Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Management of severe bone loss is one of many challenges during revision total knee arthroplasty (TKA). The restoration of a metaphyseal platform that adequately supports the subsequent joint reconstruction affects implant stability and durability. This chapter presents reconstructive techniques for handling bone loss in the setting of revision TKA with an emphasis on the emergence of modular options.
Classification of bone loss during revision TKA usually occurs intraoperatively. Although preoperative radiographs may give some insight into the degree of reconstruction required, the extent of bone loss is usually not fully appreciated until failed components or cement spacers have been removed. Classification schemes should help surgeons organize an operative plan by guiding the surgical effort and component selection during revision or reimplantation.
The Anderson Orthopaedic Research Institute (AORI) classification is a widely accepted schema that separates bone loss according to the condition of the remaining metaphysis. A type I defect of the femur or tibia has intact metaphyseal bone and usually requires little more than morselized bone grafting or cement filling to provide a platform for the revision components and joint line restoration. These small defects will not be dealt with further in this chapter.
A type II defect has a damaged metaphysis in either (IIA) or both (IIB) the medial and lateral compartments. These defects usually compromise support of the revision or reimplantation components. Type III defects result in a deficient metaphysis to or past the level of the femoral epicondyles or tibial tubercle. Historically, type II and type III defects have been treated primarily with a variety of techniques including metal augments, structural allografts, allograft–prosthesis composites, large custom components, and tumor-related megaprostheses. These treatment methods have often led to inconsistent results, with failures mainly occurring secondary to unsuccessful graft incorporation, mechanical loosening, or infection.
The emergence of noncemented metaphyseal fixation devices offers the potential to address severe bone loss and re-create a metaphyseal platform during revision TKA. These porous materials combine a high coefficient of friction, which enhances initial stability, with a favorable modulus of elasticity to produce a more physiologic transfer of forces from the prosthesis to the remaining bone. Their highly porous composition optimizes bone ingrowth for potential long-term stability and survival. In addition to promoting growth of host bone onto the external surface of these implants, their internal structure provides an excellent interface for cement interdigitation and fixation to the revision prosthesis. The modularity afforded by these devices permits implantation into a variety of bone defects and compatibility with multiple revision knee systems.
Metaphyseal fixation devices are indicated in cases in which contained or uncontained bone defects render the proximal tibia and distal femur mechanically insufficient to support revision prostheses. This usually correlates to type II and type III AORI defects. If no metaphyseal cortical rim exists in the femur or tibia, a bulk allograft or tumor prosthesis may be required. Furthermore, in young patients, for whom another subsequent revision is likely, restoration of bone stock with a structural allograft may be preferred. Traditional augments, bone grafting, or cement filling is usually adequate to address defects smaller than 10 mm and those isolated to a hemi-metaphysis.
After surgical exposure and implant removal, the existing bone defect is categorized by shape, size, and severity. Bone defects are débrided of any remaining fibrinous tissue and cement from the exposed cancellous surfaces. Intramedullary debris may be removed with the use of backbiting curettes or flexible reamers. Care should be taken to avoid overaggressive removal of cancellous bone. An assessment of the bone defect is again performed so that the preoperative plan may be confirmed or modified accordingly.
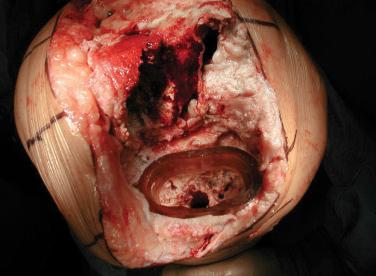
Trial cones are used to determine the appropriate device size and shape ( Fig. 23A.1 ). If necessary, more bone may be removed with a high-speed bur to allow the cone to achieve a stable interference fit with the host bone. In smaller defects, where some cancellous bone is still present, broaches that correspond to the metaphyseal cone selected may also be used. Regardless of the method used, maximal contact between bone and fixation device should be sought. Placement of an intramedullary reamer and the use of trial components with stems may be helpful in guiding proper orientation while contouring the host bone during cone preparation ( Fig. 23A.2 ).

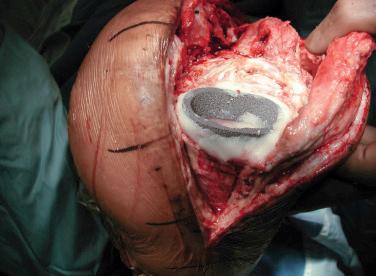
The real cone is impacted in place to achieve a stable fit. Care must be taken to avoid an intraoperative fracture during this step, especially if the remaining bone is a thin cortical shell. After the porous metal cone has been implanted, morselized bone graft or bone matrix putty is placed around the periphery of the bone–augment interface to fill the interstices where direct contact was not achieved ( Fig. 23A.3 ). This serves two purposes: to aid in bony integration and to prevent cement extrusion during pressurization.
After cone placement, the revision arthroplasty components are placed through the cones, paying close attention to their rotational alignment. Ideally, the femoral and tibial components rest flush against their respective metaphyseal cones; however, initial clinical series in which this was not achieved in every case did not show adverse mechanical consequences at early follow-up. Fully cemented stems or noncemented stems with cement solely in the metaphysis may be used according to surgeon preference or judgment regarding total construct stability. Regardless of the stem fixation selected, the metaphyseal-engaging portion of the femoral and tibial component must be cemented to the porous augment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here