Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic neuropathic pain of the lower extremity caused by sural nerve pathology is a rare reason for patients to seek medical attention. These pathologies have several underlying etiologies, and patients may have symptoms that limit their quality of life despite conservative therapy. Due to its uncommon occurrence, few clinicians have experience treating cases refractory to conservative measures, and there are few treatment options available for patients. Peripheral nerve stimulation (PNS) represents a potential intervention for these patients who have refractory symptoms of sural nerve pathology and represents an opportunity to improve quality of life for these patients.
Formed by the fusion of terminal branches of the common peroneal and tibial nerves, the sural nerve is implicated in several conditions that lead to pain of the lower extremity. In this chapter, we will examine the clinical presentation of sural nerve neuropathic pain, relevant anatomy, history and physical exam, imaging, and diagnostic nerve blocks, in addition to the technique for using PNS as a therapeutic modality.
The sural nerve, a small, superficial sensory nerve, receives contributions from multiple different components, including the medial sural cutaneous nerve (MSCN), the lateral sural cutaneous nerve (LSCN), and the peroneal communicating nerve ( Fig. 30.1 ).
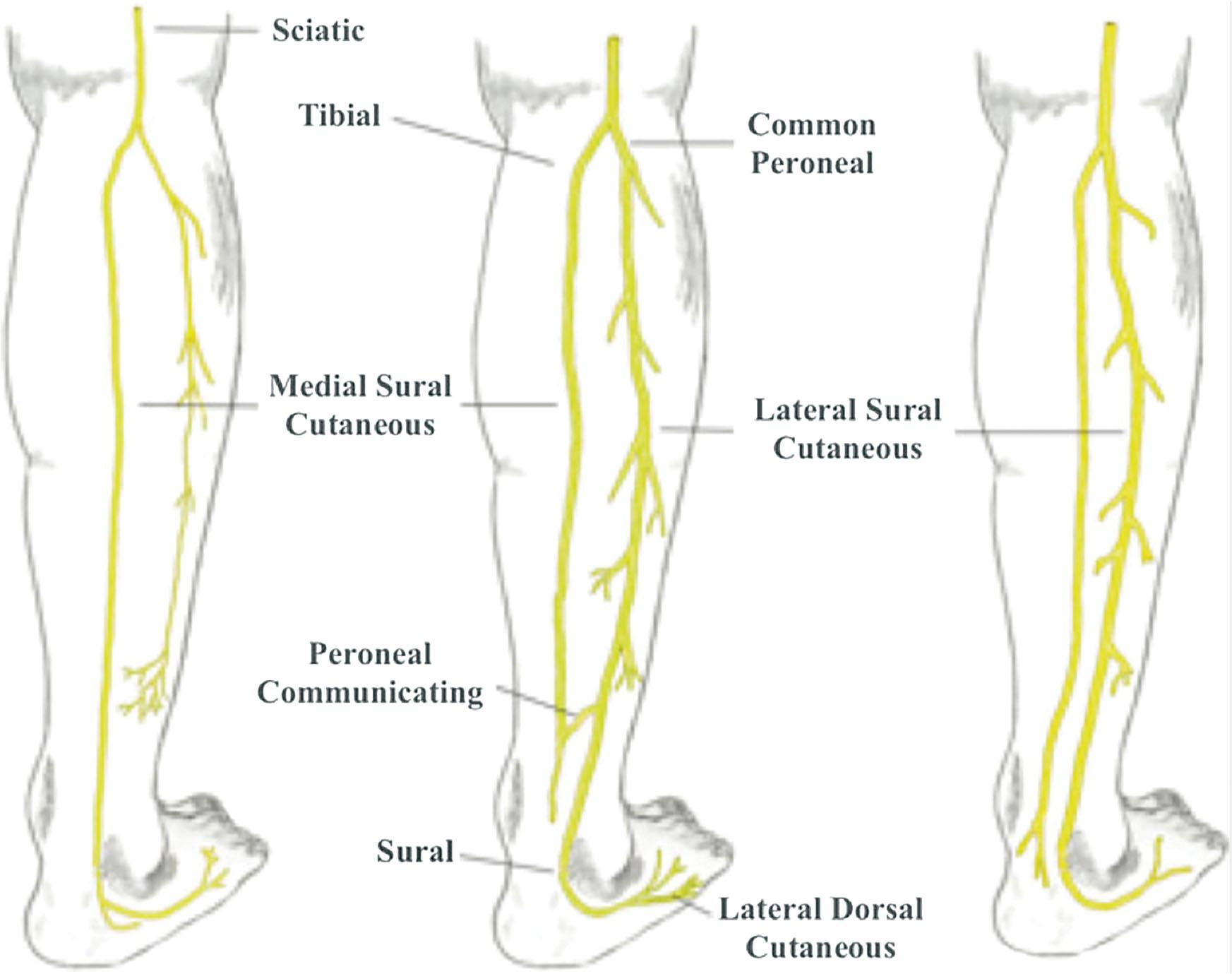
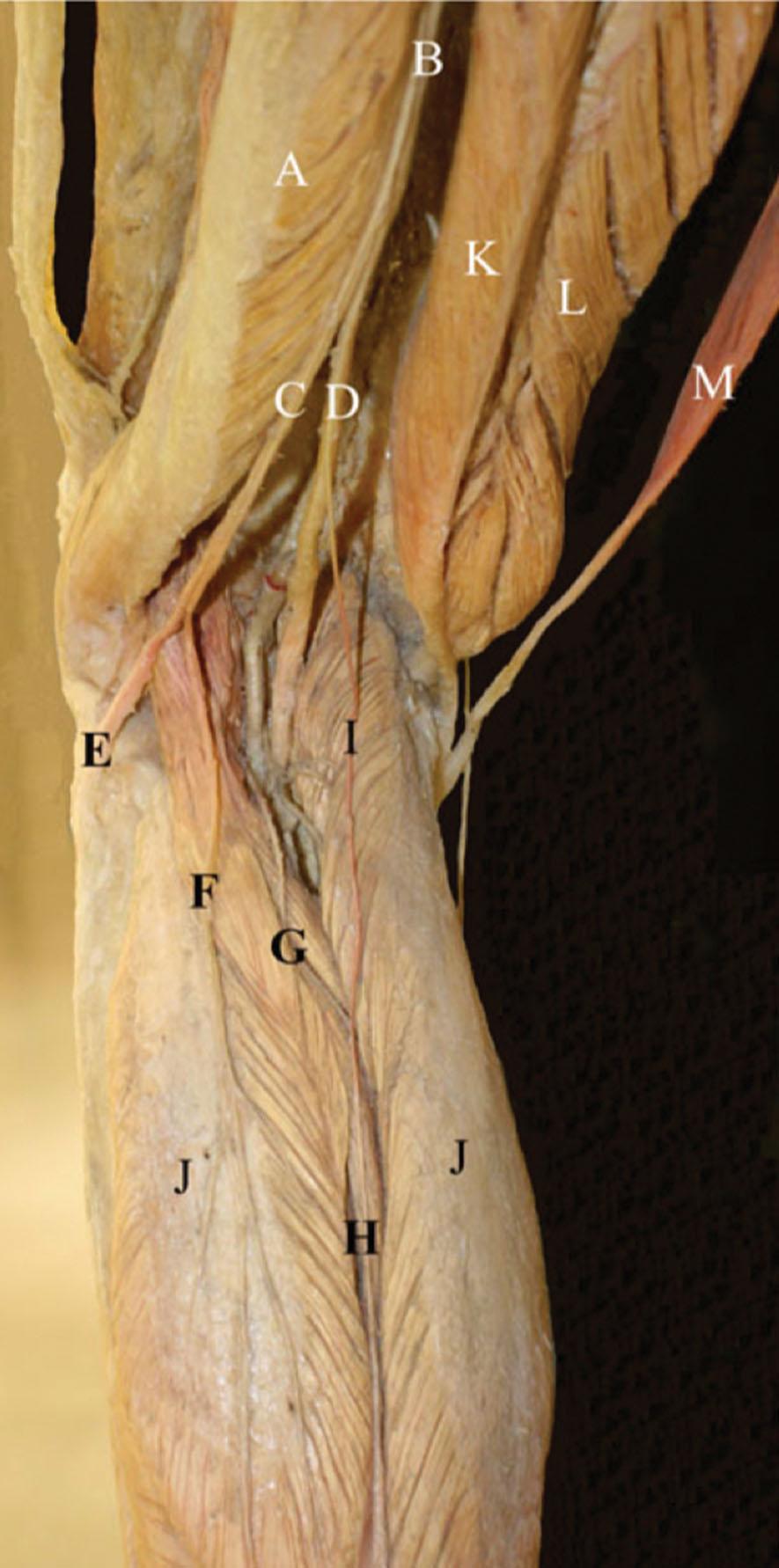
In the apex of the popliteal fossa, the sciatic nerve bifurcates into two branches: the tibial nerve and the common peroneal nerve (also known as the common fibular nerve) ( Fig. 30.2 ) The tibial nerve travels through popliteal fossa lateral to the popliteal vein and artery. Prior to diving deep into the gastrocnemius muscle, the tibial nerve gives off a cutaneous sensory branch, the MSCN. The MSCN then descends between two heads of gastrocnemius muscle and pierces the deep to the crural fascia of the calf and eventually emerges superficially at the inferior third of the leg. The MSCN finally joins the LSCN via the peroneal communicating nerve to form the distal sural nerve.
The peroneal communicating nerve originates in the popliteal fossa from the common peroneal nerve and may distally contribute to the sural nerve. The most common convergence of the sural nerve is when both the medial and lateral sural nerves merge. Less commonly, the distal sural nerve may have contributions solely from either the MSCN or the LSCN.
The sural nerve itself travels in between two heads of the gastrocnemius muscle in the distal third of the leg next to the small saphenous vein and then pierces the deep fascia at the middle third of the posterior leg. It then exits this “gastrocnemius groove” near the musculotendinous junction of the Achilles tendon and the gastrocnemius muscle ( Fig. 30.3 ). This fibrous arcade is wide, thick, and unyielding, and may fit tightly around the nerve, causing chronic friction and irritation that can lead to sural neuropathy.
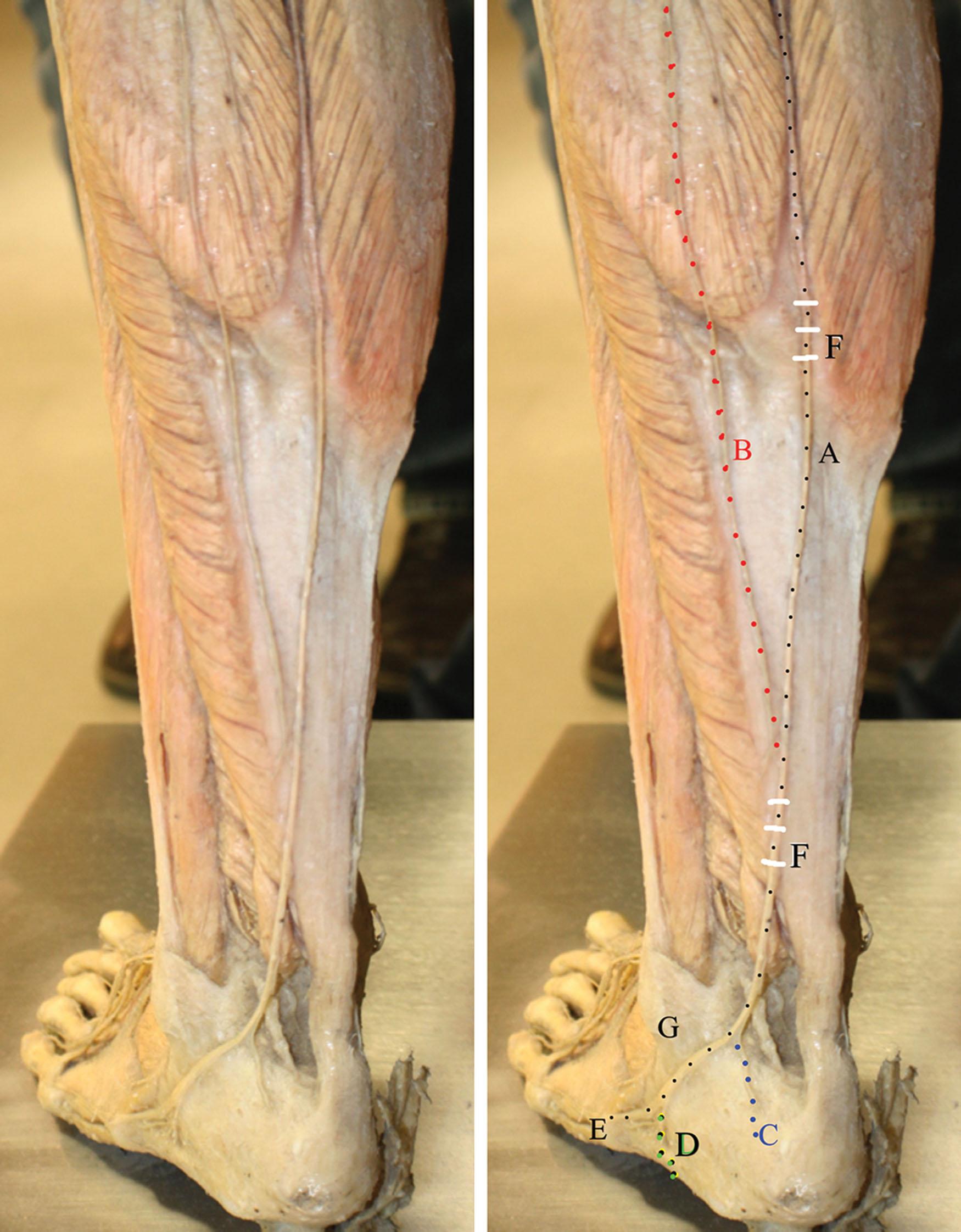
Importantly, the most common cause of sural neuropathy is traumatic injury secondary to ankle fracture. Another important etiology is repetitive injuries to the lateral ankle that can lead to neuronal damage of the sural nerve. Other possible injuries include ankle inversion sprains, metatarsal fractures, calcaneal fractures, gastrocnemius or soleus hematomas, compartment syndromes, Achilles tendon tears, and neural damage during ankle surgery. Inflammatory lesions affecting the sural nerve may include thrombophlebitis, wound infection, venous stasis ulcers, suture neuritis, and viral neuritis. Other pathologies of lateral ankle and foot pain may include lumbar radiculopathy, sciatic nerve entrapments, and peroneal nerve entrapments. Further, because the sural nerve traverses through the lateral aspect of the Achilles tendon, repetitive injuries of the Achilles tendon can cause sural neuropathic pain. Sural nerve entrapment is another common source of sural neuropathic pain. Anatomically this can occur in three potential locations, including at the level of midcalf between the heads of gastrocnemius, at the fibrous arcade superficial to the Achilles tendon, and at the lateral foot ( Fig. 30.4 ).
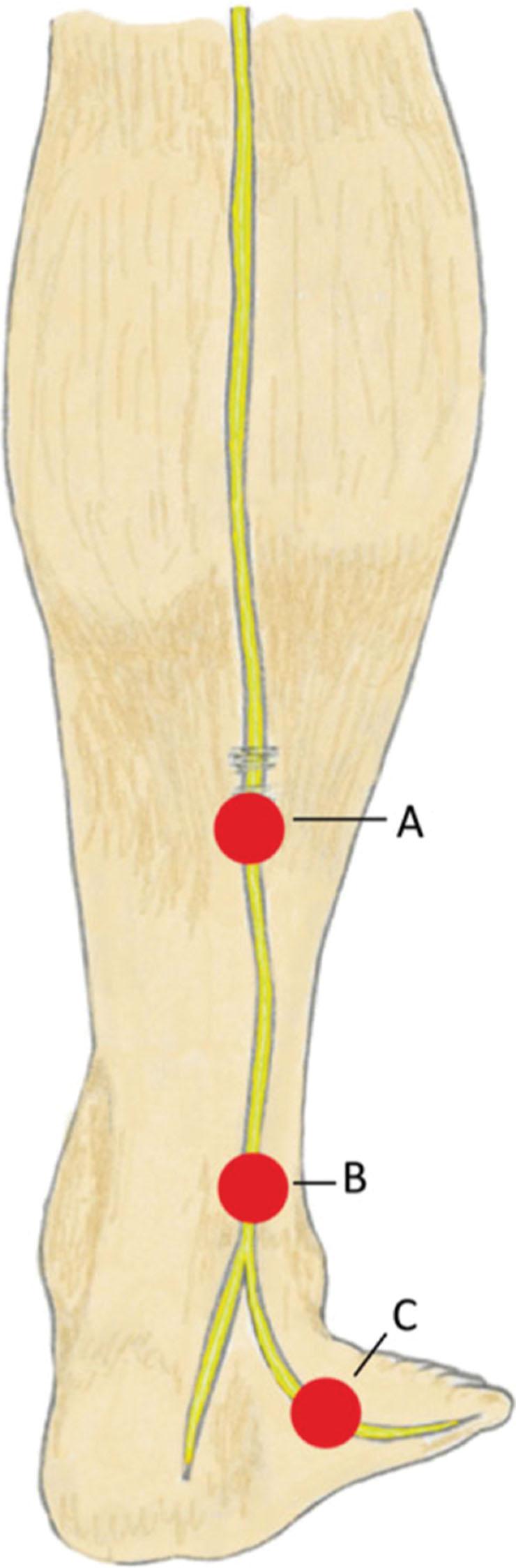
Sural nerve entrapment, neuritis, and neuropathy often present with ankle and calf pain. Specifically, patients typically report lateral calf, ankle, and foot pain with or without dysesthesia and paresthesia ( Fig. 30.5 ). In most cases, pain may be worsened by ambulation, pivoting, and daily activities. In acute and subacute cases, patients can have swelling over the lateral aspects of the ankles. Light touch, socks, and shoes may aggravate patients’ symptoms. In chronic cases, patients may present with worsening pain, burning, tingling, and cramps at night. Patients with diabetic neuropathy and generalized peripheral neuropathies may also have disease of the sural nerve with symptoms of pain in the lateral toes and plantar aspects of foot, which may radiate to the posterior lateral calf.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here