Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A malignant cartilage-producing tumour – it generally has a better prognosis than an osteosarcoma (due to late metastases)
Classification:
Central (intramedullary) vs peripheral
Primary vs secondary (e.g. arising in a pre-existing bone lesion such as a central enchondroma or a peripheral osteochondroma)
Grade I: low grade ▸ Grade II: myxoid ▸ Grade III: high grade ▸ dedifferentiated: this refers to the development of an adjacent non-chondroid tumour (e.g. an osteosarcoma, fibrosarcoma, or MFH)
A major consideration is the differentiation between a chondroma and a low-grade chondrosarcoma
This is rare in children with > 50% of patients over 40 years of age (M : F, 1.5 : 1) ▸ secondary chondrosarcoma tends to present at a slightly younger age (4th + 5th decades)
Most are low-grade tumours found incidentally ▸ it can present with insidious pain, a palpable mass or a pathological fracture
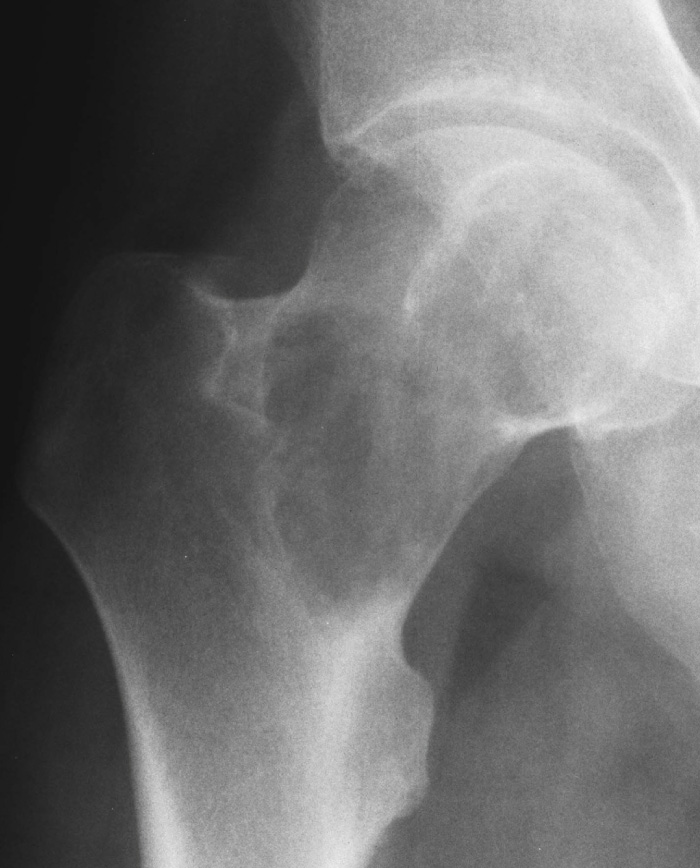
It usually affects the pelvis, proximal femur and proximal humerus (it is rare distal to the elbow or knee) ▸ it is found within the metaphysis (± epiphyseal extension) ▸ 9% of chondrosarcomas occur in the ribs, making this the most common rib primary (other than myeloma) ▸ rare in the hands and feet (c/w enchondroma)
General features of central chondrosarcoma are those of a lytic lesion, well-defined in low grade cases and progressively ill-defined in higher grade cases
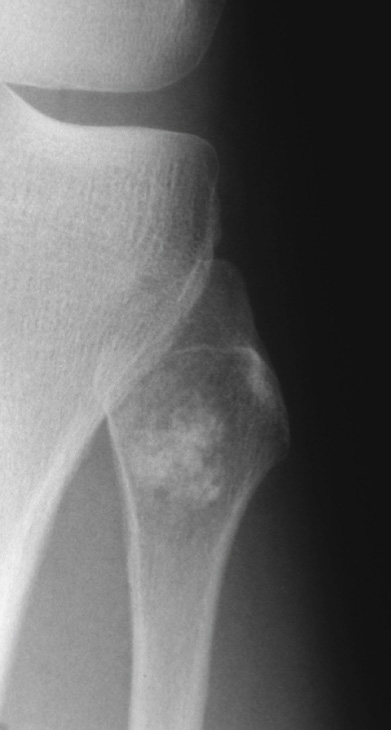
A well-defined lytic lesion with chondroid matrix mineralization (chondroid calcification visible in 75%, described as ring-and-arc, punctate, stippled or popcorn) ▸ there is a narrow zone of transition
Slow growth: this allows reactive change with periosteal new bone + bone expansion + endosteal resorption (endosteal scalloping > ![]() of the cortical width suggests a chondrosarcoma rather than a chondroma) ▸ an increased cortical thickness (if the periosteal reaction outweighs the cortical scalloping)
of the cortical width suggests a chondrosarcoma rather than a chondroma) ▸ an increased cortical thickness (if the periosteal reaction outweighs the cortical scalloping)
More aggressive tumours: cortical destruction ▸ one should consider dedifferentiation to a more malignant type
This can demonstrate a large extraosseous mass which is commonly seen with pelvic lesions (which are often radiographically and clinically occult)
T1WI: hypointense to muscle ▸ T2WI: multilobulated high SI lesion ▸ matrix mineralization appears as foci of signal void ▸ T1WI + Gad: minimal peripheral or septal enhancement (as it is poorly vascularized)
A chondrosarcoma will demonstrate greater activity than that seen within the anterior iliac crest ▸ cannot reliably distinguish between benign and malignant lesions
Suspect the development of a chondrosarcoma within a pre-existing osteochondroma if:
There is increased pain or continued growth after skeletal maturity
There is destruction of part of the calcified cap or ossified stem
US/CT/MRI: these can assess the cartilage cap – it should be < 5 mm with an osteochondroma (but is often > 20 mm with malignant change)
This is rare (and more common in men) ▸ it involves the outer long bones (usually the distal femoral or proximal humeral metaphyses) ▸ there is a good prognosis after resection
A calcificed juxtacortical cartilagenous mass (>5 cm in length) with cortical thickening and periosteal reaction ▸ distinguished from the other surface form of chondrosarcoma (peripheral chondrosarcoma) by a lack of continuity with underlying medullary bone
This is rare, affecting a younger age group than with a conventional chondrosarcoma (3 rd and 4 th decades) ▸ it has a very much more cellular malignant matrix than a normal chondrosarcoma (high grade malignancy)
It is indistinguishable from a central chondrosarcoma ▸ there is often chondroid calcification ▸ there is a predilection for the ribs and mandible
Local recurrence and metastases occur early (and more commonly than with a conventional chondrosarcoma)
This is rare ▸ it is a low-grade tumour with a better prognosis and slow growth ▸ can be mistaken for a subchondral cyst/intraosseous ganglion
It resembles a chondroblastoma or chondromyxoid fibroma – except it almost always involves the ends of the long bones after closure of the growth plate (esp. the proximal femur or humerus) ▸ it has a lytic appearance (± a loculated or ‘soap bubble’ appearance)



Commonest non-haematological primary bone malignancy ▸ a malignant osteoid producing tumour
It is usually a primary central osteosarcoma (75%) – the remainder are made up of other variants distinguished by site and histological grade ▸ it can occur secondary to Paget's disease, post radiotherapy or as a dedifferentiated chondrosarcoma
Classification:
Central (conventional high or low grade)
Intracortical
Surface (parosteal, periosteal or high grade)
Pain or a palpable mass (usually > 6cm at presentation) ▸ pathological fracture
80% of cases present between 10 – 30 years ▸ uncommon under 10 years of age ▸ rare under 5 years of age ▸ there is a 2 nd smaller peak occurring above the age of 40 years which is seen commonly within the flat bones and vertebrae and usually secondary to a pre-existing disorder (e.g. Paget's)
it commonly affects the metaphyseal region of a growing long bone (50-75% are seen around the knee, and within the distal femur or proximal tibia) ▸ other common sites include the proximal humerus and femur ▸ it can cross the growth plate with epiphyseal extension seen in 75% of cases
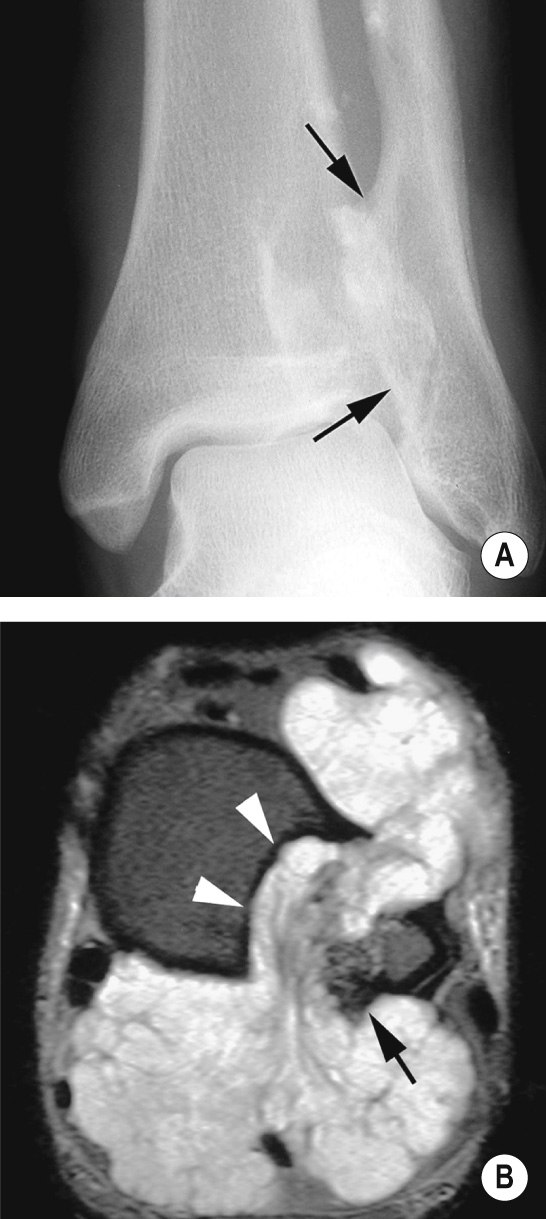
moth-eaten or permeative lytic bone destruction arising eccentrically within the medullary cavity – there can be associated medullary sclerosis due to mineralised tumour osteoid (which has been described as ‘solid’, ‘amorphous’, ‘cloud-like’ and ‘ivory-like’) ▸ there is a wide zone of transition ▸ there can be cortical destruction with an extra-osseous mass and cloudlike matrix mineralization ▸ a spectrum of appearances from purely lytic (13%) to purely sclerotic
Periosteal reaction: a ‘sunburst' appearance perpendicular to the cortex ▸ a lamellated / onion skin appearance with reactive Codman's triangles seen at the margins of the lesion
A solely lytic lesion (13% of cases) may mimic an ABC
this adds little to the diagnosis but is invaluable for local staging and assessing any extension (it can demonstrate any intramedullary and extraosseous extension as well as extension into the adjacent joint or across an open growth plate)
established role in the evaluation of treatment response and for recurrent disease
Multiple intramedullary osteosarcomas in the absence of pulmonary metastases
Synchronous: multiple osteoblastic metaphyseal lesions occurring in children or adolescents ▸ it has a poor prognosis
Metachronous: this affects older patients presenting with a solitary lytic or sclerotic lesion within a long or flat bone ▸ multiple lesions are seen after more than 5 months ▸ this has a better prognosis than a synchronous lesion
This is composed of septated blood-filled cavities (and can mimic an ABC) ▸ it accounts for 4-11% of all osteosarcomas with a mean age of presentation at 24 years (M:F 2:1) ▸ it is very malignant with a poor prognosis
femur, tibia and humerus
predominantly lytic lesions ± bone expansion
subtle matrix mineralisation ▸ extensive haemorrhage with fluid-fluid levels ▸ extra-osseous extension
Thick peripheral, septal and nodular enhancement helps differentiate from an ABC
This accounts for <1% of cases ▸ it has similar features to a conventional central osteosarcoma
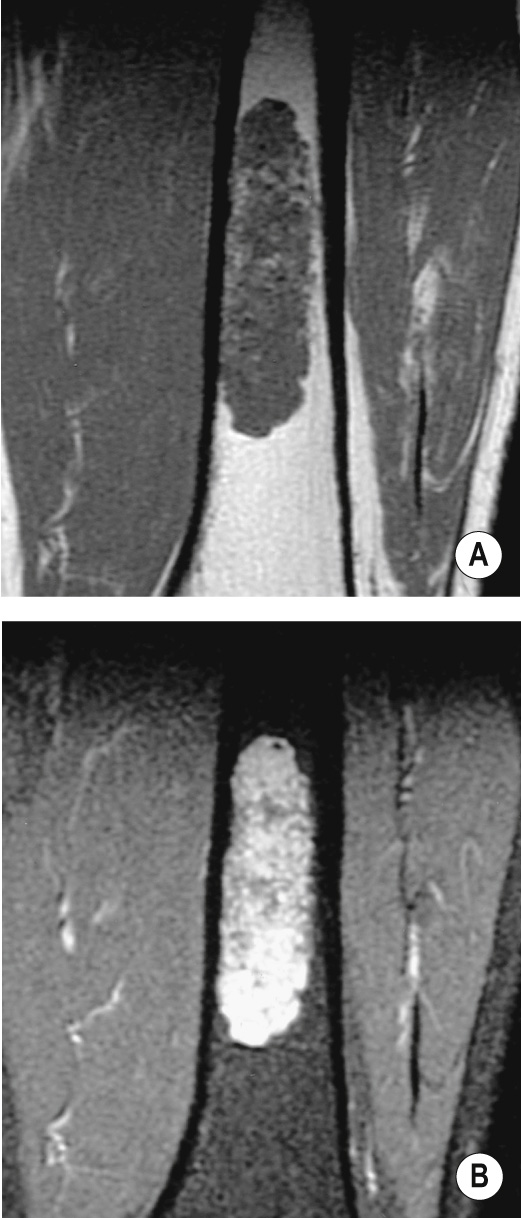
This well differentiated indolent lesion accounts for <1% of cases ▸ there is a mean age of presentation at 34 years, with a slight female preponderance
the femur and tibia (around the knee)
4 patterns: 1) lytic with varying degrees of coarse trabeculation ▸ 2) lytic with little trabeculation ▸ 3) densely sclerotic ▸ 4) mixed lytic and sclerotic
It has a relatively benign appearance that can be mistaken for fibrous dysplasia, osteoblastoma or a low grade chondroid tumour ▸ extraosseous extension aids in the differentiation
A group of tumours that arise form the surface of bone – includes parosteal, periosteal and high grade surface osteosarcomas ▸ all types account for < 10% of osteosarcomas
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here