Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Atrial fibrillation (AF) is the most common sustained cardiac rhythm abnormality. The prevalence of AF is increasing because of a combination of factors, including the aging of the population, a rising prevalence of chronic heart disease, and more frequent diagnosis by enhanced monitoring devices.
Because it is more common with advanced age, rates of AF in those older than 80 years have been reported to be 5% to 10%. It is more common in men and less common among African Americans. AF is often associated with structural heart disease, although a significant proportion of patients have no detectable heart disease.
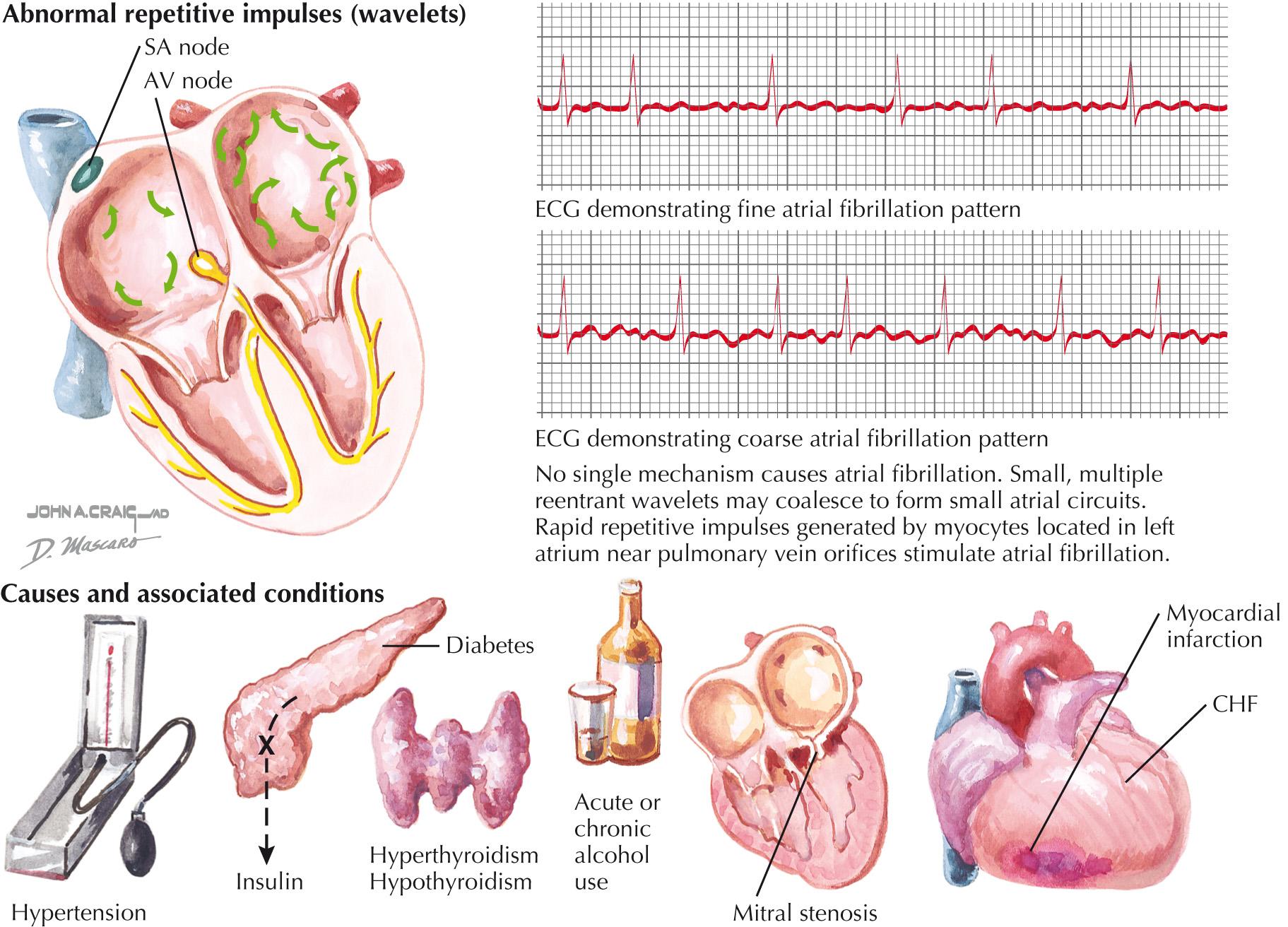
AF is a supraventricular tachyarrhythmia characterized by uncoordinated atrial activity, which leads to ineffective atrial contraction. It is identified on ECG by irregular RR intervals (if atrioventricular [AV] conduction is intact) and the absence of repetitive, organized P waves.
The duration of AF episodes is used to divide the diagnosis into three categories. Paroxysmal AF (pAF) is AF that terminates spontaneously or with intervention within 7 days of onset. Persistent AF continues for >7 days. Permanent AF describes a shared decision by the patient and provider to cease attempts at restoration or maintenance of sinus rhythm.
Two other definitions are worth noting. Nonvalvular AF refers to AF in the absence of rheumatic mitral stenosis, a mechanical or bioprosthetic heart valve, or mitral valve repair. Lone AF generally refers to AF in a younger person without cardiac disease, hypertension, or diabetes. Because it has been used inconsistently, lone AF may be a confusing term, and as such, should not be used to guide clinical decision-making.
The mechanisms underlying AF are numerous. AF can be looked at as a phenotype or common manifestation of a variety of pathologies, rather than as an isolated disease process of its own. The development of AF is promoted by disturbance of atrial architecture. Atrial fibrosis is most commonly due to those heart diseases that increase atrial pressure and wall stress (e.g., hypertension, coronary artery disease, valvular heart disease, and heart failure). The morbidity associated with AF is a reflection of the morbidity of those underlying maladies.
The initiation and maintenance of AF requires both a trigger and an appropriate atrial substrate. Ectopic foci often provide the trigger, and these commonly arise from left atrial tissue extending into the pulmonary veins. For this reason, pulmonary vein isolation remains fundamental to catheter ablation of AF. There are several theories to explain the maintenance of AF, including reentrant wavelets, spiral rotors, and multiple, rapidly firing foci. These are all potential therapeutic targets.
AF has been related to multiple risk factors ( Box 38.1 ). Its onset can be associated with acute causes, such as binge alcohol intake, surgery, myocardial infarction, pericarditis, pulmonary disease, or hyperthyroidism ( Fig. 38.1 ). Most often in these cases, treatment of the inciting conditions will lead to resolution of the AF. AF has also been associated with obesity and obstructive sleep apnea. Multiple cardiovascular conditions are linked to AF, including valvular heart disease, heart failure, coronary artery disease, hypertension (particularly with left ventricular hypertrophy), hypertrophic cardiomyopathy, restrictive cardiomyopathy, congenital heart disease, and pericardial disease. In these conditions, treatment of the underlying cause does not usually abolish AF. Familial AF has been increasingly recognized and is probably a result of genetic abnormalities, which lead to abnormal function of cardiac ion channels. Finally, approximately 30% to 45% of cases of pAF and 20% to 25% of persistent AF occur in patients without predisposing conditions.
Increasing age
Hypertension
Diabetes mellitus
Myocardial infarction
Valvular heart disease
Heart failure
Obesity
Obstructive sleep apnea
Cardiothoracic surgery
Smoking
Exercise
Alcohol use
Hyperthyroidism
Increased pulse pressure
European ancestry
Family history
Genetic variants
ECG
Left ventricular hypertrophy
Echocardiographic
Left atrial enlargement
Decreased LV fractional shortening
Increased LV wall thickness
Biomarkers
Increased C-reactive protein
Increased B-type natriuretic peptide
LV , Left ventricular.
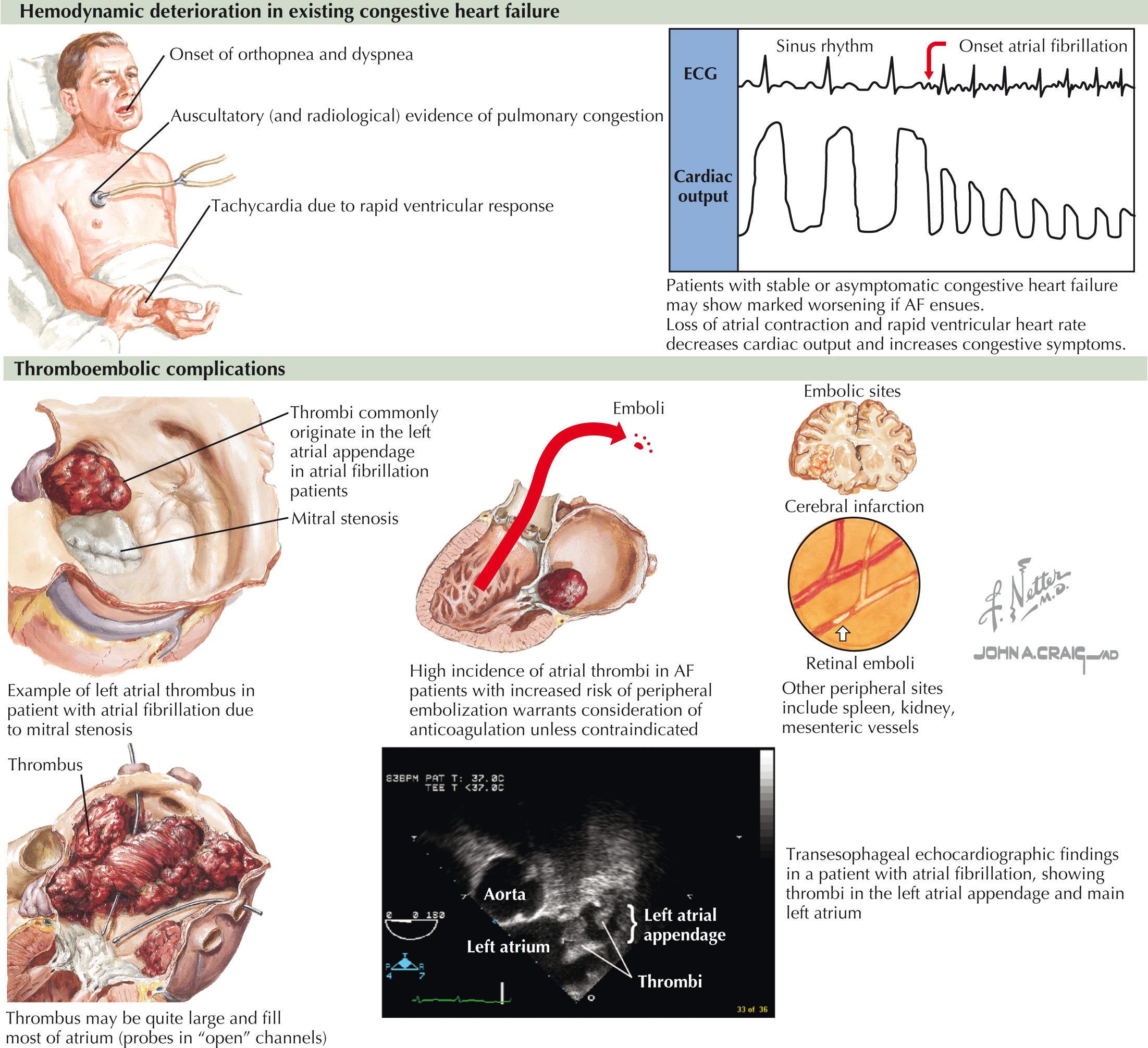
The presentation of AF is diverse. Individual experiences of AF range from no symptoms to palpitations, dyspnea, or heart failure, with the most common symptom being fatigue. The hemodynamic or thromboembolic complications of AF are not infrequently the manner of its initial presentation ( Fig. 38.2 ). Aside from the functional impairment associated with stroke, AF in and of itself can considerably impair quality of life.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here