Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A 48-year-old hospital administrator began having difficulties during meetings when her back would stiffen up every time she was asked to get up to speak. Subsequently, she developed episodes of anxiety accompanied by her left leg tightening up. Her internist referred her to a counselor thinking these episodes were “emotionally driven.” However, they became more frequent, usually occurring when standing and talking to people at work. She described her legs as feeling like walking “on stilts.” On one occasion when she started to laugh, her left leg stiffened and she fell “like a tin soldier.” The primary finding on examination was her spontaneous reaction to any sensory stimuli wherein her back stiffened. Other than hyperlordosis and marked hyperreflexia at her knees, her neurologic examination was normal. Magnetic resonance imaging (MRI) of her brain and spine proved normal. A needle electromyography (EMG) study demonstrated cramp discharges in contracting muscles during episodes of stiffness, but was otherwise normal. Immunoprecipitation assay showed a high level of serum glutamic acid decarboxylase 65 (GAD-65) antibodies (47 nmol/L; reference range: ≤0.02 nmol/L). She was diagnosed with stiff-person syndrome (SPS). Diazepam dramatically alleviated symptoms at a daily dose of 40 mg. Treatment with corticosteroids or intravenous immunoglobulin was contemplated, but was ultimately not required thanks to sufficient control with symptomatic therapy. Over the subsequent 5 years, she was successfully tapered off the benzodiazepine.
Stiff-person syndrome (SPS) is an autoimmune central nervous system disorder with localization primarily to the brainstem and spinal cord. It is characterized by fluctuating muscle stiffness with superimposed spasms and is often accompanied by exaggerated startle response. Possible manifestations include classic SPS, stiff-limb syndrome (SLS), and a rare presentation with some or all components of progressive encephalomyelitis with rigidity and myoclonus (PERM). Also, increasingly recognized are variants of SPS with additional neurologic symptoms of cerebellar ataxia, epilepsy, or limbic encephalitis. The recently introduced term “stiff-person spectrum disorder” (SPSD) reflects this emerging clinical heterogeneity.
SPS is a rare disease with an estimated prevalence of 1 in 1,250,000 people. Women are more often affected than men. SPS generally presents in the fourth through sixth decades. Childhood onset was only recently recognized, with onset as early as 1 year of age. Owing to its rarity and protean symptomatology, SPS is still often misdiagnosed as a psychogenic movement disorder or dystonia. As a result, a delay in diagnosis is not uncommon.
The current understanding is that SPS is an autoimmune disease targeting proteins associated with gamma-amino-butyric acid (GABA)- or glycine-related inhibitory pathways in the spinal cord and brainstem. Antibodies targeted against GAD-65 (glutamic acid decarboxylase) are found most often in SPS; GlyR (glycine receptor) and amphiphysin are some of the less common antigens, and there are likely others yet to be characterized. The precise pathophysiologic role for the specific antibodies is unclear. The autoimmune basis for SPS is further supported by its frequent association with other autoimmune disorders such as type 1 diabetes mellitus (in almost half of patients), thyroiditis, vitiligo, and pernicious anemia. Rarely, SPS can be a manifestation of paraneoplastic autoimmunity; amphiphysin antibody is detected in some of these cases, most often in older women with breast cancer.
GAD-65 antibodies are found in 60%–80% of patients with classic SPS, and less frequently in other subtypes such as PERM. The antibody titer is typically high (>20 nmol/L). The same antibody, but in low titer, is detected in 90% of patients with type 1 diabetes mellitus. GAD-65 antibody is not specific for SPS; it has been associated with immune-mediated cerebellar ataxia, limbic encephalitis, and temporal lobe epilepsy. Because it is directed against a cytoplasmic antigen, GAD-65 antibody is probably not pathogenic. It is more likely to be a marker for organ-specific autoimmune attack by cytotoxic T-cells. Consequently, the response to GAD-65 antibody-depleting therapy is variable and rarely leads to complete recovery.
Antibodies against glycine receptor (GlyR) are associated with PERM. Unlike GAD-65, GlyR is expressed on the surface of motor neurons in the brainstem and spinal cord. Therefore, GlyR antibodies are more likely to be causative. This may explain why PERM patients, if diagnosed early, may have a better response to antibody-depleting therapy than those with GAD-65 antibodies.
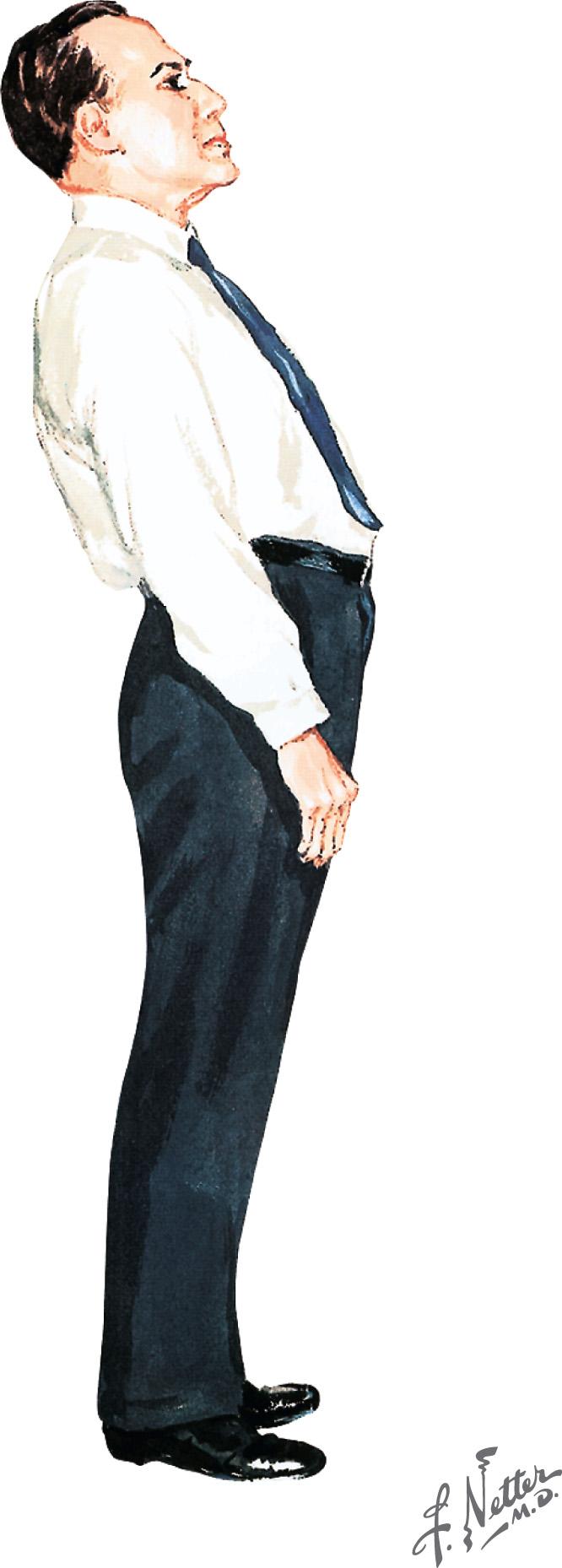
Typically, classic SPS is characterized by spine and leg rigidity with lumbar hyperlordosis as a key feature ( Fig. 64.1 ). Coined “Frankenstein's gait,” the patient walks with a wide base and extended legs and tends to fall in a manner similar to a stiff board. Patients experience superimposed painful spasms that may be precipitated by sudden noise, anxiety, or touch. The spasms can be of such abrupt onset and power that these individuals may unexpectedly and precipitously fall. Patients soon recognize that emotional stress often provokes their spasms, and they may develop agoraphobia secondary to the fear of falling in public. Neurologic examination often reveals hyperlordosis, leg rigidity, and “board-like” hardness of paraspinal and abdominal muscles. These findings may not be present until late in the clinical course. Brisk muscle stretch reflexes may be observed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here