Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vascular laboratory technology offers many cost-effective applications in the practice of vascular medicine. Vascular testing includes both physiological testing and duplex ultrasonography. Physiological testing includes segmental pressure measurements, pulse volume recordings (PVRs), continuous wave (CW) Doppler, and plethysmography. These tests use sphygmomanometric cuffs, Doppler instruments, and plethysmographic recording devices. Duplex ultrasonography combines gray-scale and Doppler imaging with spectral and color Doppler and is used for the majority of vascular laboratory tests. An ultrasound machine should be equipped with vascular software and two transducers/probes, at least 5- to 12-MHz transducers for the neck and extremities and 2.25- to 3.5-MHz transducers for the abdomen. There are currently many options available, such as 6- to 15-MHz transducers.
Limb segmental systolic blood pressure measurements and PVRs are used to confirm a clinical diagnosis of peripheral artery disease (PAD) and further define the level and extent of the obstruction. Segmental pressures are typically measured in conjunction with segmental limb plethysmography (PVRs). These techniques are used predominantly in the lower extremities but are also applicable to the arms. Both procedures are performed using sphygmomanometric cuffs that are appropriately sized to the diameter of the limb segment under study. The patient rests in the supine position for at least 10 minutes prior to measuring limb pressures. Commercially available machines with automatic cuff inflation are able to digitally store the pressures and waveforms. A CW Doppler instrument with a 4- to 8-MHz transducer frequency is used to detect the arterial flow signal. The cuff is quickly inflated to a suprasystolic pressure and then slowly deflated until a flow signal occurs. The cuff pressure at which the flow signal is detected is the systolic pressure in the arterial segment beneath the cuff. For example, if the cuff is on the high thigh and the sensor is over the posterior tibial artery at the ankle, the measured pressure is reflective of the proximal superficial and deep femoral arteries beneath the cuff, as well as any collateral arteries, and not only the posterior tibial artery. The Doppler flow signal from an artery at the ankle is typically used for all limb measurements. It is more accurate, although less convenient, to place the Doppler transducer probe close to the cuff being inflated.
Sphygmomanometric cuffs are positioned on each arm above the antecubital fossa, on the upper portion of each thigh (high thigh), on the lower portions of the thighs above the patella (low thigh), on the calves below the tibial tubercle, and on the ankles above the malleoli. Typically, foot pressures are measured by insonating the posterior tibial and anterior tibial arteries at the ankle level. Both arm pressures at the brachial artery are determined. A difference of greater than 20 mm Hg between the arm pressures indicates the presence of stenosis on the side of the lower pressure. Pressure measurements are made at the high thigh, low thigh, calf, and ankle levels with a tibial or dorsalis pedis signal selected as the flow indicator. There is a second method which uses one long contoured thigh cuff rather than two separate thigh cuffs. The lower extremity pressure evaluation should begin at the ankle level and proceed proximally. Patients who are found to have a normal pressure measurement at rest may require a treadmill exercise test to detect PAD. If disease distal to the ankle is suspected, pedal or digital artery obstruction can be evaluated with cuffs sized appropriately for the toes.
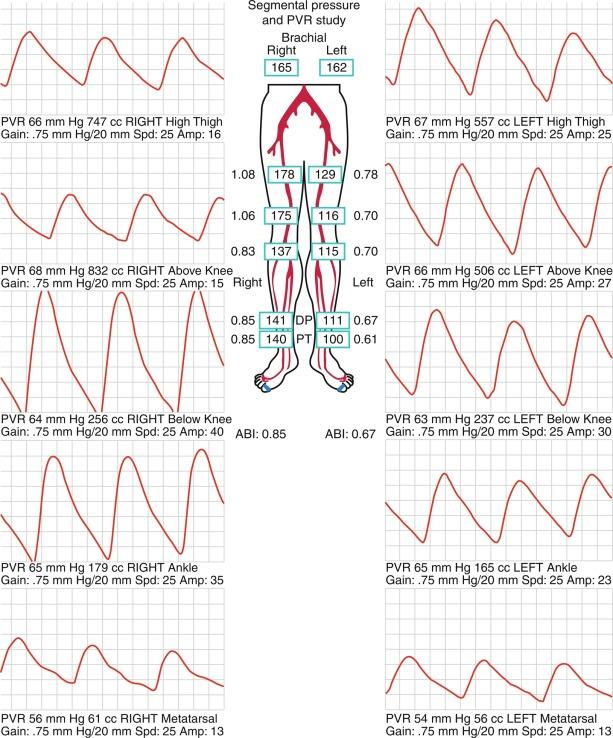
Segmental limb pressures are compared with the highest arm pressure. The ankle pressures are used to calculate the ankle-brachial indices (ABIs) for each extremity. This is accomplished by dividing each of the ankle pressures by the higher of the brachial artery pressures. A normal ABI is between 1.0 and 1.4, whereas an ABI > 0.9 to 1.0 is borderline abnormal. Studies that evaluated the ABI in healthy subjects and patients with PAD confirmed by arteriography found that an ABI of ≤ 0.9 was diagnostic of PAD with 79% to 95% specificity and 96% to 100% sensitivity. Pressures are compared between levels. A 20 mm Hg or greater reduction in pressures from one level to the next is considered significant and indicates stenosis between those two levels. In healthy subjects, the high thigh pressure determined by cuff typically exceeds the brachial artery pressure by approximately 30 mm Hg. A thigh/brachial index > 1 is interpreted as normal, and an index ≤ 1 indicates stenosis proximal to the thigh ( Fig. 12.1 ). When the high thigh pressures are low compared with the arm pressure, the site of obstruction could be in the aorta or in the ipsilateral iliac artery, common femoral artery, or proximal superficial femoral artery (see Fig. 12.1 ). If only one high thigh pressure is less than the brachial pressure, then an ipsilateral iliofemoral artery stenosis is inferred.
In the presence of severe vascular calcification, systolic pressures cannot be determined because the vessels are noncompressible. An index ≥ 1.4 suggests vascular calcification artifact and makes interpretation of the pressure measurement unreliable. The presence or absence of a significant pressure gradient cannot be determined in the presence of vascular calcification artifact. In this setting the toe-brachial index (TBI) is a useful measurement. The TBI is the ratio of the systolic pressure in the toe to the brachial artery systolic pressure. This should be performed in a warm room, because cold-induced vasoconstriction may lower the digital pressure. To perform the procedure, a cuff is placed on a toe. Typically, the great toe is used. The pulse waveform is obtained by photoplethysmography or Doppler. The cuff is inflated to suprasystolic pressure and then deflated. Systolic pressure is determined as the pressure at which the waveform reappears. A normal value for TBI is 0.70, and a value less than 0.70 indicates the presence of PAD.
The same cuffs used to measure segmental pressures may be attached to a plethysmographic instrument and used to record the change in volume of a limb segment with each pulse, designated the pulse volume. The pulse volume waveform evaluation allows assessment of arterial flow in regions of calcified vessels because the test does not rely on cuff occlusion of the calcified artery. Each cuff is inflated in sequence to a predetermined reference pressure, up to 65 mm Hg. The change in volume in the limb segment causes a corresponding change in pressure in the cuff throughout the cardiac cycle. Interpretation of the PVR requires calibration of the amount of air in the cuff.
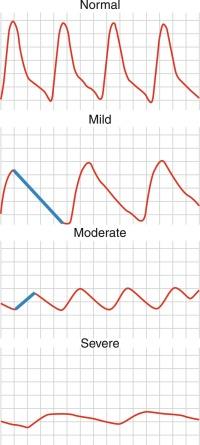
A pulse volume waveform is recorded for each limb segment. PVR analysis is based on evaluation of waveform shape, signal, and amplitude ( Fig. 12.2 ). The configuration of the normal pulse volume waveform resembles the arterial pressure waveform and is composed of a sharp systolic upstroke followed by a downstroke that contains a prominent dicrotic notch. A hemodynamically significant stenosis manifests as a change in the PVR contour with broadening of the wave toward a tardus parvus waveform. Both the slope and amplitude decrease when there is more severe disease. Severity of PAD can be defined by the slope of the upstroke and the amplitude of the pulse volume (see Fig. 12.2 ).
Pulse waveforms can also be obtained using photoplethysmography, recording reflected infrared light. In photoplethysmography, the signal is proportional to the quantity of red blood cells in the cutaneous circulation; it does not measure volume changes. Waveform shape is assessed in a similar fashion in pulse volume and photoplethysmography recordings. Low photoplethysmographic waveforms in the toes identify increased risk of amputation, in addition to the toe pressure.
Exercise testing is an adjunctive physiologic test to evaluate PAD. It is useful to assess functional capacity and determine the distance patients with claudication are able to walk. Moreover, it can be used to clarify whether leg symptoms are related to PAD. This is relevant in patients with symptoms that are atypical for claudication and in those who have a history of intermittent claudication, yet normal ABIs at rest. There is also a role for TBI and transcutaneous tissue oxygen pressure in the evaluation of PAD. Relative contraindications to treadmill exercise testing for PAD include rest pain in the leg, shortness of breath with minimal exertion, or unstable angina. The test cannot be performed if the patient cannot walk on a treadmill.
Patients are instructed to fast for 12 hours prior to walking on the treadmill. The constant load treadmill test is performed at a speed of 2 miles per hour and an incline of 12%. Graded exercise protocols increase the grade and/or speed in 2- to 3-minute stages. The Gardner protocol is the most commonly used graded protocol to evaluate walking exercise capacity. It begins at a speed of 2 mph and an incline of 0% and the grade increases by 2% progressively every 2 minutes, allowing for a wider range of responses to be measured. It is often used to determine clinical trial end points, such as change in walking time in response to therapy. Other graded exercise protocols, such as the Bruce protocol, are not commonly used because the rapid rate of speed and incline limits the assessment of exercise capacity in claudicants.
The treadmill exercise test is terminated when the patient cannot continue due to leg claudication or chest pain or is limited by other symptoms such as shortness of breath or fatigue. The patient then immediately lies down on the stretcher. The ankle pressures are obtained starting with the symptomatic leg, followed by the highest brachial pressure. The pressures are repeated approximately every 1 to 2 minutes until they return to baseline. Data recorded from the exercise test should include ankle pressures, length of time the patient could walk, time required for the pressures to return to baseline, nature and location of the patient’s symptoms, and reason for discontinuing the test. A decrease in ABI to < 0.90 or decrease in ABI of more than 20% immediately following exercise is diagnostic for PAD. The time before ankle pressure returns to normal is increased in more severe disease (e.g., from 2 minutes in mild disease to 10 minutes in more severe disease).
By exploiting the variations in color absorbance of oxygenated and deoxygenated hemoglobin, transcutaneous oximetry can determine the state of blood oxygenation. Oximeters use two light frequencies, red at 600 to 750 nm and infrared at 800 to 1050 nm, to differentiate oxygenated and deoxygenated hemoglobin. Deoxygenated blood absorbs more red light, whereas oxygenated blood absorbs more infrared light. Oximeters typically use both an emitter and receiver. Red and infrared light is emitted and passes through a relatively translucent structure, such as the finger or earlobe. A photodetector determines the ratio of red and infrared light received to derive blood oxygenation. When measured continuously, oxygenation peaks with each heartbeat as fresh, oxygenated blood arrives in the zone of measurement. The normal values for oxygen tension are from 50 to 75 mm Hg. One probe is placed on the chest as a control to ensure that the oxygen tension is from 50 to 75 mm Hg. A second probe is placed on the limb in the area of interest. Measurements are obtained from the probe, which is sequentially positioned from proximal to distal segments of the limb. The normal limb TcO 2 should approximate that of the chest. Transcutaneous oximetry is most often used to determine the level of amputation. A value of > 20 mm Hg can predict healing at the site with 80% accuracy. This measurement is not affected by arterial calcification.
An ultrasound transducer, or probe, emits sound waves in discrete bundles or pulses into the tissue of interest. On encountering a tissue, a portion of the waves are reflected to the transducer. The fraction of returning waves depends on the density and size of the tissue examined. The depth of tissue is determined by the time required for pulse emission and return. Thus, by integrating the number of returning pulses and the time required for return, a B-mode, or gray-scale, image may be created. The time for wave reflection decreases with higher ultrasound probe frequencies. Transducer probes with higher frequencies image superficial tissues better than probes with lower frequencies but lose depth imaging because of attenuation of the returning emitted pulses.
Improvements in technology have permitted a widening of the bandwidth of vascular transducers and can improve gray-scale imaging using harmonics of the fundamental frequency. A harmonic represents a whole number multiple of the emitted frequency. Because the tissue compresses and expands in response to the application of ultrasound, the fundamental wave may become distorted, impairing image quality. However, the distortion also creates harmonics of the original frequency that can be detected by the transducer. By detecting only the fundamental frequency and its harmonics, artifact (e.g., speckle and reverberation) may be reduced to create a clearer image.
Normal blood flow is laminar in a straight segment of an artery. If thought of as a telescopic series of flow rings, blood moves forward most rapidly in the middle ring and velocity decreases in the outer rings as blood comes closer to the vessel wall. The cardiac cycle, defined by its pulsatile nature of flow, causes a continual variation in blood flow velocity, highest with systole and lowest with diastole. The concentric or laminar flow of blood may be disturbed at a normal branching point or with abnormal vessel contours, such as those caused by atherosclerotic plaque. Disturbed or turbulent flow causes a much greater loss of pressure than does laminar flow.
Determination of flow velocity is a mainstay of vascular ultrasonography. Abnormalities in the vessel wall cause changes in flow velocity and permit the detection and assessment of stenotic regions within the vessel. Flow in a normal vessel is proportional to the difference of pressure between the proximal and distal end of the vessel. The prime determinant or limitation of flow is the radius of the vessel because volume of blood flow is determined by the fourth power of the radius. For example, a 50% reduction in vessel radius causes a greater than 90% reduction in blood flow. Thus blood flow represents an example of Poiseuille’s law, which determines flow of a viscous fluid through a tube. Specifically,
where Q denotes the volume of flow; Δ P is pressure at inflow minus the pressure at outflow; r is the radius; η is the viscosity; and L is tube length. Because blood viscosity, blood vessel length, and pressure remain relatively stable, the most important determinant of blood flow is vessel lumen size.
Vascular ultrasonography can depict flow velocity by taking advantage of Doppler shift frequencies. The frequency will shift, either positively or negatively, depending on the direction of blood flow. The variables, which determine the size of the shift, include the speed of sound, the speed of the moving object, and the angle between the transmitted beam and the moving object. Christoph Doppler described this relationship using the following equation:
where F d is the Doppler frequency shift; F t is the Doppler frequency transmitted from the probe; V is the velocity of flow; cos is the cosine, θ is the angle between the beam and direction of the moving object, and c is the velocity of sound.
Although a highly reliable imaging modality, ultrasound does suffer from occasional image artifact. Dense objects, such as vessel wall calcium deposits, permit few sound waves to penetrate, resulting in acoustic shadowing and diminishing imaging of deeper tissues. Tissue imaging enhancement may be noted on the far side of echo-free or liquid-filled zones. Tissue interfaces may generate multiple sound wave reflections, causing “additions” to the tissue termed reverberation artifact. Refraction of the sound pulse may cause improper placement of a structure of an image and shadowing at the edge of a large structure. Highly reflective surfaces may create mirror images because the reflecting tissue alters the timing of the returning sound wave. The mirror image should be equidistant from the reflecting surface or tissue.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here