Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
There is a subset of patients with refractory epilepsy in whom palliative interventions are indicated.
Palliative surgical procedures for epilepsy are not curative, but they lessen disease burden and can improve quality of life for patients with refractory epilepsy.
Identification of seizure focus and its relationship to eloquent cortex is paramount in palliative surgery.
Epilepsy affects approximately 1% of the population. While the majority of patients achieve seizure freedom by medical therapy alone, 30% to 40% of all new cases of epilepsy ultimately become refractory to treatment. , Further diagnostic evaluation can identify 25% of patients with seizure foci that are amenable to surgical intervention. , Resective surgery offers a 50% to 70% (extratemporal versus temporal) chance of seizure freedom in carefully selected patients. Despite exhaustive diagnostic and interventional testing, approximately one-third of patients remain refractory to treatment. In this population of patients, palliative surgical procedures including neuromodulation can be reasonable options aimed at seizure reduction. Surgical treatment of epilepsy should be considered when (1) the seizures have not been controlled by adequate attempts at treatment with maximally tolerable doses of correct anticonvulsant medications; (2) the seizures interfere with psychological and intellectual development, employment, or social performance; (3) all potentially epileptogenic areas have matured and there is no tendency toward spontaneous regression; and (4) the patient is strongly motivated to cope with an exhaustive diagnostic regimen and a lengthy operative procedure, possibly under local anesthesia.
The length of time between diagnosis of medically refractory epilepsy and surgical evaluation has decreased as the superior surgical results have been widely recognized. While the previous dogma of unsuccessful medical therapy was lengthened up to 5 years, the Early Randomization Surgery for Epilepsy Trial (ERSET) established unsatisfactory seizure control with medical therapy at 2 years as sufficient to warrant referral to epilepsy surgery. , In exceptional cases, urgent cortical resection may be considered for the relief of status epilepticus.
This chapter reviews palliative surgical options for patients with refractory epilepsy in whom traditional epilepsy surgery is not an option or has failed. Patients included in this category have multifocal epilepsy, seizure foci in eloquent cortex, or syndromic seizure pathologies. The reviewed procedures are reserved as end-line surgical options; however, it is imperative that they are part of the surgeon’s armamentarium, particularly in light of accumulating evidence supporting their efficacy in seizure reduction.
The corpus callosum is the largest white matter tract connecting the two cerebral hemispheres. The foundational premise behind transection of corpus callosum is prevention of seizure propagation to the contralateral hemisphere. First described in a series of 10 patients in 1940 by van Wagenen and Herren, the technique was created after observations of seizure improvement in epileptic patients in whom the corpus callosum had been destroyed by tumor or stroke. Despite the promising initial results, the technique was largely abandoned for 20 years before resurfacing as a plausible technique for non–temporal lobe epilepsy.
Modernization of surgical technique and evolving technologies have led to modification of corpus collosotomy. These include the use of limited anterior callosotomies, or staged procedures, coupled with image guidance that have produced excellent outcomes in multiple series. , However, the introduction of vagal nerve stimulation (VNS) has resulted in a decline in the use of the more invasive callosotomy in recent decades. More recently, the technique has seen a revival owing to the use of laser interstitial thermal therapy as a less invasive method of obtaining interhemispheric disconnection.
At the time van Wagenen and Herren published their groundbreaking article, the limitations of resection surgery for cases with multiple epileptogenic sites were already well recognized. The investigators conceptualized “seizure isolation” to one hemisphere after observing a series of patients in whom seizures improved after destruction of the corpus callosum. The cases had a variety of etiologies including glioblastoma, meningioma, and cerebral infarcts. Although the investigators acknowledged the extensive list of complications previously reported from transection of the corpus callosum, they believed the advantages of seizure control justified the added risk. The article reported 10 cases of corpus callosotomy with favorable outcomes, albeit with limited follow-up. The procedure involved a frontal parietal craniotomy and subsequent callosotomy of variable length. Despite the success reported by van Wegenen and Yorke, the next report of a callosotomy for treatment of refractory epilepsy was not published until 1965 by Bogen and colleagues. A series of successful case reports , and the application of microsurgical technique by Wilson and Reeves and their associates , resulted in improved results and wide acceptance of the procedure by the 1980s. Since that time, magnetic resonance imaging (MRI) has markedly improved preoperative evaluation and postoperative assesment. To date, multiple large studies have shown favorable long-term results for children and adults with various pathologic conditions. , , The addition of radiosurgery for corpus callosotomy has had positive results in several small series ; however, additional patients and long-term follow-up are required to uncover potential side effects of this treatment modality.
Patients being considered for corpus callosotomy must be evaluated by a multidisciplinary team consisting of epileptologists, neurosurgeons, neuroradiologists, and neuropsychologists. After failure of medical therapy for 2 years, meaning continued disabling seizures despite maximal medical therapy, or unacceptable medication side-effect profile, the patient’s epilepsy is deemed to be refractory, and surgical procedures may be considered. Evaluation proceeds as with all neurosurgical patients with a thorough clinical history, physical examination, and extensive analysis of previously attempted treatments. Electroencephalography (EEG) is used to better characterize the nature, frequency, and location of seizure activity. Corpus callosotomy is a palliative procedure and does not achieve a cure, and thus it is not a suitable option for patients with resectable seizure foci. Hence a focal resectable lesion must be ruled out. Additional testing with video-EEG, epilepsy protocol MRI, positron emission tomography (PET), single-photon emission tomography (SPECT), and magnetoencephalography (MEG) is done.
Corpus callosotomy has shown the best results in patients with atonic seizures, ranging from 80% to 100% reduction in drop attacks. , Other seizure semiologies that are appropriate for callosotomy include unresectable or multifocal seizure foci. Benefit has also been shown in patients with Lennox-Gastaut syndrome, Rasmussen encephalitis, and infantile hemiplegia. , In patients who have lateralizing conditions such as Rasmussen encephalitis or infantile hemiplegia, a disconnection intervention may be of greater benefit if a functional hemispherectomy jeopardizes motor or visual processes. In recent years, VNS before callosotomy has gained favor owing to its less invasive nature. Patients who fail VNS are still candidates for callosotomy and have been shown to respond to disconnection surgery. , ,
See , , .
In studying preoperative imaging, it is critical to be familiar with the normal anatomy and to pay special attention to the regional cerebral vasculature. Preoperative contrast-enhanced high-resolution MRI, magnetic resonance angiography, and magnetic resonance venography allow a detailed understanding of the targeted white matter tracts and the relationship to the surrounding vasculature. Close attention is paid to the draining veins and the superior sagittal sinus. The craniotomy should be placed in an area relatively devoid of draining veins, allowing for better exposure to avoid potential complications associated with venous compromise. Preoperative imaging can also identify hyperostosis (such as seen in patients who have received long-term phenytoin treatment), which may result in deviation of the original craniotomy site and possible avoidance of exposing the superior sagittal sinus in lieu of injury risk.
Patients undergoing callosotomy are young and typically do not have medical conditions that would contraindicate general anesthesia. All antiepileptic medications should be continued before and during the surgical procedure. Sedation should be in keeping with general principles of neuroanesthesia. Electrocorticography (ECoG) is not performed during callosotomy, and thus restricted use of anesthetics and paralytics is not necessary. If the patient’s head is raised during the procedure, a precordial Doppler ultrasound probe is placed on the patient’s chest and its readings are monitored throughout the case because of the risk of air embolus. Once intubated and sedated, the patient is placed in three-point clamp fixation and positioned in the supine position, maintaining the head straight to ease the surgeon’s anteroposterior orientation. Lastly, the patient is registered with frameless stereotactic neuronavigation.
Barring any vascular anatomy identified on preoperative imaging that would favor a particular side of access, the approach is usually performed on the nondominant side to limit the risk of injury to the dominant hemisphere. Multiple types of incisions may be used including linear, coronal, or U-shaped. The craniotomy is located with the midpoint just anterior to the coronal suture, extending just lateral to midline on the contralateral side. The location of craniotomy may be adjusted to avoid exposure of cortical veins. Once the craniotomy is completed, the dura is opened laterally and retracted toward the sinus ( Fig. 96.1 ; see ). Excessive retraction of dura should be avoided to prevent occlusion of the superior sagittal sinus.
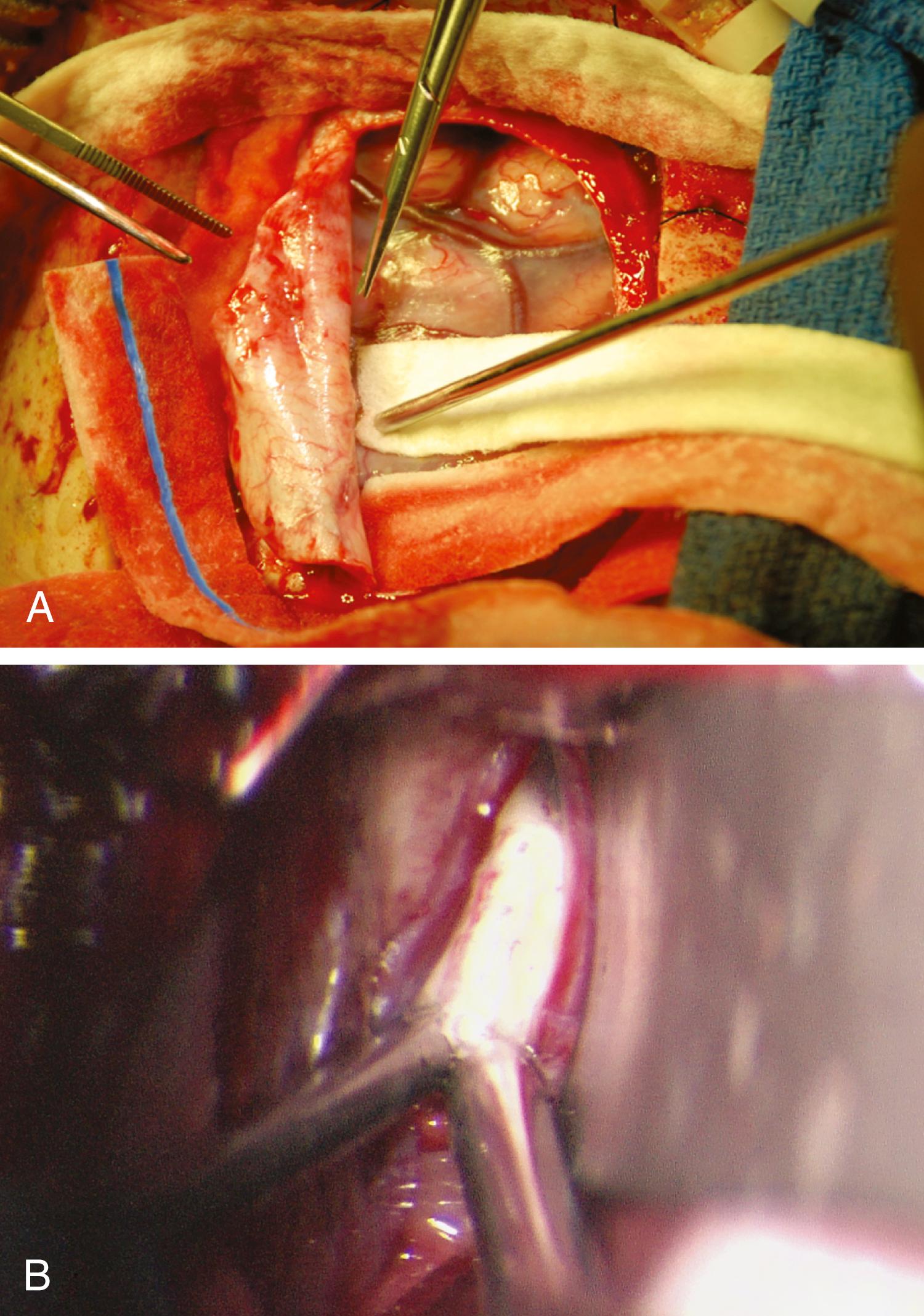
The interhemispheric fissure is entered and carefully divided. A self-retaining retractor may be useful for visualization. During the approach, care is taken to identify the callosal marginal arteries and then the pericallosal arteries. If adhesions between the frontal lobes must be divided, it is important that the division stay medial to the arteries to avoid disrupting small perforators. The corpus callosum is identified by its characteristic glossy white appearance. Adhesion of cingulate gyri is quite common in patients undergoing this procedure, perhaps secondary to multiple falls and head injuries. It is important to distinguish the corpus callosum from fused cingulate gyri and to take care to separate the frequently adherent cingula.
Once the corpus callosum is identified, stereotactic guidance can be used to confirm its location and determine the posterior extent of the sectioning. Callosotomy begins 3 cm posterior to the genu, where the midline is easier to identify. Resection proceeds ventrally to the midline leaves of the septum pellucidum and then anteriorly to the anterior commissure. A combination of suction and bipolar cautery, microdissector, or carbon dioxide laser can be used to perform the disconnection. Care is taken to identify and preserve the anterior cerebral arteries and associated perforators during the anterior dissection. If complete disconnection is the goal, a larger craniotomy needs to be performed, or a complete callosotomy can be accomplished with multiple craniotomies. During a posterior callosotomy, the internal cerebral veins and the vein of Galen just below the splenium pose a hazard; identification of the deep cerebral vein through the arachnoid signals completion of the dissection. In addition, in the posterior callosal division, it is important that the dissection remains midline and is advanced cautiously to avoid injuring the fornices, located just below the corpus callosum.
Corpus callosotomy is an effective treatment for patients with medically refractory epilepsy of multiple seizure types. , , , , A caveat to be considered in studies involving corpus callosotomies is that there is heterogeneity in the types of seizures addressed and the extent of disconnection performed. Patients with atonic seizures benefit the greatest and may become free of drop attacks entirely. Oguni and colleagues reported a series of 43 patients who underwent anterior corpus callosotomies with a greater than 75% reduction in drop attacks in 33% of patients. In 1996, Rossi and associates reported a series of 19 patients who experienced a 47% freedom from drop attacks after the procedure. The same year, Maehara et al. reported cure of drop attacks in 25% of adult patients and 42% of pediatric patients. Five years later Maehara and Shimzu reported achieving a more than 90% reduction in drop attacks in 85% of 52 patients. Despite these positive results in patients with atonic seizures, longer follow-up is required to assess long-term seizure control. A meta-analysis reviewing long-term results for all epilepsy surgeries found that 35% of patients undergoing callosotomy were without drop attacks after 5 years.
Positive results have also been reported for other types of generalized seizures. Wong and colleagues, in reviewing their series of 268 pediatric patients with a variety of seizure types, demonstrated a greater than 50% reduction of seizures in more than half of patients. Cukiert and colleagues reported a series of 76 patients who underwent extended callosotomy sparing only the splenium. The response rate was 91%, defined as a greater than 50% reduction in seizures. Among the seizure types, atonic seizures had the best response rate at 92%, and myoclonic seizures had the poorest response rate at 27%. Additional studies have shown modest improvements in rates of absence, tonic-clonic, and myoclonic seizures after callosotomy. , A contemporary meta-analysis of 12 studies, all retrospective in nature but one, revealed similar results of 88.2% seizure control after a total corpus collosotomy and seizure control rate of 58.6% in patients with anterior callosotomy alone. The study also confirmed that patients with drop attacks had the greatest benefit.
There is considerable debate regarding the ideal length of the callosotomy, with multiple series showing benefit for both partial and complete disconnection. , , , , It is generally accepted in the literature that more extensive callosotomies offer a greater chance of seizure reduction albeit with the possibility of greater morbidity. For this reason, callosotomies are usually performed in a staged manner. Patients with low functional status who are unlikely to be impaired by disconnection syndromes may benefit from a single-stage, complete callosotomy and thereby avoid additional surgery. Younger age at seizure onset and at surgery has been shown to be a predictor of both seizure control and lower rates of adverse side effects. , , Younger patients are more resilient and are able to avoid the repeated trauma associated with a life of drop attacks. Higher IQ has also been shown to be a positive predictor of favorable outcome. Low IQ is often associated with severe bilateral structural impairment, which results in poor seizure control with both medications and surgery. However, mental retardation is not a contraindication to surgery in the population that is most in need of seizure relief. , A durability study of patients who underwent collosotomy with a mean follow-up of 14 years revealed the reduction of seizures by 50%, drop attacks by 65%, generalized tonic-clonic seizures by 53%, and complex partial seizures by 50%. The study was congruent in that drop attack seizures had the best response and durability, with better outcomes seen in early intervention cases.
The results of callosotomy have been compared directly with VNS. Nei and colleagues compared seizure control and complication rates in 53 patients undergoing corpus callosotomy and 25 patients undergoing VNS. Although patients who underwent callosotomy had better seizure control, there was also a permanent complication rate of 3.8% compared with no complications in the group undergoing VNS. Despite the proven effectiveness of callosotomy, the complications associated with craniotomy and the side effects of disconnection syndromes have made VNS more attractive as an initial procedure for patients with refractory epilepsy. As previously mentioned, patients in whom VNS fails are often later referred for callosotomy. ,
Complications associated with corpus callosotomy are attributed to the operative approach or syndromes that develop as a result of the disconnection itself. Despite the invasive nature of the operation, operative approach complication rates remain relatively low, ranging from 2.4% to 6%. Complications include epidural hematoma, subdural hematoma, meningitis, and deep venous thrombosis. , , ,
Complications associated with disconnection of the hemispheres include mutism, acute disconnection syndrome, posterior disconnection syndrome, and split-brain syndrome. There are a wide variety of disconnection syndromes, and they may be acute or chronic. Disconnections of the prefrontal lobe may demonstrate symptoms identical to those of supplementary motor area syndrome in the immediate postoperative period. This syndrome is characterized by paresis of the nondominant leg, incontinence, and decreased spontaneous speech. Acute callosal disconnection symptoms have been reported to occur in 89% of patients in a series of extended callosotomies. The duration and severity of the syndrome are shown to be worse for patients undergoing single-stage, complete callosotomy. The patient may also have apraxia of the nondominant hand, nondominant hypotonia, repetitive grasping with the nondominant hand, and bilateral Babinski response. In the most severe form of supplementary motor area syndrome, patients are minimally reactive to the environment despite being awake, with symptoms lasting days to weeks. Injury to the vasculature during the approach, the fornices, the septal area, or the hypothalamus is rare. External hydrocephalus can result if the lateral ventricle is entered during the callosal section.
Several months after callosotomy, patients typically appear to be at their neurological baseline. However, detailed testing detects persistent deficits that are referred to as chronic disconnection syndromes. Manifestation of chronic disconnection syndrome is related to the extent of the callosotomy. Chronic syndromes include alien hand syndrome owing to frontal lobe disconnection, poor sound localization owing to temporal lobe disconnection, tactile dysnomia and pure word blindness owing to parietal dysfunction, and visual suppression owing occipital lobe isolation. Reported rates of symptomatic disconnection syndromes have ranged from 45% to 80%, with adults having higher rates than children. Because of the anatomic configuration of the corpus callosum, patients undergoing complete or posterior callosotomy are at higher risk for development of permanent interhemispheric sensory dissociation. The surgeon must also recognize and discuss the increased risk of language deficits in patients with crossed cerebral dominance. ,
We present two cases illustrating corpus callosotomy. The first case shows a partial (anterior) disconnection, and the second case shows a complete disconnection.
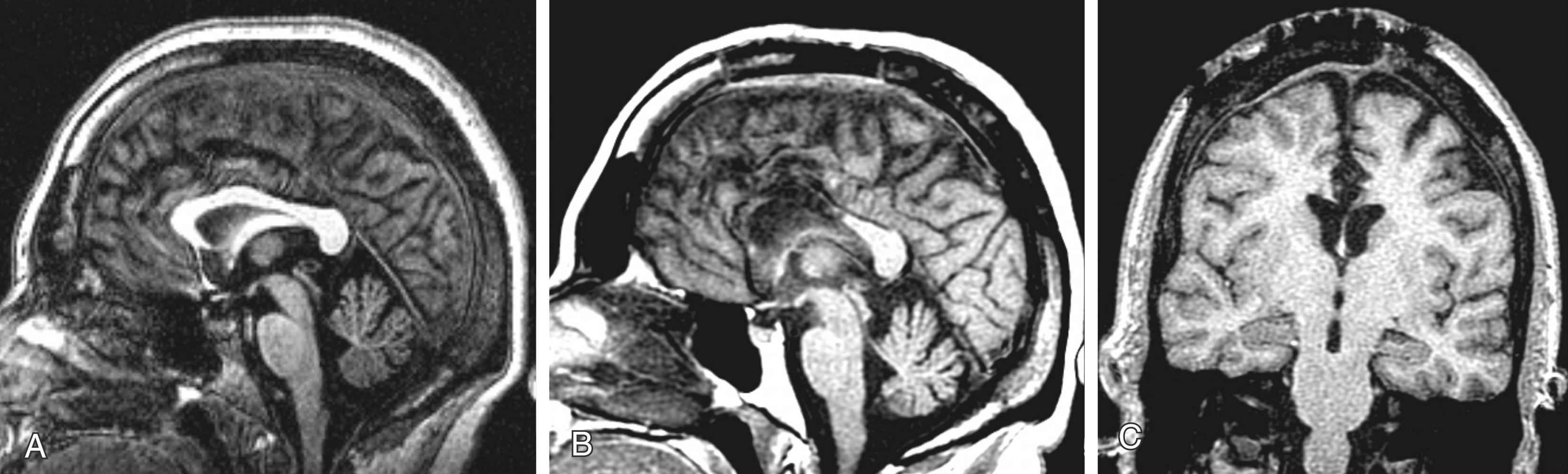
In case 1, a 32-year-old right-handed woman with a history of drug-resistant idiopathic generalized epilepsy underwent an anterior corpus callosotomy. She had three different seizure types: absence seizures, myoclonic jerks, and generalized tonic-clonic seizures. MRI showed no abnormalities, and neuropsychological evaluation demonstrated visuospatial impairment. Video-EEG demonstrated bifrontal generalized spikes and polyspike waves, with shifting predominance from side to side. She had previously tried VNS, which was not effective, and therefore an anterior corpus callosotomy was planned. Figure 96.2 shows preoperative and postoperative MRI scans. After the procedure, seizures were less severe, and the postictal period was significantly shorter.
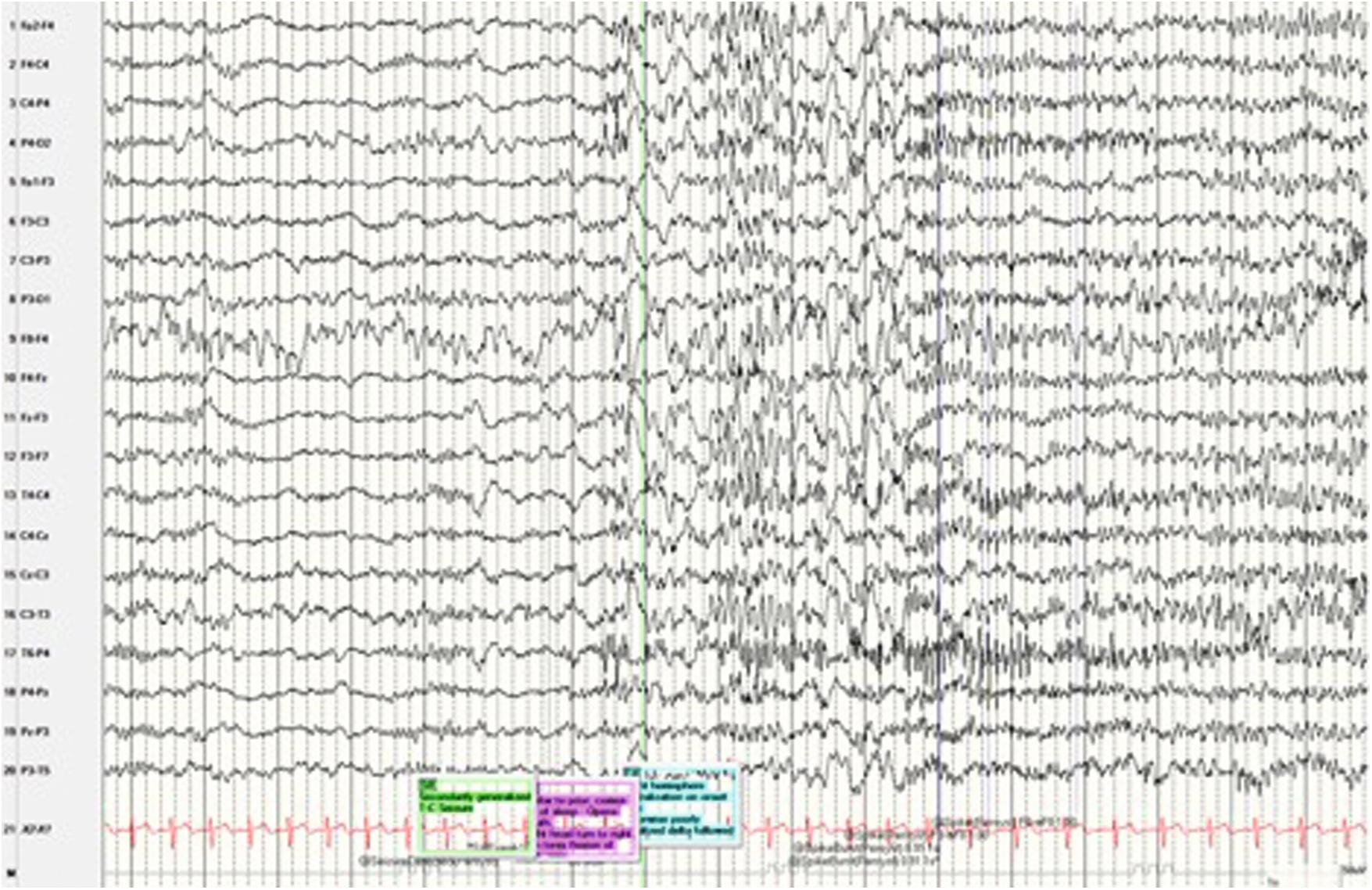
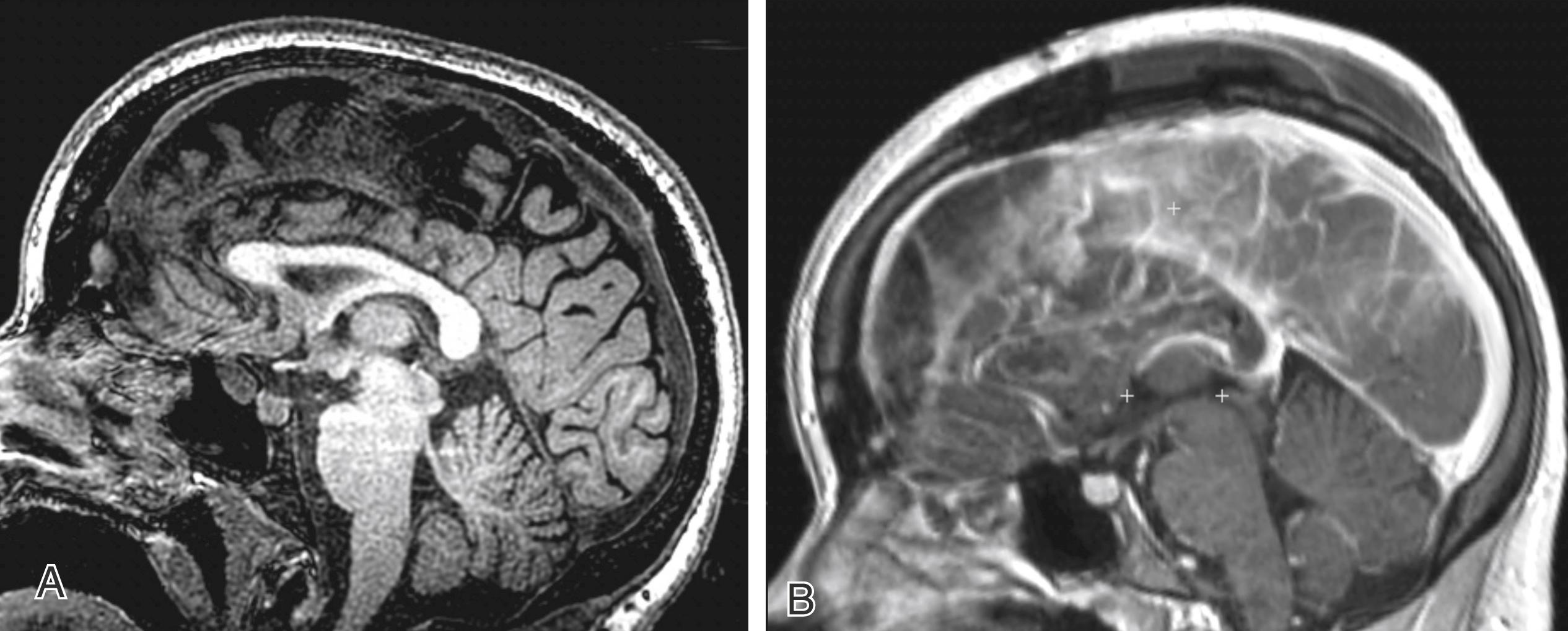
In case 2, a 20-year-old right-handed woman with a history of autism and intellectual disability (IQ of approximately 40) with drug-resistant epilepsy underwent a complete corpus callosotomy after being evaluated by the multidisciplinary epilepsy surgery team. She had two types of seizures: focal with impaired awareness seizures and secondarily generalized tonic-clonic seizures. MRI showed no abnormalities, and neuropsychological evaluation showed an estimated verbal intelligence of 40 (<40th percentile) with an age equivalent of 2 years 5 months. Video-EEG demonstrated right hemisphere lateralization on onset, building to right midline to fronto-parietal spiking then secondary generalization ( Fig. 96.3 ). Based on her low functional status and the abnormal EEG findings also on the parietal lobe, a decision was made to perform a complete disconnection, avoiding a second procedure in the future. Figure 96.4 shows preoperative and postoperative MRI scans. After the procedure, there was a seizure-free period of 5 months, following which seizure frequency was significantly decreased and seizure duration became shorter.
Corpus callosotomy is an established surgery to address medically refractory epilepsy. It has been a last-line surgical intervention for multiple seizure types but has shown the best results in patients with atonic and tonic seizures. A tailored microsurgical approach has decreased postoperative complications of disconnection syndromes. Corpus collosotomy is a palliative surgical procedure for epilepsy, and less invasive VNS can be trialed before consideration of this surgery. With proper patient selection, callosotomy holds a place in the treatment of patients with refractory epilepsy with significant and durable results.
Surgical resection of seizure foci in noneloquent cortex is a relatively straightforward surgery. However, resection of epileptic foci in eloquent cortex is much more difficult. Even with proper intraoperative mapping for language and motor, the deficits may be unacceptable. MST surgery was developed in such situations to address the lateral spreading depolarization of an eloquent area seizure focus. The surgical strategy revolves around the anatomic arrangement of the cortex. The vertical column organization of the cerebral cortex is perpendicular to the gray matter spread of seizures. The aim of the surgery is to disrupt the gray matter columns in eloquent cortex to inhibit synchronization and spread of seizures, while at the same time causing minimal damage to the functional unit of the cortex. This section reviews the history and development of MSTs including hippocampal transection for mesial temporal lobe epilepsy, highlighting patient selection, indication, surgical technique, and outcomes.
In the 1930s, two treatments emerged for patients with chronic epilepsy that brought hope for better seizure control. The anticonvulsant effects of phenytoin were discovered in 1938, and it was effective in controlling the seizures of many patients with chronic epilepsy. At the same time, Penfield at the Montreal Neurological Institute expanded the use of surgical resection of seizure foci, primarily in the temporal lobe, for “psychomotor seizures.” News of Penfield’s success spread, and in 1951, Bailey and Gibbs at the University of Illinois Neuropsychological Institute reported their results of temporal lobectomy for psychomotor seizures guided by EEG findings. One class of patients who would not benefit from standard surgical therapy consisted of patients with a seizure focus in eloquent cortex because excision of this seizure focus would lead to unacceptable deficits.
Several discoveries in neuroscience in the 1950s and 1960s, along with his own work, led Morrell to believe that nonresection surgical therapy might be safe and effective. The first discovery, by Mountcastle, , was that gray matter in the neocortex was organized in vertical functional columns with afferent and efferent connecting fiber tracts oriented perpendicular to the surface of the cortex. Although some horizontal interconnections between neurons exist, experiments by Sperry and colleagues demonstrated that if these horizontal connections are interrupted in the cat visual cortex, the function of that cortex is largely preserved. These investigators placed mica plates in gray matter perpendicular to the cortical surface, thus severing the horizontal fibers in the cortex but preserving the vertical fibers. Visual testing showed preservation of function. Experiments by Morrell , demonstrated the role of these horizontal fibers in the synchronization and spread of an epileptic discharge. He found that in the monkey, he could inhibit the seizure focus but preserve motor function when he transected through a penicillin-induced seizure focus in the motor cortex. These findings led to a long-term collaboration in the surgical treatment of seizure foci in eloquent cortex between the neurologist Morrell and Whisler, a neurosurgeon who had worked at the Illinois Neuropsychological Institute with Gibbs. By 1989, Morrell and colleagues had used MSTs to treat more than 120 patients. Since the report of their original series, many other epilepsy centers have also reported their findings, some with less favorable outcomes ( Table 96.1 ). , , More recently, with the advent of neuromodulation techniques (discussed later in the chapter), use of MSTs as a palliative technique has declined.
| Study | N | Significant Improvement | No Significant Improvement | Neurological Complications | |||
|---|---|---|---|---|---|---|---|
| MSTs Only | MSTs/Resection | MSTs Only | MSTs/Resection | n | Type ( n ) | ||
| Shimizu et al. | 12 | 12 | — | 0 | 0 | 0 | — |
| Devinsky et al. | 3 | 0 | 0 | 0 | 0 | 2 | Mild speech deficits (2) |
| Sawhney et al. | 21 | 8 | 12 | 1 | 0 | 0 | — |
| Wyler et al. | 6 | 6 | — | 0 | — | 1 | Mild motor deficits (4) |
| Mild speech deficits (2) | |||||||
| Hufnagel et al. | 22 | 4 | 15 | 2 | 1 | 7 | Overt speech deficits (2) Mild dysnomia (7) Moderate dysphasia (1) |
| Smith | 100 | 25 | 56 | 7 | 12 | 17 | Sensorimotor (13) |
| Schramm et al. | 20 | 9 | — | 11 | — | 0 | — |
| Shimizu et al. | 17 | — | 17 | — | — | 0 | — |
| Spencer et al. | 211 | ||||||
| Patients with simple partial seizures | 85 | 14 | 47 | 5 | 19 | 10 | Aphasia, memory, hemiparesis |
| Patients with complex partial seizures | 113 | 17 | 71 | 4 | 21 | 37 | Aphasia, memory, hemiparesis |
In patients in whom preoperative work-up reveals that a seizure focus is located in functional eloquent cortex, MSTs may be an option. MST surgery has been used to treat patients with epileptogenic lesions of the speech, motor, or primary sensory cortex. MST surgery has also been used for the treatment of Rasmussen encephalitis; however, it is of questionable benefit for progressive disease states when the underlying disease cannot be controlled. , , MSTs have also been used to treat carefully selected patients with epilepsia partialis continua, Landau-Kleffner syndrome, and status epilepticus. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here