Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Many imaging modalities are available for the evaluation of skeletal lesions. In most cases, standard radiographs are sufficient for detecting skeletal tumors. When evaluated together with clinical data (e.g., patient's age and sex, anatomic location of the lesion, clinical presentation), radiographs are the best predictors of the histologic condition of the lesion. To fully characterize a tumor in an anatomically complex area such as the spine, scapula, or pelvis or in a periarticular location, however, magnetic resonance imaging (MRI) or computed tomography (CT) is often necessary.
PET/CT has partially replaced bone scintigraphy as the modality of choice to screen for skeletal metastases. PET/CT with sodium F-fluoride (NaF) has higher sensitivity, specificity, positive predictive value, negative predictive value, and accuracy in detecting bone metastases than conventional 99m Tc-methylene diphosphonate (MDP) skeletal scintigraphy. Although MRI is more sensitive than scintigraphy in detecting metastases, it is not an efficient technique for evaluating the entire skeleton. However, with improvements in hardware, such as the introduction of multichannel MR scanners, a system of multiple phased-array coils covering the whole body, and acquisition acceleration techniques, high-resolution whole-body MRI has become clinically feasible.
Whereas plain radiographs may be sufficient for diagnosis, MRI and CT are fundamental in staging skeletal tumors. Optimal treatment of primary skeletal neoplasms in the absence of distant metastases includes complete surgical resection of the tumor. In the past, amputation was the treatment of choice. With improved surgical technique and aggressive chemotherapy, however, limb-sparing operations can be performed, providing better functional results without affecting survival. In planning resection, accurate preoperative staging is essential. The initial CT or MRI procedures should be performed before biopsy; afterward it is often difficult to distinguish tumor from edema, hemorrhage, and granulation tissue.
Numerous studies have compared the usefulness of CT and MRI in the staging of musculoskeletal tumors. MRI is superior for determining muscle compartment and vascular involvement because of the intrinsic contrast among tumor mass, muscle, and fat, without the need for enhancement with contrast medium. CT is superior for detecting subtle cortical invasion and periosteal and endosteal reaction and for depicting matrix calcification or ossification. Another advantage of CT is scan times of less than 10 seconds; this is particularly helpful when evaluating pediatric patients because it virtually eliminates the need for sedation and minimizes the dependence on patient cooperation. Both MRI and CT are useful in evaluating the response to chemotherapy and radiation therapy. Signs of response to treatment are decreased tumor size, improved delineation of the mass, reappearance of fat planes between muscle groups, and calcification or ossification of the tumor.
With the advent of multidetector CT, images can be acquired with subsecond gantry rotation times at a slice thickness of 0.5 to 0.625 mm, which yields true isotropic high-resolution volume data sets. The isotropic volume data provide the ability to retrospectively reconstruct multiple high-resolution image sets from the original raw data, requiring only one acquisition for the production of three-dimensional CT images in numerous planes. For evaluation of bone lesions, images are reconstructed using bone algorithms, and the images are reviewed using both bone and soft tissue window settings. Intravenous administration of a contrast agent aids in visualizing major vascular bundles and assessing the vascularity of a lesion; it may also be helpful in distinguishing necrotic from viable tumor. CT angiography is useful in the assessment of the neurovascular bundle and in surgical planning.
Numerous pulse sequences are available for the evaluation of musculoskeletal tumors, including spin echo and fast-spin echo, inversion recovery, gradient echo, chemical shift, and diffusion-weighted sequences. Our protocol for evaluating musculoskeletal masses includes images in at least two planes: usually a T1-weighted sequence in the sagittal or coronal plane, followed by either a double-echo (proton-density, T2-weighted) fast-spin echo sequence or a T2-weighted, fat-saturated, fast-spin echo sequence in the axial plane. A short tau inversion recovery (STIR) sequence is occasionally obtained to increase the conspicuity of a lesion.
Whenever possible, imaging is performed with a surface coil for enhanced spatial resolution and an improved signal-to-noise ratio. Body coils are used when an entire bone or soft tissue region is being evaluated for the detection of skip lesions or for surgical planning. Use of contrast-enhanced MRI for characterization of musculoskeletal tumors has yielded controversial results. Contrast enhancement is useful in grading a lesion, assessing response to treatment, and distinguishing postoperative changes from recurrence.
Enchondroma is a common benign primary osseous tumor; only nonossifying fibromas and exostosis are more common. There is no sex predilection, and approximately 50% of these tumors occur in the hands. They are asymptomatic unless they are undergoing malignant transformation or the bone is fractured, and they are often an incidental finding on radiographs.
Enchondromas are typically round or oval lesions with well-defined lobulated borders. The unmineralized matrix exhibits soft tissue attenuation on CT and homogeneous high signal intensity on T2-weighted MRI. Calcification with a ring-and-arc appearance, which suggests a chondroid matrix, is best identified on plain radiography and CT. Calcifications are not consistently identified with MRI; when seen, however, they have low signal intensity on all sequences ( Figs. 60-1 and 60-2 ).
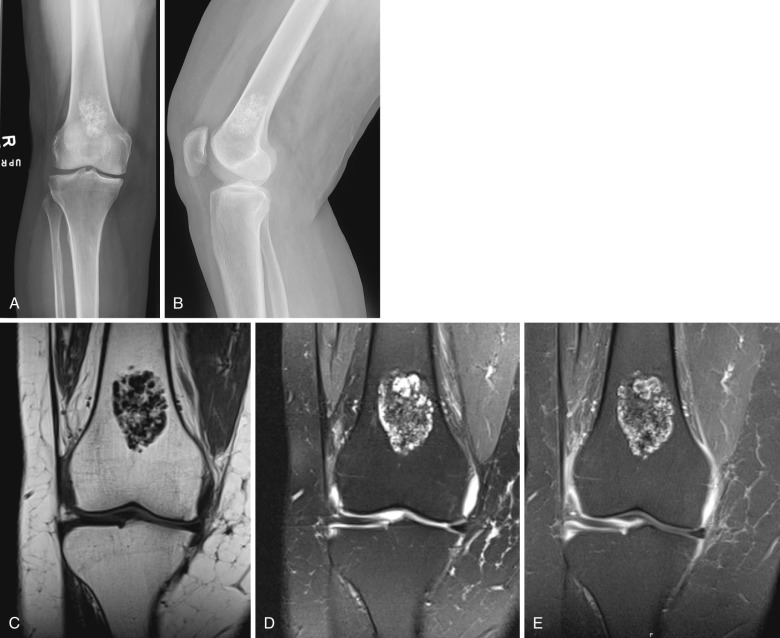
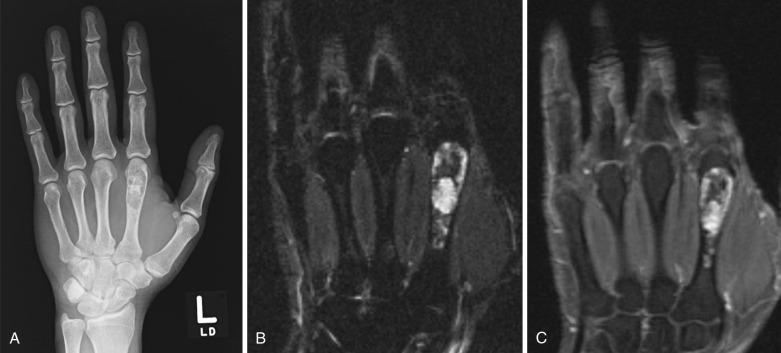
Benign and malignant chondroid lesions can have a similar appearance, making it difficult or impossible to differentiate an enchondroma from a low-grade chondrosarcoma. The presence of a soft tissue mass or cortical erosion or pain in the absence of fracture, however, increases the likelihood of malignancy.
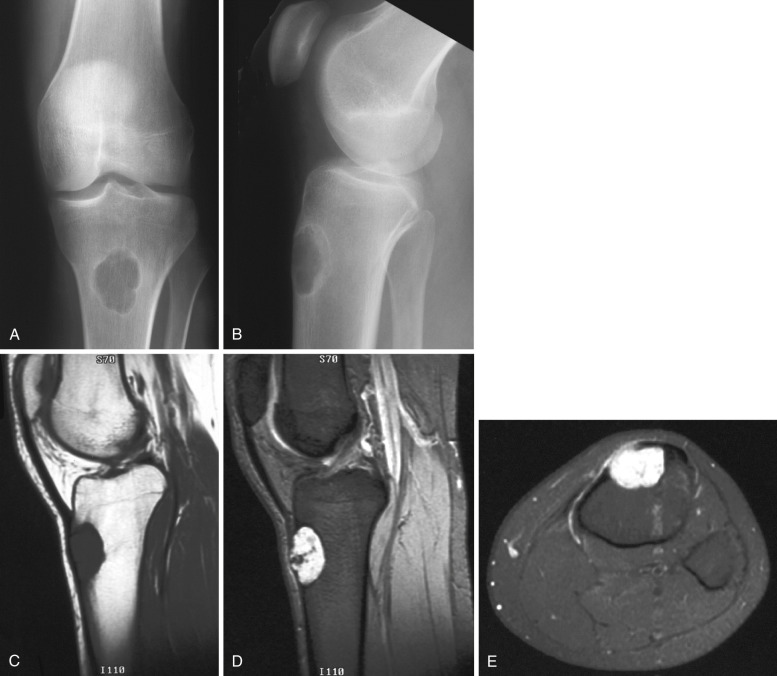
Chondroblastoma is a rare benign tumor of cartilaginous origin composed of chondroblasts. Its peak incidence is in individuals between 10 and 20 years of age. It is more common in males, with a male-to-female ratio of 2 : 1.
Chondroblastoma involves the epiphysis, apophysis, or both; the tumor may extend into the metaphysis after destroying the growth plate. CT accurately demonstrates the extent of the lesion as well as matrix calcifications and subtle cortical infractions. Extension through the growth plate, however, is best detected with conventional tomography or MRI because the growth plate is usually best visualized in the sagittal or coronal plane ( Fig. 60-3 ). Both T1- and T2-weighted MRIs demonstrate a peripheral rim of signal void that corresponds to the sclerotic margin of the lesion. Abnormal signal intensity in large areas of bone marrow surrounding the lesion has been seen and probably represents bone marrow edema. Fluid levels may be present in cystic components, corresponding to aneurysmal bone cysts.

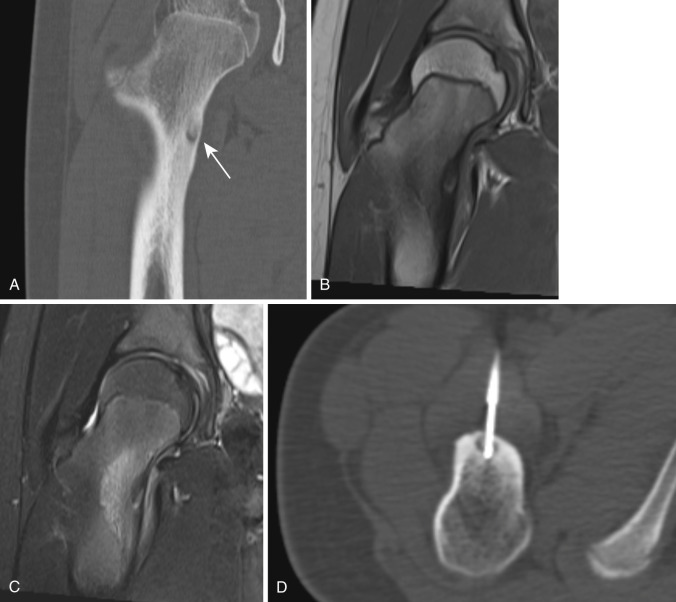
Osteochondromas (exostoses) are the second most common benign tumor of bone after nonossifying fibromas. The male-to-female ratio is 1.5 : 1 to 2 : 1. Although these are congenital lesions, they are usually discovered in individuals between 10 and 20 years of age. Multiple exostoses are uncommon, occurring only one tenth as frequently as solitary exostosis, but they manifest earlier, usually before 10 years of age.
Ninety percent of osteochondromas originate from a long bone close to the metaphysis. The most common locations are around the knee (distal femur and proximal tibia) and the proximal humerus. The morphology of an osteochondroma is more important than the signal intensity in terms of diagnosis. The incidence of malignant transformation is approximately 1% for solitary osteochondromas and 5% to 25% for hereditary multiple exostoses.
Both CT and MRI demonstrate the continuity of the cortex and medullary cavity of the osteochondroma with that of the parent bone ( Fig. 60-4 ). The perichondrium is well seen on T2-weighted MRI as an area of low signal intensity surrounding the outer surface of the high-signal-intensity cartilage cap. MRI measurements of cartilage cap thickness are also accurate, whereas CT measurements of maximal cartilage thickness are often imprecise. The thickness of this structure is important in distinguishing benign osteochondroma from exostotic chondrosarcoma. According to most authors, the cartilage cap is usually thicker than 1.5 cm in chondrosarcoma.

Complications of osteochondroma include nerve injury, vascular injury, deep venous thrombosis, and bursa formation. Formation of a bursa over an osteochondroma is common, and the bursa is usually asymptomatic; if it becomes inflamed and distended, it can be painful. On T2-weighted images, bursal fluid has high signal intensity similar to that of the cartilage cap, and it can be difficult to differentiate the two. On gradient echo sequences, cartilage has a lower signal intensity than that of fluid, and the diagnosis is easily made. A rarer complication is formation of a pseudoaneurysm adjacent to the exostosis.
Chondromyxoid fibroma is composed of three principal elements: chondroid, fibrous, and myxoid tissue. It is the least common of the benign cartilaginous bone neoplasms. There is a male predominance, with a male-to-female ratio of 1.5 : 1 to 2 : 1. The tumor tends to occur around the knee joint but can involve any bone. The tumor is usually solid but may contain cystic or hemorrhagic areas and rarely may be associated with an aneurysmal bone cyst. On MRI the signal intensities of this tumor vary with the proportions of chondroid, fibrous, and myxoid tissues present. CT may be better than MRI in delineating matrix calcification and sclerosis around the tumor ( Fig. 60-5 ).
Osteoid osteomas are relatively common; only osteochondromas and fibrous cortical defects are more prevalent. The male-to-female ratio is 3 : 1. They typically occur in teenagers and young adults and are rare before age 5 and after age 30. These tumors occur most frequently in the femur, tibia, and humerus and involve the diaphysis and less commonly the metaphysis. When the spine is involved, the posterior elements are typically affected. The main clinical symptom is pain relieved by aspirin.
CT is very accurate in detecting the nidus and is preferable to MRI for evaluating osteoid osteoma. Occasionally an osteoid osteoma can be confused with a stress fracture on MRI because of edema in the bone marrow. On CT the typical appearance of an osteoid osteoma is an area of sclerosis surrounding a small (<1 cm) radiolucent nidus ( Fig. 60-6 ). Lesions larger than 1.5 cm are considered osteoblastomas.
The nidus may contain a variable number of calcifications ranging from none to enough to cause almost complete calcification, with only a thin peripheral rim of low density. For full evaluation of the nidus, thin-section CT with less than 2-mm slices is needed because the nidus is often less than 1 cm in diameter. The nidus enhances on dynamic CT scans ; this enhancement helps in differentiating osteoid osteoma from Brodie's abscess. Depending on the degree of calcification, the nidus has low signal intensity on T1-weighted images and variable intensity on T2-weighted images.
The surrounding bone marrow has low signal intensity on all pulse sequences in the presence of reactive sclerosis or high signal intensity on T2-weighted images in the presence of edema (see Fig. 60-6 ). Osteoid osteomas in younger patients tend to be associated with more extensive peritumoral edema. When the osteoid osteoma is intraarticular, an associated joint effusion may be detected.
CT is used to direct percutaneous ablation of osteoid osteomas.
Osteoblastoma is a rare benign tumor. It is at least four times less common than osteoid osteoma. There is a male predominance, with a male-to-female ratio of 2.5 : 1. Its peak incidence is in the second decade, and it is rare before age 10 and after age 30. Its most common location is the spine, usually in the posterior elements. In the long bones it is most often located in the metadiaphyseal region; in rare circumstances it can extend into the epiphyses in adults. Osteoblastomas may be associated with aneurysmal bone cysts.
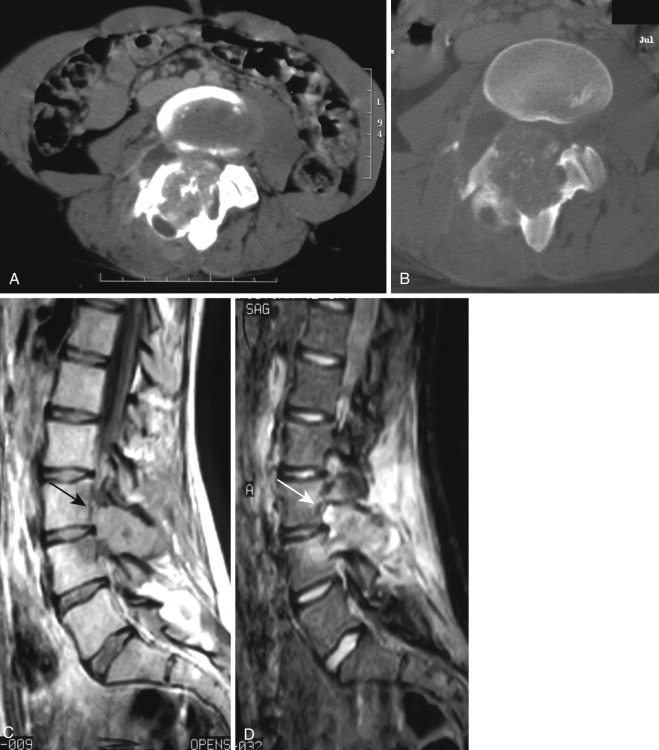
On CT, osteoblastoma appears as an expansile lytic lesion, often with a mineralized matrix surrounded by a thin bony shell. Dense sclerosis and periosteal reaction may occasionally be present. Osteoblastoma typically has low to intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Edema in the surrounding soft tissues and in the bone marrow beyond the tumor margins is common ( Fig. 60-7 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here