Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Describe the internal, surface, and relational anatomies of the gallbladder
Explain the function of the gallbladder
Differentiate the sectional anatomy of the hepatobiliary system and adjacent structures
Describe the normal sonographic pattern of the gallbladder, cystic duct, hepatic ducts, and common bile duct
Differentiate the sonographic appearances of the gallbladder and biliary system pathologies discussed in this chapter
Together with the liver and pancreas, the biliary system plays a role in the digestive process. The gallbladder serves as a reservoir for bile that is drained from the hepatic ducts within the liver. Sonographic evaluation of the gallbladder and biliary system is used as a primary diagnostic tool and has proven effective in diagnosing various types of gallbladder disease, including the more common problems of cholelithiasis, cholecystitis, and dilation of the ductal system.
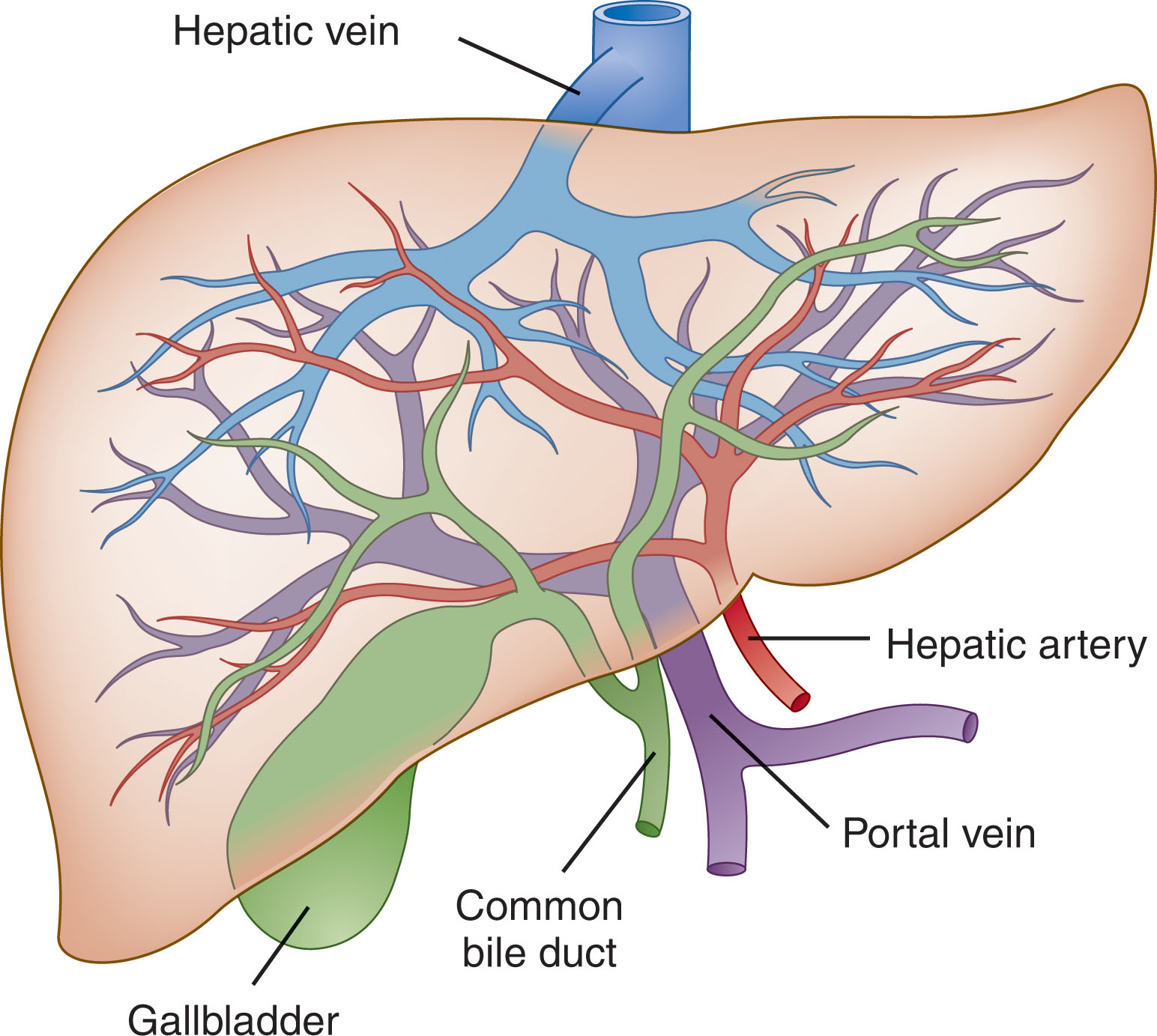
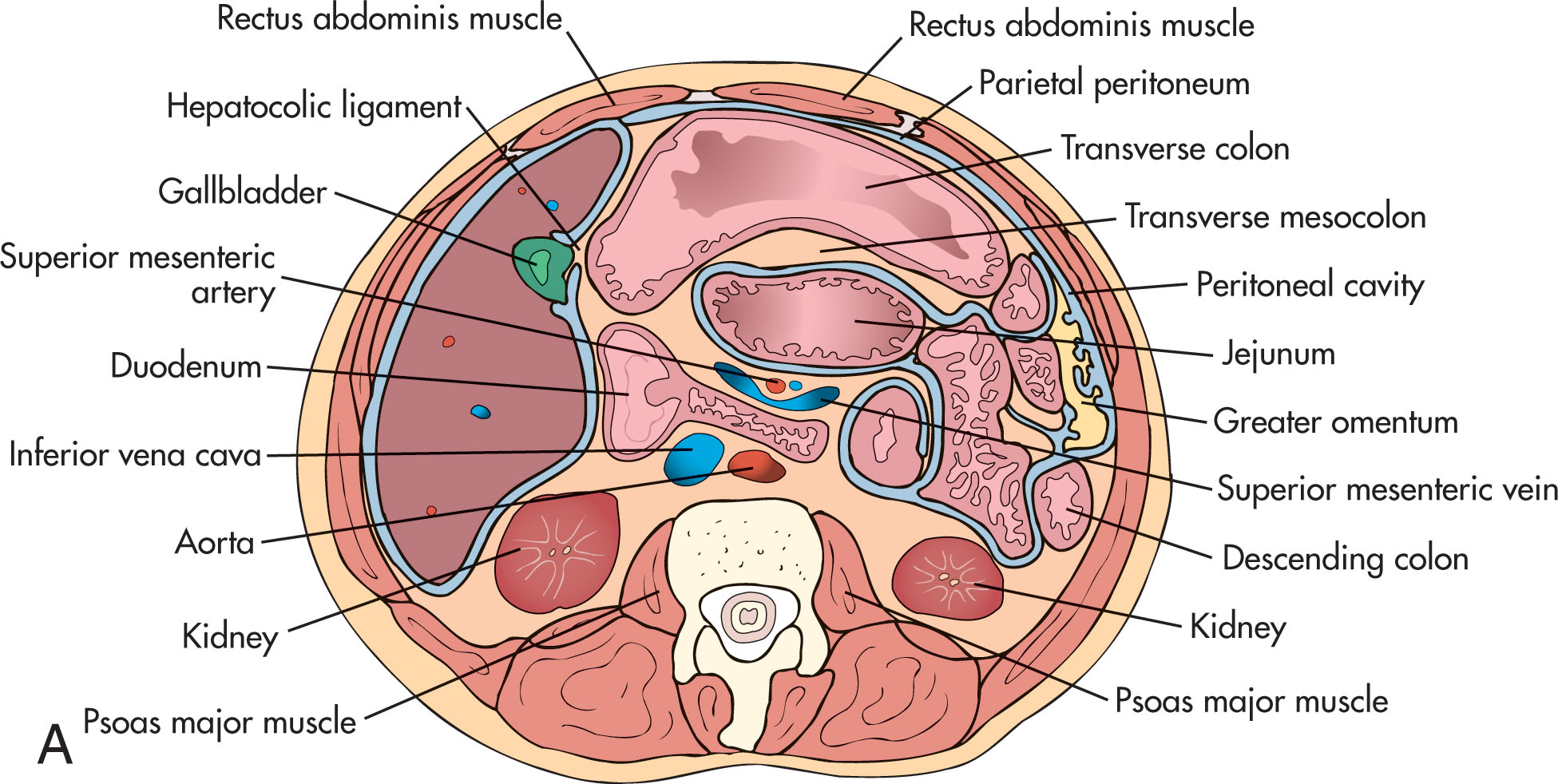
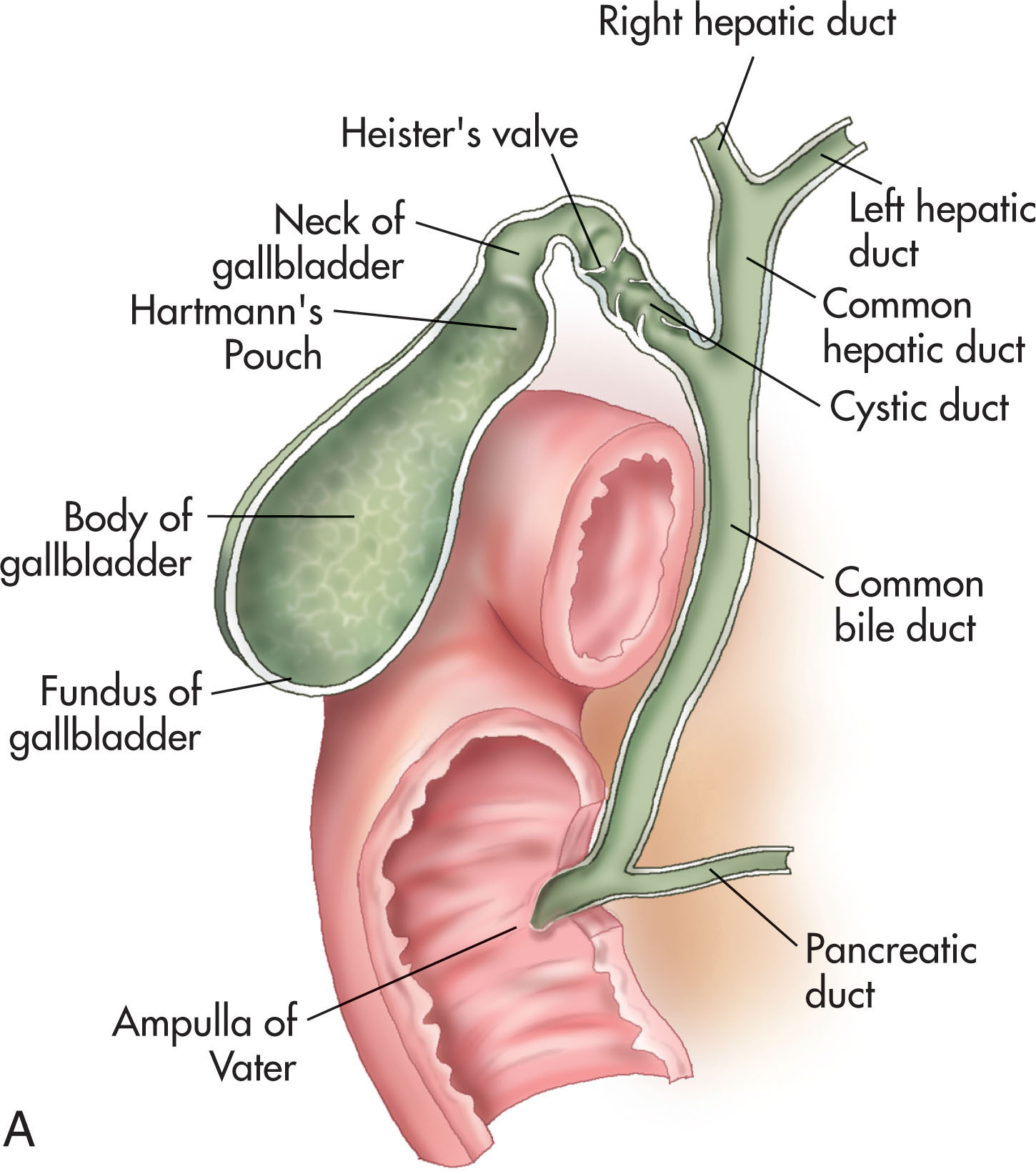
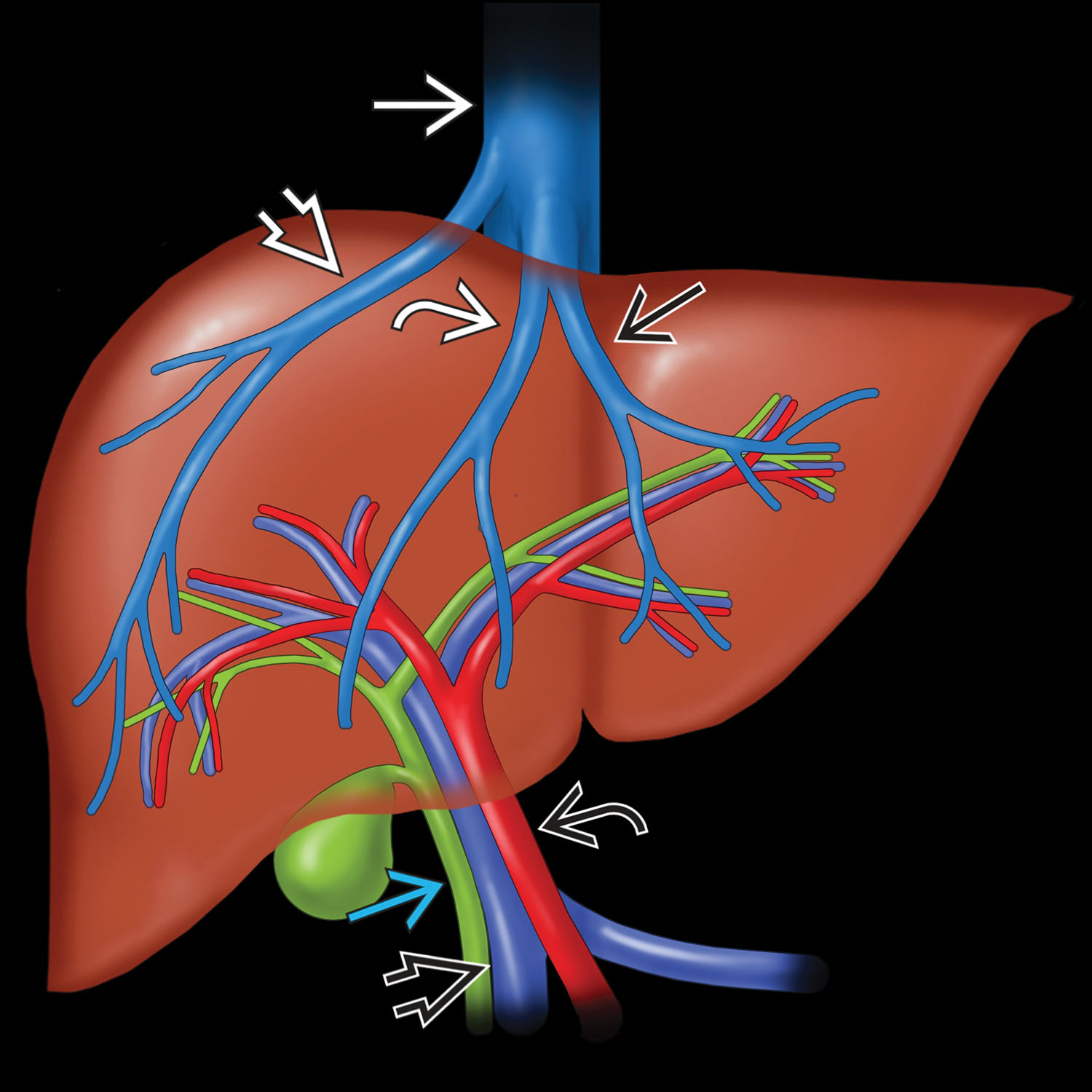
The biliary apparatus consists of the right and left hepatic ducts, the common hepatic duct, the common bile duct, the pear-shaped gallbladder, and the cystic duct ( Fig. 10.1 ). The bile ducts are divided into intrahepatic and extrahepatic segments. The intrahepatic ducts run in the portal triads along with the portal veins and hepatic arteries ( Fig. 10.2 ). The peripheral intrahepatic ducts run parallel and adjacent to the hepatic arteries and portal veins. The anterior and posterior relationship of the three structures is more variable than that of the extrahepatic ducts.
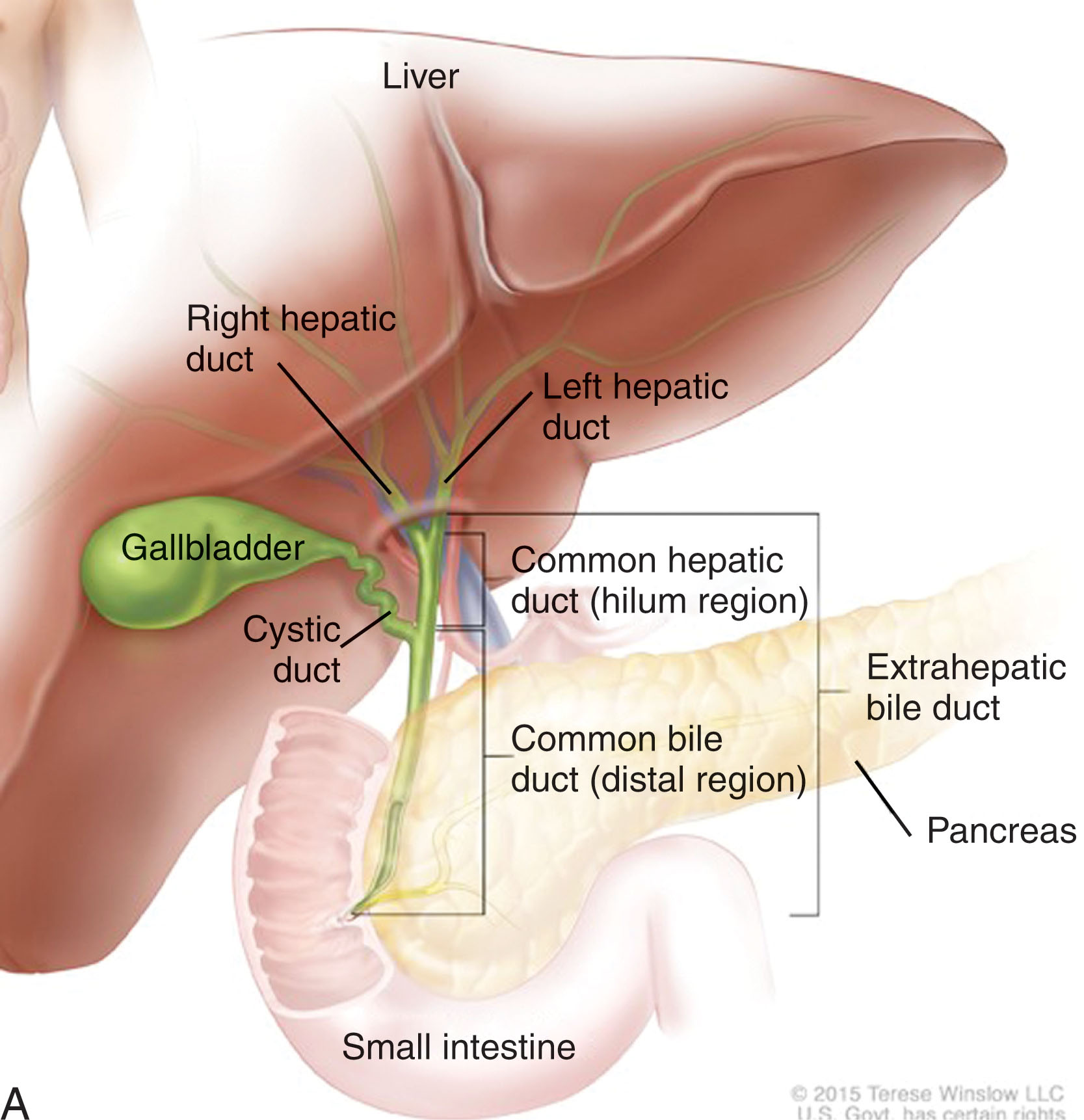
The extrahepatic portion of the bile ducts includes the common hepatic duct, common bile duct, and a portion of the central right and left ducts (see Fig. 10.1 ). The right and left hepatic ducts emerge from the right lobe of the liver in the porta hepatis and unite to form the common hepatic duct, which then passes caudally and medially. The hepatic duct runs parallel with the portal vein. Each duct is formed by the union of bile canaliculi from the liver lobules.
The common hepatic duct is approximately 4 mm in diameter and descends within the edge of the lesser omentum. The common hepatic duct is the segment above the cystic duct, and the common bile duct is the segment below. The cystic duct may be difficult to image on sonography; therefore, the sonographer may use the general term as the proximal or distal segments of the “common duct.” The common hepatic duct is the bile duct system that drains the liver into the common bile duct.
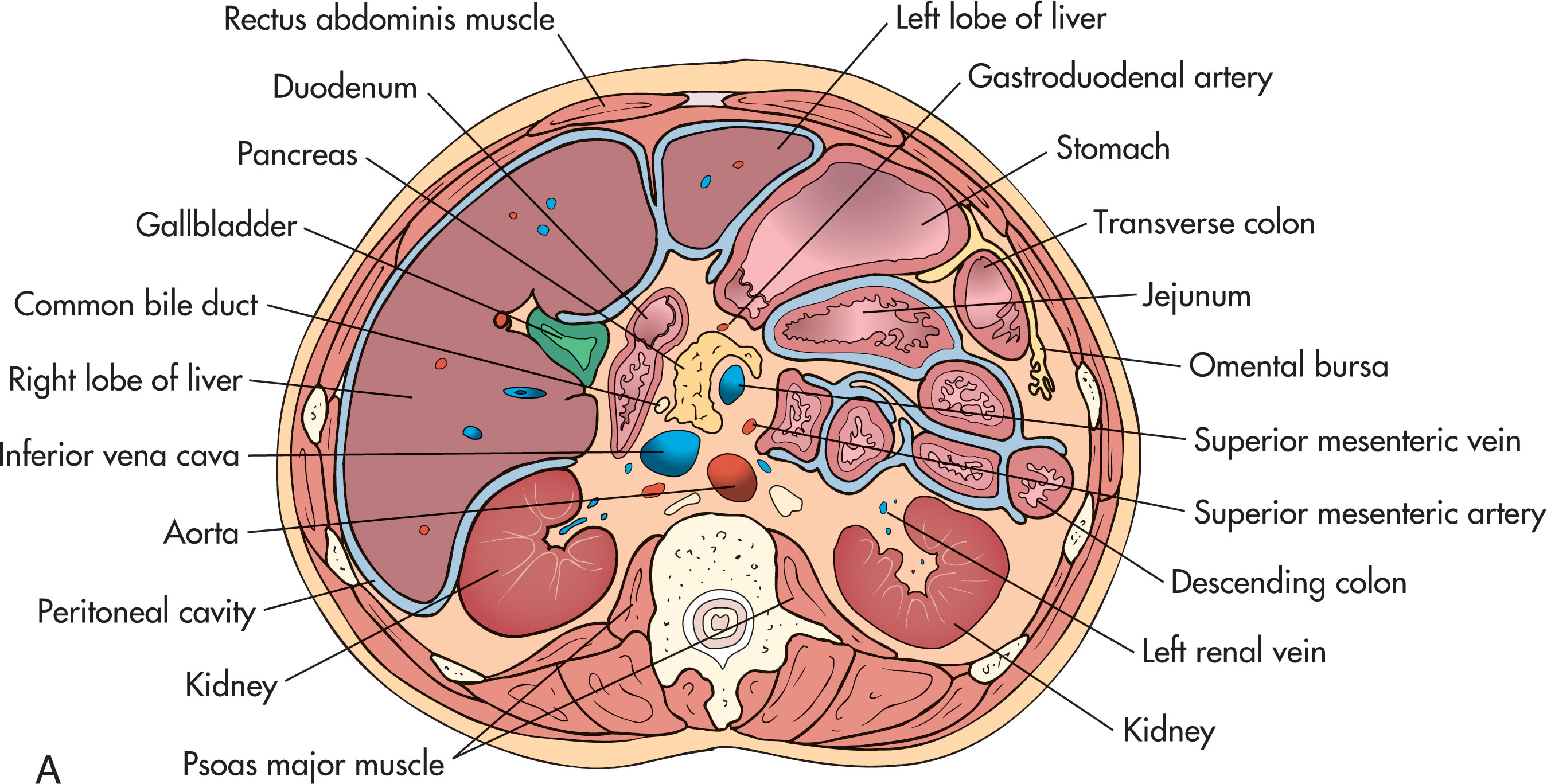
The normal common bile duct has a diameter of up to 6 mm. The first part of the duct lies in the right free edge of the lesser omentum ( Fig. 10.3 ). The second part of the duct is situated posterior to the first part of the duodenum. The third part of the duct lies in a groove on the posterior surface of the head of the pancreas. It ends by piercing the medial wall of the second part of the duodenum about halfway down the duodenal length. The main pancreatic duct joins the common bile duct, and together they open through a small ampulla (the ampulla of Vater ) into the duodenal wall. The end parts of both ducts (common bile duct and main pancreatic duct ) and the ampulla are surrounded by circular muscle fibers known as the sphincter of Oddi .
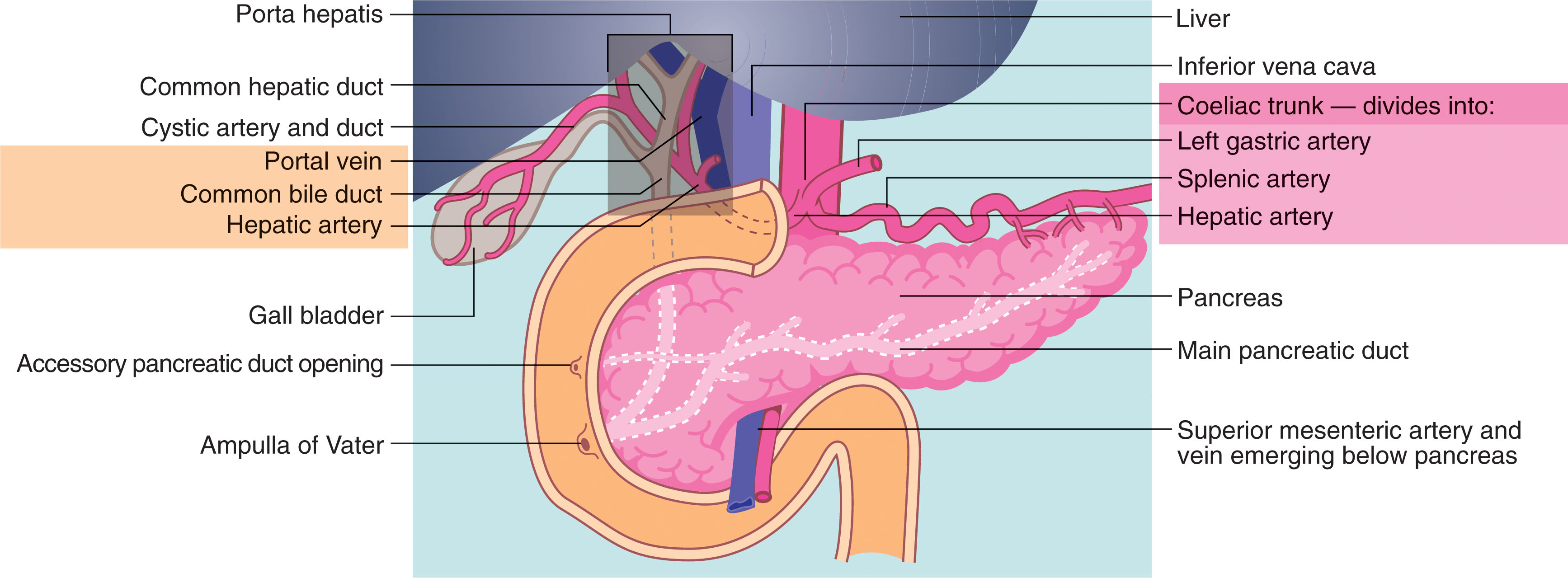
The proximal portion of the common bile duct is lateral to the hepatic artery and anterior to the portal vein. The duct moves more posterior after it descends behind the duodenal bulb and enters the pancreas. The distal duct lies parallel to the anterior wall of the vena cava.
Within the liver parenchyma, the bile ducts follow the same course as the portal venous and hepatic arterial branches. The hepatic and bile ducts are encased in a common collagenous sheath, forming the portal triad. The hepatic artery arises from the celiac axis and travels in the hepatoduodenal ligament anterior to the portal vein and medial to the common duct. On transverse views, this is known as the “Mickey Mouse” sign with the portal vein as the head, the hepatic artery the left ear, and the bile duct the right ear. In most patients, the right hepatic artery passes between the common duct and the portal vein; however, in a small percentage, the hepatic artery passes either anterior to the common duct, or there may be a variant of two hepatic arteries anterior and/or posterior to the duct. The hepatic artery can be quite tortuous, so only a small segment is usually imaged. A replaced right hepatic artery that arises from the superior mesenteric artery is a normal variant that alters the anatomy of the porta hepatis. Color Doppler and tracing the vessel to its point of origin help to define the vessel.
The cystic duct is about 4 cm long and connects the neck of the gallbladder with the common hepatic duct to form the common bile duct. It is usually somewhat S-shaped and descends for a variable distance in the right free edge of the lesser omentum.
The gallbladder is a pear-shaped organ found on the inferior margin of the liver between the right and left lobes of the liver ( Fig. 10.4 ). Two useful anatomical landmarks are utilized to locate the gallbladder. The middle hepatic vein is in alignment with the gallbladder fossa. The interlobar fissure extends from the right portal vein to the gallbladder fossa. The gallbladder lies in the intrahepatic position, but as it migrates to the surface of the liver during embryologic development, it acquires a peritoneal covering over most of its surface ( Fig. 10.5 ). The remainder of the gallbladder surface is covered with adventitial tissue that merges with the connective tissue with the liver. This potential space between the liver and the gallbladder is an area for infection or inflammation to collect. If this migration does not occur, the gallbladder remains intrahepatic, or it may be enveloped in the visceral peritoneum, hanging into the lower abdomen. The gallbladder has been found to lie in various ectopic positions (suprahepatic, suprarenal, within the anterior abdominal wall, or in the falciform ligament). Failure of the gallbladder to develop is rare; this failure is known as agenesis of the gallbladder. These patients may still have the biliary ductal system, which can become inflamed or filled with stones.
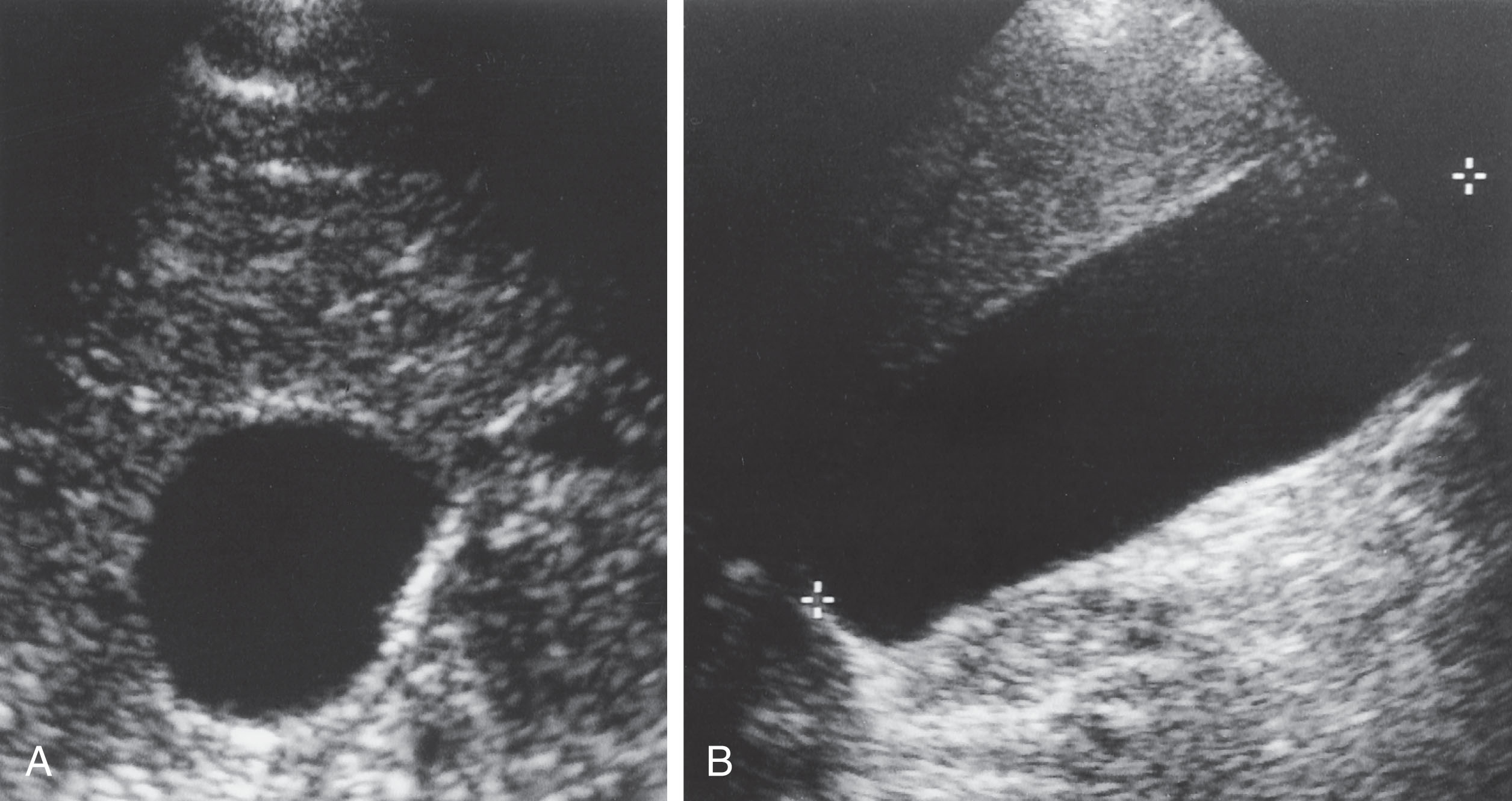
The gallbladder is divided into the fundus, body , and neck ( Fig. 10.6A ). The rounded fundus usually projects below the inferior margin of the liver, where it comes into contact with the anterior abdominal wall at the level of the ninth right costal cartilage. The body generally lies in contact with the visceral surface of the liver and is directed upward, backward, and to the left. The neck becomes continuous with the cystic duct, which turns into the lesser omentum to join the right side of the common hepatic duct to form the common bile duct. The neck of the gallbladder is oriented posteromedially toward the porta hepatis. The fundus is situated lateral, caudal, and anterior to the neck.
The size and shape of the gallbladder are variable. Generally, the normal gallbladder measures approximately 2.5 to 4 cm in diameter and 7 to 10 cm in length. The walls are less than 3 mm thick. Dilation of the gallbladder is known as hydrops .
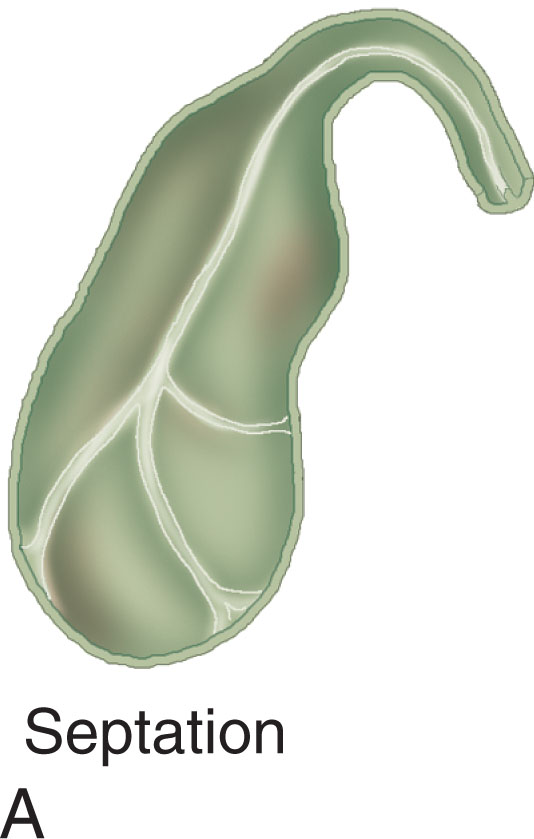
Several anatomic variations may occur within the gallbladder to give rise to its internal echo pattern on the sonogram. The gallbladder may have a small outpouch, also known as the infundibulum, forming Hartmann’s pouch ; this is significant as gallstones may collect in this pouch (see Fig. 10.6B ). Other anomalies include partial septation, complete septation (double gallbladder), and folding of the fundus ( Phrygian cap ) ( Fig. 10.7 ).
With a capacity of 50 mL, the gallbladder serves as a reservoir for bile. It also has the ability to concentrate the bile. To aid this process, its mucous membrane contains folds that unite with each other, giving the surface a honeycomb appearance. Heister valve in the neck of the gallbladder helps prevent kinking of the duct (see Fig. 10.6A ).
The arterial supply of the gallbladder is from the cystic artery, which is a branch of the right hepatic artery (see Fig. 10.3 ). The cystic vein drains directly into the portal vein. Smaller arteries and veins run between the liver and the gallbladder.
The primary functions of the extrahepatic biliary tract are (1) the transportation of bile from the liver to the intestine and (2) the regulation of its flow. These are important functions as the liver secretes approximately 1 to 2 L of bile per day. When the gallbladder and bile ducts are functioning normally, they respond in a fairly uniform manner in various phases of digestion. Concentration of bile in the gallbladder occurs during a state of fasting. It is forced into the gallbladder by an increased pressure within the common bile duct, which is produced by the action of the sphincter of Oddi at the distal end of the gallbladder.
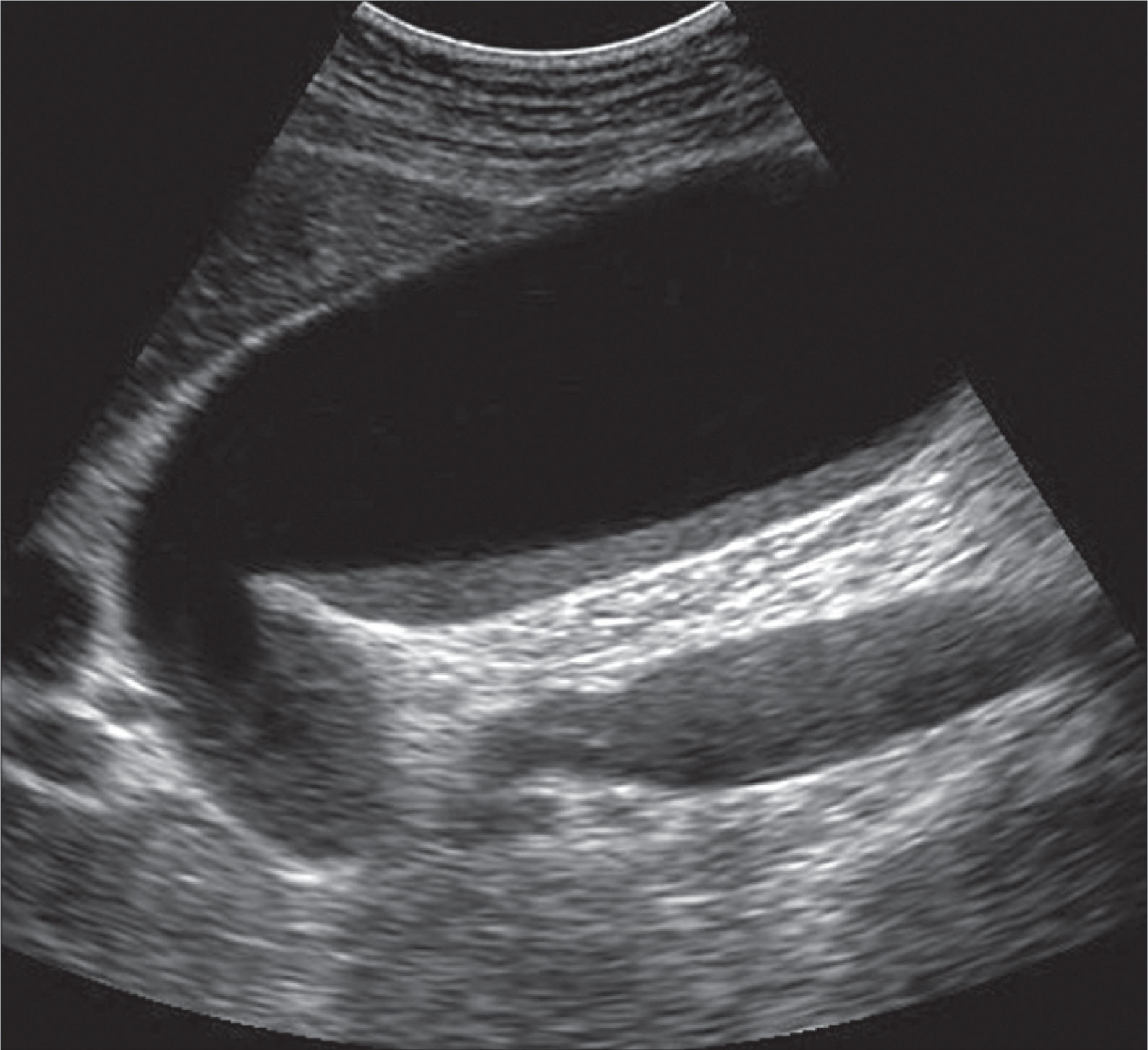
During the fasting state, very little bile flows into the duodenum. Stimulation produced by the influence of food causes the gallbladder to contract, resulting in an outpouring of bile into the duodenum. When the stomach is emptied, duodenal peristalsis diminishes, the gallbladder relaxes, the tonus of the sphincter of Oddi increases slightly, and thus very little bile passes into the duodenum. Small amounts of bile secreted by the liver are retained in the common duct and forced into the gallbladder. The contracted gallbladder appears on sonography as a thick-walled structure with a slit for the bile. It is nearly impossible to see luminal or wall abnormalities when the gallbladder is contracted.
When the gallbladder is removed, the sphincter of Oddi loses tonus, and pressure within the common bile duct drops to that of intraabdominal pressure. Bile is no longer retained in the bile ducts but is free to flow into the duodenum during fasting and digestive phases. Dilation of the extrahepatic bile ducts (usually less than 1 cm) occurs after cholecystectomy .
Secretion is largely caused by a bile salt–dependent mechanism, and ductal flow is controlled by secretion. Bile is the principal medium for excretion of bilirubin and cholesterol. The products of steroid hormones are also excreted in the bile, as are drugs and poisons (e.g., salts of heavy metals). The bile salts from the intestine stimulate the liver to make more bile. Bile salts activate intestinal and pancreatic enzymes.
Ultrasound examinations of the gallbladder and bile ducts are performed to determine cholelithiasis, changes secondary to acute and chronic cholecystitis, obstruction, and primary or metastatic tumor involvement. The examination is performed as part of a comprehensive general abdominal evaluation ( Table 10.1 ).
Patient preparation: NPO for at least 6 hours.
Transducer selection: broadband curvilinear or section probe 2.5 to 5 MHz.
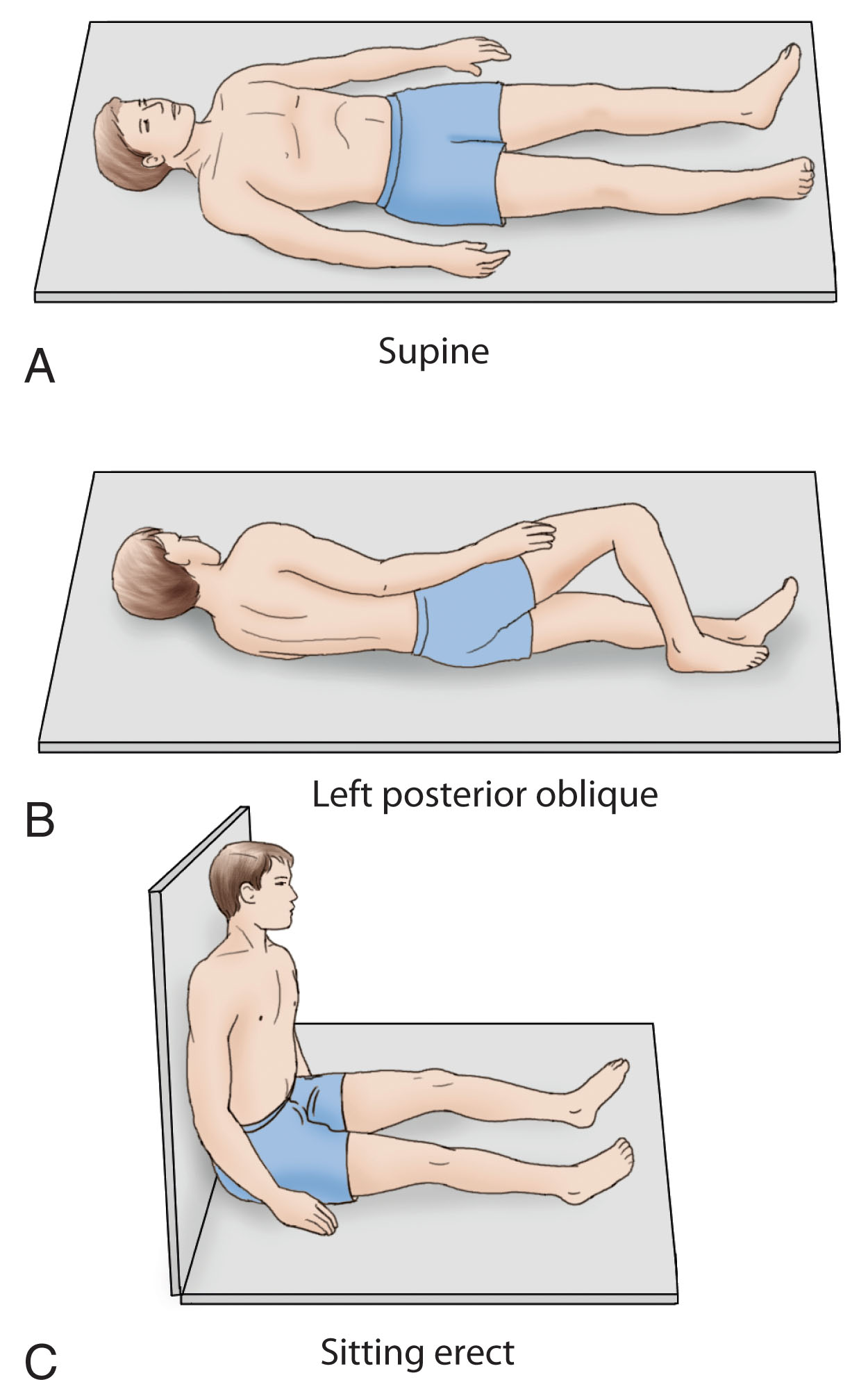
Patient position: Supine and decubitus (see Fig. 10.8 A–C ).
Images and observations should include the following ( Fig. 10.9 ):
The fundus, body, and neck should be surveyed.
Gallbladder wall thickness (normal is less than 3 mm) should be recorded. If thickened, the wall should be measured from the anterior wall to the posterior wall with the transducer perpendicular to the anterior wall.
The presence of echogenic foci (e.g., stones, polyps) within the gallbladder lumen should be evaluated. If echogenic foci are present, the sonographer should attempt to demonstrate acoustic shadowing and mobility with change in patient position.
The common bile duct should be imaged in at least the oblique long-axis plane as it lies anterior to the main portal vein (MPV) before coursing posterior to the head of the pancreas.
The transverse scan of the porta hepatis may help delineate the portal vein from the common duct (anterior and to the right) and hepatic artery (anterior and to the left).
Visualization of the intrahepatic ducts may be difficult unless dilation is present. Ductal dilation may be seen as the liver is scanned, demonstrating right and left branches of the portal vein as the hepatic ducts follow a parallel course.
To examine gallstones, the focal point of the transducer is placed at the region of the posterior gallbladder wall, and the gain reduced. This facilitates demonstration of acoustic shadowing.
| Organ | Scan Plane | Anatomy |
|---|---|---|
| GB (supine and LLD) | Long | Body/fundus |
| Trv | Body/neck (measure wall) Body/neck | |
| CBD | Trv | Portal triad |
| Long | Measure duct |
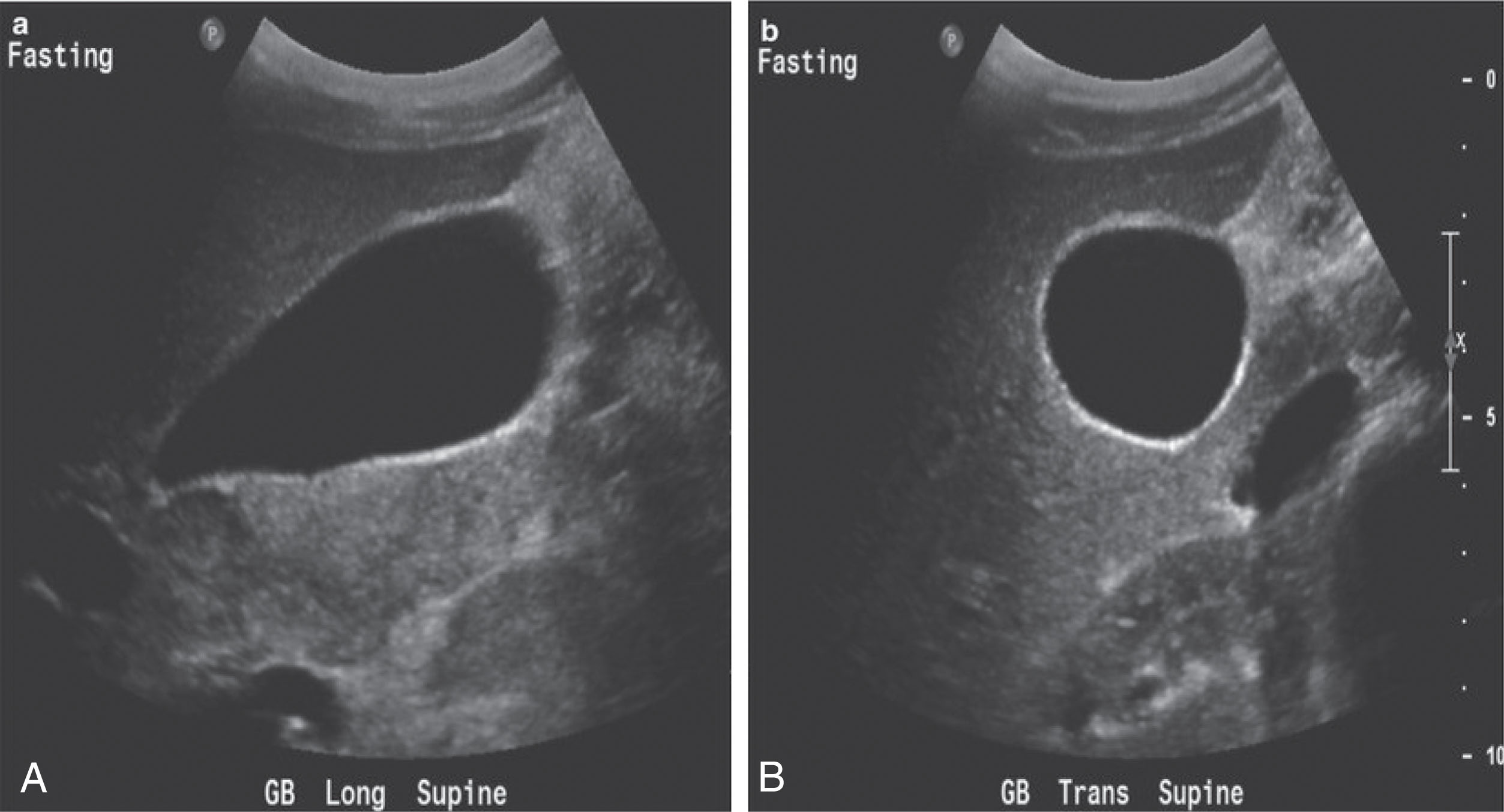
To ensure maximum dilation of the gallbladder, the patient should be given nothing to eat for at least 6 hours prior to the ultrasound examination. The patient is initially examined in the supine position in full inspiration. Transverse, sagittal, and oblique scans are made over the upper abdomen to identify the gallbladder, biliary system, liver, right kidney, and head of the pancreas. The oblique scans are made with the transducer in the subcostal position with a slight cephalic angulation. The probe sweep is aligned between the right shoulder and left hip of the patient. If stones or polyps are suspected, the patient should also be rolled into a steep decubitus or upright position (to ensure there are no stones within the gallbladder) in an attempt to separate small stones from the gallbladder wall or cystic duct ( Fig. 10.10 ).
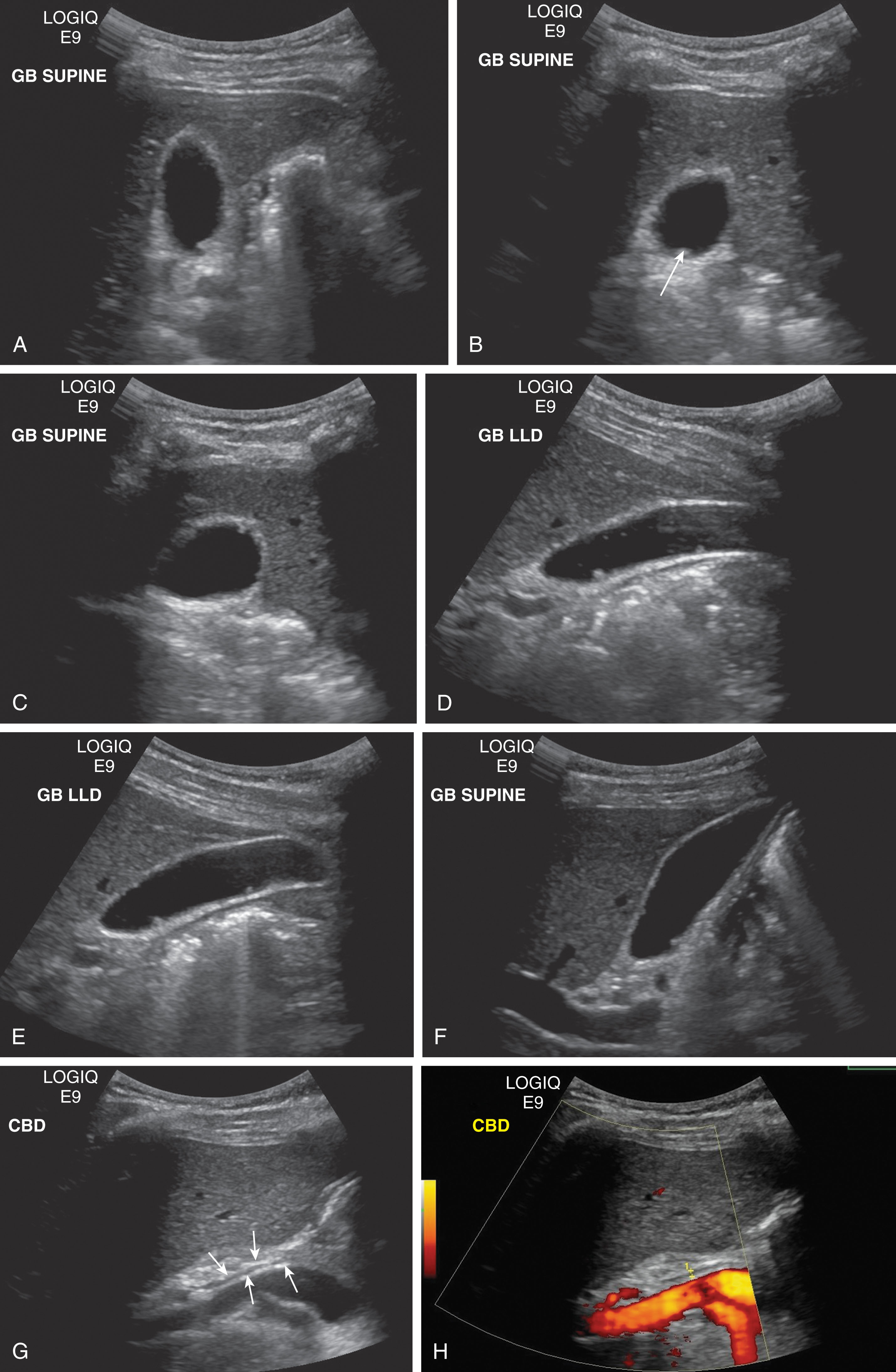
The gallbladder may be identified as a sonolucent oblong structure located anterior to the right kidney, lateral to the head of the pancreas and duodenum. The gallbladder fossa causes a slight indentation on the posterior surface of the medial aspect of the right lobe of the liver. The sagittal scans may show the right kidney posterior to the gallbladder when the probe is angled toward the right hip. The fundus is generally oriented slightly more anterior and, on sagittal scans, often reaches the anterior abdominal wall. Box 10.1 lists the sonographic characteristics of the normal gallbladder.
Size: ≤4 cm transverse; ≤10 cm longitudinal
Wall thickness: <3 mm
Lumen: anechoic
Landmarks: right upper quadrant, between right and left lobes of liver, right kidney, main lobar fissure, and portal vein
The middle hepatic vein lies in the same anatomic plane and may prove to be a useful landmark in locating the gallbladder. A sweep from cephalad to caudad shows the interlobar fissure (a structure that separates the right and left hepatic lobes) as a bright linear echo within the liver connecting the gallbladder fossa and the right portal vein. The neck of the gallbladder usually comes into contact with the main segment of the portal vein near the origin of the left portal vein. The gallbladder commonly resides in a fossa on the medial aspect of the liver. Because of fat or fibrous tissue within the main lobar fissure of the liver (which lies between the gallbladder and the right portal vein), this bright linear reflector is a reliable indicator of the location of the gallbladder. The gallbladder lies in the posterior and caudal aspect of the fissure. The caudal aspect of the linear echo “points” directly to the gallbladder. If the gallbladder has been removed, the fossa appears as an echogenic line as a result of the remaining connective tissues.
A small echogenic fold has been reported to occur along the posterior wall of the gallbladder at the junction of the body/neck. It may be very small (3 to 5 mm) but may give rise to an acoustic shadow in the supine position. It is not duplicated in the oblique position. The cause for such a junctional fold is the indentation between the body/neck or Heister valve, a spiral fold beginning in the neck of the gallbladder and lining the cystic duct (see Fig. 10.6 ).
A prominent gallbladder may be normal in some individuals secondary to their fasting state ( Fig. 10.11 ). A large gallbladder has also been detected in patients with diabetes, patients bedridden with protracted illness or pancreatitis, and patients taking anticholinergic drugs. A large gallbladder may even fail to contract after a fatty meal or intravenous cholecystokinin; other studies may be needed before making a diagnosis of obstruction.
If a gallbladder appears abnormally enlarged, a fatty meal may be administered and further sonographic evaluation made to detect whether the enlargement is abnormal or normal. If the gallbladder fails to contract during the examination, the pancreatic area should be investigated further. Courvoisier sign indicates an extrahepatic mass compressing the common bile duct, which can produce an enlarged gallbladder ( Fig. 10.12 ). In addition, the liver should be carefully examined for the presence of dilated bile ducts.
In a well-contracted gallbladder, the wall changes from a single to a double concentric structure with the following three components: (1) a strongly reflective outer contour, (2) a poorly reflective inner contour, and (3) a sonolucent area between both reflecting structures.
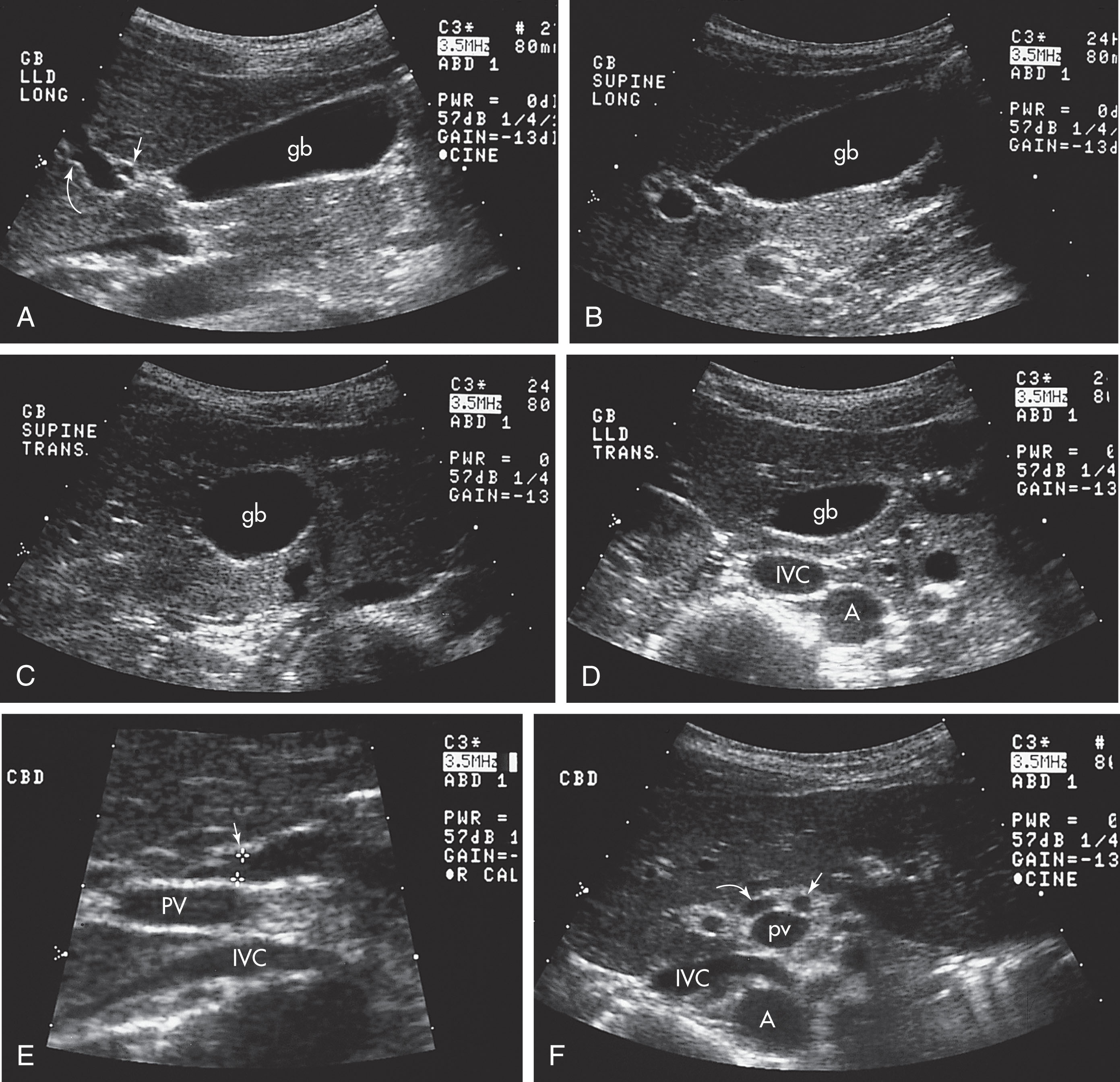
Sonographically, the common duct lies anterior and to the right of the portal vein in the region of the porta hepatis and gastrohepatic ligament. The hepatic artery lies anterior and to the left of the portal vein. On a transverse scan, the common duct, hepatic artery, and portal vein have been referred to as the portal triad or “Mickey Mouse sign” ( Fig. 10.13 ). The portal vein serves as Mickey’s face, with the lateral ear the common duct and the medial ear the hepatic artery. To obtain such a cross-section, the transducer must be directed in a slightly oblique path from the left shoulder to the right hip.
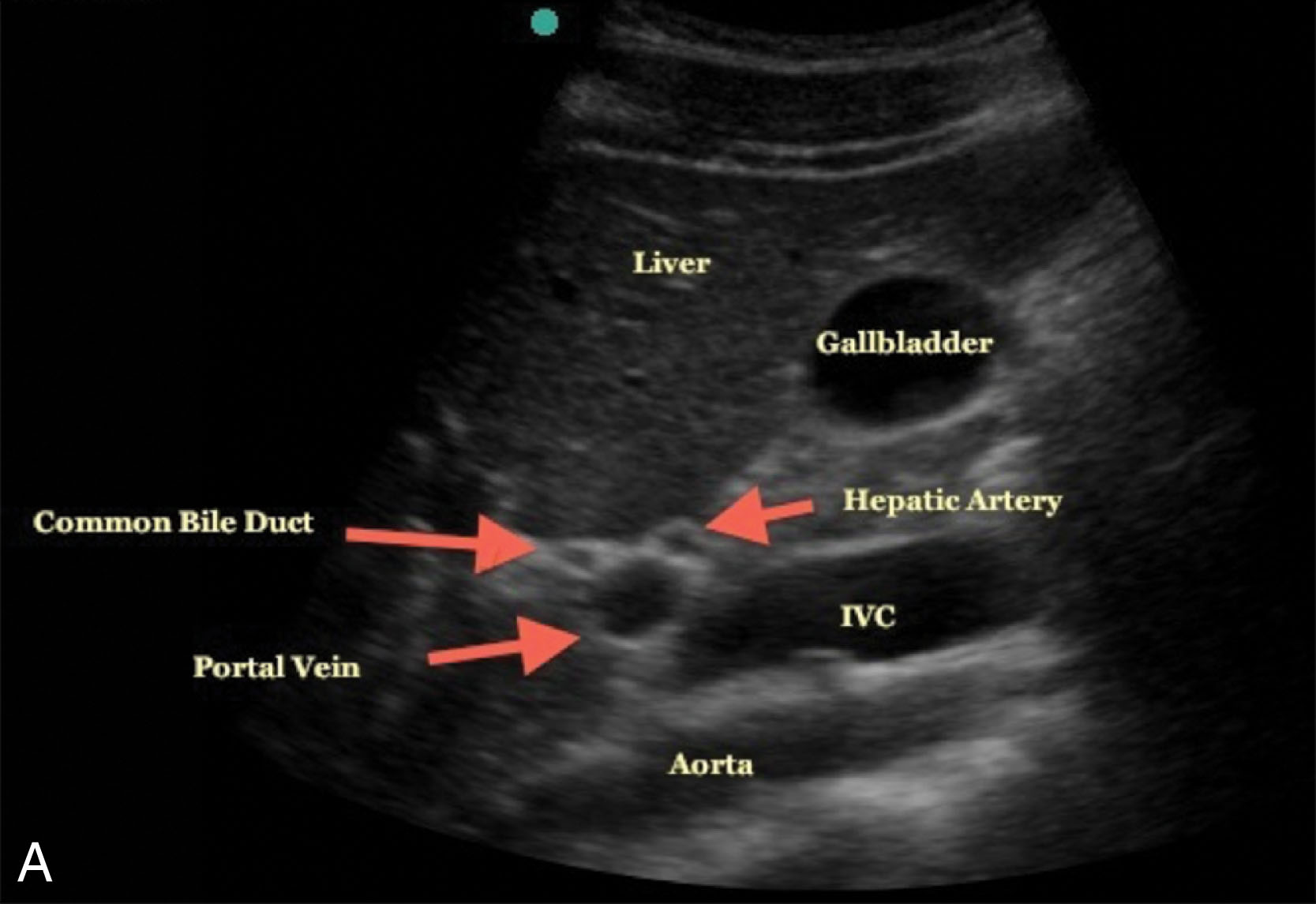
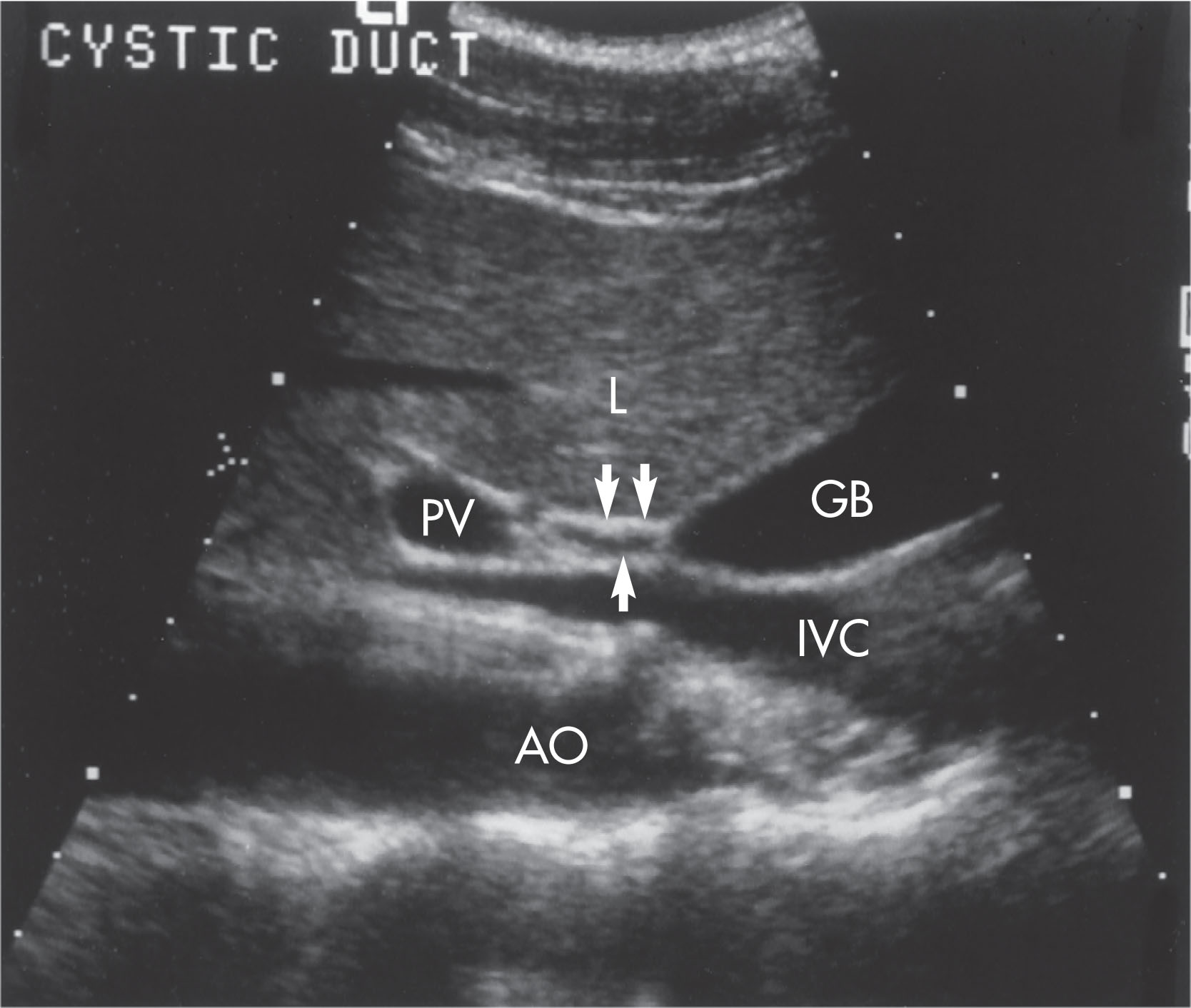
On sagittal scans, the right branch of the hepatic artery usually passes anterior to the common duct ( Figs. 10.14 and 10.15 ). The common duct is seen just anterior to the portal vein before it dips posteriorly to enter the head of the pancreas. The patient may be rotated into a slight (45-degree) or steep (90-degree) right anterior oblique position, with the beam directed posteromedially to visualize the duct. This enables the examiner to avoid cumbersome bowel gas and to use the liver as an acoustic window.
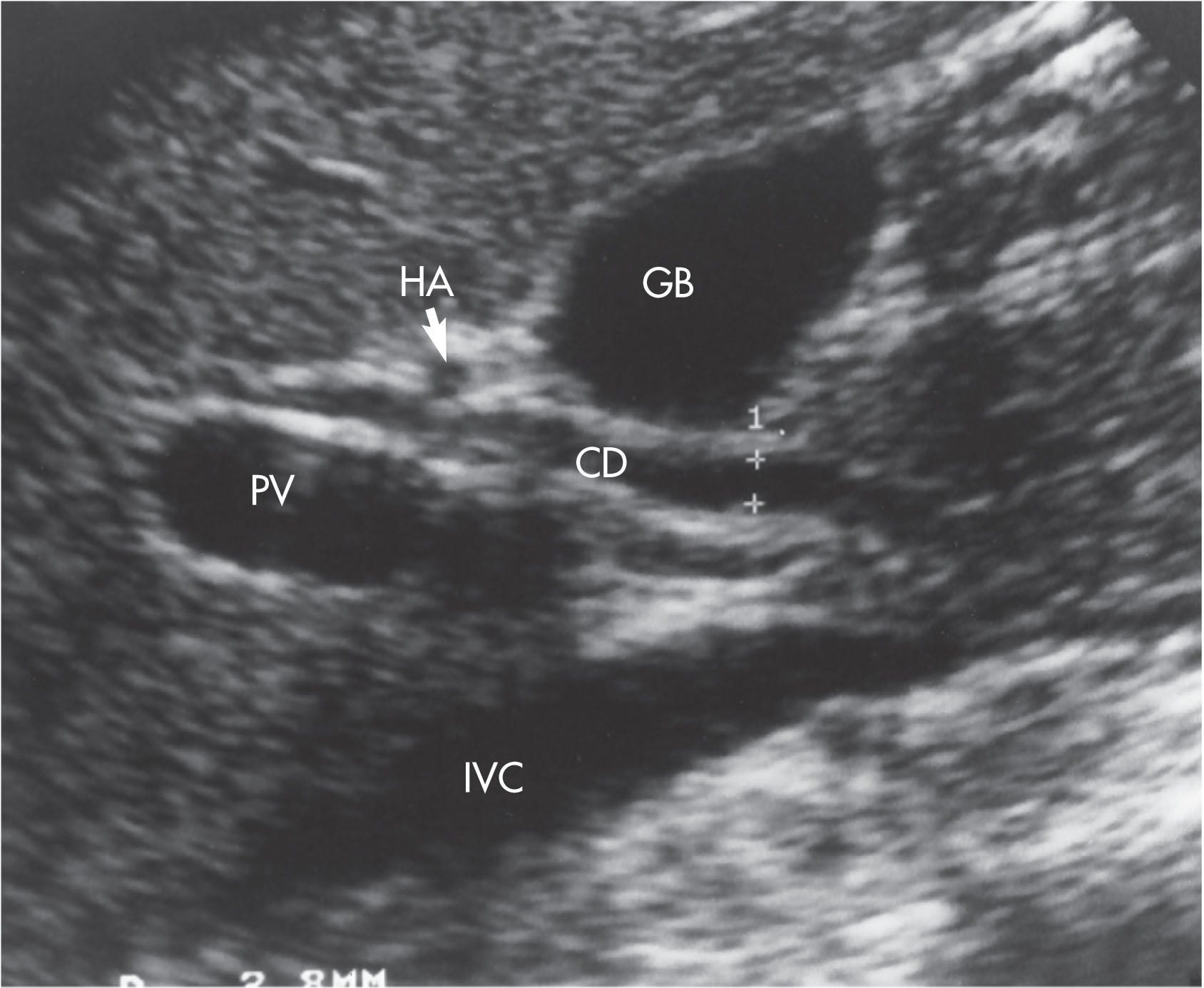
When the right subcostal approach is used, the main portal vein may be seen as it bifurcates into the right and left branches. As the right branch continues into the right lobe of the liver, it can be followed laterally in a longitudinal plane. The portal vein appears as an almond-shaped sonolucent structure anterior to the inferior vena cava. The common hepatic duct is seen as a tubular structure anterior to the portal vein. The right branch of the hepatic artery can be seen between the duct and the portal vein as a small circular structure.
The small cystic duct is generally not identified. Because this landmark is necessary to distinguish the common hepatic duct from the common bile duct, the more general term common duct is used to refer to these structures ( Fig. 10.16 ).
See Table 10.2 for clinical findings, sonographic findings, and differential considerations for gallbladder and biliary diseases and conditions.
| Clinical Findings | Sonographic Findings | Differential Considerations | |
|---|---|---|---|
| Sludge | |||
| May be asymptomatic |
|
|
|
| Acute Cholecystitis | |||
|
|
|
|
| Chronic Cholecystitis | |||
|
|
|
|
| Acalculous Cholecystitis | |||
|
|
|
|
| Emphysematous Cholecystitis | |||
|
|
|
|
| Gangrenous Cholecystitis | |||
| Abnormal LFTs |
|
GB carcinoma | |
| Cholelithiasis | |||
|
|
|
|
| Choledochal Cysts | |||
|
4.Dilated CBD and CHD |
|
|
| Adenoma of the Gallbladder | |||
| Occurs as flat elevations located in the body of the GB, almost always near the fundusDoes not change with positionNo shadow produced | Adenomyomatosis | ||
| Adenomyomatosis of the Gallbladder | |||
|
Adenoma | ||
| Porcelain Gallbladder | |||
|
GB wall thickly calcified with shadowing | Gallstones with emphysematous cholecystitis | |
| Choledocholithiasis | |||
|
|
|
|
The most classic symptom of gallbladder disease is right upper quadrant abdominal pain, usually occurring after ingestion of greasy foods. Nausea and vomiting sometimes occur and may indicate the presence of a stone in the common bile duct. A gallbladder attack may cause referred pain to the right shoulder, with inflammation of the gallbladder often causing referred pain in the right shoulder blade.
Jaundice is characterized by the presence of bile in the tissues with resulting yellow-green color of the skin. It may develop when a tiny gallstone blocks the bile ducts between the gallbladder and the intestines, producing pressure on the liver and forcing bile into the blood.
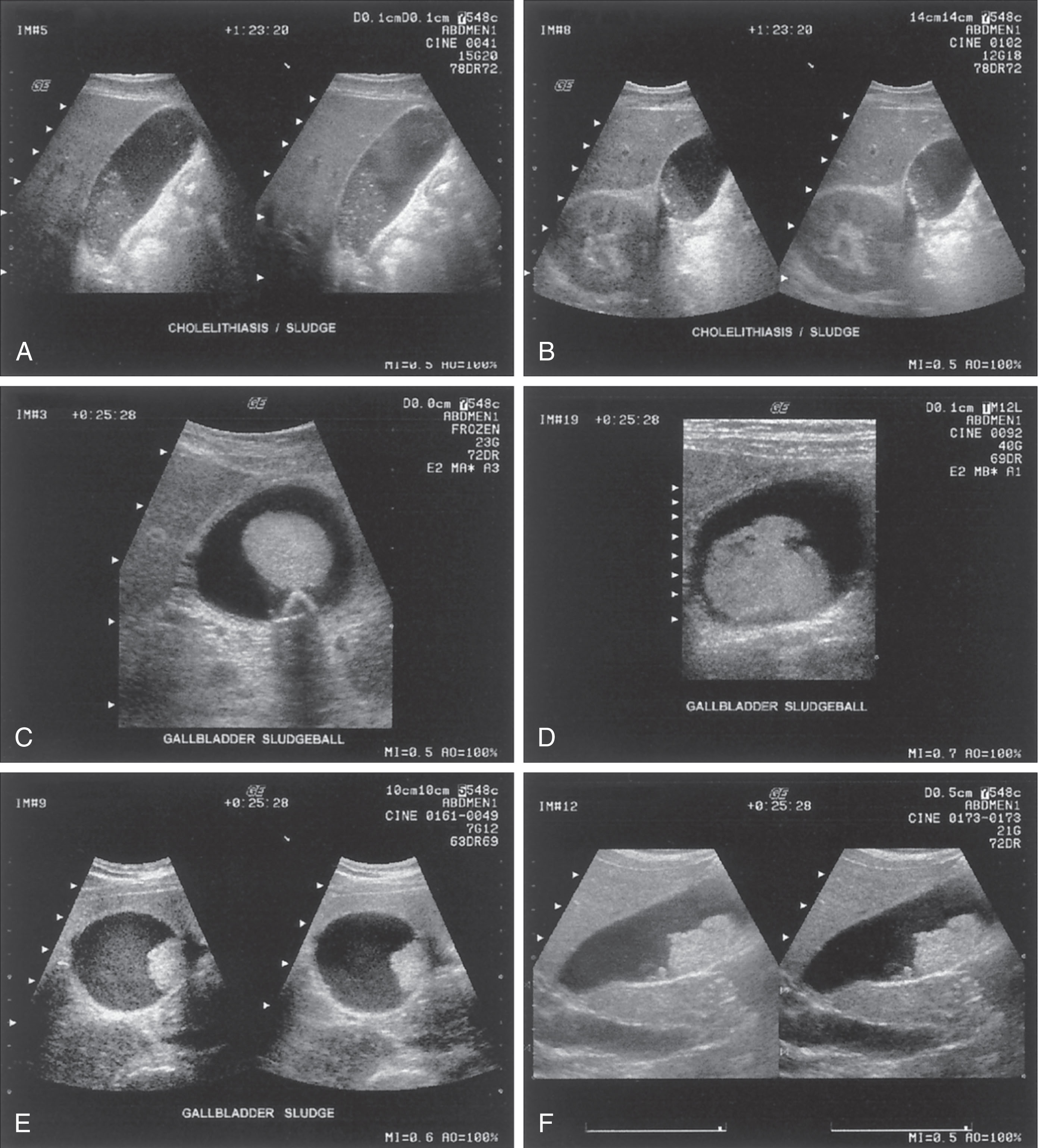
Sludge , or thickened bile, frequently occurs from bile stasis. Sludge may be seen in patients with prolonged fasting, hyperalimentation therapy, or with obstruction of the gallbladder. Some gallbladders may be so packed with this thickened bile that the gallbladder is isoechoic and difficult to distinguish from the liver parenchyma. Occasionally sludge is also found in the common duct. Sludge is gravity dependent; therefore with alterations in the patient’s position, the sonographer may be able to separate sludge from occasional artifactual echoes found in the gallbladder. Sludge will slowly resettle as the patient changes their position. Sludge should be considered an abnormal finding because either a functional or a pathologic abnormality exists when calcium bilirubin or cholesterol precipitates in bile. Complications of biliary sludge are stone formation, biliary colic, acalculous cholecystitis, and pancreatitis.
Occasionally a patient presents sonographically with a prominent gallbladder containing amorphous, low-level internal echoes without acoustic shadowing, which may be attributed to thick or inspissated bile. The source of echoes in biliary sludge is thought to be particulate matter (predominantly pigment granules with lesser amounts of cholesterol crystals). The viscosity does not appear to be important in the generation of internal echoes in fluids. The particles can be small and still produce perceptible echoes ( Fig. 10.17 ). Sludge may mimic polypoid tumors (tumefactive sludge). Sludge will not present with gallbladder wall thickening or internal vascularity as tumor would. Sludge may also be seen in combination with cholelithiasis, cholecystitis, and other biliary diseases.
The normal wall thickness of the gallbladder is less than 3 mm. Biliary causes of gallbladder wall thickening include cholecystitis, adenomyomatosis, cancer, acquired immunodeficiency syndrome, cholangiopathy, severe hypoalbuminemic state, and sclerosing cholangitis ( Box 10.2 ). Nonbiliary causes include diffuse liver disease (cirrhosis and hepatitis), pancreatitis, portal hypertension, and heart failure. A thickened wall is a nonspecific sign and is not necessarily related to gallbladder disease.
The gallbladder wall thickness should be measured when the transducer is perpendicular to the anterior gallbladder wall. This is usually done in the transverse plane, but in some cases, the longitudinal plane allows a better alignment. The gain should be reduced and the focal zone aligned to the gallbladder area to clearly demarcate the anterior wall. The anterior wall is measured from outer to outer margins. Sonographically the gallbladder wall may be underestimated when the wall has extensive fibrosis or is surrounded by fat ( Fig. 10.18 ).
Cholecystitis is an inflammation of the gallbladder that may have one of several forms: acute or chronic, acalculous, emphysematous, or gangrenous ( Box 10.3 ).
Thickened gallbladder wall >3 mm
Distended gallbladder lumen >4 cm
Gallstones
Impacted stone in Hartmann’s pouch or cystic duct
Positive Murphy sign
Increased color Doppler flow
Pericholecystic fluid collection
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here