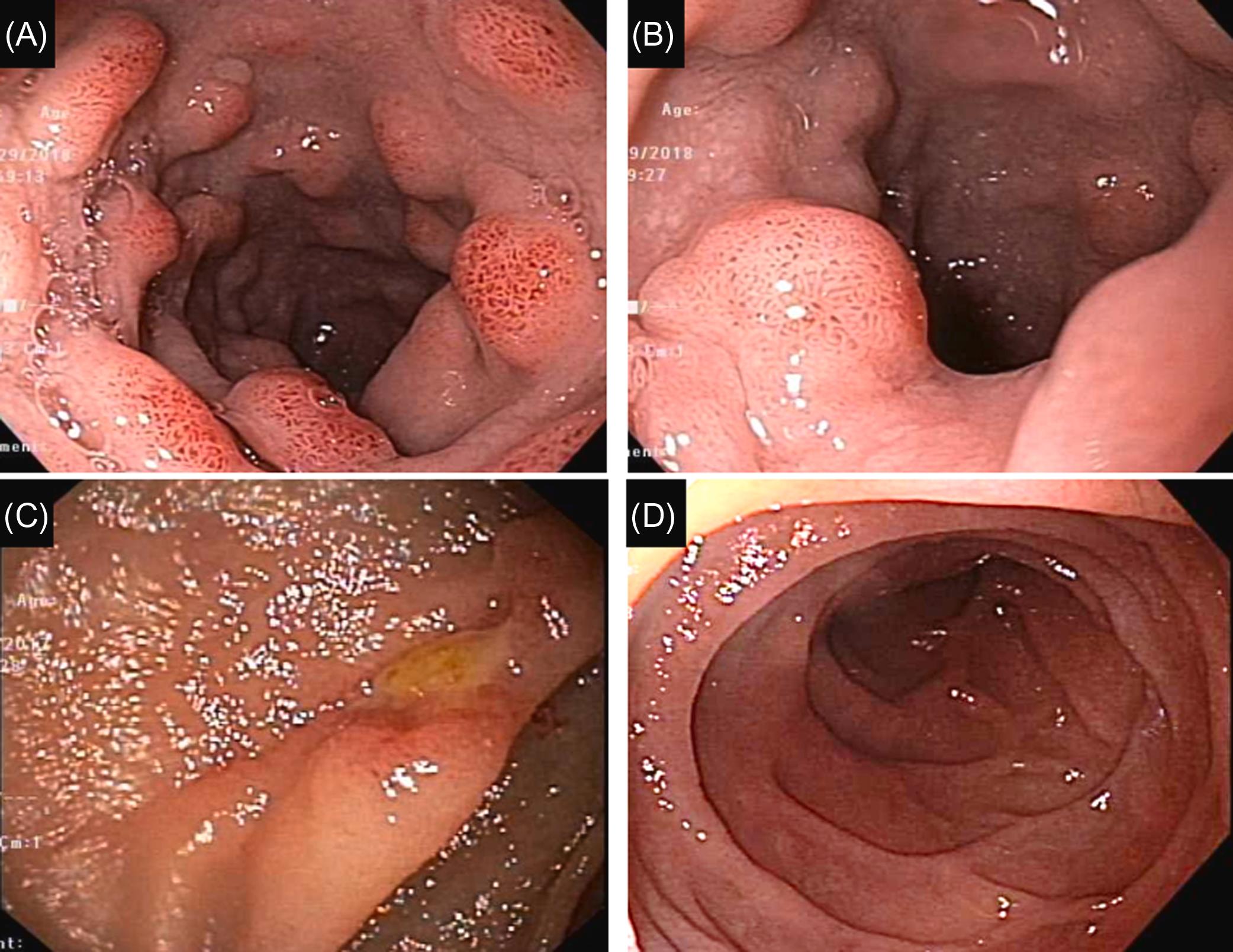
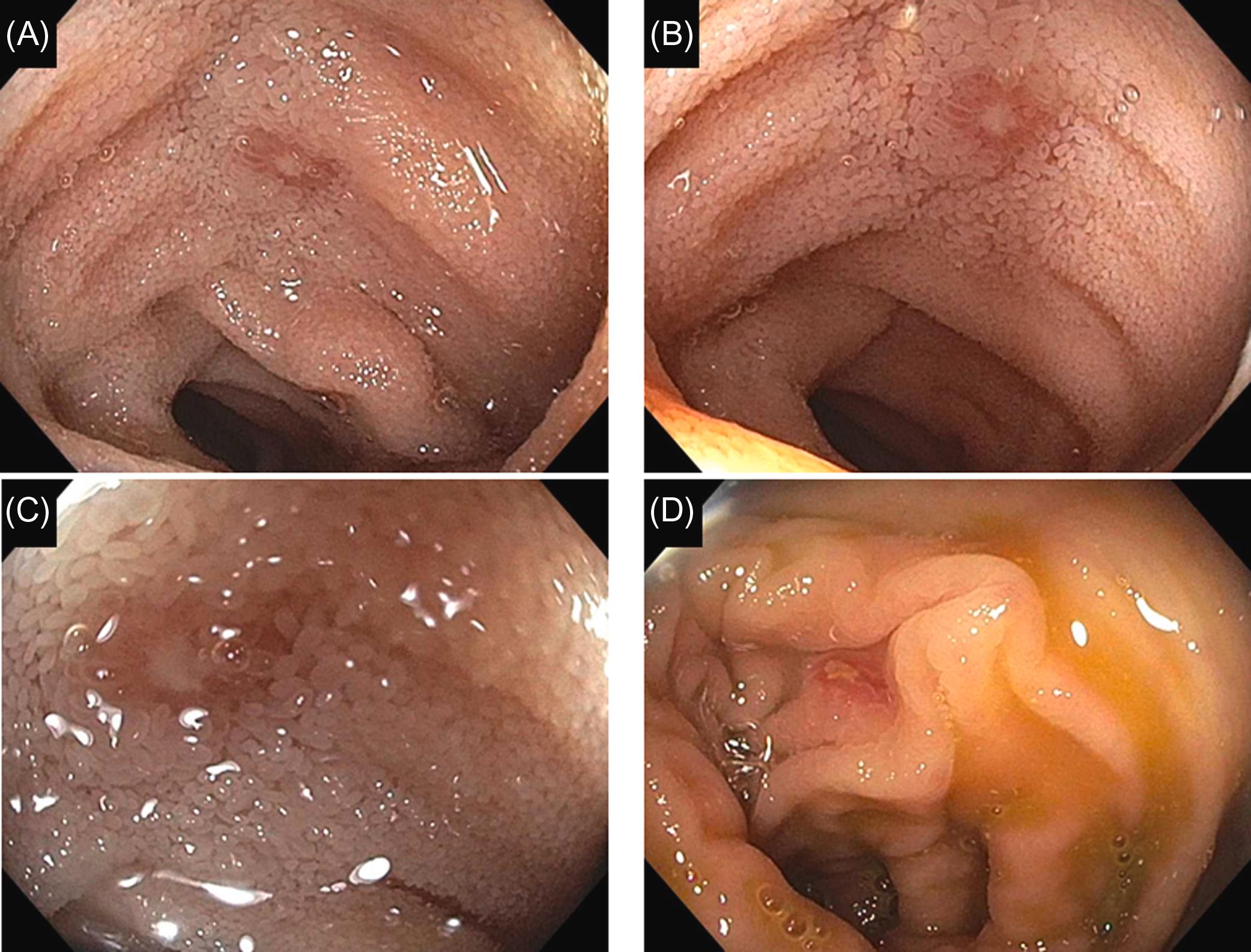
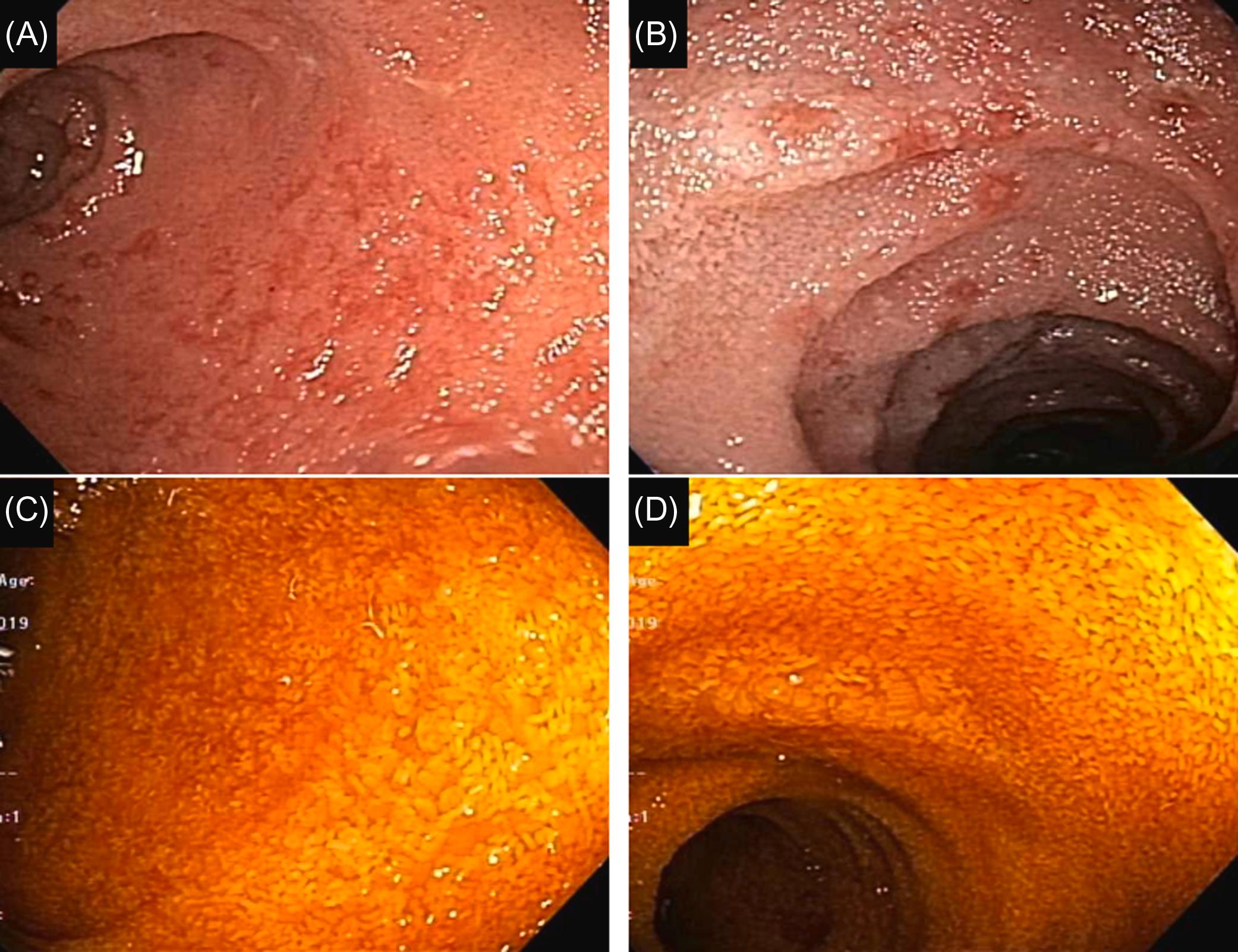
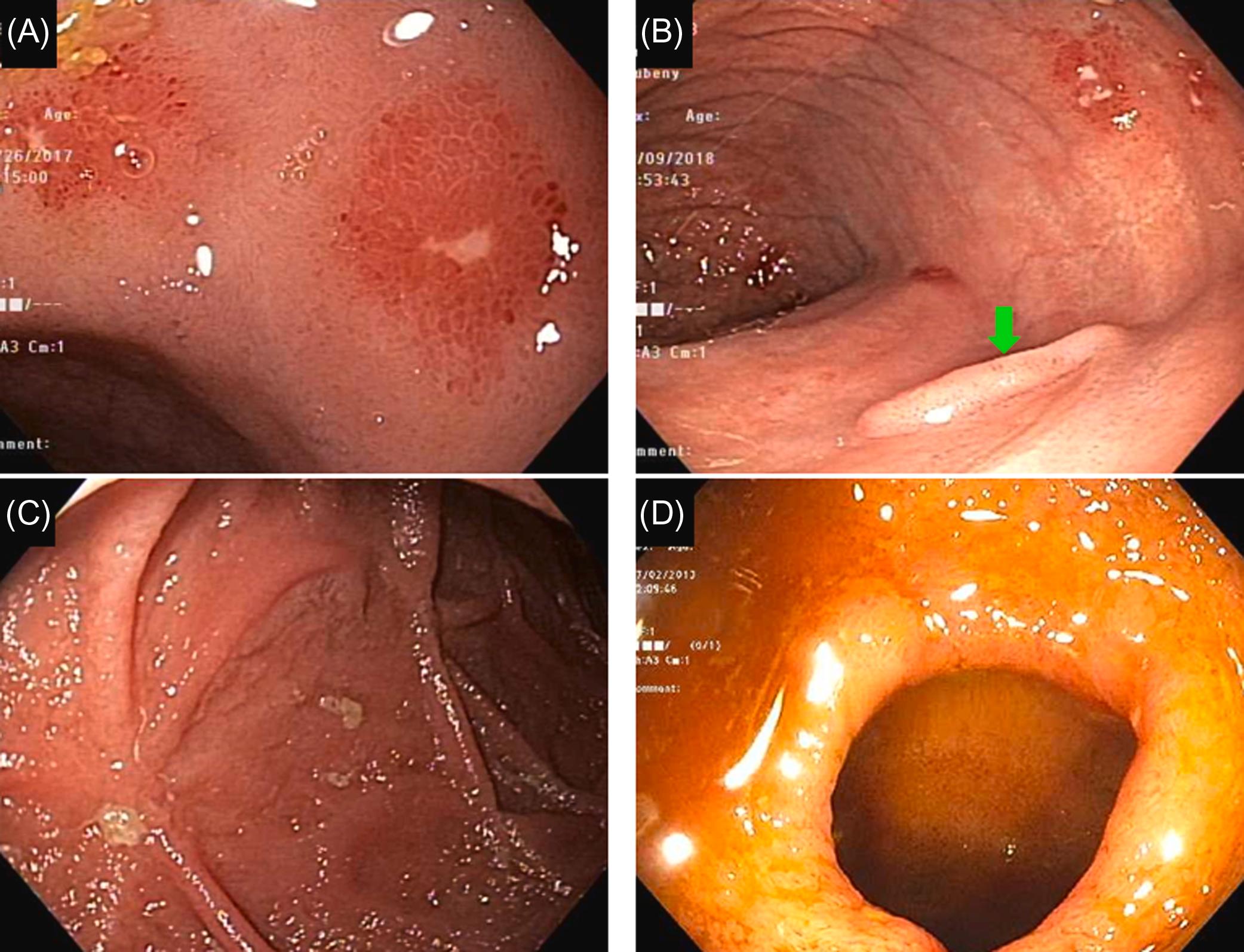
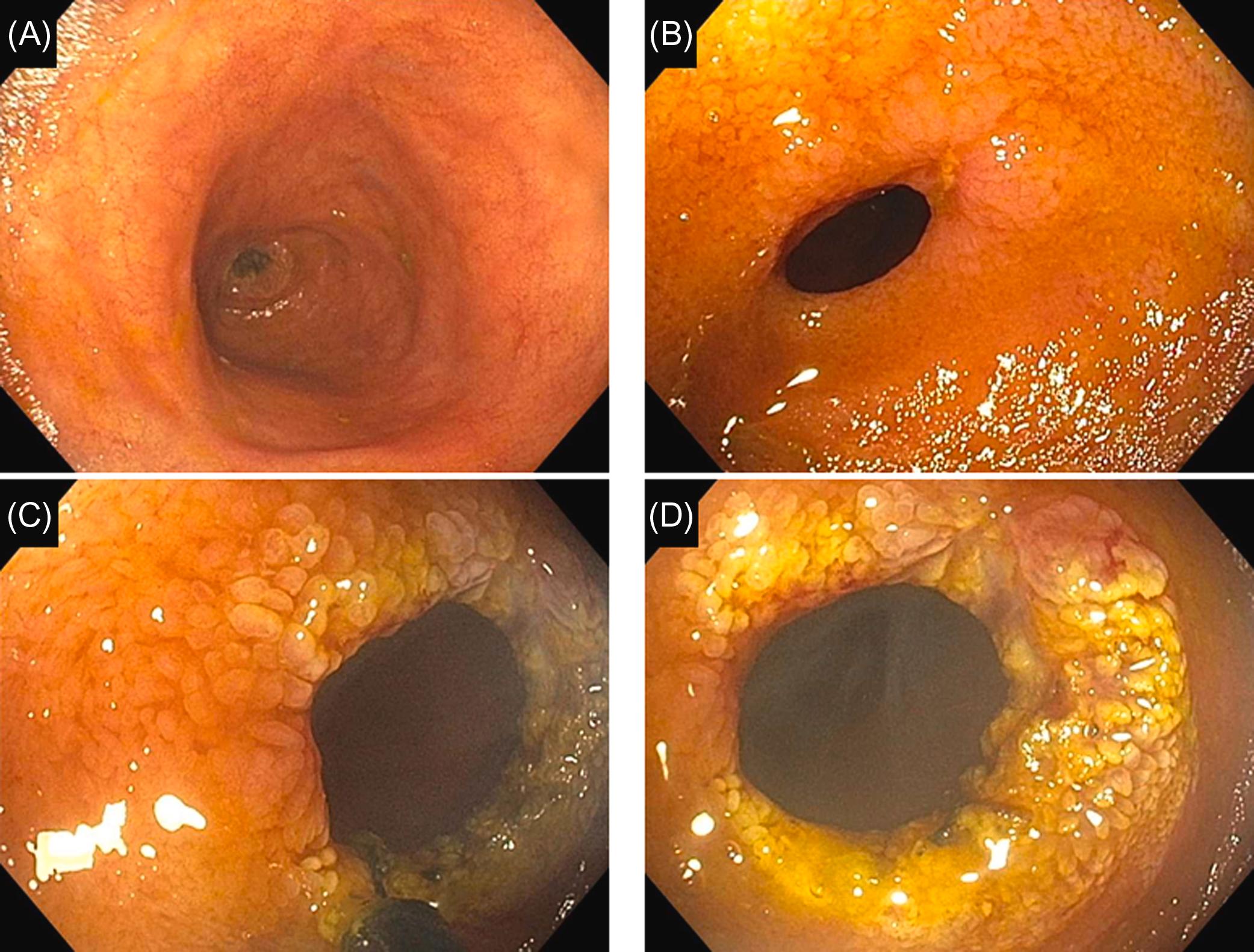
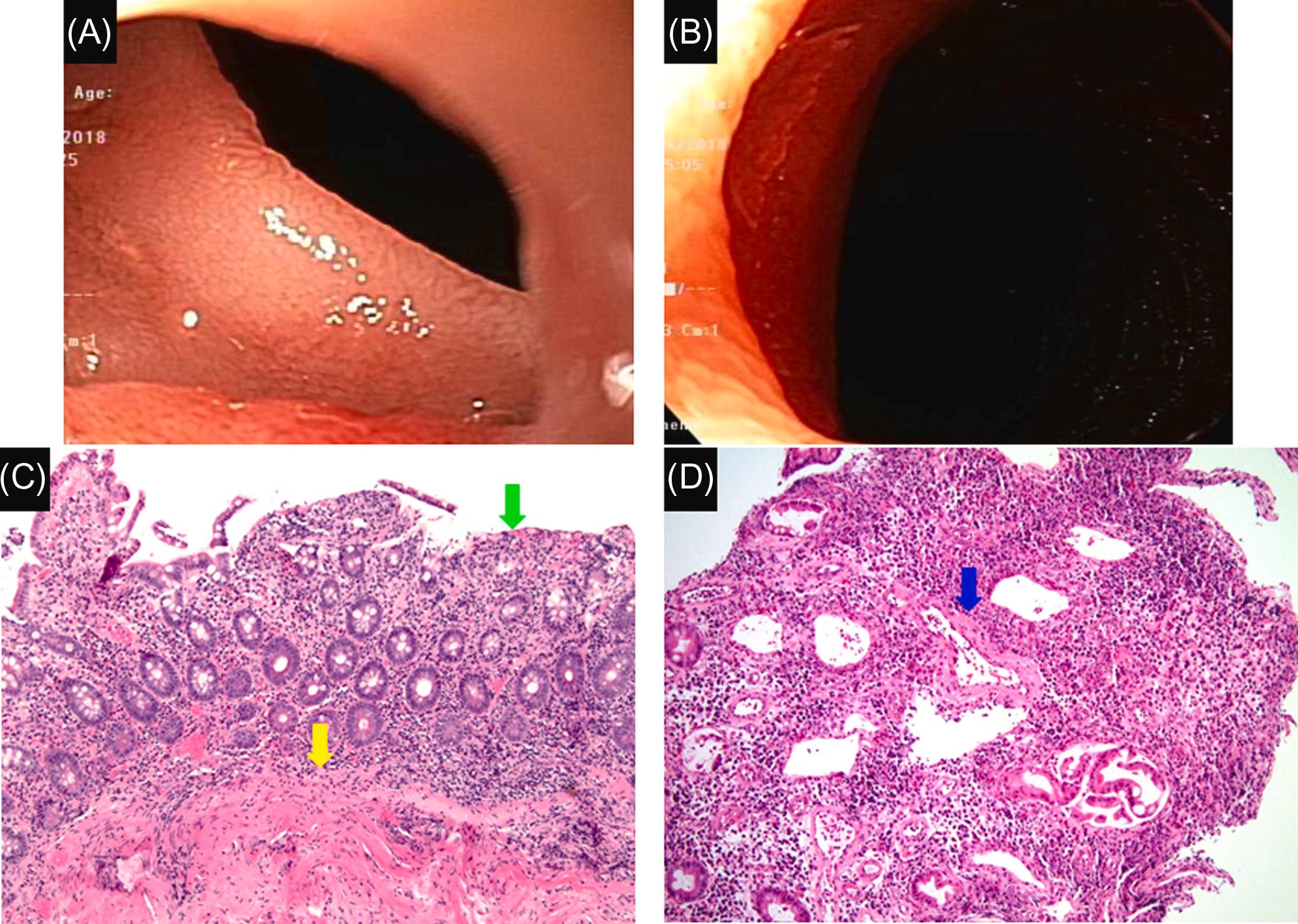
NSAIDs have also been associated with nonulcerative inflammation, ulcers, friability, spontaneous bleeding, and strictures in the afferent limb, pouch body, or cuff in patients with restorative proctocolectomy and ileal pouch-anal anastomosis ( Figs. 29.12–29.17 ). The afferent limb ulcers and strictures may thereby mimic CD . Histologic features of NSAID-induced enteritis include reactive epithelial changes, subepithelial fibrosis, crypt apoptosis, cytolysis, tissue eosinophilia, and overall increased number of inflammatory cells .
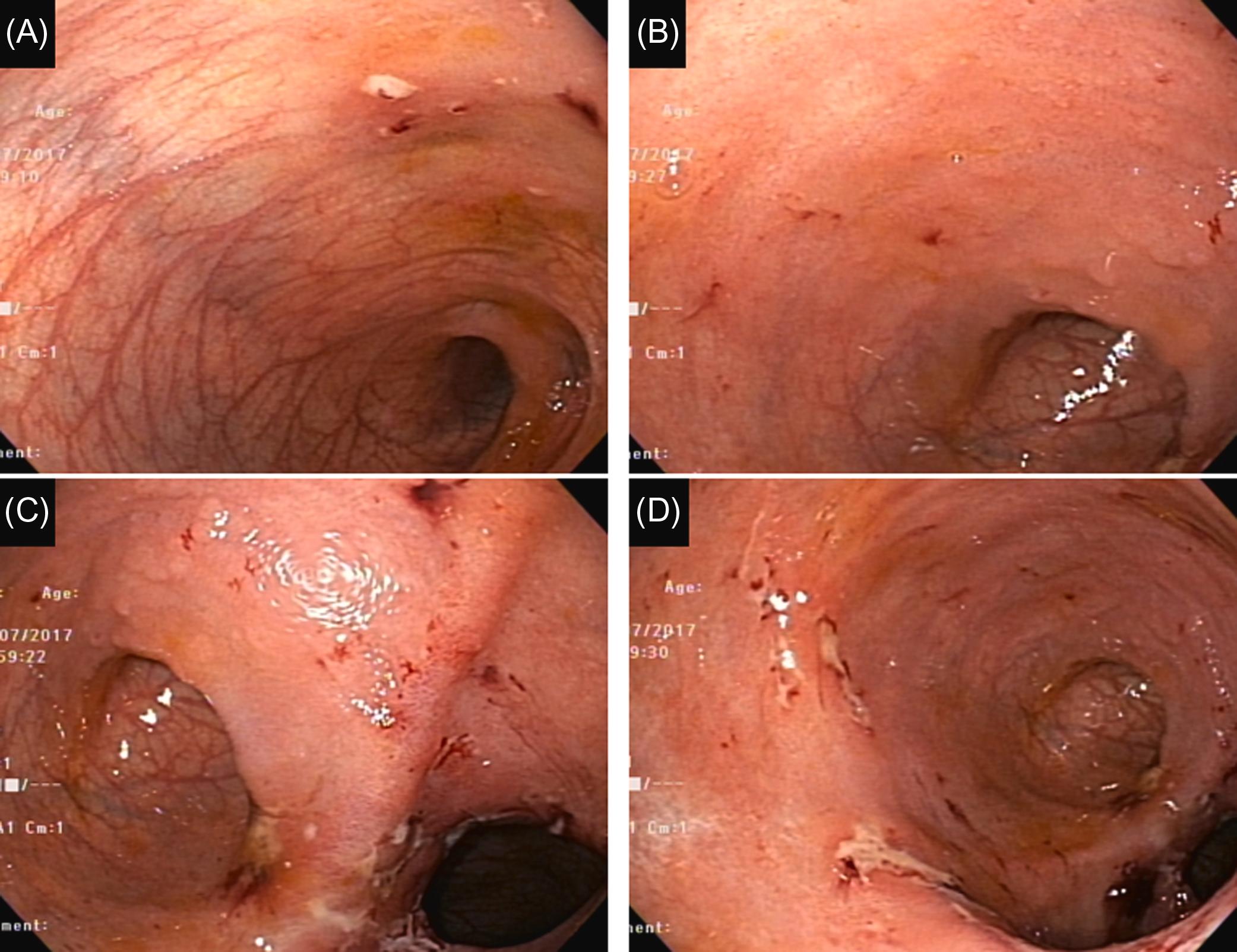
The first step in the management of NSAID-induced enteropathy is the discontinuation of the drug. In a retrospective analysis, improvement in the endoscopic ulcers upon discontinuation of NSAIDs for 3 to 10 weeks was documented . Further management modalities vary and depend on the underlying type of lesion. Endoscopic hemostasis may be required in the setting of active GI bleeding. Endoscopic intervention such as balloon dilation, endoscopic stricturotomy, or surgery might be required in the case of refractory, symptomatic stricturing disease ( Fig. 29.10A and B ) .
Oral potassium agents, particularly slow-release potassium chloride tablets, can cause ulcerations in the esophagus, stomach, or small intestine . Oral potassium agents may also cause mucosal injury to GI tract in patients with CD ( Fig. 29.18 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here