Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
* Disclosure: Dr. Coselli serves as a consultant for Vascutek Ltd., a subsidiary of Terumo Corporation.
Frequently, and in a variety of clinical settings, cardiovascular surgeons encounter occlusive disease involving the branches arising from the aortic arch. As a result of the increasing average life expectancy of human beings, there is a growing subset of older patients who are found to have brachiocephalic occlusive disease incidentally during preoperative evaluation for more routine cardiac surgery. In addition, the widespread use of the internal thoracic artery (ITA) as the conduit of choice for patients with surgically correctable coronary artery disease has created a subset of patients who, postoperatively, are susceptible to coronary ischemia from occlusive disease involving the subclavian vessels, which produces coronary-subclavian steal syndrome.
Although atherosclerosis is the most common cause of brachiocephalic occlusive disease, other, less common causes of aortic branch occlusive disease, such as Takayasu arteritis and radiation-induced arteritis, can also manifest as occlusion of the aortic arch branch vessels that occasionally requires surgical intervention. Regardless of the cause of intrathoracic brachiocephalic occlusive disease, advancements in diagnostic imaging, technical improvements in end-organ protection, the development of endovascular techniques, strategic anesthetic management, and a better understanding of critical care all have enabled cardiovascular surgeons to perform a wide variety of procedures to treat patients with this problem with low operative risk.
Concomitant occlusive disease involving coronary and carotid arteries can pose particular challenges for cardiovascular surgeons, and the ideal treatment strategy for these combined lesions remains controversial. Treatment algorithms for concomitant coronary and carotid occlusive disease have recently expanded with the advent of endovascular techniques. Current strategies for treating patients with this problem include synchronous revascularization, staged procedures, hybrid approaches using endovascular devices, and medical treatment.
Atherosclerosis of the aortic arch has been recognized recently as a significant contributor to and an independent predictor of embolic stroke and generalized atherosclerotic disease, and it is the most common cause of intrathoracic brachiocephalic occlusive disease. In addition to its well-known associations with cigarette smoking, peripheral arterial occlusive disease, dyslipidemia, hypertension, male sex, and diabetes mellitus, atheroma has also been associated with elevated levels of fibrinogen and homocysteine. Aortic arch atheroma, first seen early in the patient's adult life, is characterized by gradually increasing severity. The progression of aortic arch atheroma to brachiocephalic occlusive disease is influenced directly by the presence of aggravating risk factors.
Two important pathologic sequelae directly related to aortic arch plaques are atheroembolism and thromboembolism. Within the aging aortic arch, a variety of pathophysiologic processes occur: these include calcification, the destruction of smooth muscle and elastic fibers (including the loss of internal elastic lamina), the formation of thrombi, and most importantly, the deposition of atherosclerotic plaques. The vast majority of occlusive lesions of branching vessels of the arch and of the upper-extremity arterial branches are atherosclerotic in origin, and disease often involves multiple vessels. In addition, because of the irregular nature of these plaques, embolic phenomena resulting from thrombus deposits—composed of both platelets and fibrin—can occur in nearly a third of such patients. Thrombotic or thromboembolic events predominantly occur in patients with multifocal disease. Embolic phenomena owing to ostial disease of the aortic arch branches are uncommon. A cardiogenic source of embolism must be excluded before emboli can be conclusively attributed to arch branch disease.
Inflammatory disorders, such as Takayasu arteritis or polymyalgia rheumatica, are among the less common causes of arch branch occlusive disease. The prototypic vasculitis syndrome that commonly leads to occlusive disease of the thoracic aorta and its branches is Takayasu arteritis. This disease is characterized by immune-mediated destruction of the medial elastic fibers of the affected vessel, followed by scarring of the media and internal elastic lamina, which causes compensatory intimal proliferation. Takayasu arteritis remains an idiopathic large-vessel vasculitis that generally affects women of reproductive age and predominates in Asians; however, it has been reported in patients of all ethnicities. Cardiac failure and cardiomegaly are usually secondary to hypertension and aortic valvular insufficiency. Approximately 60% of patients with Takayasu arteritis require some form of vascular intervention, most commonly involving the coronary arteries, followed by the carotid and upper-extremity arteries.
Additional disorders that can be causative include arteritis stemming from radioactive therapy (for malignancies of the neck or Hodgkin disease), traumatic injuries (e.g., penetrating missile injuries and blunt deceleration injuries), vasospastic disorders, thoracic outlet syndrome, and possibly connective tissue disorders. Radiation therapy can lead to stenosis of the brachiocephalic vessels and induce unpredictable atherosclerotic changes several years after treatment, ultimately resulting in embolic or diminished-flow phenomena.
Clinical manifestations of brachiocephalic occlusive disease ( Fig. 73-1 ) are predominately related to the degree of luminal encroachment in the primary vessel affected and the extent of collateral disease if multiple vascular beds are compromised. Stenosis of aortic arch branches can have direct ischemia-related consequences or lead to steal syndromes in which increases in blood flow to one region result in ischemia in another. Involvement of the innominate artery can lead to anterior, posterior, or combined cerebral symptoms, depending on the amount of collateral flow from the contralateral side via the circle of Willis and the extent of concomitant subclavian or common carotid artery (CCA) involvement. Isolated right-sided steal syndromes can occur, but only if the disease arises in the right subclavian artery and the innominate is relatively spared. In contrast, involvement of the left subclavian artery can result in either upper-extremity claudication or vertebral steal manifesting as vertebrobasilar symptoms, depending on the exact location of the stenotic lesion.
![FIGURE 73-1, Common symptoms of occlusive disease involving the brachiocephalic branches. Compromised flow or emboli from common carotid artery lesions can cause a variety of neurologic symptoms, including transient ischemic attacks (TIAs) and amaurosis fugax. Subclavian artery lesions can cause vertebrobasilar insufficiency (including vertebral-subclavian steal), cardiac complications (including angina, myocardial infarction [MI], and congestive heart failure [CHF]) caused by coronary-subclavian steal, and upper-extremity arterial insufficiency or microembolization. FIGURE 73-1, Common symptoms of occlusive disease involving the brachiocephalic branches. Compromised flow or emboli from common carotid artery lesions can cause a variety of neurologic symptoms, including transient ischemic attacks (TIAs) and amaurosis fugax. Subclavian artery lesions can cause vertebrobasilar insufficiency (including vertebral-subclavian steal), cardiac complications (including angina, myocardial infarction [MI], and congestive heart failure [CHF]) caused by coronary-subclavian steal, and upper-extremity arterial insufficiency or microembolization.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/OcclusiveDiseaseoftheBrachiocephalicVesselsandManagementofSimultaneousSurgicalCarotidandCoronaryDisease/0_3s20B9780323241267000739.jpg)
In general, the clinical presentation of patients with brachiocephalic occlusive disease involves either an acute embolic or a chronic stenotic event. Acute embolic symptoms tend to involve cerebral hemispheric events related to anterior circulation and, similar to carotid bifurcation disease, amaurosis fugax. Less often, emboli can affect the upper extremities, usually evidenced by cold or numb hands or fingers. Commonly, stenotic lesions reduce blood flow to upper extremities (and occasionally to lower extremities) and can result in subclavian steal syndrome. Exercise can induce ischemia and cause hand or arm cramping or fatigue (this process is also known as claudication ); in time, these symptoms can progress to rest pain and possibly to tissue loss.
Takayasu arteritis is associated with a broad spectrum of clinical presentations that range from a fairly indolent chronic course to an acute fulminant disease. The initial symptoms most commonly reported by patients are constitutional and include myalgia, arthralgia, and headaches. Vascular symptoms commonly include claudicatory symptoms, carotidynia, and pulseless extremity. The diffuse involvement of major branches of the aorta contributes to an overall diminution of peripheral pulses in these patients, which is why Takayasu arteritis is sometimes referred to as pulseless disease . The nonspecific nature of the initial presentation contributes to the delay in the diagnosis of most cases of Takayasu arteritis. The Ueno classification system categorizes the disease into four types according to the extent and location of involvement. Types 1 and 3 are characterized by a disease process that affects the aortic arch and its branches. Stenosis and occlusion are typical of Takayasu arteritis, and the lesions can be either short and segmental or long and diffuse. De novo aneurysms are rare but have been reported in all major branches of the aortic arch. Most aneurysms arise from sites of previous anastomoses or surgical repair.
The age at presentation for patients with radiation-induced disease primarily depends on the age at which they were exposed to radiation, and is often younger than for those with atherosclerotic occlusive disease. These patients have angiographically atypical lesions that appear diffuse, unlike the focal lesions typical of atherosclerosis. Presentation includes either embolic or flow-limiting symptoms.
Diagnostic imaging, performed after a detailed initial vascular and neurologic examination, plays an important role in determining the appropriate treatment for each patient. A thorough neurologic examination, even in patients with isolated upper-extremity ischemic symptoms, is essential, because such symptoms could potentially be a manifestation of a steal syndrome and concomitant disease elsewhere. Other critical components of a thorough physical examination include measuring the blood pressure in both arms (a systolic difference greater than 20 mm Hg usually suggests proximal occlusive disease) and conducting a detailed pulse examination of the subclavian artery distribution at several locations: the wrist (radial and ulnar arteries), the upper arm and elbow (brachial artery), the armpit (axillary artery), and in the supraclavicular fossa. An absent or weakened pulse found anywhere other than the supraclavicular fossa tends to indicate arterial occlusion. In addition, an Allen test should be performed because the absence of a blush in any section of the hand usually indicates an incomplete palmar arch. Palpation of the infraclavicular and supraclavicular fossae is helpful to identify a subclavian aneurysm or cervical rib. A bruit identified during auscultation of the subclavian artery may indicate thoracic outlet compression of the artery.
The diagnosis of Takayasu arteritis is usually suspected from the patient's history and clinical presentation, and it is supported by the findings of specific serologic tests, tests for inflammatory markers, and angiography. Angiographic studies show a characteristic pattern of stenosis, poststenotic dilation, aneurysm formation, and occlusion with collateral formation. These findings tend to be localized to the aorta and the proximal aspect of its branches. Total body arteriography is an important component of the diagnostic workup of these patients to characterize the full extent of the disease and to provide a baseline for future comparison, because these patients require frequent serial imaging and monitoring for the rest of their lives.
Digital subtraction angiography offers the opportunity for immediate endovascular intervention if a problem is discovered. As with any intravascular manipulation and imaging technique, the risk of embolic stroke always exists, especially in patients with atherosclerotic disease and plaques. The development of high-resolution computed tomographic angiography with reconstructive capabilities has allowed this modality to substitute for digital subtraction angiography in the assessment of the aortic arch branches in specific circumstances. Computed tomography (CT) and magnetic resonance imaging (MRI) provide valuable imaging for assessing the extent of brachiocephalic disease. Contrast-enhanced MRI with reconstruction provides information equivalent to that obtained from conventional CT angiography. Magnetic resonance angiography (MRA), in addition, can yield useful information about occluded vessels reconstituted via collaterals because the imaging process is not contrast dependent. In addition, MRA provides valuable information about factors that affect the risk of embolization and consequent stroke, including the size, extent, and composition of atherosclerotic lesions. We recommend obtaining a preoperative CT angiogram or MRA for all patients who undergo surgical intervention on the branches of the aortic arch; the images serve as a baseline for future comparisons and for assessing the progression of the disease. Lifelong postoperative surveillance imaging and follow-up is an essential component of the care of these patients.
Transthoracic echocardiography, although reliable for assessing the ascending aorta, is not ideal for assessing the arch and its branches because of its shallow depth of penetration and because the overlying ribs obscure these vessels. Similarly, transesophageal echocardiography (TEE) is limited in its ability to image the branches of the aortic arch, primarily because of shadowing from the trachea. Intravascular ultrasonography is an emerging technology that may be useful during endovascular interventions.
The advent of transesophageal magnetic coils has made it possible to perform transesophageal MRI (TEMRI). Although TEMRI allows multiplanar reconstruction and provides better quantification of the extent of aortic atherosclerosis, real-time imaging and assessment of plaque mobility are feasible only with the help of TEE. Nonetheless, TEMRI provides a better assessment of the circumferential extent of atherosclerotic involvement than TEE does, and it could become an important option for imaging the supra-aortic great vessels.
A thorough knowledge of thoracic anatomy is invaluable for the successful exposure of the supra-aortic vessels, and operative success is heavily dependent on good exposure with appropriate proximal and distal control. A median sternotomy provides adequate exposure for all the major arch vessels, including, in most cases, the left subclavian artery. A mini upper sternotomy up to the third or fourth intercostal space provides good exposure for the mid to distal innominate artery. This is useful in situations in which the proximal innominate artery is free of disease and the aorta does not require clamping for proximal control. A Rummel tourniquet can be used for proximal control in these cases; however, this approach can be challenging to use when innominate artery bypass is necessary or when multiple vessels must be addressed. A full sternotomy is preferred in these circumstances. Extending the median sternotomy incision along the anterior border of the right sternocleidomastoid muscle provides adequate exposure of the bifurcation of the innominate artery and the right CCA. The same incision can be extended over the upper border of the right clavicle if exposure of the more distal aspects of the right subclavian artery is required. The right sternoclavicular joint may need to be dislocated to enhance exposure. Extending the median sternotomy along the anterior border of the left sternocleidomastoid enhances exposure for the left CCA.
The posterior location of the left subclavian artery makes exposure more challenging. When a median sternotomy is performed, it may be necessary to extend the incision over the left clavicle and to dislocate the left sternoclavicular joint for adequate exposure of the intrathoracic course of the left subclavian artery. Isolated left subclavian artery disease can be approached easily via a left posterolateral thoracotomy incision through the fourth intercostal space.
Structures that can interfere with exposure, as well as conduit positioning, are the thymic remnant and the left brachiocephalic vein. The thymus can be split longitudinally or even resected to provide adequate exposure. The brachiocephalic vein can be mobilized as far laterally as necessary so that it may be retracted out of the way to provide better exposure of the proximal arch branches. Ligating the vessel is occasionally necessary to enhance exposure of the left subclavian artery and left CCA. Ligation usually has no significant consequences except for transient left upper-extremity venous congestion. Ligating the brachiocephalic vein is not usually required for bypass procedures; bypass grafts can generally be safely tunneled behind the vein. Attention should be paid to the course of the recurrent laryngeal nerves if the dissection is carried out far laterally into the right subclavian artery and when one is gaining proximal control of the left subclavian artery and the subjacent aorta. The phrenic nerve is vulnerable to injury along its course over the anterior scalene muscle when the sternotomy incisions are extended over the clavicle. In addition, excessive traction in these incisions could jeopardize the functional integrity of the brachial plexus, producing undesirable long-term sequelae.
Cerebral protection is of concern in any operative manipulation involving the innominate artery or the CCAs. During the preoperative evaluation, one should thoroughly ascertain the patient's vascular anatomy, including the patency and size of the vertebral arteries and the completeness of the circle of Willis. Caution should be exercised, as usual, during placement of the proximal clamp and selection of the site for the proximal anastomosis to avoid any area on the aorta with atherosclerotic involvement. Epiaortic ultrasound can be helpful in selecting an ideal clamp site. The robust collateral circulation of the cerebral vasculature allows safe clamping of the innominate artery or proximal CCAs, provided there is no diffuse or multivessel involvement. Flow through the left CCA should be ensured while the innominate artery is clamped. Similarly, it may be prudent to monitor a right subclavian arterial line when the left CCA is intervened on to ensure that there is flow through the innominate system. Furthermore, it may be helpful to monitor estimated hemispheric perfusion by using near-infrared spectroscopy to perform transcranial oximetry during innominate or left CCA clamping. The strategy for cerebral protection is more complicated in patients with contralateral carotid occlusion or multivessel disease, which occasionally necessitates the use of intraoperative shunts to ensure cerebral protection.
Surprisingly, postoperative neurologic complications are rare, even in patients with multivessel disease. Unless multivessel disease involving one or both carotids is encountered, electroencephalographic monitoring or shunting is usually unnecessary. Cerebral protection is more challenging in patients with a bovine aortic arch configuration, in whom clamping the innominate artery is not an option because this would compromise blood flow through both CCAs; shunting or temporary bypass conduits are essential in this circumstance.
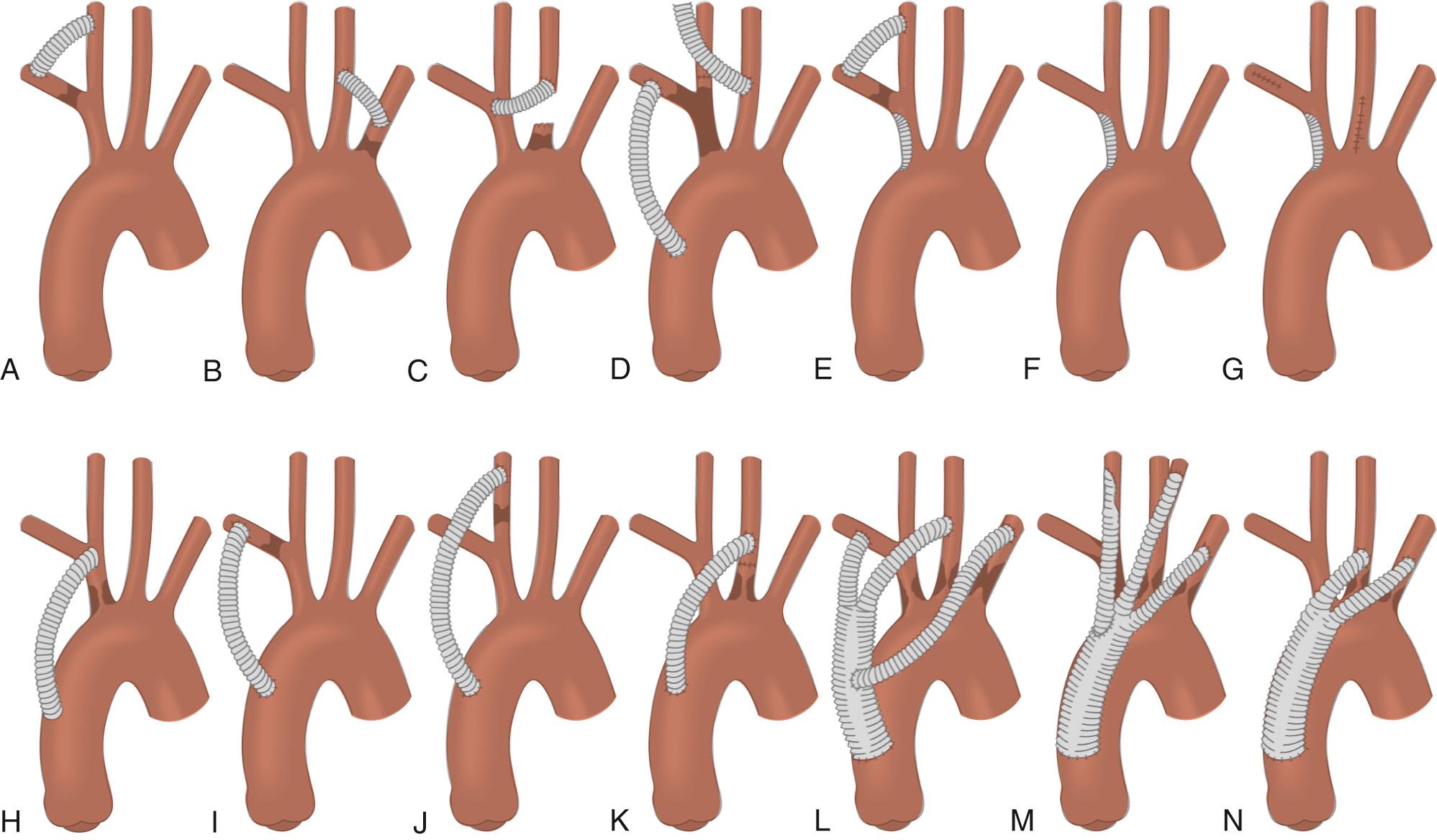
In 1958, DeBakey and colleagues reported a large series of cases that included a direct transthoracic repair of the supra-aortic trunks—a major feat at that time. Surgical treatment was further advanced by Crawford and coworkers with the use of extra-anatomic bypass techniques, which dramatically decreased the mortality associated with these operations from 22% to 5.6%. Currently, extra-anatomic bypass with synthetic grafts is the most common technique for treating these complex lesions ( Fig. 73-2 ). The use of shunting for cerebral protection when necessary and the recognition of high-risk patients who are likely to benefit from cerebral protective measures have dramatically curtailed the adverse neurologic consequences associated with these procedures. Alternative techniques include direct endarterectomy, endovascular stenting, and transposition. In general, direct surgical approaches, such as bypass techniques, are preferred for multivessel and long-segment disease, whereas endovascular techniques are preferred for isolated ostial disease or short-segment disease. Surgical intervention has reportedly produced survival rates of 98% and relieved symptoms in 94% of patients at a mean follow-up of 7.5 years. Crawford and associates reported survival rates of 85% at 5 years, 58% at 10 years, and 25% at 15 years. Hybrid and endovascular approaches have been added recently to the surgeon's armamentarium, and they are gradually becoming the preferred treatment modalities for occlusive disease of the supra-aortic trunks, particularly for older patients with significant comorbidity.
Innominate artery disease is uncommon. It typically involves the ostium or the proximal aspect of the artery and extends along the posterior and lateral walls. Innominate artery occlusion accounts for only 4.7% of cases of extracranial cerebrovascular disease. In these cases, the innominate artery is seldom the only vessel requiring revascularization. Reul and colleagues found that 60% of patients undergoing revascularization for innominate artery symptoms required intervention in at least one other vessel. Early studies of treatments for innominate atherosclerotic disease favored an extrathoracic approach because of the high morbidity and mortality rates associated with intrathoracic repair. Advances in surgical technique and anesthesia, however, produced equivalent results of either extrathoracic or intrathoracic approaches. Current clinical indications for treating symptomatic stenosis include transient ischemic attacks (TIAs), stroke, vertebrobasilar insufficiency, subclavian steal syndrome, and upper limb ischemia.
In patients with atheroembolic manifestations, direct operative treatment by excluding the embolic source is an essential element of the treatment strategy for symptom relief. Direct repair or bypass using the transthoracic approach is preferred because it produces less morbidity than using the extrathoracic approach, which is reserved for patients in whom transthoracic repair is contraindicated. Relative contraindications to intrathoracic revascularization include a heavily diseased or calcified arch, previous thoracic surgery, and advanced age or poor medical condition. Extra-anatomic bypass techniques can be used in cases of primary graft infection, in which one would consider routing the graft well away from the preferred primary route. When revascularization of isolated innominate artery disease is contemplated, two transthoracic options exist: endarterectomy and bypass. Recent advances in endovascular treatment also represent a viable treatment strategy.
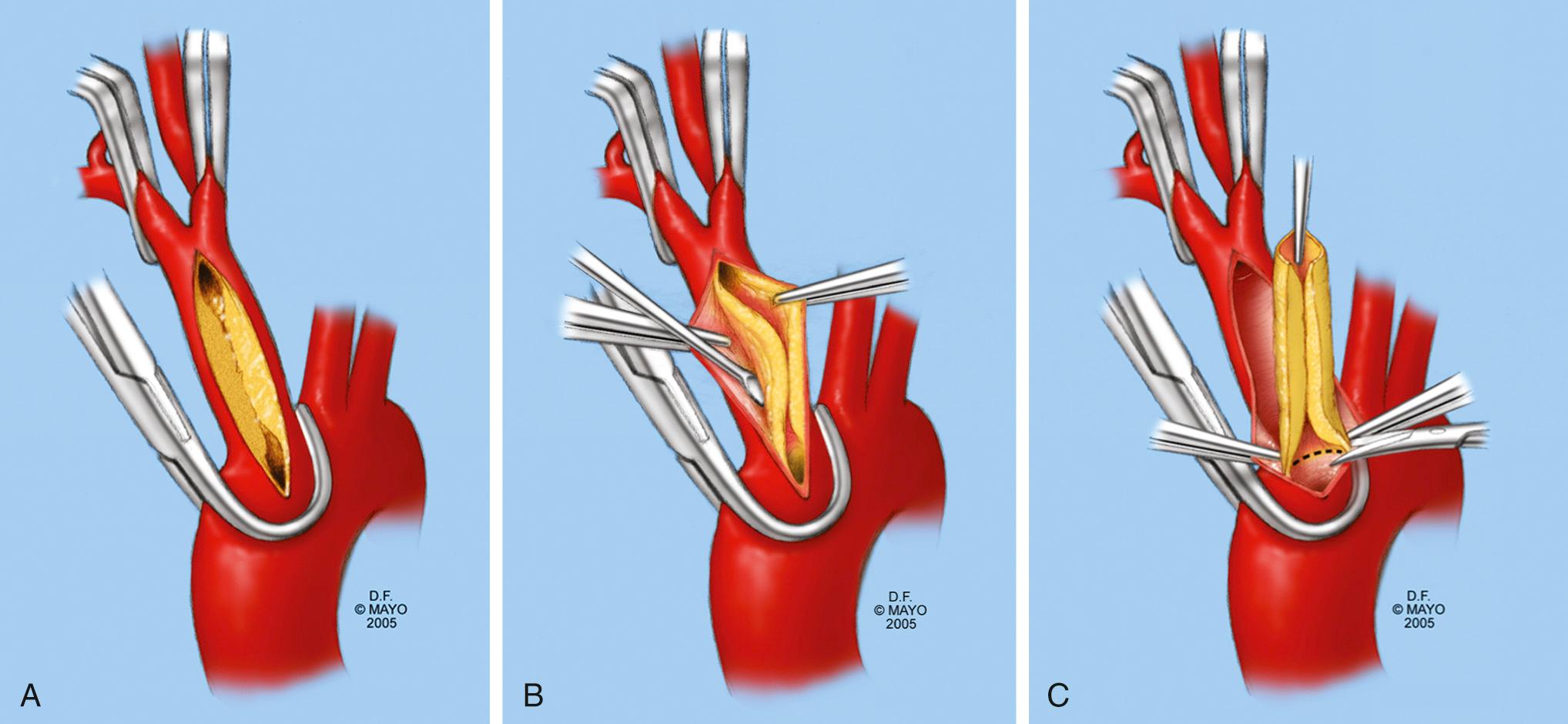
Endarterectomy for isolated branch disease is reported to have excellent results. Relative contraindications include inability to clamp the innominate artery, severe arch atherosclerosis, proximal origin of the left CCA (including a common brachiocephalic trunk), and multivessel disease; a bypass procedure may be preferable in these cases. Whenever possible, endarterectomy should be avoided in patients with Takayasu disease or radiation arteritis, because the transmural inflammatory process complicates the creation of an endarterectomy plane. The endarterectomy proceeds as illustrated in Figure 73-3 . Performing intraoperative epiaortic ultrasonography before clamping may be of benefit, because most of these patients have aortic arch atherosclerosis. The vessel can be closed primarily or by patch angioplasty if luminal narrowing is of concern. Long-segment endarterectomies reportedly have been accomplished by extending the arteriotomy or performing separate arteriotomies on the branch vessels.
Bypass grafting with synthetic prosthetic graft material has produced excellent results and has become the operative procedure of choice. Although the results are comparable to those of endarterectomy, the technical ease of the operation has led surgeons to favor the bypass approach. Bypass techniques are especially well suited for use in cases of Takayasu arteritis, radiation injury, and recurrent atherosclerotic disease.
During the early phases of the development of arterial replacement surgery, operative techniques involved resecting the primary vessel and then placing an interposition graft; this approach was associated with significant perioperative morbidity and mortality. The introduction of the bypass technique by Crawford and coworkers eliminated unnecessary manipulation and dissection of the diseased native artery while allowing the restoration of antegrade flow in the affected territory. This strategy reduced postoperative morbidity rates and significantly improved results. Late graft patency and patient survival (in those without stroke) appear to be good. Berguer and colleagues reported 10-year estimates of 88% ± 6% and 81% ± 7%, respectively. Concomitant coronary artery disease significantly influences both early and late death rates.
As with endarterectomy, epiaortic ultrasound is often useful in selecting the site of the proximal anastomosis and aortic clamping. Typically, an 8- to 10-mm Dacron graft is used to construct the bypass. When there is multivessel disease, a bifurcated or branched graft can be used. If at all possible, the proximal anastomosis should be constructed toward the right lateral aspect of the ascending aorta to avoid potential compression from the sternum or mediastinal contents. As reported by Crawford and colleagues, the potential complications of such compression include venous compression and tracheal compromise resulting in death. Care should be taken to construct the bevel with the appropriate orientation to prevent kinking of the graft. The distal anastomosis is constructed in an end-to-side fashion unless the innominate artery is suspected to be the source of embolic disease. In that situation, the surgeon should consider excluding the diseased segment and performing the distal anastomosis in an end-to-end fashion.
Appropriate positioning of the graft is essential to avoid kinking or compression of the graft, which is directly responsible for most eventual failures of this operation. Several maneuvers have been described to create adequate space to accommodate the graft, including ligating the brachiocephalic vein and resecting the innominate artery. Properly gauging the length of the graft avoids leaving a redundant portion of the graft that will be prone to either kinking or traversing anterior to the aorta and being compressed by the sternum. To avoid overestimation, the sternal retractor is released before the graft length is determined. Theoretically, single-branch grafts have the advantage of being less bulky than bifurcated grafts. When bifurcated grafts are used, the common trunk should be left longer, which makes the flow more laminar at the bifurcation of the graft by reducing interference from the high flow of the ascending aorta. In certain circumstances, the lack of intrathoracic domain may preclude proper placement of a bypass graft. These circumstances include a mediastinal reoperation, saphenous vein conduits placed in certain locations during previous coronary artery bypass grafting (CABG) operations, extensive periaortic inflammation, and stents inserted during previous endovascular interventions. Endarterectomy may be preferred to bypass techniques in these circumstances.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here