Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Psoriasis is common, affecting over 125 million worldwide.
Comorbidities include diabetes, hypertension, dyslipidemia, obesity, myocardial infarction, stroke, cardiovascular death, lymphoma, autoimmune disorders, and renal disease.
TNF signaling and the IL-23/Th17 pathways are critical in the pathogenesis of psoriasis, and effective therapies interfere with these pathways.
Treatment with systemic therapy may improve risk for cardiovascular disease.
About one-third of psoriasis patients may develop psoriatic arthritis, on average 10 years after the onset of skin disease.
Psoriatic arthritis can be differentiated from other arthritides with the CASPAR diagnostic criteria.
Psoriasis is a chronic immune-mediated skin condition that affects 2% to 3% of the US population. Psoriasis is found worldwide, and over 125 million people are thought to be afflicted. The lowest prevalence rates are reported in Asia with less than 0.5%, and the highest in Norway at 4.82% and France at 5.20%.
Psoriasis is more than just a skin disease. Several comorbidities are associated with psoriasis. About one-third of patients may develop psoriatic arthritis, on average 10 years after psoriasis appears. It has been shown that those with psoriasis are also at higher risk for cardiometabolic conditions such as diabetes, hypertension, dyslipidemia, obesity, and metabolic syndrome. These patients are at higher risk for myocardial infarction, stroke, and cardiovascular death. They are more likely to develop lymphoma, autoimmune disorders, and renal disease. Furthermore, patients with psoriasis are more likely to have psychiatric conditions such as depression and anxiety, and are more likely to smoke and drink alcohol.
The most striking feature of psoriasis is the silvery scaling and redness that sharply demarcates the plaques from the surrounding normal skin. Histologically it is characterized by marked hyperproliferation of keratinocytes, altered epidermal differentiation, and proliferation of endothelial cells accompanied by an influx of various inflammatory cells. Substantial evidence implicates activated T-cells in the pathogenesis of psoriasis. Both CD4+ and CD8+ T-cells are found in psoriatic skin lesions, with CD4+ T-cells being primarily located in the upper dermis and CD8+ T-cells within the epidermis. CD8+ T cells in the epidermis are required for the development of psoriasis lesions. The CD8+ T-cells are oligoclonal, suggesting that they are responding to a restricted set of antigens, likely in the psoriatic epidermis. Multiple other cell types participate in this process including keratinocytes, dendritic cells, macrophages, mast cells, endothelial cells, and neutrophils. Cytokines initiate and sustain inflammation through pathways that involve cells of both the innate and acquired immune systems. These pathways, including tumor necrosis factor (TNF) signaling and the IL-23/Th17 (interleukin-23/T helper 17) pathways, are critical, as blockade of either one is highly effective for treatment. Interestingly, the mechanism of action for TNF inhibitors, such as etanercept, appears to be due to suppression of IL-17 signaling rather than a direct response to TNF. Besides IL-17 and TNF-α, multiple other cytokines and growth factors participate in this process, and the interaction is incompletely understood.
It has been known for over 100 years that psoriasis has a strong genetic component. However, it is only in the past few years that major strides have been made in identifying the specific genetic risk factors, mostly through genome-wide association studies. To date over 40 independent genetic signals have been identified. One of the most prominent genetic signals identified in psoriasis is HLA-Cw6. Several other risk loci are close to genes involved in antigen processing and presentation, including the ERAP1 and ERAP2 genes, which may tie in with the role of CD8+ T-cell function, as those cells respond to antigens in the context of major histocompatibility complex class I. Several of the risk loci are close to genes that play key roles in IL-23/IL-17 responses and others map to regions involved in epidermal barrier formation, inflammatory dendritic cell function, nuclear factor kappa beta, interferon signaling, and Th1/Th2 polarization. These genetic findings, along with progress in our understanding of the immunology, highlight the key pathogenic circuits and increase our ability to more effectively treat this disease.
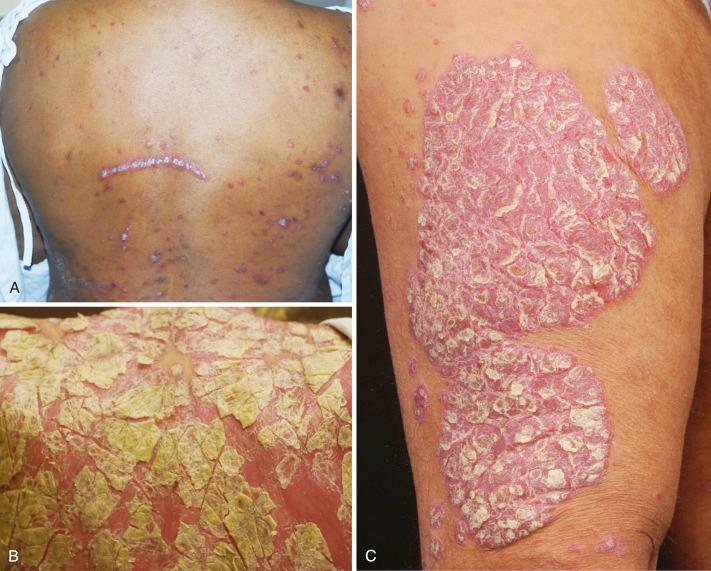
Chronic plaque psoriasis/psoriasis vulgaris is the most common clinical form of psoriasis, and is found in approximately 90% of patients. The skin manifestations are characterized by well-demarcated, raised, erythematous plaques with a white scaly surface ( Fig. 6-1 ). Lesions can vary in size from a few millimeters up to plaques that cover an entire extremity or large areas of the trunk. Under the scale, the skin has a homogeneous shiny appearance, and small bleeding points can appear when the scale is removed (Auspitz’s sign). Symmetrical distribution of lesions is a helpful feature in establishing a diagnosis. The lesions in chronic plaque psoriasis are characteristically located on the extensor aspects of the extremities, including elbows and knees. Other sites of predilection include the scalp. When the lesions are predominantly located in the umbilicus, axillary or intergluteal clefts, the term inverse psoriasis is commonly used. Signs of nail psoriasis are listed in Table 6-1 . Lesions themselves may have variable presentation and may be geographic, resulting from merging of many individual lesions, annular, and less commonly verrucous or hyperkeratotic. A ring of hypopigmentation may sometimes be seen around individual plaques (Woronoff’s rings). This phenomenon is usually associated with treatment response during active treatment, most commonly UV phototherapy.
| Psoriasis of the Nail Matrix | Psoriasis of the Nail Bed |
|---|---|
|
|
Guttate psoriasis is a common form of psoriasis during childhood and early adolescence that classically arises concomitant with and shortly after streptococcal throat infection. It is characterized by eruption of small scaly plaques and papules, 5 to 10 mm in size, over the trunk and proximal extremities ( Fig. 6-2 ). These eruptions are usually self-limited and resolve over 3 to 4 months. About a third of patients may develop repeated episodes of guttate psoriasis and about a third go on to develop chronic plaque psoriasis. This subtype of psoriasis has the strongest association with HLA-Cw6. Patients with chronic plaque psoriasis may experience guttate flares following streptococcal throat infections.

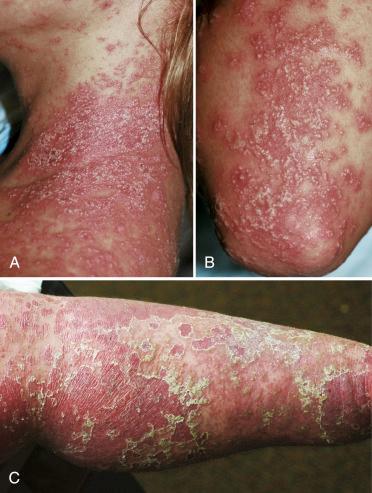
Erythrodermic psoriasis is a severe form that involves most if not all of the skin surface. Diffuse erythema is the most prominent sign, and in contrast to the thick adherent scale seen in chronic plaque psoriasis, erythrodermic psoriasis is characterized by fine delicate scale that easily flakes off ( Fig. 6-3 ). Patients with this form of psoriasis generally feel unwell. They have difficulties maintaining thermoregulation, and are often hypohidrotic due to occlusion of the sweat ducts. High-output cardiac failure may occur given the increased blood flow to the skin surface.

Pustular psoriasis is an uncommon presentation of psoriasis. Several variants exist, including generalized pustular psoriasis, acrodermatitis continua of Hallopeau, annular pustular psoriasis, and palmoplantar pustulosis ( Fig. 6-4 ). Generalized pustular psoriasis is the most severe form. This is an acute form characterized by fevers that last several days followed by a sudden eruption of sterile pustules 3 to 4 mm in size. The pustules arise on erythematous skin that may become confluent. Characteristically this form occurs in waves of fevers and pustules. It may resolve spontaneously, although treatment is usually required given the severe nature of this eruption. Generalized pustular psoriasis can occur on the background of chronic plaque psoriasis, is commonly triggered by withdrawal of treatments especially systemic steroids, and has been shown to be associated with CARD14 mutations. Whereas spontaneous pustular psoriasis is associated with mutations in the IL-36 receptor antagonist ( IL36RN ), suggesting that it belongs within the spectrum of autoinflammatory diseases.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here