Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter discusses the management of coronary artery anomalies in patients without other congenital heart defects. Most coronary artery anomalies in number, origin, and distribution are of intellectual interest only. However, a few are clinically significant because they may result in myocardial ischemia, left ventricular dysfunction, and sudden death. Anomalies discussed in this chapter include anomalous origin of a coronary artery from the pulmonary artery, anomalous coronary artery that courses between the aorta and pulmonary artery, coronary artery fistula, and congenital atresia of the left main coronary artery.
In normal coronary anatomy, two coronary arteries arise from separate ostia in the right and left aortic sinuses of Valsalva. The left main coronary artery (LMCA) originates from the left aortic sinus and usually bifurcates into the left anterior descending coronary artery (LAD) and the left circumflex coronary artery. The LAD runs in the anterior interventricular groove, and the left circumflex coronary artery courses in the left atrioventricular groove. The right coronary artery (RCA) originates anteriorly from the right aortic sinus, runs along the right atrioventricular groove, and usually gives rise to the posterior descending artery at its terminus.
In most individuals, each coronary artery ostium is located centrally in the appropriate sinus of Valsalva. In some patients, the ostium may be eccentrically located, and in others a coronary artery may arise close to a valve commissure. One or both coronary ostia may arise from the tubular aorta above the sinotubular junction, which is usually a benign finding. However, this high take-off of the coronary artery becomes significant if an aortotomy is necessary for aortic valve replacement or for another indication; if not recognized, the coronary artery could be transected. Another anomaly is when both coronary arteries arise from the same aortic sinus with either a single ostium or two separate ostia ( Box 124-1 ). This is generally not clinically significant if the aberrant vessel courses posterior to the aorta or anterior to the pulmonary artery, but it becomes important if either the aberrant LMCA or RCA courses between the two great vessels, because this may lead to myocardial ischemia and sudden death.
Left main coronary artery originates from right sinus of Valsalva (either from right coronary artery or separate ostia).
Left main coronary artery courses anterior to pulmonary artery.
Left main coronary artery courses through interventricular septum.
Left main coronary artery courses between aorta and pulmonary artery.
Left main coronary artery courses posterior to aorta.
In rare cases, the left anterior descending coronary or left circumflex coronary artery alone may originate from the right sinus.
Single left main coronary artery arises from the left sinus and bifurcates into the left anterior descending coronary and left circumflex coronary arteries. The left circumflex coronary artery crosses the crux and continues as the right coronary artery.
Single right coronary artery from sinus, which crosses crux, continues as left anterior descending coronary and left circumflex coronary artery.
Right coronary artery originates from left sinus of Valsalva (either from left main coronary artery or as separate ostium).
Right coronary artery courses posterior to aorta.
Right coronary artery courses interior anterior to pulmonary artery.
Right coronary artery courses between aorta and pulmonary artery.
Anomalous origin of a coronary artery from the pulmonary artery is a rare congenital anomaly that is almost always fatal if not diagnosed and treated. Although anomalous origin of the LMCA from the pulmonary artery (ALCAPA) is the most common, other coronary arteries may rarely also arise from the pulmonary artery. The RCA arises from the pulmonary artery approximately 10 times less frequently than ALCAPA but is also associated with ischemia and sudden cardiac death. The LAD, the circumflex, or both the left and right coronary arteries may arise from the pulmonary artery; these variants are extremely rare and are almost uniformly fatal.
ALCAPA is the most important congenital coronary artery anomaly in this class. The incidence of ALCAPA ranges from 1 in 30,000 to 1 in 300,000 people. It is the most common cause of myocardial infarction in childhood. If not diagnosed and treated, the mortality rate is 90% by age 1 year. ALCAPA is otherwise known as the Bland-White-Garland syndrome, after Bland and colleagues reported on both clinical and autopsy findings in an infant with this anomaly in 1933.
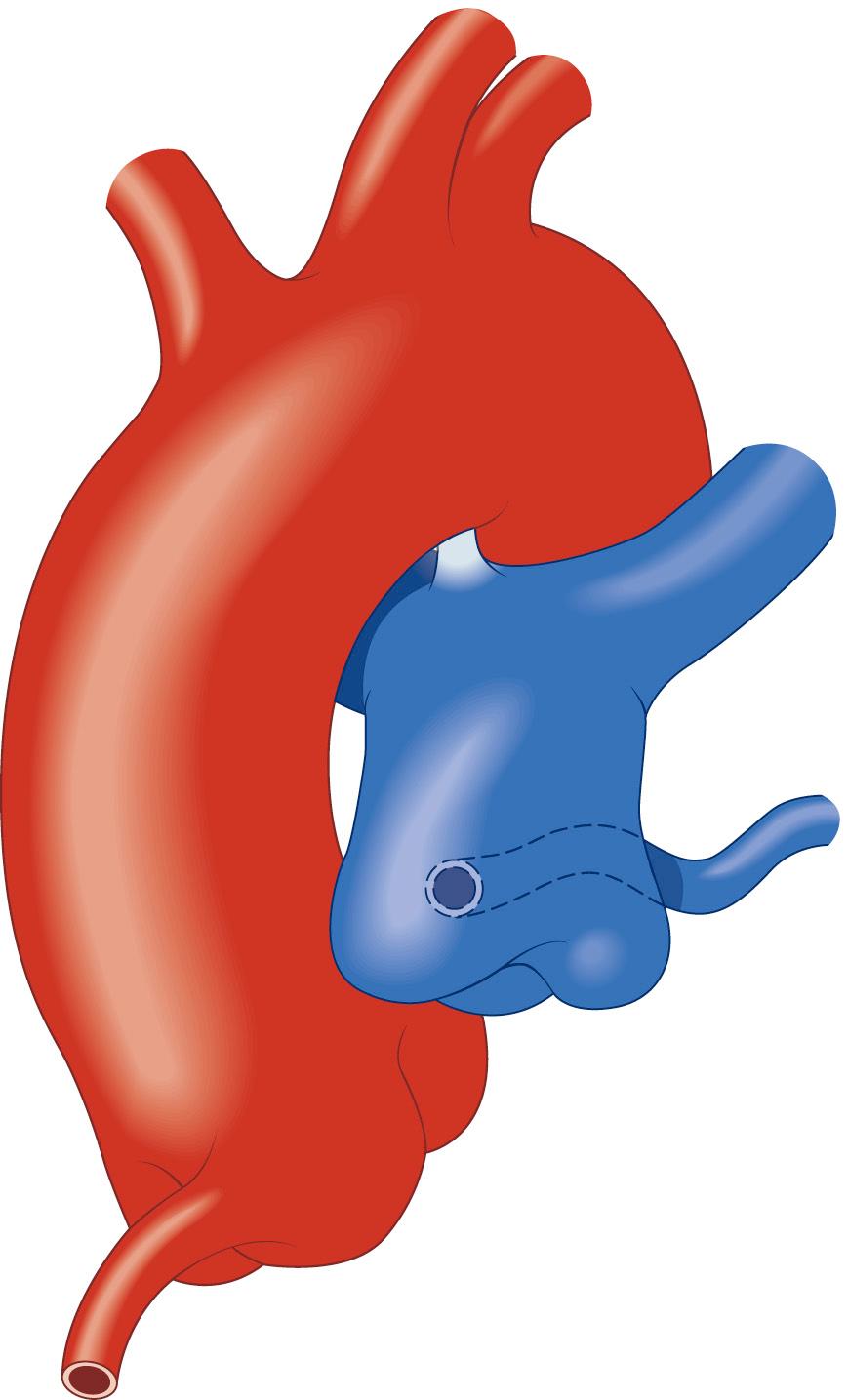
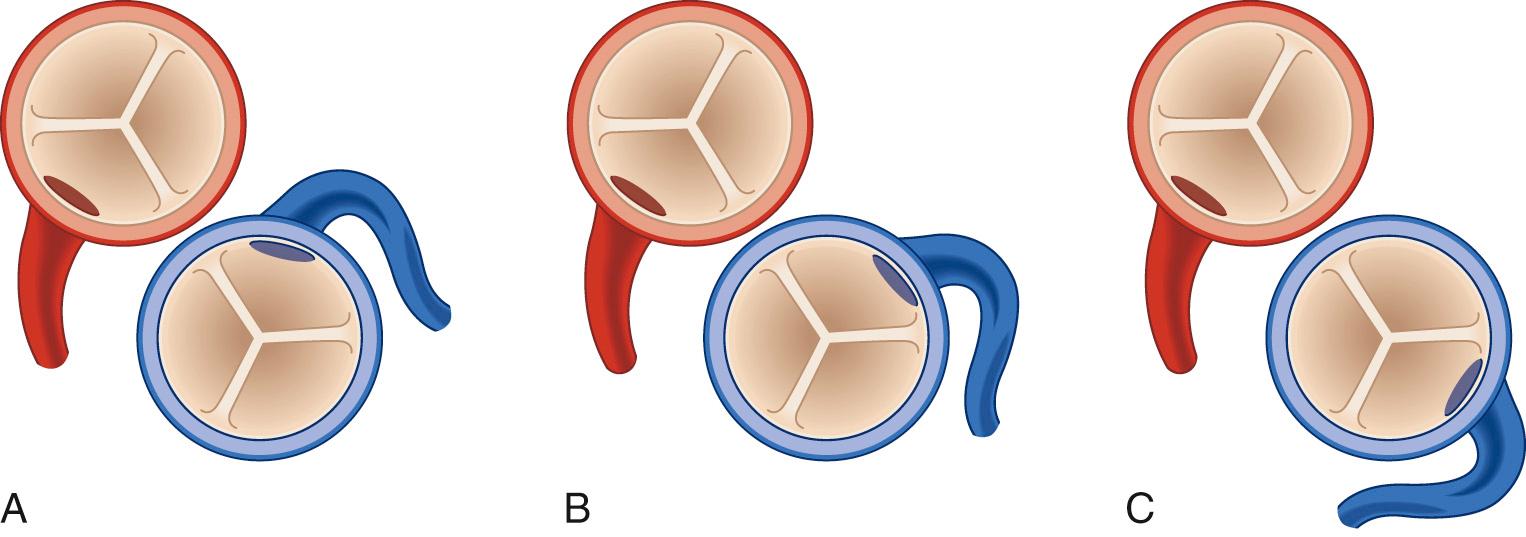
In ALCAPA, the LMCA usually arises from the main pulmonary artery (MPA); occasionally, it arises from the right pulmonary artery. It usually originates from the rightward aspect of the posterior (facing) sinus of the MPA ( Figs. 124-1 and 124-2 ), but it may also originate from the leftward aspect of the posterior (facing) and, in rare cases, from the anterior (nonfacing) sinus of the MPA (see Fig. 124-2 ). An anomalous RCA most commonly originates from the anterior portion of the pulmonary artery.
Although ALCAPA usually occurs in isolation, other associated cardiac defects include patent ductus arteriosus (PDA), ventricular septal defect (VSD), coarctation of the aorta, and tetralogy of Fallot.
Children with ALCAPA usually develop symptoms after closure of the ductus arteriosus and the subsequent fall in pulmonary vascular resistance. During fetal life, the systemic and pulmonary circulation pressures are similar, and myocardial perfusion remains intact because the pulmonary arterial pressure is systemic. After birth but before ductal closure, the pulmonary artery pressure remains elevated, thereby maintaining perfusion of the anomalous coronary artery. This explains why children are rarely diagnosed with ALCAPA in the first few days of life. The clinical course after ductal closure is largely determined by the presence or absence of collaterals from the RCA to the left coronary system. If there is inadequate collateral circulation, myocardial ischemia and ventricular dysfunction result from insufficient myocardial perfusion. This occurs because of subsystemic pulmonary artery pressure, and the left ventricle is thus perfused with desaturated blood at a low pressure. However, if the pulmonary artery pressure remains elevated because of the presence of another cardiac defect, such as PDA or VSD, left ventricular perfusion pressure may be adequate to prevent ischemia. If this coronary anomaly is unknown before the catheter or surgical closure of these defects, it will become apparent shortly after closure because of the subsequent drop in pulmonary arterial pressure—usually with a fatal outcome.
Alternatively, if there is adequate collateralization, perfusion of the left coronary system is maintained. As the pulmonary vascular resistance falls, however, a left-to-right shunt develops from the RCA to the pulmonary artery. There is progressive dilation of the RCA and left coronary artery systems, with reversal of flow in the left coronary leading to a pulmonary-coronary steal. Although the shunt is relatively small compared with overall cardiac output, it is significant with regard to coronary blood flow. Children with extensive collaterals may survive past infancy; however, there is usually progressive left ventricular dysfunction. In a small percentage of cases, the collateral vessels are enough to maintain adequate myocardial perfusion at rest and sometimes even during exertion, and these patients may not come to clinical attention until adulthood. In most children, however, severe mitral regurgitation is present secondary to papillary muscle dysfunction and ventricular dilation.
Infants frequently present between 4 and 6 weeks of age after the pulmonary vascular resistance has dropped. However, infants may not be diagnosed until 2 to 3 months of age, when symptoms have increased in severity. Infants usually show signs and symptoms of congestive heart failure, including sweating and discomfort with feeding, tachypnea, poor weight gain, and pallor. The discomfort with feeding most likely represents myocardial ischemia. Children who do not present when they are infants may be diagnosed in later infancy as a result of the loud murmur of mitral regurgitation. Older children, adolescents, and adults may remain asymptomatic, whereas others may come to clinical attention because of exertional chest pain, pre-syncope, or syncope. There have been reports of sudden death with exercise in these older patients. The symptoms associated with anomalous origin of the RCA from the pulmonary artery are less severe, but myocardial ischemia and death can still occur.
Physical examination of the infant with ALCAPA may reveal signs of congestive heart failure, including tachypnea, tachycardia, and hepatomegaly. Left ventricular dysfunction caused by ALCAPA can be difficult to distinguish from a dilated cardiomyopathy. The left heart is usually enlarged, often with associated mitral regurgitation, and a gallop rhythm also may be present. If left heart failure has resulted in pulmonary hypertension, then there may also be evidence of right heart enlargement and an accentuated pulmonary component of the second heart sound on examination.
Infants with ALCAPA generally have an enlarged cardiac silhouette on chest radiograph, resulting mainly from the enlarged left atrium and left ventricle. In infants with congestive heart failure, the electrocardiogram (ECG) can provide a useful diagnostic clue because there are classic findings of Q waves and ST-segment elevation in leads I, aVL, and V4-V6 as a result of lateral or anterolateral wall infarction. Although this pattern can be found in other causes of myocardial infarction or cardiomyopathy, if these electrocardiographic abnormalities are seen in an infant with congestive heart failure, the diagnosis of ALCAPA needs to be strongly considered. Certainly, any infant diagnosed with dilated cardiomyopathy must be extensively evaluated for ALCAPA. This diagnosis should also be considered in older children and adolescents with a dilated cardiomyopathy, because occasional patients survive past infancy.
Echocardiography with color flow Doppler usually demonstrates a dilated left ventricle with severe mitral regurgitation. The mitral regurgitation commonly seen with ALCAPA is caused by infarction of the posterior leaflet of the mitral valve and subsequent poor movement of the leaflet; fibrosis and fibroelastosis of the papillary muscle also can be present. Imaging of the coronary arteries, including origin and course, has become possible as a result of improved echocardiographic techniques, but it can still be challenging. An enlarged RCA is almost always present and should raise suspicion of this diagnosis. Careful attention should be paid to the origins of both coronary arteries, including the abnormal origin of the LMCA to the pulmonary artery. If visualization of the anomalous vessel is unclear, color flow Doppler may reveal retrograde flow from the coronary artery to the pulmonary artery. However, underdiagnosis by echocardiography is relatively common; thus, if any question remains about visualization of both coronary ostia, then cardiac catheterization is mandatory to rule out ALCAPA.
Cardiac catheterization with angiography remains the gold standard in the diagnosis of ALCAPA. Cardiac catheterization demonstrates elevated filling and pulmonary arterial pressures and a low cardiac output. In older asymptomatic patients, it may show only mildly elevated pulmonary arterial pressures but normal filling pressures and cardiac output. A small left-to-right shunt may be present. An aortogram will demonstrate a single, dilated RCA arising normally from the aorta. If significant collaterals are present, aortic root angiography will show the collaterals providing late, retrograde filling of the left coronary artery with a blush of contrast subsequently filling the MPA. If there is a large left-to-right shunt from the collaterals, a step-up in oxygen saturation may be noted in the MPA. If doubt remains regarding the diagnosis, a main pulmonary arteriogram with distal balloon occlusion should demonstrate the anomalous left coronary artery.
Magnetic resonance imaging (MRI) has emerged as a useful noninvasive diagnostic tool for delineating congenital coronary anomalies. Although there have been case reports of using this method in diagnosing ALCAPA, no case series with this anomaly have been reported. However, studies have shown that magnetic resonance angiography has a similar sensitivity and specificity when compared with coronary angiography and may be especially helpful in delineating the proximal course of anomalous coronary arteries. Computed tomography (CT) has been used extensively for coronary artery delineation in adults. Advantages of this technique include rapid acquisition time and high resolution, but the disadvantages include radiation exposure and the need for a slower heart rate with ECG gating, precluding its use in infants.
Surgical repair is indicated in all patients with ALCAPA. In infants with congestive heart failure, surgery should occur within the first few days of diagnosis because risk of continuing myocardial ischemia and death is very high. In older patients who present without symptoms, surgery is necessary but can be performed electively. In an infant who presents in severe heart failure secondary to myocardial infarction, surgery will probably need to be delayed for at least 24 hours to stabilize the patient using mechanical ventilation, inotropic support, and vasodilators, when necessary. Del Nido and colleagues reported that even in the sickest infants, a two-vessel surgical repair is possible if left ventricular assist devices (LVADs) are used postoperatively. Others may need extracorporeal membrane oxygenation (ECMO). Because infants requiring surgery are often quite ill, it is important that centers performing ALCAPA surgery have these options available, or else the child should be transferred to a hospital with these capabilities.
The goal of surgery is restoration of a two-coronary system; therefore, simple ligation of the anomalous coronary should not be performed. Severe left ventricular dysfunction and mitral insufficiency are not contraindications to revascularization in infants, because significant recovery of function usually occurs. Because the severity of mitral regurgitation almost always decreases after revascularization, left ventricular aneurysmectomy and mitral valve repair or replacement are rarely indicated at the time of initial procedure, even if severe mitral regurgitation is present.
The first successful operation for correction of ALCAPA was simple ligation of the anomalous artery at the pulmonary artery. Ligating the anomalous vessel prevents the left-to-right shunt, thereby allowing perfusion of the left ventricle through collaterals from the RCA. Because of the early mortality rates and increased risk of late sudden death with this procedure, a variety of techniques have been developed to create a dual coronary artery system, including coronary artery bypass grafting, aortopulmonary window, and direct reimplantation.
Bypass grafts were accomplished using the left subclavian artery, the internal mammary artery (IMA), and the saphenous vein. Meyer and colleagues reported the first successful left subclavian artery–to–left coronary artery bypass in 1968. The results of bypass grafting, especially with saphenous vein grafts, have been disappointing. Takeuchi and associates were the first to describe the creation of an aortopulmonary window and intrapulmonary artery baffle using a pulmonary artery flap to direct blood flow from the aorta to the anomalous coronary artery. Finally, the procedure of choice in many institutions has become direct reimplantation of the anomalous coronary onto the aorta, as experience with the arterial switch operation for transposition of the great vessels has increased.
Coronary artery bypass grafting is rarely used in patients with ALCAPA. In the current era, it is usually used to create a dual coronary artery system after previous ligation or because of stenosis or occlusion after a previous attempt at repair. The IMA is the conduit of choice and can be used successfully, even in neonates and infants; in addition, there is some evidence for growth of the IMA after bypass grafting. The saphenous vein should not be used unless it is the only conduit available, because of the risk of occlusion and poor long-term results. Similarly, left subclavian–to–left coronary artery anastomosis is infrequently used because of the risk of anastomotic stenosis or occlusion.
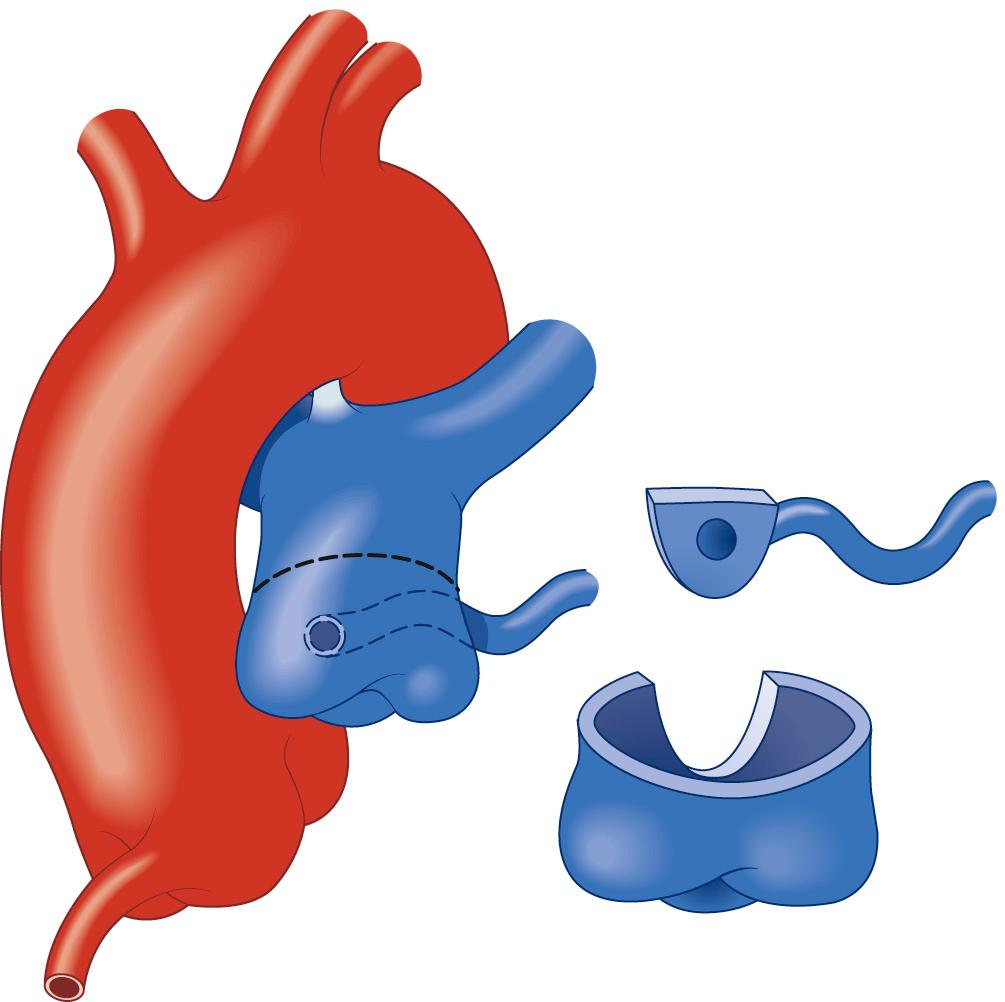
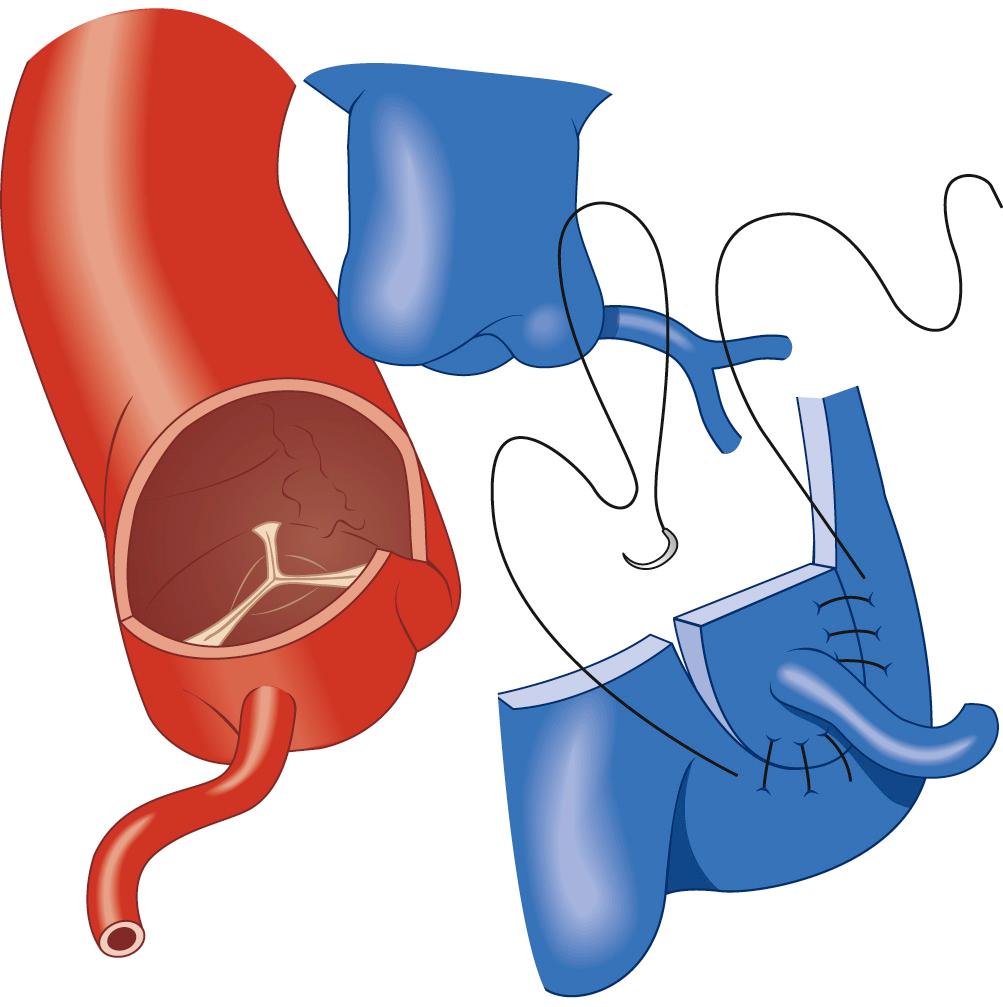
In most patients with ALCAPA, direct reimplantation of the anomalous coronary artery onto the aorta can be performed ( Fig. 124-3 ). When the anomalous coronary ostium is in the posterior-facing sinus, the procedure is fairly straightforward. Direct implantation is possible even if the ostium is located in the nonfacing sinus by excising a large button of pulmonary artery to extend the coronary artery.
After induction of anesthesia and placement of monitoring lines, a median sternotomy is performed. The thymus is resected. The pericardium is opened and suspended in stay sutures. Because of the likelihood of myocardial ischemia and left ventricular dysfunction, there is a risk of ventricular fibrillation, so contact with the myocardium should be kept at a minimum until the patient is placed on cardiopulmonary bypass. This operation may be performed using either continuous low-flow bypass with moderate hypothermia (25° to 28° C) or deep hypothermic circulatory arrest (18° C) in very small infants. Before cannulation, an aortic purse-string suture is placed distally near the innominate artery, and another is placed in the right atrial appendage for a single venous cannula. Heparin is administered, the aortic and right atrial cannulas are inserted, and cardiopulmonary bypass is established. The left ventricle should be decompressed by placing a left ventricular vent via the right superior pulmonary vein. The pulmonary artery and epicardial course of the left coronary artery are visualized. If the anomalous left coronary artery originates far leftward in the posterior-facing sinus or on the anterior nonfacing sinus, direct reimplantation may not be possible.
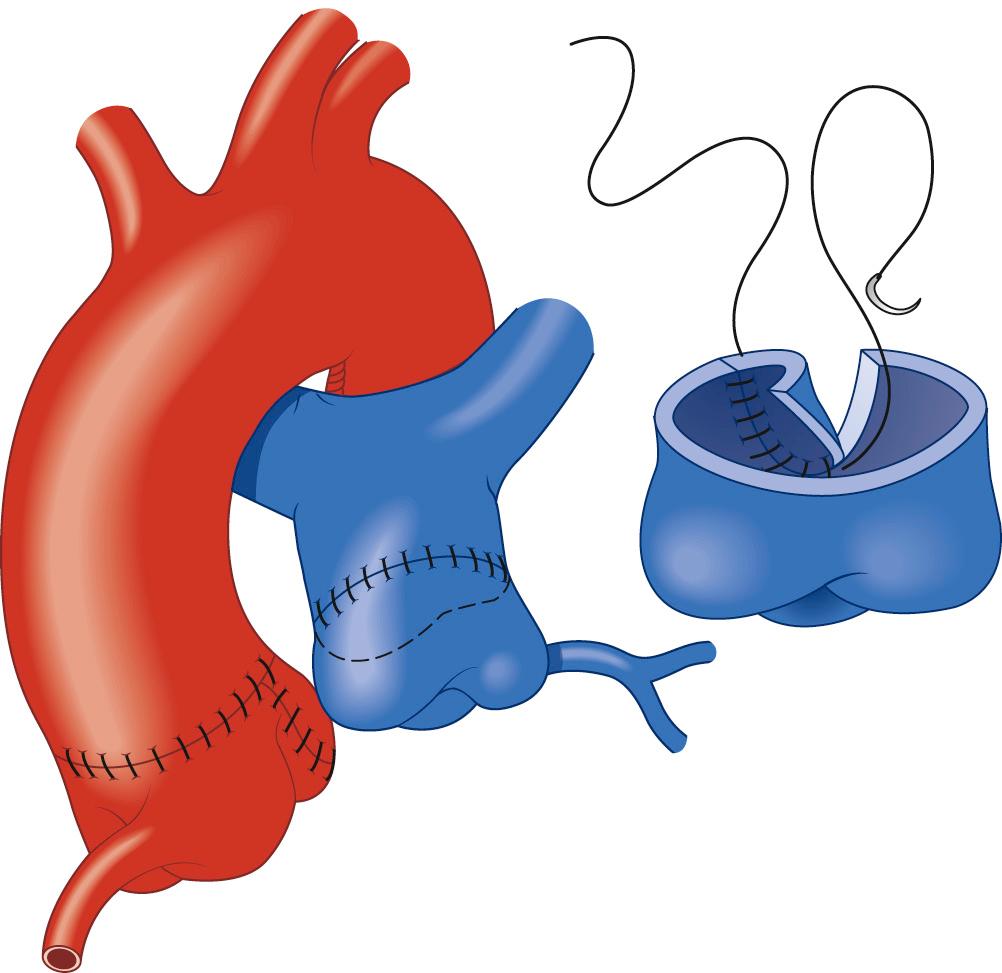
The aorta and both pulmonary arteries are fully mobilized. To improve mobility of the pulmonary artery, the ductus (or ligamentum) arteriosus is ligated. Tourniquets are placed around both the right and the left branch pulmonary arteries to occlude the branch pulmonary arteries and prevent runoff of cardioplegia solution into the lungs. Another option to prevent runoff is to compress the origin of the coronary artery from the pulmonary artery during administration of cardioplegia solution. A cannula is inserted in the ascending aorta for administration of cardioplegia solution, the aorta is cross-clamped, and cold cardioplegia is administered via the aortic root. If circulatory arrest is used, the head vessels are then occluded with tourniquets after adequate cooling, the circulation is arrested, venous blood is drained into the reservoir, and the cannulas are removed. After adequate arrest, the pulmonary artery is transversely opened just above the sinotubular junction (see Fig. 124-3 ). The anomalous coronary orifice is identified. The pulmonary artery is divided and the coronary ostium is excised from the pulmonary artery with a generous button of arterial wall, as in the procedure used for the arterial switch operation. The segment of the pulmonary wall that is excised extends the proximal end of the coronary artery, thus allowing the aortic anastomosis to be accomplished without tension. To excise the coronary button, the pulmonary commissure may need to be taken down if the coronary ostium is located near a commissure. An alternative technique that can be used if the coronary arises anteriorly from the pulmonary artery or from a branch pulmonary artery involves extension of the coronary artery with a tube constructed from pulmonary artery wall to allow reimplantation ( Fig. 124-4 ). The proximal portion of the coronary artery is mobilized with cautery, using caution to avoid any small branches. As in the arterial switch operation, the aorta is then opened transversely immediately above the sinotubular junction, and the incision is carried posteriorly above the left posterior sinus ( Fig. 124-5 ). The sinus is then incised vertically to accept the coronary button. The coronary button is carefully aligned with the aortic incision to avoid twisting or kinking. A continuous suture of 7-0 polypropylene (Prolene) is used to start the anastomosis at the most inferior aspect of the coronary button, which is attached to the most inferior aspect of the incision in the sinus. The suture line is carried to the top of the incision anteriorly and posteriorly. The aorta is closed with a continuous suture of 7-0 Prolene, which is tied to the coronary button suture as the anastomosis is completed (see Fig. 124-5 ). Once the aorta has been closed, cardioplegia solution is administered and the anastomotic site is inspected for adequate filling of the coronary and for hemostasis. Occasionally, the anomalous artery may arise from the right pulmonary artery and run along or within the aortic wall to the sinus. If there is a common wall with the aorta, mobilization may not be possible. In this case, unroofing of the intra-mural segment should be performed.
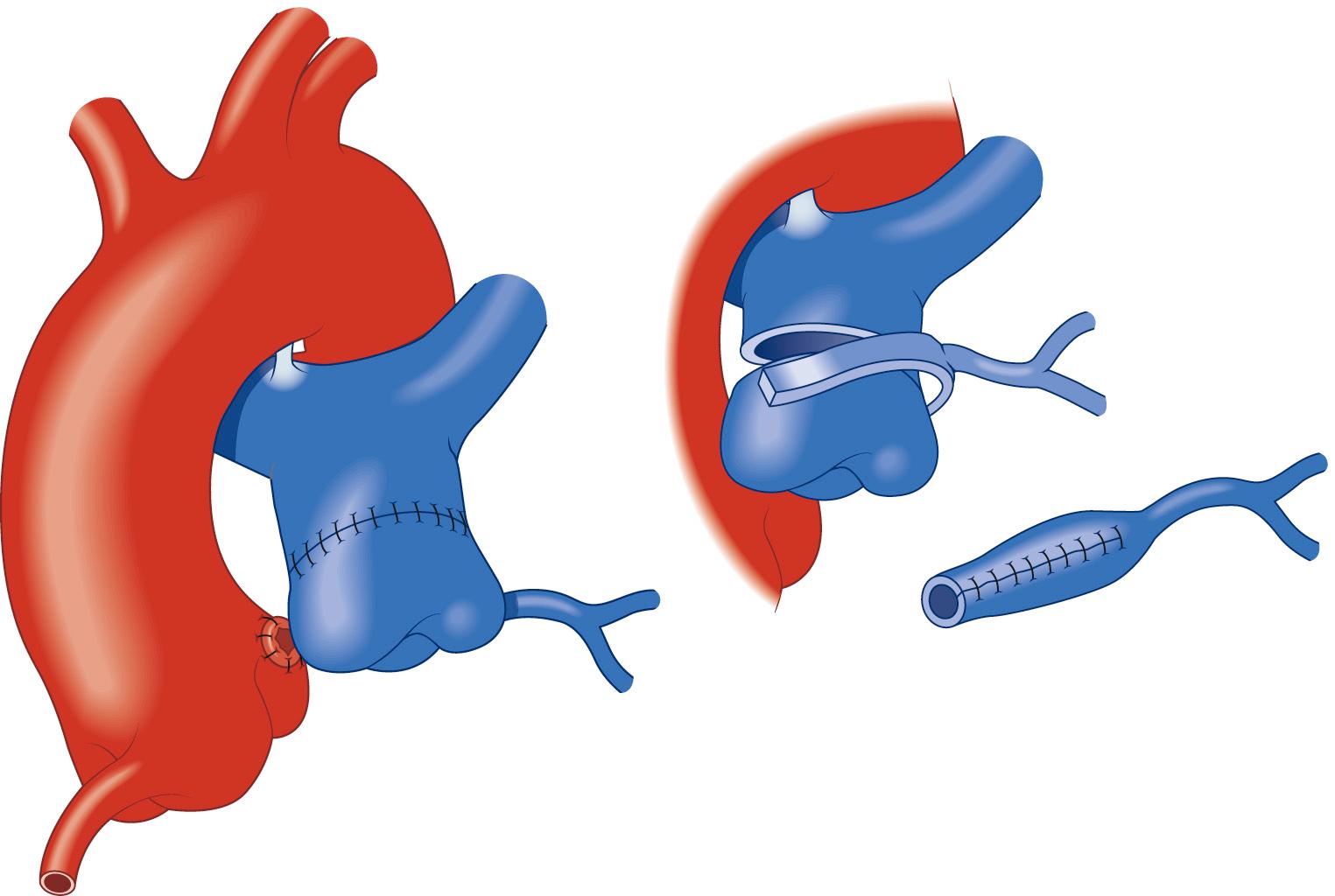
In some cases, the pulmonary artery can be repaired primarily with a continuous suture of 7-0 Prolene ( Fig. 124-6 ). The ductus should be divided to improve mobility of the pulmonary artery confluence, thus allowing reconstruction without tension. However, more often, the pulmonary artery is repaired with a patch of autologous pericardium (see Fig. 124-6 ). If a commissure was taken down during excision of the coronary button, the pulmonary artery should be reconstructed with pericardium and the commissure resuspended.
The patient is rewarmed and the aortic cross-clamp is removed. The cross-clamp may be removed before the pulmonary artery reconstruction to minimize ischemia time. The left ventricle is inspected to assess for adequate perfusion and function, and suture lines are inspected for hemostasis. Right and left atrial lines are placed to adequately monitor pressure and for drug administration. Atrial and ventricular pacing wires are also placed. The patient is separated from cardiopulmonary bypass after complete rewarming. Attention should be paid to the ECG during reperfusion and after separation from bypass for evidence of ischemia. Inotropic support may be necessary temporarily if there was left ventricular dysfunction preoperatively.
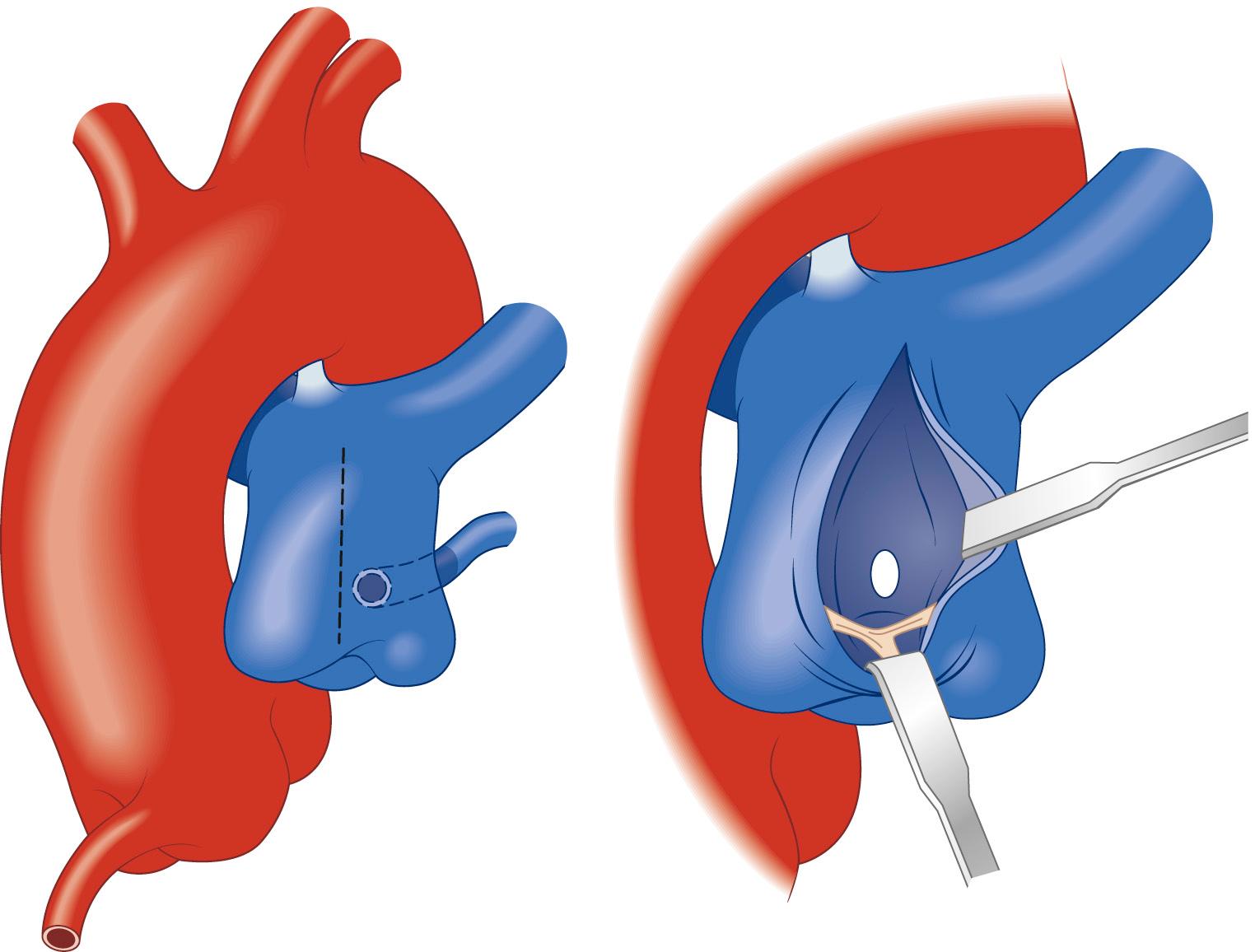
The Takeuchi operation, or intrapulmonary artery tunnel, is an alternative surgical strategy for repair of ALCAPA. Originally, Takeuchi and colleagues described the creation of an aortopulmonary window using a portion of anterior pulmonary artery wall to form a baffle that would direct blood from the aorta to the ostium of the anomalous coronary artery. In the modified repair, the baffle is constructed using a polytetrafluoroethylene (PTFE) (Gore-Tex) patch. Creating a baffle may not be possible if the ostium is located near a commissure or arises from a branch pulmonary artery. The procedure may be performed with either continuous low-flow cardiopulmonary bypass (25° C to 28° C) or deep hypothermic circulatory arrest (18° C). Cannulation is performed as for direct reimplantation.
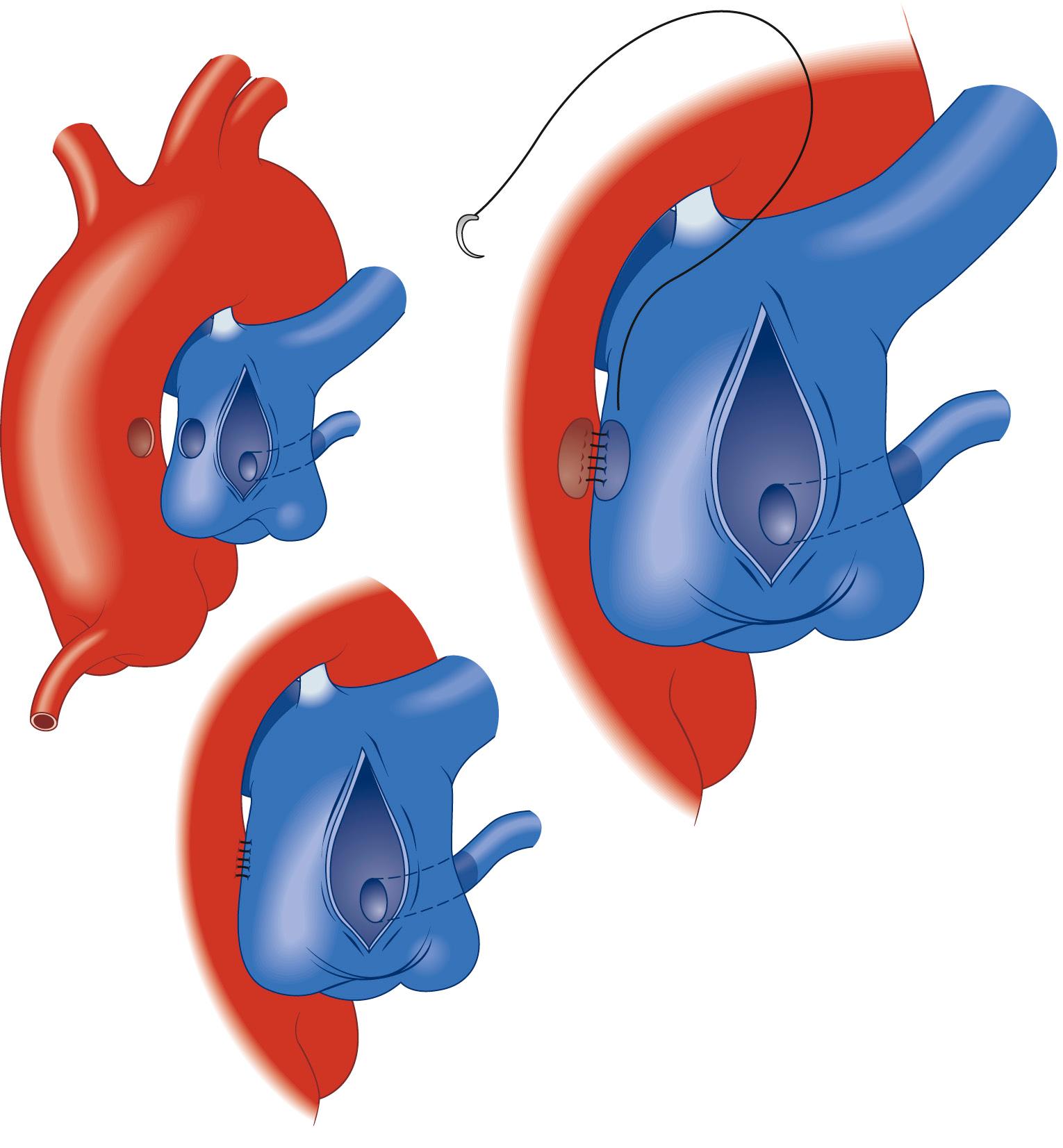
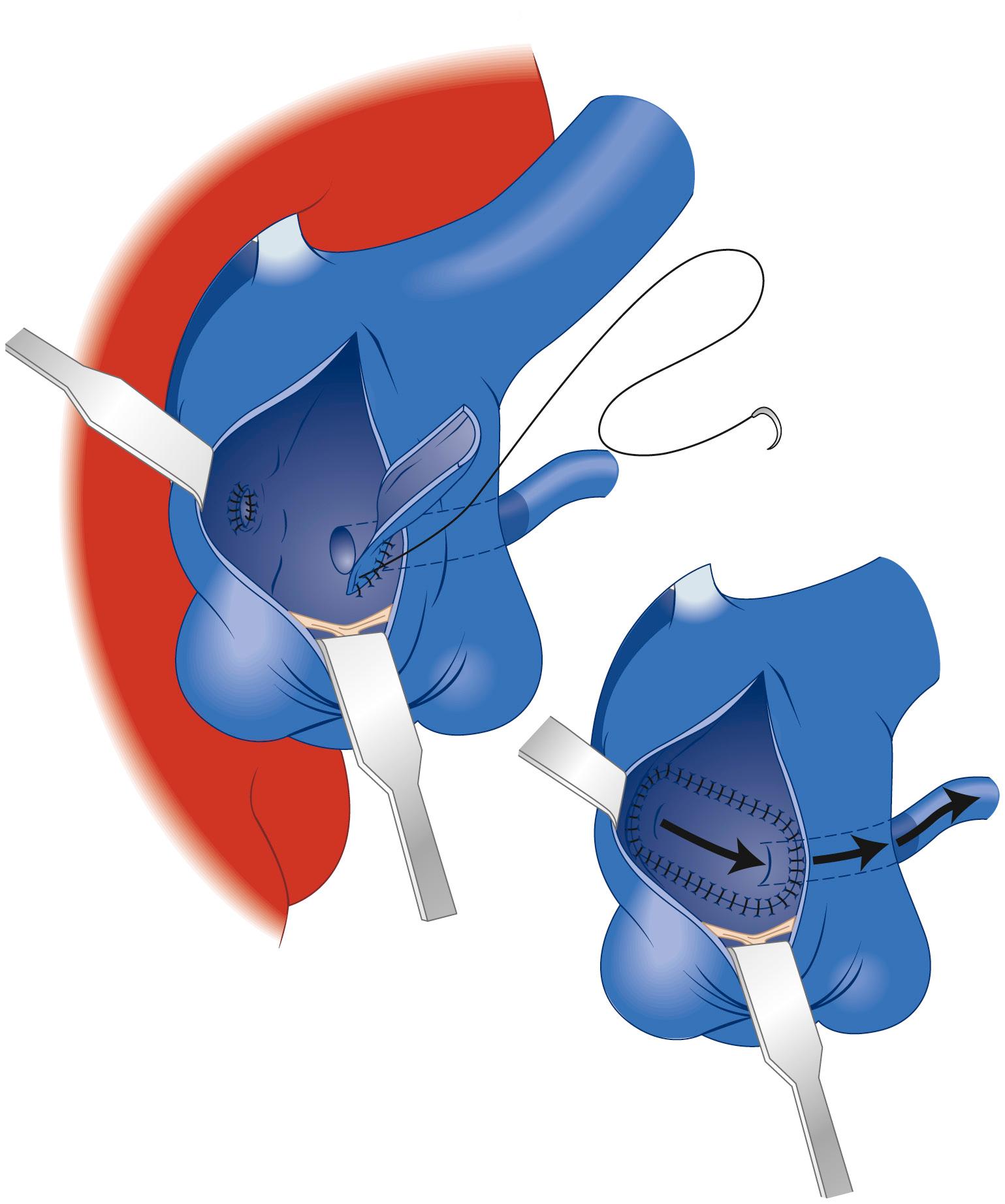
After induction of cardioplegia, a longitudinal incision is made in the anterior portion of the pulmonary artery ( Fig. 124-7 ), and the ostium of the anomalous coronary is identified. Using a punch, a 5-mm diameter opening is made on the leftward aspect of the aorta above the sinotubular junction ( Fig. 124-8 ). An anterior aortotomy should be performed if there is any question about placement of the aortic opening, and the incision should be directly visualized to avoid damage to the aortic valve. Creating the aortopulmonary window above the sinotubular junction allows a downward angle of the baffle into the sinus if the ostium is located deep in a sinus. After a similar incision is made in the pulmonary artery directly opposite the opening in the aorta, these are anastomosed using a continuous suture of 7-0 Prolene and creating an aortopulmonary window (see Fig. 124-8 ). A 4-mm PTFE tube graft is split longitudinally and customized to an appropriate length ( Fig. 124-9 ). This graft acts as an intrapulmonary artery tunnel, baffling blood from the aortopulmonary window to the anomalous coronary ostium. The suture line starts at the anomalous coronary and is continued inferiorly along the pulmonary artery wall to the aortopulmonary window. The suture line is completed by returning to the coronary artery and completing the superior aspect of the baffle. After the baffle is created, repair of the pulmonary artery can be accomplished using a prosthetic patch or autologous pericardium to avoid supravalvar pulmonary artery obstruction ( Fig. 124-10 ). The main complications of the modified Takeuchi operation include baffle leak, baffle occlusion, and supravalvar pulmonary artery obstruction.

Regardless of the surgical technique used, the most common postoperative issues are those related to the infant's preoperative state: low cardiac output, left ventricular dysfunction, and hypotension. Optimizing the patient's hemoglobin, electrolytes, acid-base status, and fluid status and providing adequate inotropic support are extremely important. In infants and children with severe preoperative cardiac dysfunction, temporary support with an LVAD or ECMO may be necessary in the postoperative period. Bleeding is also common postoperatively and is more frequently encountered in small infants and those who require mechanical support. Platelets and fresh-frozen plasma should be used aggressively to replace ongoing loss. Patients with low cardiac output or bleeding issues may require delayed sternal closure (2 to 3 days).
Simple ligation of ALCAPA has been shown to have unacceptable early and late mortality rates. In general, survival after establishment of a dual coronary system is excellent. In 1987, Bunton and colleagues from Boston reported on 24 patients with ALCAPA. From among these 24 patients, 11 received coronary ligation or ostial closure, 11 had a Takeuchi repair, and 2 underwent other procedures. Of the patients who underwent coronary ligation or ostial closure, there was a 27% early mortality and a 25% late mortality over an average 10.5-year follow-up period. In those who underwent a Takeuchi procedure, there were no early or late deaths in over an 18.5-month follow-up period. After Takeuchi repair, two patients developed right ventricular outflow tract obstruction (one required a second operation), and one patient was found to have baffle occlusion.
Backer and colleagues reported the follow-up surgical results of 20 patients with ALCAPA who underwent different procedures. There were two early deaths and one late death among nine patients who underwent ligation. In contrast, there were no deaths among the 10 patients who underwent creation of a dual coronary artery system and the one patient who had cardiac transplantation. Five patients had left subclavian–to–left coronary anastomosis, and two developed significant anastomotic stenosis.
Vouhe and associates from France reported on reimplantation of the anomalous coronary in 31 consecutive children. Three hospital deaths and two additional deaths occurred within the first 3 months. No late deaths occurred. The only risk factor identified for early mortality was a shortening fraction of less than 20%. Twenty-three survivors were studied more than 1 year after repair. All patients had normal left ventricular function, and in five of seven patients who had severe mitral regurgitation preoperatively, the severity had decreased to mild or no regurgitation. The reimplanted coronary artery was patent in all patients.
A 2007 report by Lange and colleagues reviewed the long-term results of 56 patients with ALCAPA who underwent either subclavian artery anastomosis or coronary artery transfer. Patients who had had a Takeuchi procedure or a left mammary artery graft were excluded. There were similar early mortality rates (14%) for both surgical groups but no mortality in those undergoing repair in the last 13 years. Late mortality in each group was also similar, with one patient in each group. At final follow-up (mean 14.5 years for subclavian artery group and 8.7 years for coronary transfer group), 95% of patients had normal left ventricular function and 84% had mitral regurgitation less than grade 2. However, if left ventricular function does not improve after revascularization, cardiac transplantation may be indicated.
There has been controversy regarding the management of mitral regurgitation during the initial surgery. In general, at least a moderate degree of mitral regurgitation is found at the initial presentation. Even in patients with severe mitral regurgitation, there have been several reports of significant improvement after coronary reperfusion alone, probably because of better left ventricular dysfunction and a decrease in left ventricular size postoperatively. Furthermore, valve repair at the time of initial surgery can result in longer ischemic times and can be technically more difficult to perform in an infant's heart than when the child is bigger. However, some authors recommend routine annuloplasty at the time of initial repair, whereas others propose annuloplasty or mitral valve replacement only with severe mitral regurgitation. In summary, early surgical repair of the mitral valve is generally not necessary. If valve repair in the setting of severe mitral regurgitation is needed later, it is likely to be more successful and easier to do technically. However, if severe mitral regurgitation persists late postoperatively, possible causes of ongoing myocardial ischemia should be investigated.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here