Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Palliation is reserved for symptomatic iAVMs deemed untreatable with surgery.
Palliation includes partial embolization or staged stereotactic radiosurgery.
The goal of palliation is to alleviate ischemic symptoms, headache, or seizures in patients with noncurable iAVMs.
New innovative transvenous embolization techniques may increase the number of iAVMs that are potentially curable.
Observation is a very reasonable option for high-risk iAVMs.
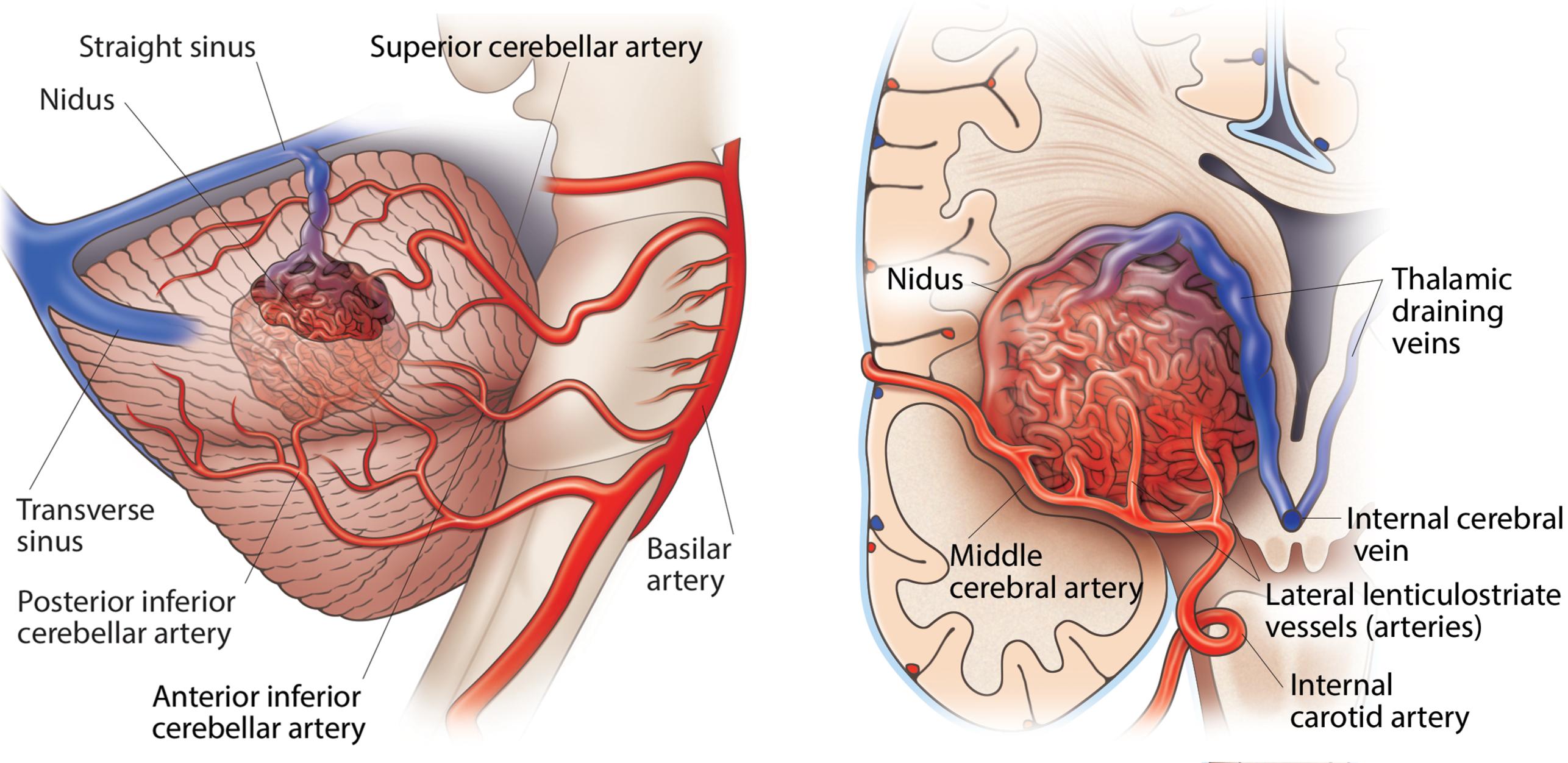
Defining nonresectable intracranial arteriovenous malformations (iAVMs) involves complex decision-making that weighs the risks of the lesion’s projected natural history vs the risks of resection while also considering the impact of endovascular and radiosurgical treatment modalities. Given the anatomical, pathological, and hemodynamic heterogeneity of iAVMs, evaluating these risks can prove difficult. Ultimately, in order for an iAVM to be defined as nonresectable, attempts to resect it must pose a risk of permanent morbidity or mortality that is significantly greater than the risks of not doing so. Two examples of nonresectable iAVMs are shown in Fig. 17.1 .
Both the most common and the most feared consequence of having an iAVM is intracranial hemorrhage. For patients with iAVM-associated hemorrhage, the 1-month case fatality is 11%, and poor outcomes occur in 40% of individuals with hemorrhagic events. The risk of hemorrhage has been associated with several factors that must be considered.
For untreated, previously unruptured iAVMs, hemorrhage rates are approximately 1%–3% per year. However, for previously ruptured iAVMs, the risk can be significantly higher, especially during the first year after rupture. Indeed, a history of hemorrhage is the most consistent risk factor for future hemorrhage. One meta-analysis showed hemorrhage rates of 2.2% for unruptured iAVMs compared to 4.5% for ruptured ones. Another study found hemorrhage rates of 2.2% vs 4.3%, respectively, supporting these data. Yet another analysis showed hemorrhage rates from 2.1% to 4.1% per year, with the highest rates among those with prior hemorrhage.
Other important factors that may elevate hemorrhage risk include deep venous drainage, fewer draining veins, deep and infratentorial nidus location, larger nidus size, associated arterial aneurysms, and venous varices. These angioarchitectural features can be evaluated by angiography to better assess the level of risk for the individual patient. While there are several well-described genetic conditions associated with iAVMs and hemorrhage risk, there are mixed data about other patient characteristics, with some suggestion that young age and female sex may increase iAVM rupture risk.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here