Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patellofemoral pain is common, with an incidence as high as 50% in some populations. Often referred to as anterior knee pain, patellofemoral pain can be challenging for both patients and clinicians, as it can often be difficult to determine the underlying etiology responsible for the pain. Some patients with patellofemoral pain have no definable pathology. This process has been described by different names, including patellofemoral pain syndrome (PFPS) and idiopathic anterior knee pain. It is important to note that these terms to some extent are diagnoses of exclusion and should not be used to mislabel a definable disease process. It is also a misnomer to attribute all patellofemoral pain to “chondromalacia,” because in many cases, no true chondral pathology exists.
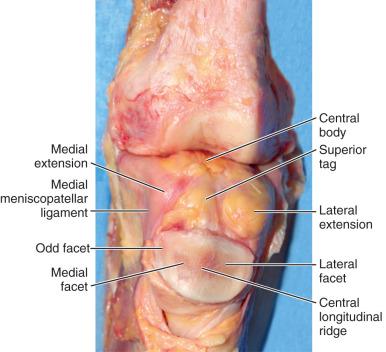
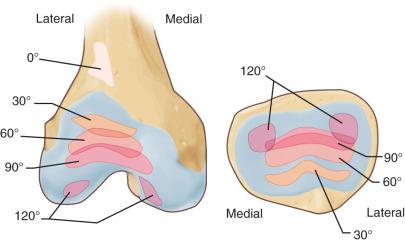
The anterior aspect of the knee has several unique properties that serve as a predisposition for pain. The patellofemoral joint itself is a sliding articulation with six degrees of freedom. Patellar tracking is defined by translation (medial/lateral), glide (superior/inferior), and tilt (medial/lateral). During initial knee flexion, the patella translates approximately 4 mm medially to engage the trochlear groove at approximately 20 degrees of knee flexion. With progressive flexion, the patella translates approximately 7 mm laterally by the time the knee reaches 90 degrees of flexion, associated with approximately 7 degrees of lateral tilt. Maximum contact between the trochlear groove and the patella occurs at 45 degrees of knee flexion.
In addition to the bony anatomy described above, there are both passive and dynamic restraints that contribute to the stability of the patellofemoral joint. Passive restraints include the osseous morphology, the medial patellofemoral ligament (MPFL), the medial patellomeniscal ligament, and the lateral retinaculum. Dynamic restraints include the vastus medialis oblique (VMO) and the vastus lateralis. A thorough understanding of these structures allows for a better ability to understand the common clinical problems associated with the patellofemoral joint as it attempts to meet its contradictory demands of providing both mobility and stability. Any imbalance to this complex network of structures can result in pain, instability, or both.
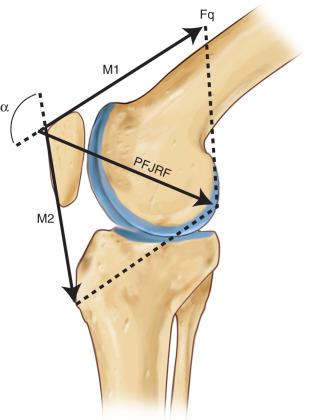
The patella serves to improve the mechanical leverage of the quadriceps muscle by increasing the lever arm and transmitting the tensile forces generated by the quadriceps to the patellar tendon. There is a delicate interplay of forces acting on the patella, which sees an incredible amount of force. In particular, the patellofemoral joint experiences joint reaction forces that become higher as the knee flexion angle increases ( Fig. 106.1 ). Squatting and jumping, for example, have been reported to create forces 7.6-times and 12-times body weight, respectively.
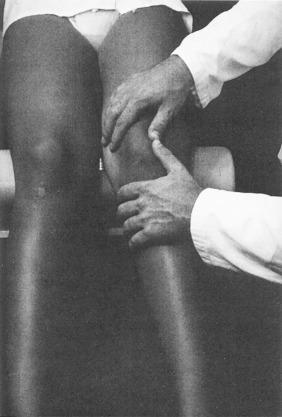
The anterior aspect of the knee also provides significant sensory feedback. In a 1998 study by Dye et al., in which SF Dye (first author of that study) underwent bilateral knee arthroscopies without anesthesia in an effort to determine conscious neurosensory characteristics of the knee, the authors described the highest subjective pain sensations in the anterior synovium, fat pad, and joint capsule. Interestingly, structures that commonly require intervention (e.g., the menisci, articular cartilage, and ligaments) were much less sensitive. Dye and colleagues also reported accurate spatial localization to palpation in the anterior structures ( Fig. 106.2 ), which correlates with previous findings about the relatively high concentration of type IVa afferent nerve fibers in the patellar ligament and retinaculum.
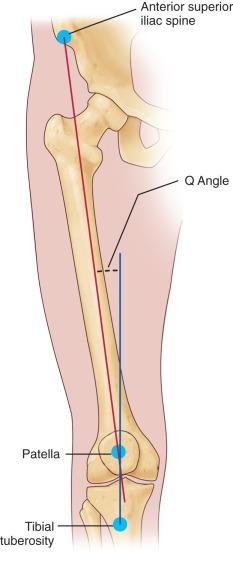
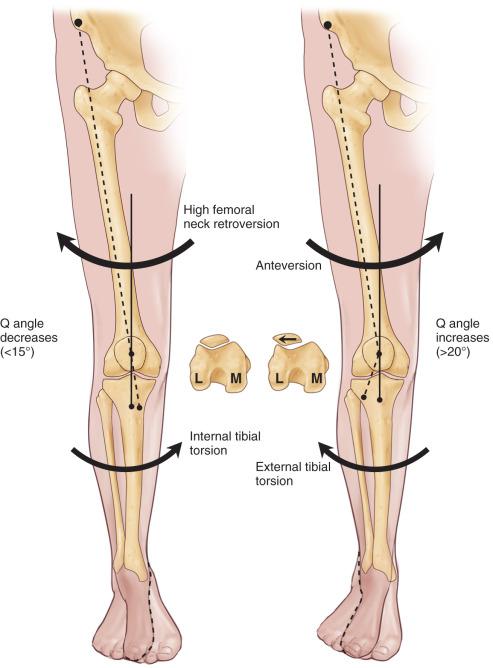
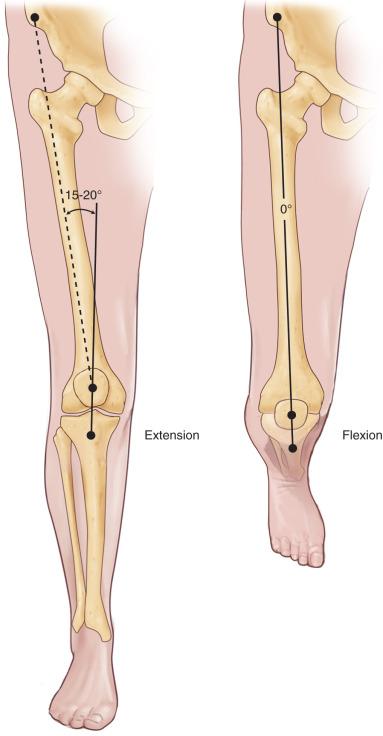
Malalignment is a commonly proposed mechanism for patellofemoral pain. Overall limb malalignment can cause or exacerbate patellofemoral joint disorders. The lines of action of the quadriceps and the patellar tendon are not collinear—the angular difference between them is called the quadriceps (Q) angle ( Fig. 106.3 ). The Q-angle is an angle formed from a line drawn from the anterior superior iliac spine to the middle of patella, and from the middle of the patella to the tibial tuberosity on a full-length weight-bearing radiograph. A normal Q-angle in males is 13 to 14 degrees and 17 to 18 degrees in females. Because of this angle, the force generated by the quadriceps both extends the knee and pulls the patella laterally. The relative magnitude of this laterally directed force is proportional to the Q-angle. External rotation of the tibia, internal rotation of the femur, and increasing knee valgus each result in an increase in Q-angle and an associated increase in the laterally directed force within the patellofemoral joint. While patella maltracking as a result of any of the above-listed factors can cause substantial pain and dysfunction, some authors have questioned the link between malalignment and patellofemoral pain. The common occurrence of pain at rest in patients with patellofemoral pain is an argument against malalignment as a major component of anterior knee pain. Dye proposed that pain is from a loss of tissue homeostasis. Increased intraosseous pressure in the patella with resultant tissue ischemia has also been proposed. Other studies suggested altered vascular flow (arterial and venous) and concomitant degenerative conditions as being associated with symptoms generation in patellofemoral syndrome.
A comprehensive history is critical to evaluation of patients presenting with patellofemoral pain. The first distinction is determining if the patient is presenting with pain or if the patient is complaining of patellar instability. While in many cases, patients have both of these complaints, when asked about their primary complaint, patients will often endorse either a chief complaint of instability with reasonable pain resolution after an acute incident, or significant pain with no symptoms of true instability. Many of the diagnoses associated with acute traumatic injuries (e.g., extensor mechanism disruption, patellar fractures, and patellar instability) are addressed in other chapters. Chronic, activity-related anterior knee pain is a common clinical complaint that occurs in a variety of knee disorders and is associated with a broad differential diagnosis ( Table 106.1 ).
| Acute Pain | Chronic Pain | Constant Pain |
|---|---|---|
|
|
|
Patients should be asked about activities that cause pain, if pain occurs at rest and/or during sleep, and if the pain is associated with swelling and/or mechanical symptoms. A history of effusions often is associated with an intra-articular problem, such as a chondral lesion, whereas the absence of effusions may suggest an extra-articular etiology of pain. Details on prior successful, as well as unsuccessful treatments, including activity modification, physical therapy, injections, and/or surgeries, should be documented. In the setting of chronic, activity-related anterior knee pain without a history of trauma, patients will often complain of discomfort while ascending or descending stairs, during deep squats, or after sitting for prolonged periods. In addition, it can be common for patients to complain of symptoms bilaterally. An onset of patellofemoral pain is also common during sudden periods of increased activity, such as during high-intensity training with military recruits.
Similar to a comprehensive history, a thorough physical examination is essential in the evaluation of patients with patellofemoral pain. Notably, it is important to appreciate that many variations exist with respect to patellofemoral anatomy. These variations can become evident during examination, and while for some patients, they may be responsible for patellofemoral pain, in other cases, they may simply be “normal” for that particular patient. The examination findings are a portion of the complex clinical picture commonly encountered in the patient with anterior knee pain.
Patients presenting with anterior knee pain should undergo a standard physical examination of both knees, including an assessment of gait and alignment, range of motion (ROM), strength, generalized ligamentous laxity, stability, and neurovascular status. In addition, the clinician should examine the ipsilateral hip, particularly in pediatric and adolescent patients, as primary hip pathology can often present as knee pain.
While there are many different techniques for performing a physical examination of the knee, it can be efficient to begin with the patient standing, then seated, and then supine (and prone, if desired). The critical aspect is ensuring that all components of the examination are completed for every patient. If beginning with the patient standing, the clinician can assess limb alignment, rotation profile, and gait. Patients with increased femoral anteversion, genu valgum, and pes planovalgus may be at an increased risk for patellofemoral pain. In addition, patients with external tibial torsion and foot pronation may experience increased patellofemoral pain. Monitoring the patient's gait as well as observing a single-leg squat can be helpful in the assessment of patellar tracking and general core strength.
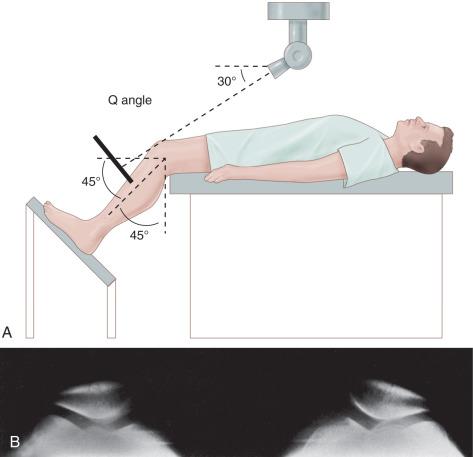
Once seated with the legs hanging off the end of the examination table, an evaluation of patellar tracking and an assessment of the Q-angle can be performed. Techniques for assessing Q-angle are variable, and can be performed with the patient in the standing, seated, or supine position. In addition, Q-angle measurements can be performed statically (static Q-angle) with the quadriceps contracted or with the quadriceps relaxed, as well as in a dynamic-fashion (dynamic Q-angle). It is important to appreciate that the Q-angle value may be affected by the relationship of the proximal femur and the amount of knee flexion ( Figs. 106.4 and 106.5 ), as well as by the method in which the assessment is performed. The Q-angle assessment with the knee in flexion may be more accurate than with the knee extended, as in flexion the patella is well-seated in the trochlear groove, whereas in extension, a laterally translated patella may falsely result in a “normal” Q-angle. Some authors have suggested a dynamic Q-angle evaluation may be of more utility than a static measurement in the evaluation of patients with patellofemoral pain, though this is controversial. An elevated Q-angle may predispose the patient to anterior knee pain, although significant variability exists. In the seated position, asking the patient to actively flex and extend his/her knee will allow for an assessment of patellar tracking. A J-sign is noted when the patella deviates laterally when the knee reaches terminal extension; the Q-angle may be less accurate in full extension in a patient with a positive J sign.
At any point during the inspection portion of the examination, the clinician should assess for muscular atrophy, particular with respect to the vastus medialis obliquus (VMO), prior surgical incisions, and the presence/absence of an effusion.
Many of the structures about the knee that may be pain generators can be directly palpated, including the patella itself, the infrapatellar fat pad, quadriceps and patellar tendon attachments on the patella, retinaculum/patellofemoral ligaments, tibial tubercle, iliotibial band, joint lines, and femoral condyles (among other structures). Palpating these structures can be helpful in determining an underlying anatomical source of pain, if one exists. In addition, palpating the patella during knee flexion/extension allows for an assessment of crepitus. In one study, 98% of adolescent patients with patellofemoral pain experienced pain with palpation over the MPFL. Notably, larger body habitus as well as guarding can make the palpation portion of the examination more difficult.
Knee ROM can be assessed in the seated, supine, or prone positions. Regardless of the position used, it is important to compare the symptomatic knee to the uninvolved knee, and to assess for baseline hyperextension. During ROM assessment, strength to resisted knee flexion and extension can also be assessed and compared side to side.
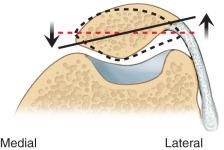
Provocative tests about the patella generally fall into two categories: tests to elicit pain, and tests to provoke instability. A variety of different tests have been described in which pressure is applied to the patella, including the patellar grind test, patellar compression test, and Clarke sign. These tests involve some variation of applying pressure on the superior aspect of the patella with the examiner's thumb, often while asking the patient to contract their quadriceps muscle. If pain occurs, these tests are considered positive for retropatellar chondral pathology. A more gently applied posterior force to the patella during flexion and extension may elicit crepitus and pain in patients with retropatellar chondral pathology ( Fig. 106.6 ). This test may help identify the location of pathology, because a more distal lesion will be painful in early flexion as the patella engages the trochlea, whereas a more proximal lesion will be painful at greater degrees of knee flexion ( Fig. 106.7 ).
Patellar instability testing is discussed in detail in Chapter 105 . The patellar apprehension test is performed by application of a laterally directed pressure to the medial aspect of the patella with the knee in approximately 20 to 30 degrees of flexion. The test is positive if the patient experiences apprehension that the patella may dislocate laterally. If the patient experiences no apprehension but his/her patella is able to be subluxated or substantially translated laterally, the patient may have baseline ligamentous laxity and the clinician should examine the opposite knee for similar findings. Notably, while patients with patellofemoral pain may experience pain during apprehension testing, pain itself does not represent a positive test for instability. Manipulation of the patella in the transverse plane may reveal a tight retinaculum, as evidenced by a lack of motion ( Fig. 106.8 ). The patellar tilt test should also be performed as an assessment for a tight retinaculum and may have some utility in determining possible interventions. The Ober test is useful to assess for iliotibial (IT) band tightness that can contribute to anterolateral knee pain as well as patellar maltracking.
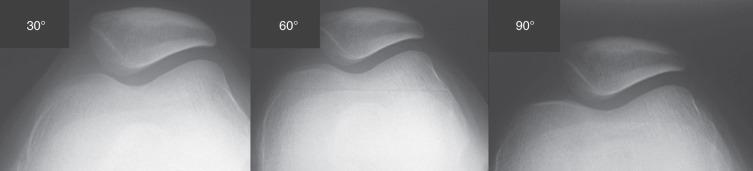
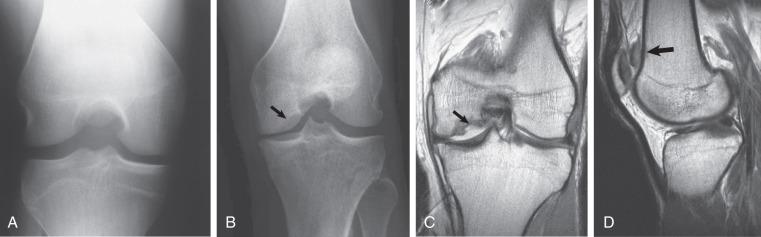
Imaging studies, including radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) can be helpful in the valuation of patients with patellofemoral pain. Radiographs, including anterior-posterior (AP), lateral, and axial (merchant or sunrise), are useful for evaluating the osseous morphology of the patellofemoral and tibiofemoral joints, as well as for identifying signs of arthritis. The lateral radiograph is perhaps the most useful in the evaluation of the patellofemoral joint, as it is useful for determining patellar height ( Fig. 106.9 ) as well as trochlear dysplasia. Patella height can be determined via several different techniques, including the Caton-Deschamps index, Insall-Salvati ratio, Blackburne-Peel ratio, and the relationship of Blumensaat line to the inferior pole of the patella at 30 degrees of knee flexion. Patients with patella alta may have a predisposition to instability, whereas patients with patella baja may encounter increased patellar load and the subsequent risk of degenerative conditions. The lateral view is also helpful for identifying abnormal trochlear morphology according to the Dejour classification system. In the Dejour system, trochlea dysplasia is classified as types A, B, C, or D (most severe), depending on if a crossing sign, supratrochlear spur, and/or double contour are present. Axial views such as the Merchant view ( Fig. 106.10 ) can help determine sulcus angle as well as the depth of the groove. Murray et al. demonstrated that the lateral and axial views are the most useful views for evaluating instability and noted a high sensitivity of the lateral view for detecting prior dislocation; thus a normal lateral radiograph can help rule out instability as a component of anterior knee pain in some patients. The axial view is also useful for evaluating patellar tilt and subluxation. Different parameters have been defined, and the clinical utility of these parameters remains uncertain ( Fig. 106.11 ). When evaluating axial radiographs, it is important to note that the sulcus of the trochlea lies lateral to the midline of the femoral condyles and is not completely centered as previously thought. Interestingly, articular congruity may exist on magnetic resonance arthrogram (MRA) imaging, even when osseous incongruity appears on plain radiographs.

Advanced imaging with CT can be very helpful given its ability to analyze the three-dimensional relationships of the patellofemoral joint. Data from CT imaging can help identify patellar tilt and tibial tuberosity–trochlear groove (TT-TG) value. Notably, indications for CT imaging in patients without patellar instability are limited, as patellar tilt and TT-TG measurements are most useful in the evaluation of patients experiencing patellar subluxation or dislocation events (see Chapter 105 for details on these measurements).
MRI is the imaging modality of choice for evaluating the articular cartilage and underlying subchondral bone and soft tissue structures such as the MPFL ( Fig. 106.12 ). One study demonstrated that edema in the superolateral fat pad on MRI correlates with other anatomic parameters (e.g., trochlear morphology and patellar alignment) suggestive of patellar maltracking or impingement in the young, symptomatic patient. Data points helpful for evaluating patellar instability, including TT-TG (originally described on CT scan) and TT-posterior cruciate ligament (TT-PCL), can be taken on MRI. In addition, lateral trochlear inclination and medial trochlear inclination measurements can be taken on MRI, which may be more accurate than the sulcus angle in identifying abnormal trochlea morphology.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here