Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Interventional radiology (IR), also known as vascular and interventional radiology (VIR), is a medical specialty that utilizes image guidance to perform minimally invasive diagnostic or therapeutic procedures. Image guidance may be provided by fluoroscopy, ultrasound (US), computed tomography (CT), or magnetic resonance imaging (MRI).
Interventional radiologists perform a wide variety of procedures that can be characterized as vascular or nonvascular and subdivided into the vascular distribution or organ system for the procedure being performed.
This chapter will discuss the indications, techniques, and benefits of image-guided interventions that cover a broad gamut of interventional procedures.
Arterial access and arteriography are fundamentals of interventional radiology, allowing for diagnostic evaluation of numerous arterial pathologies (e.g., arteriovenous fistula, aneurysm, vascular occlusion, or vascular stenosis).
The Seldinger technique is the basis for modern vascular access, both arterial and venous. This method, first described by Dr. Sven Seldinger (a Swedish radiologist), uses a hollow needle to gain entry into a blood vessel. A wire is then passed through this needle, which is then removed and exchanged for a catheter placed over the wire. This exchange is the basis for the initial steps in a majority of endovascular interventional radiology procedures ( Fig. 28.1 ).
Arterial access is used to facilitate image-guided arterial interventions (e.g., embolization for active bleeding, angioplasty for arterial stenosis, and sclerotherapy for arteriovenous malformation).
Arterial access is most commonly accomplished from a femoral or radial artery approach , though other arteries can be used. The selection depends on a number of factors, including the type of intervention, the anatomic orientation of the vasculature, and the presence of a coagulopathy.
Arterial access is traditionally performed over a bony landmark , which aids in compression of the artery to obtain hemostasis after the procedure is complete. In the case of femoral artery access, the segment of artery over the femoral head is targeted with palpatory, fluoroscopic, and/or ultrasound guidance.
Using the Seldinger technique, an access needle is ultimately exchanged over a wire for a vascular sheath ( Table 28.1 ).
| Device | Description |
|---|---|
| Access needle | The entry needle used at the puncture site for percutaneous procedures; all contain a central channel for introduction of a guidewire. |
| Guidewires | Thin wires of varying lengths, composition, and flexibility that are fed through the channel of the access needle, and over which other devices, themselves containing a hollow channel, can be fed. |
| Catheters | Tubular structures usually made of some kind of plastic with varying lengths, diameters, shapes, and coatings through which substances can be either withdrawn from or introduced into the body. |
| Sheath | A vascular access hollow tube, usually made of plastic, which allows for the exchange of catheters during a given procedure while maintaining vascular access through the same puncture site. |
| Dilator | Short, tapered catheters used to increase the diameter of the hole from percutaneous access to an organ, space, or vessel to allow easier passage of a catheter, sheath, or other device; sometimes used in a serial fashion from smaller to larger. |
Ultrasound guidance during the arterial puncture can sometimes facilitate vascular access, especially in cases of weakly palpable pulses or challenging anatomy.
Radial artery or brachial artery access is similar to the femoral artery approach. In the case of brachial artery access, care must be taken to choose an access site that would allow for compression to obtain hemostasis after the procedure.
Once arterial access is obtained and a catheter or sheath is in place, the injection of iodinated contrast can be performed for arteriography in the desired location.
Arterial access and arteriography allow for diagnostic evaluation and localization of abnormalities and provide a route for endovascular treatment by minimally invasive means.
Risks of arterial access include bleeding and injury to tissues and organs adjacent to the vessels as attempts are made to gain access, such as a pseudoaneurysm at the groin access site from puncture and arterial extravasation (see Fig. 19.6 ).
Arterial access carries the further risk of dissection , bleeding , or thrombosis of the accessed vessel. There is a risk of infection and injury to the surrounding structures at the access site. Meticulous technique and experience can help mitigate many of these complications.
Indications for Central Venous Access
Central venous access is a fundamental technique used throughout medicine that allows for entry into the venous system for:
Intervention (e.g., thrombolysis for an occlusive venous thrombus or inferior vena caval filter placement for prevention of pulmonary embolus or stenting).
Placement of a port or catheter for pharmaceutical treatment for oncologic pharmacotherapy.
Hemodialysis/pheresis (i.e., procedures in which blood is filtered, separated, and returned to the patient), as in plasmapheresis.
For venous access, ultrasound guidance is utilized to locate and gain entry into the central veins without injury to adjacent tissues/organs. Nearby anatomic landmarks or the relationship to a known artery may be used instead of ultrasound.
The venous access site of choice depends on the type of procedure performed.
For central venous catheter placement, the internal jugular, femoral, and subclavian veins are commonly used as access points ( Fig. 28.2 ).
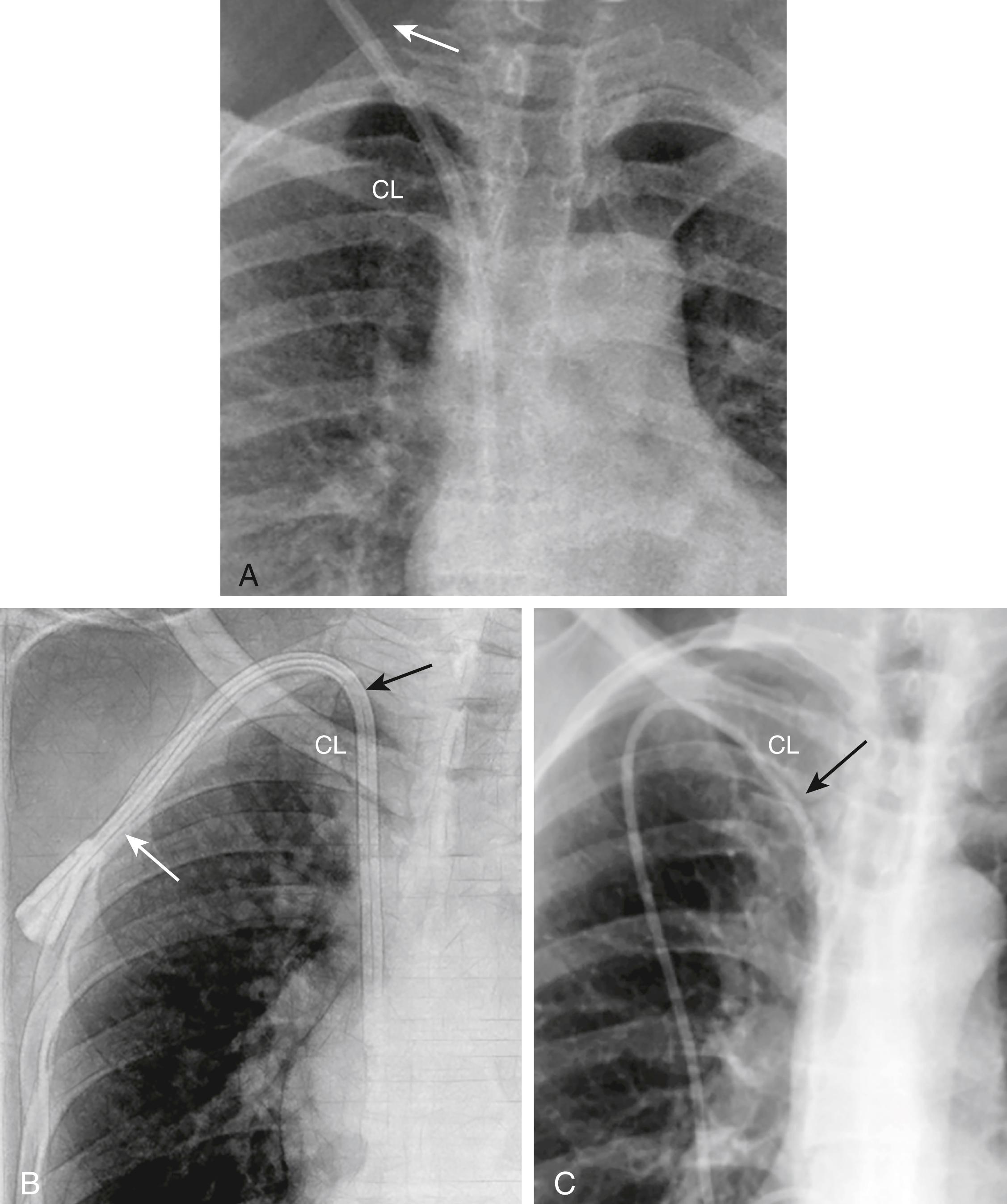
Peripherally inserted central venous catheters (PICCs) are placed in the upper extremity veins, above the elbow, with the tip of the catheter usually located in the superior vena cava (see Fig. 9.9 ).
Most commonly, a needle is inserted into the selected vein with subsequent exchange for a catheter via a wire, using the Seldinger technique. Central venous catheters can be either tunneled or nontunneled ( Fig. 28.3 ).
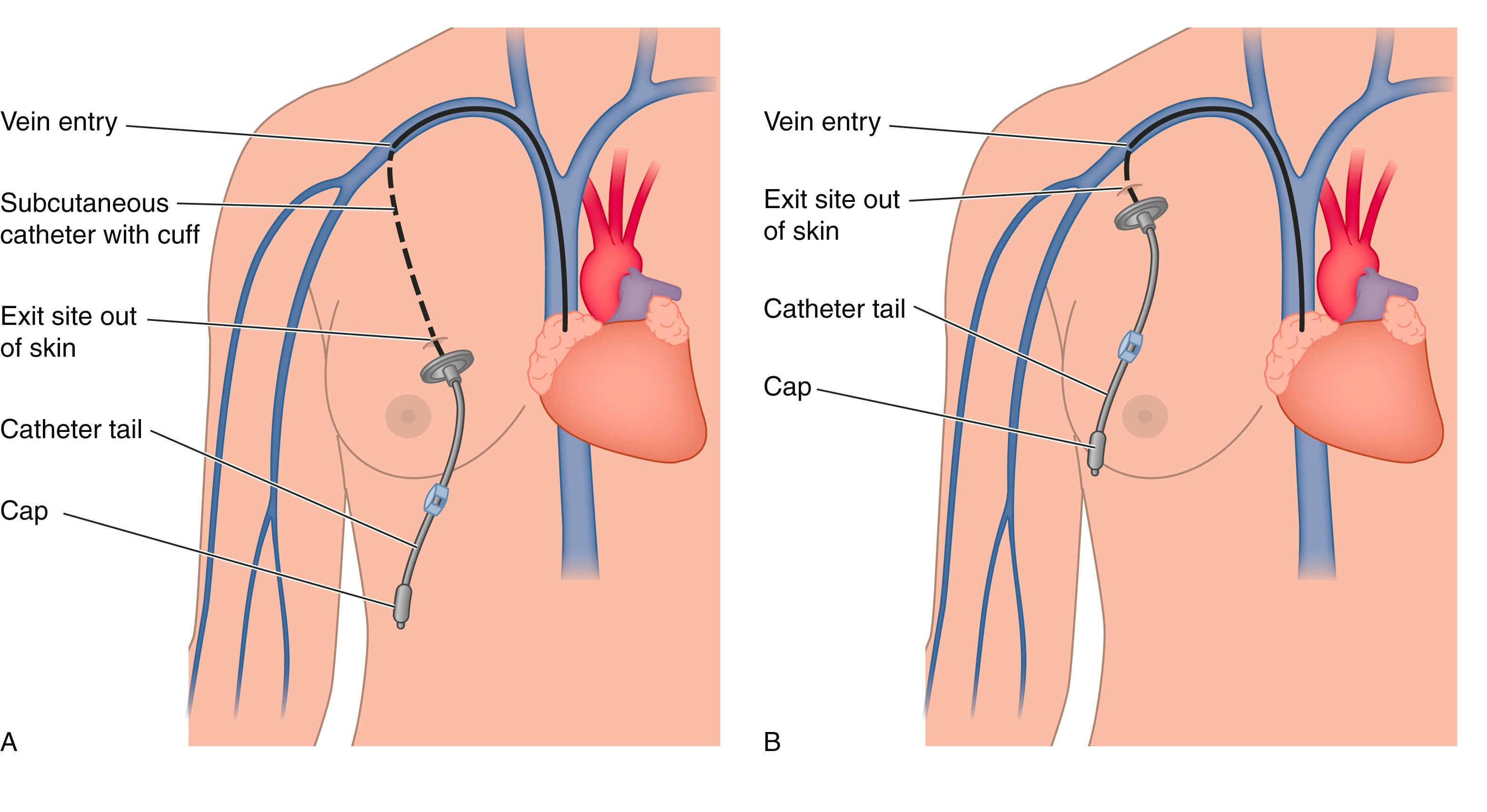
Central venous catheter placement allows for venous access, intervention, and pharmacotherapy. Tunneled or subcutaneous central venous access may obviate the need for repeated central access procedures if multiple treatments are necessary.
Risks of venous access include bleeding and injury to tissues and organs adjacent to the vessels as attempts are made to gain entry. Access from the neck can be complicated by pneumothorax, hemothorax, and inadvertent subclavian and carotid puncture. Arteriovenous fistula formation is a rare, but reported, complication.
Massive pulmonary embolism (PE) is defined as PE with sustained hypotension. This condition may be unrelated to the radiologic burden of clot in the pulmonary arterial tree. The burden of clot generally refers to the qualitative assessment of thrombus in the pulmonary arteries. Quantitative scoring methods exist but are used infrequently.
First-line treatment for massive PE, in the absence of a known contraindication, is intravenous thrombolysis, where a medication, such as tissue plasminogen activator (tPA), is administered in large doses to dissolve the clot.
Indications for catheter-directed pulmonary embolism thrombolysis include:
Patients who have massive PE and would be at high risk for developing a bleeding complication if they were to receive systemic intravenous thrombolytic medication.
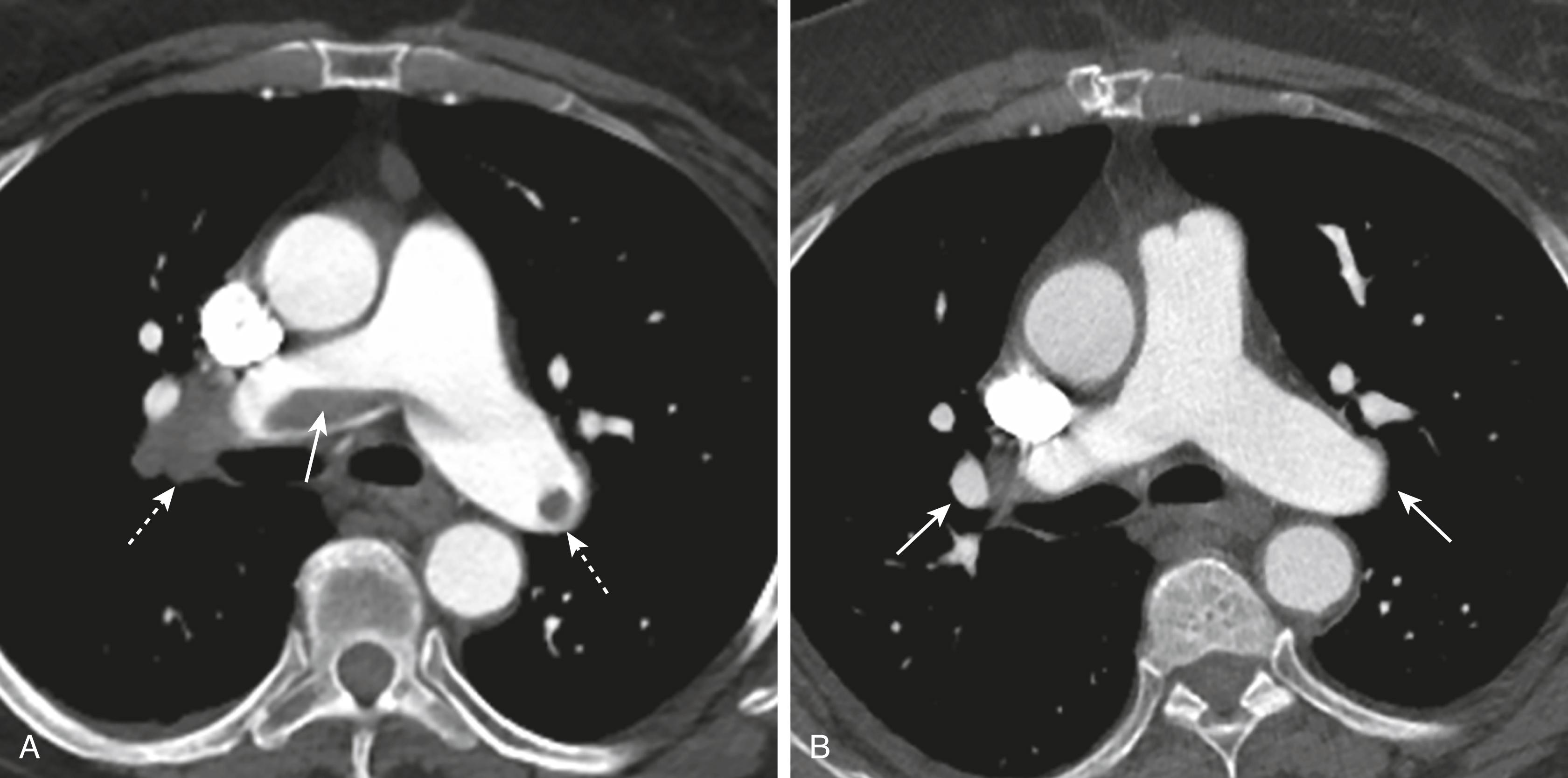
Those who already have active bleeding, are perioperative from major surgery, or who have known metastatic cancer in the brain, for example, are at high risk to receive systemic thrombolytic therapy. They may be candidates for a more focal catheter-based intervention, such as catheter clot fragmentation ( Fig. 28.4 ), aspiration of clot, or lysis catheter placement.
Submassive pulmonary embolism is defined as PE without hemodynamic instability. There is a wide spectrum of disease in this category, from a clinically asymptomatic subsegmental PE that was incidentally noted on chest CT to a large burden of clot in a patient who is tachycardic and may be short of breath.
Although the traditional treatment for submassive PE is intravenous anticoagulation, there has been research and a clinical movement toward catheter-based therapies for the subgroup with high-risk features for progressing to massive PE.
Among others, these risk features include elevated biomarkers (troponin and brain natriuretic peptide) and evidence of right heart strain on imaging.
Under fluoroscopic guidance, a flexible catheter is inserted in the common femoral vein or internal jugular vein and threaded through the heart to access the pulmonary arteries.
Various types of catheters with multiple holes can be placed into the clot itself to administer thrombolytic medications that can be infused over time to dissolve the clot. Other catheters that incorporate technologies to accelerate clot lysis, such as ultrasound , are also in use clinically. Still other devices can also be introduced that fragment or aspirate the thrombus.
Catheter-based thrombolysis or thrombus removal can decrease the right heart pressure rapidly and may prevent the patient from developing further hemodynamic compromise compared with anticoagulation alone.
In the case of massive pulmonary embolism, catheter-based therapies may be lifesaving when systemic thrombolysis is contraindicated or is used but is unsuccessful in improving the patient’s clinical status.
Risks of catheter-based lysis include bleeding at other sites remote to the lytic infusion due to the systemic circulation of the medication after it passes through the lungs back through the heart.
Additional risks include arrhythmias when passing catheters and wires through the heart and, rarely, injury to the pulmonary artery , cardiac valves, or heart itself.
IVC filter placement is a controversial topic but is generally accepted for the following US Food and Drug Administration–approved indications:
Pulmonary thromboembolism when anticoagulation is contraindicated
Progression of venous thromboembolic disease despite use of anticoagulation
After massive PE when anticipated benefits of conventional therapy are reduced
Chronic, recurrent PE when anticoagulant therapy has failed
Vena caval filters may be placed off-label on a case-by-case basis for other indications, such as prolonged immobility after trauma, prior to some types of surgery where the postoperative risk of PE is felt to be high, and as protection for proximal iliac or IVC deep-venous thrombosis.
Contraindications to filter placement include an inability to access the IVC (e.g., due to thrombosis or anatomic anomalies) or a vena caval size too large or too small for a filter to deploy properly.
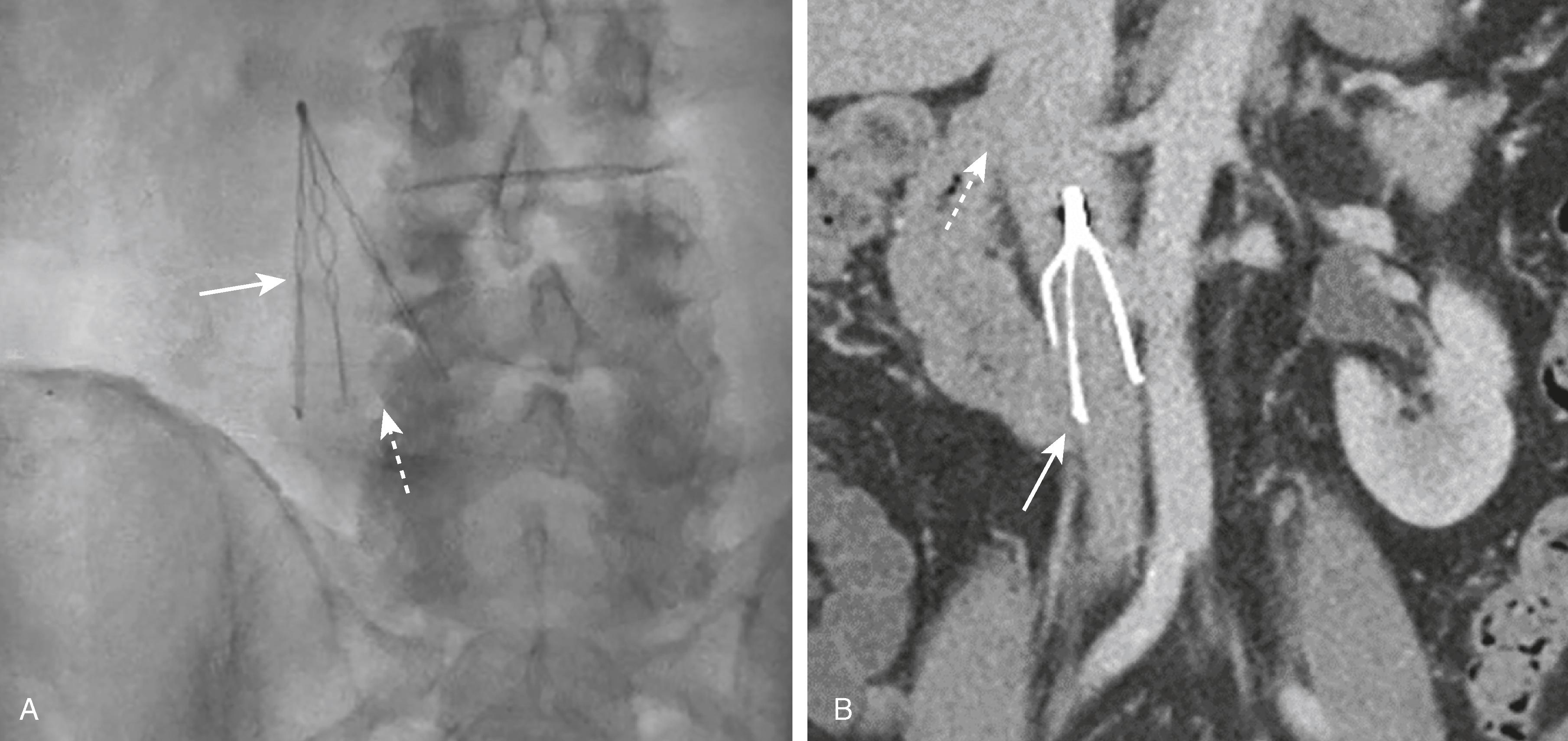
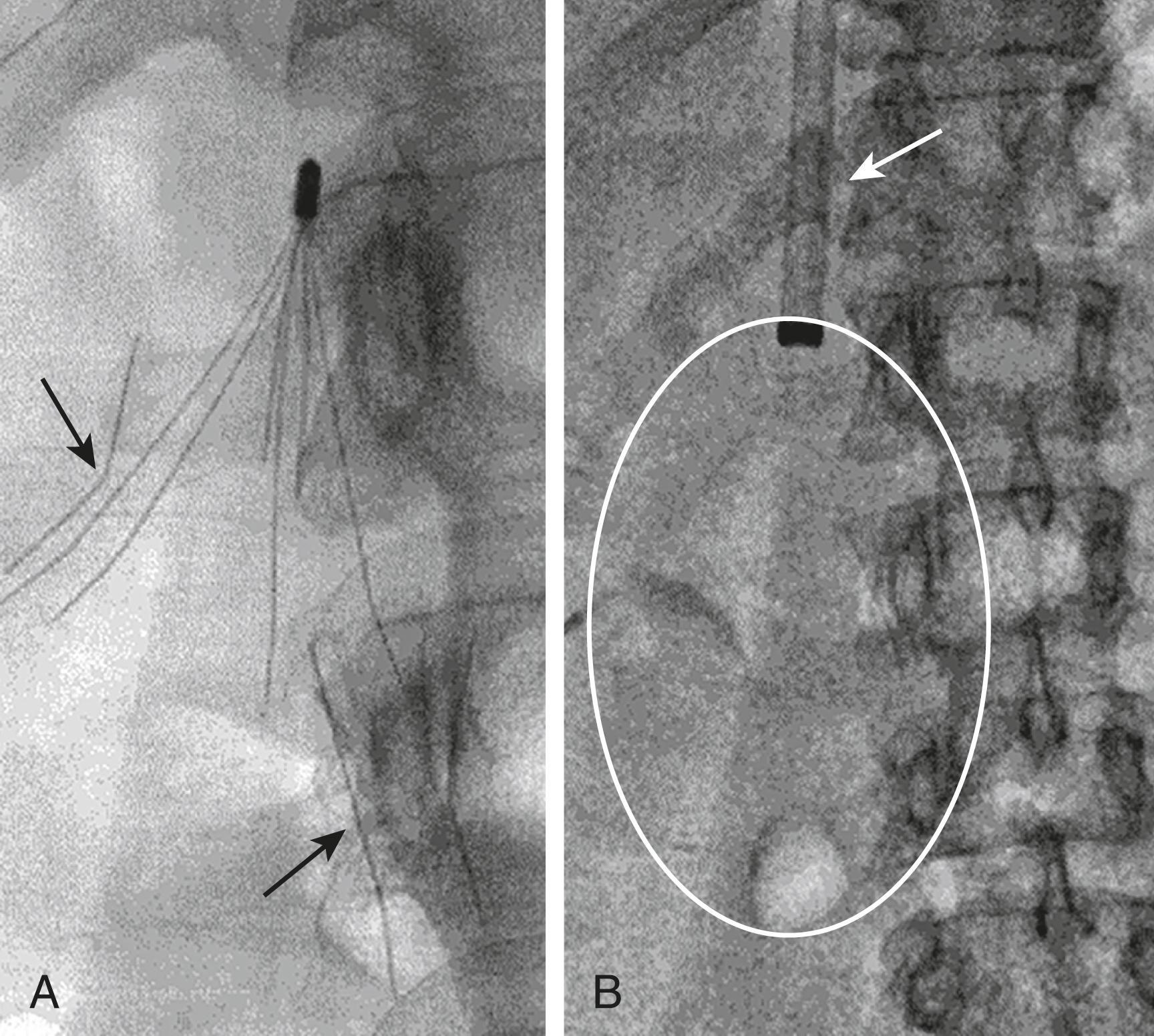
IVC filters are most commonly placed in the infrarenal IVC in proximity to the renal vein inflow. This is felt to promote lysis of clot captured in the filter and prevent filter thrombosis ( Fig. 28.5 ).
A suprarenal filter is sometimes placed above the renal veins when required during pregnancy, when there is insufficient room below the renal veins to accommodate a filter, and in instances where there is variant renal vein anatomy.
Central venous access is obtained via a jugular or femoral vein. The right jugular or right femoral vein is preferred given the typical rigidity of the IVC filter-delivery system, but the left common femoral vein is also commonly used and placement via the upper extremity veins has been described.
IVC venography is first performed with a diagnostic catheter to allow for:
Visualization of the venous anatomy , including location of the renal veins, and to see if any venous variants are present
Determination of the size of the IVC , which can affect the filter type chosen
Determination of IVC patency
After the IVC anatomy and desired filter location have been determined, the catheter is exchanged for an IVC filter-delivery sheath. The filter is deployed from inside the sheath and the sheath is withdrawn.
Postplacement venograms are sometimes performed to confirm appropriate positioning. The catheter and wire are removed. Pressure is then applied to the access site until hemostasis is achieved.
The intended benefit is to potentially decrease the incidence of new clinically significant emboli to the lungs. IVC filters do not prevent new deep-venous thrombi from forming nor do they decrease the amount of thrombus burden already present. The actual clinical benefit, which is still under investigation, is a source of debate.
Potential risks include filter migration, filter fracture, or filter element penetration through the IVC wall. Caval and renal vein thrombosis are other rare, but significant, complications. Some of the risks can be mitigated by retrievable filters if they are removed promptly after caval filtration is no longer medically necessary ( Fig. 28.6 ).
Although counterintuitive, IVC filters have been associated with an increased risk of deep vein thrombosis in the lower extremities.
Image-guided biopsy is a means of accurately obtaining a tissue sample of a lesion for diagnostic analysis.
Sampling of a lesion can determine its characteristics (benign or malignant) or provide additional information about a known lesion (cytogenetics).
The lesion to be sampled should be reliably visualized on at least one imaging modality.
Image-guided biopsy is indicated for the minimally invasive sampling of a lesion previously identified on an imaging study or when pathology is in question in order to aid in yielding a definitive diagnosis.
Sampling of a lesion can be obtained through one of two techniques:
Fine needle aspiration (FNA): A small-gauge needle (e.g., 25 G) is inserted into the lesion under imaging guidance. The needle is then moved back and forth within the lesion to collect cells. Thyroid nodules are commonly sampled with this technique ( Fig. 28.7A ).
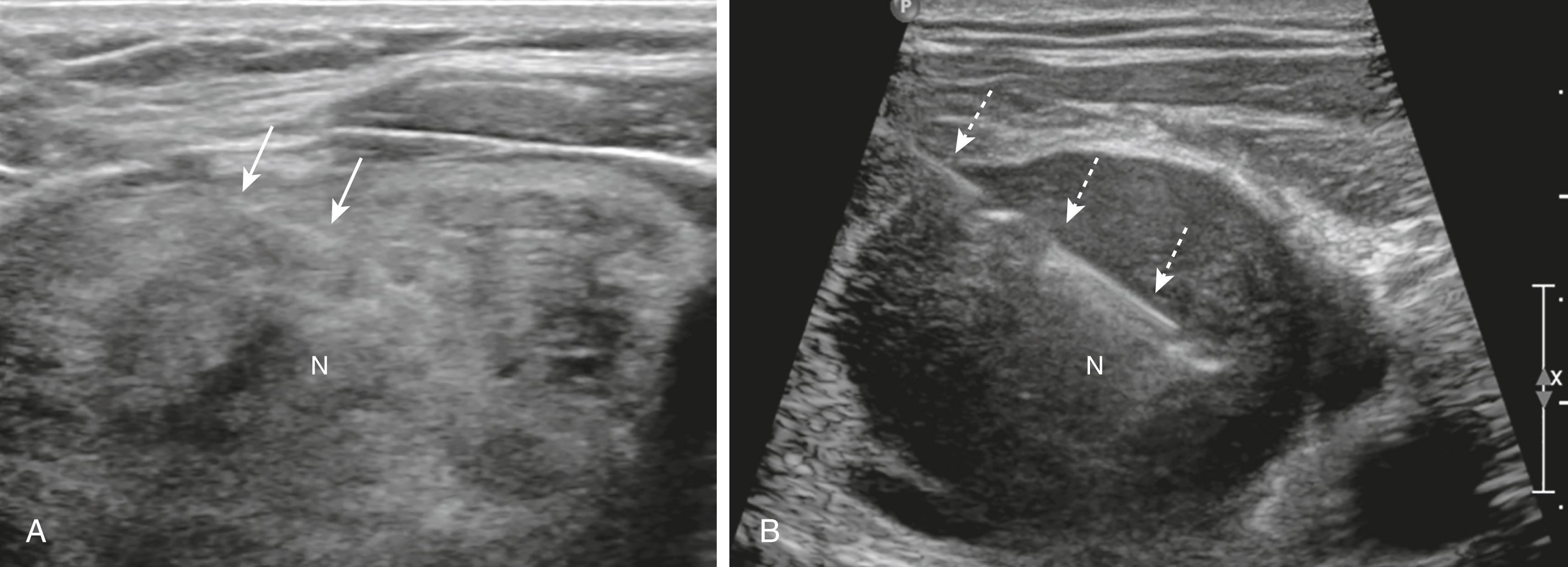
Core biopsy : A larger-gauge needle (e.g., 18 G) is inserted into the lesion under imaging guidance to remove a small piece of tissue. If the situation calls for multiple samples from a challenging location, a coaxial system is often used, which involves placing a larger needle into the lesion (called the access needle ) and performing the biopsy using smaller needles/devices through the larger access needle ( Fig. 28.7B ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here