Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hip joint pain and pathology is traditionally separated into anterior and posterior innervations. Anterior innervation is provided by the articular branches of the femoral (anterior capsule) and obturator (anteromedial capsule) nerves. The posterior innervation is by articular branches of the sciatic nerve (posteromedial), nerve to quadratus femoris (NQF) (posteromedial), and superior gluteal nerve (SGN) (posterolateral). Techniques regarding peripheral nerve stimulation of the NQF are limited at this time. This chapter will focus on the SGN, as the femoral, obturator, and sciatic nerves are covered elsewhere in this book.
Patients with SGN pathology present with the “SGN triad,” consisting of gluteal pain, tenderness, and hip abductor weakness. Patients will point to the buttocks as the site of their pain ( Fig. 31.1 ) and may experience pain from the buttocks to the foot with prolonged sitting and standing, forwarding leaning, or twisting to the contralateral side. Pain may resolve or decrease with sitting. Patients may present with aching, claudication-type buttock pain, and they may report tenderness to palpation in the area of the superomedial gluteal region. Patients may demonstrate weakness of abduction of the affected hip, resulting in a waddling gait. Other symptoms include the inability to sit for prolonged durations, limping, and pain at night that gets better during the day.

SGN entrapment or injury can result from forced internal rotation of the hip, trauma, extension of the hip under mechanical load, spasm of the piriformis, or hip surgery. Entrapment may also result from compression by anterior-superior tendinous fibers of the piriformis muscle. Surgical approaches to hip interventions have been cited as a source of injury to the SGN. Specifically, the SGN is commonly injured during the direct lateral approach to hip surgery. SGN branches to the tensor fasciae latae (TFL) are injured during anterolateral or anterior hip surgery. Of patients requiring total hip arthroplasty, 77% were found to have electromyography (EMG) abnormalities postoperatively indicating disruption of the SGN.
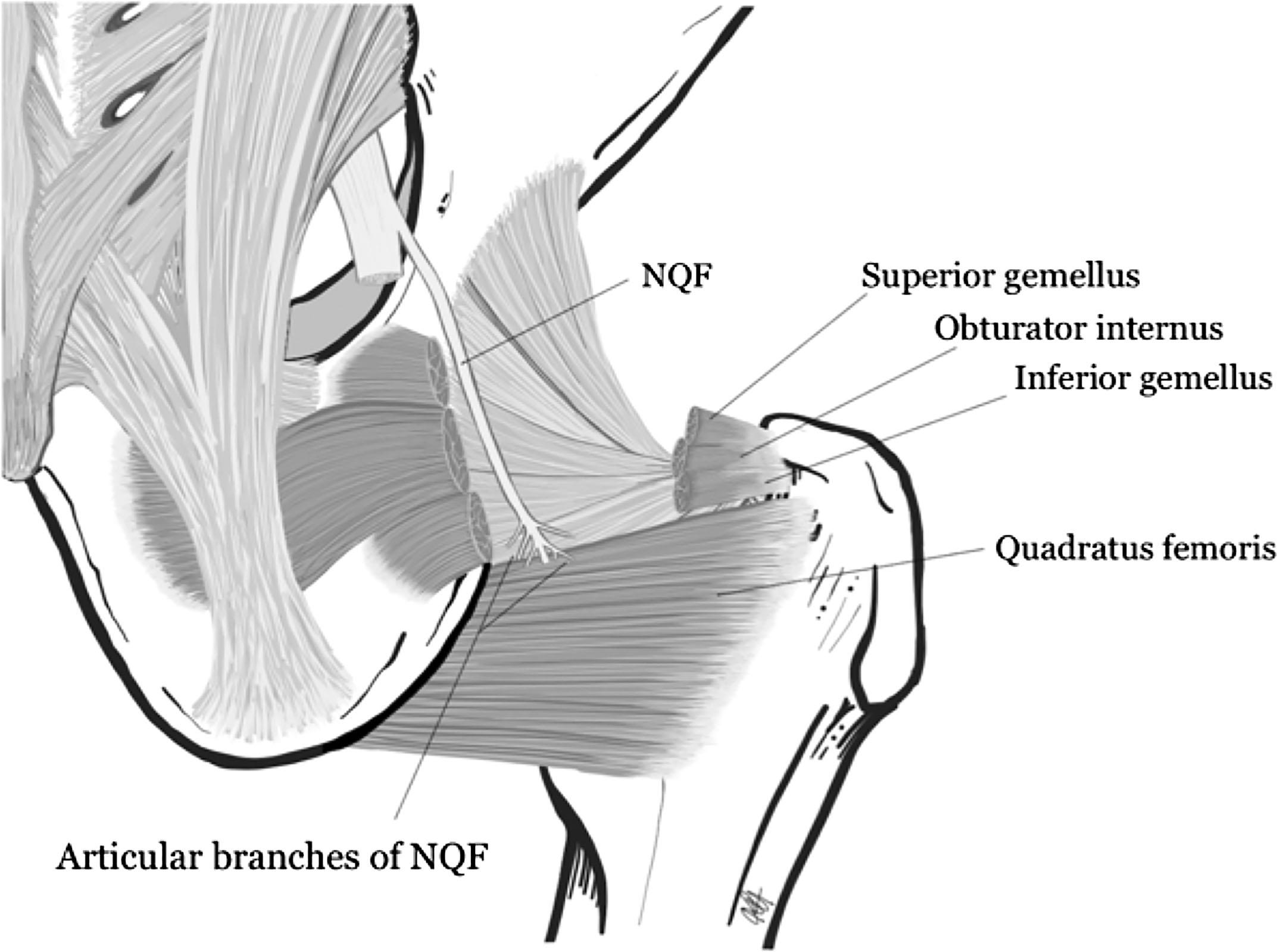
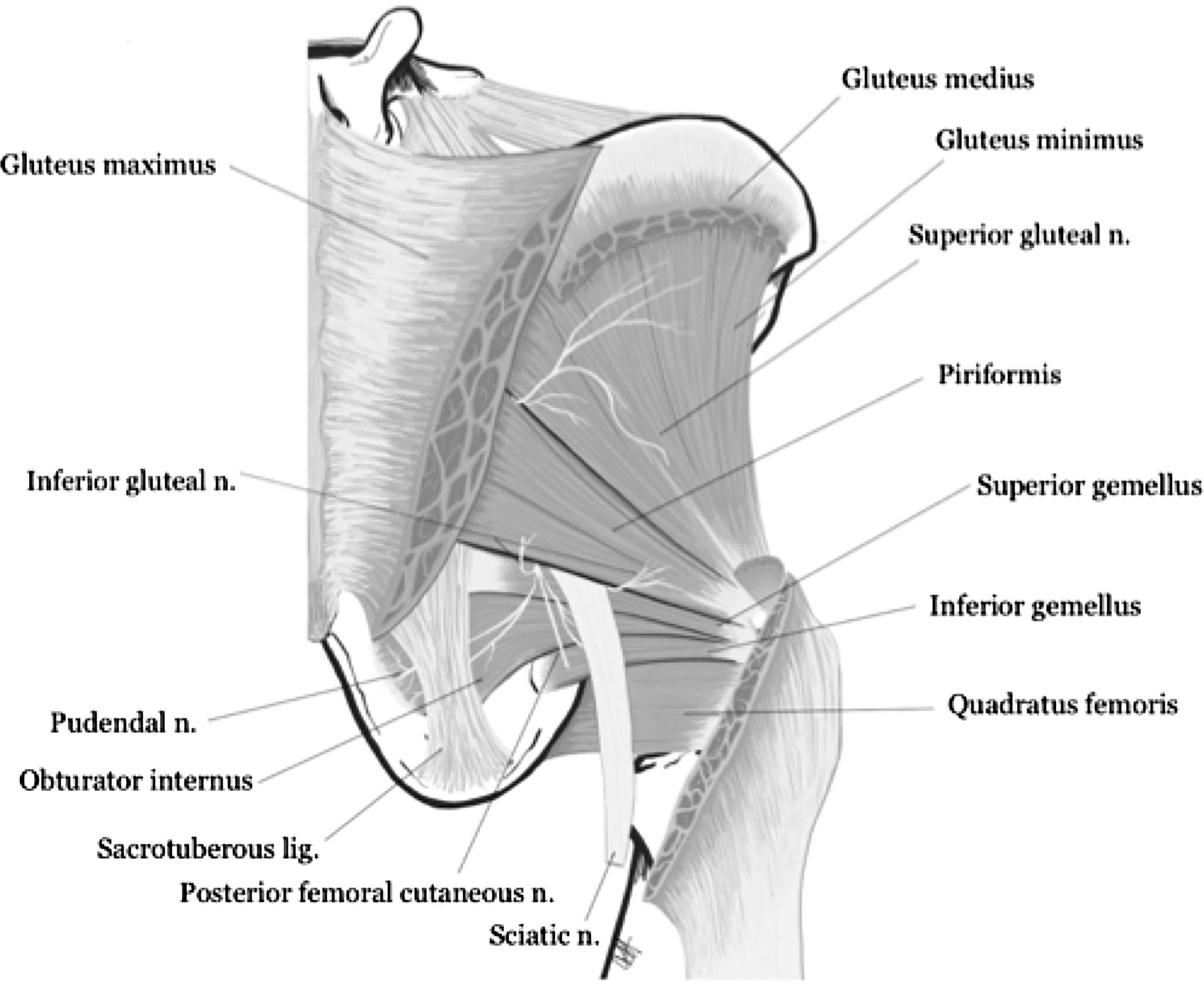
As described earlier, the NQF is located inferior to the piriformis and deep to the gemelli and the obturator internus muscle ( Fig. 31.2 ). The SGN originates from the sacral plexus and arises from the posterior divisions of the lumbosacral plexus (ventral rami of L4, L5, and S1). The SGN passes through the greater sciatic foramen superior to the piriformis, as seen in Fig. 31.3 , in the fascial plane between the gluteus minimus and gluteus medius extending to the TFL. The inferior branch supplies the gluteus minimus and the TFL. The superior branch supplies the gluteus medius. For a majority of patients, the SGN also innervates the piriformis muscle. The SGN is deep to the gluteus maximus and medius. It is accompanied by the superior gluteal artery and the superior gluteal vein over the surface of the gluteus minimus muscle. The nerve passes approximately 5 cm superior to the tip of the greater trochanter. The SGN is the only nerve to exit the greater sciatic foramen above the piriformis muscle.
Clinical history and thorough physical exam can often result in valuable diagnostic impressions of neuropathic pain. Ultrasonography, EMG, computed tomography, and magnetic resonance imaging can be applied and interpreted alongside clinical results to further identify the underlying pathology of pain. Nerve conduction studies and EMG can be applied for select cases.
A quality history begins with obtaining information regarding the onset, provocative/palliating factors, quality, radiation, site, symptoms associated with pain, and time course of the pain. Investigating trauma is of specific importance for the SGN because it can guide identification of mechanisms of injury and management. Patients with SGN nerve injury will most often have pain the upper gluteal area or in the deep lateral hip area (lateral branch runs near the greater trochanter).
Patients with SGN pathology may report a history of trauma, direct loading on an internally rotated hip, or surgery. They may complain of the “SGN triad,” as mentioned above (gluteal pain, tenderness, and hip abductor weakness). Patients may present with aching and claudicating pain of the superolateral buttock, weakness of hip abduction, and a waddling gait.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here