Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Lymphedema is a progressive disease that can occur as a result of congenital defects, iatrogenic injury, or infection of the lymphatic system.
The lymphatic system is comprised of capillary lymphatics that drain into progressively larger collecting vessels.
Lymphedema can develop due to genetic/developmental abnormalities of the lymphatic system (i.e., primary lymphedema) or more commonly, after trauma or infection of the lymphatic system (secondary lymphedema).
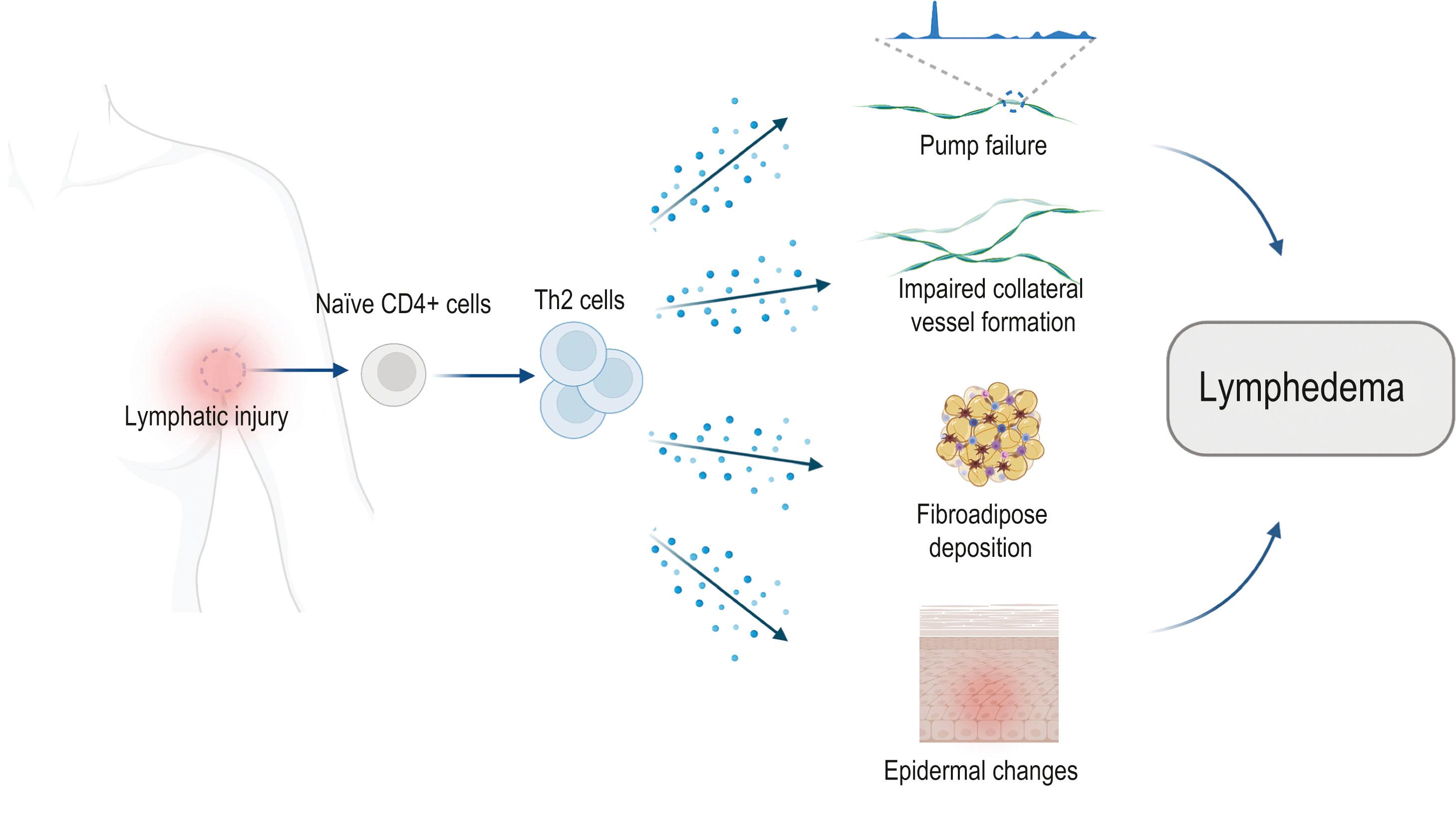
The pathophysiology of lymphedema is complex and involves multiple processes driven by chronic inflammatory reactions, including pumping failure, impaired collateral vessel formation, fibroadipose deposition, and epidermal changes.
Obesity and lymphedema are intimately related.
Although there is currently no definite cure for lymphedema and its late changes are likely not reversible, early identification and comprehensive evaluation are key for improved outcomes.
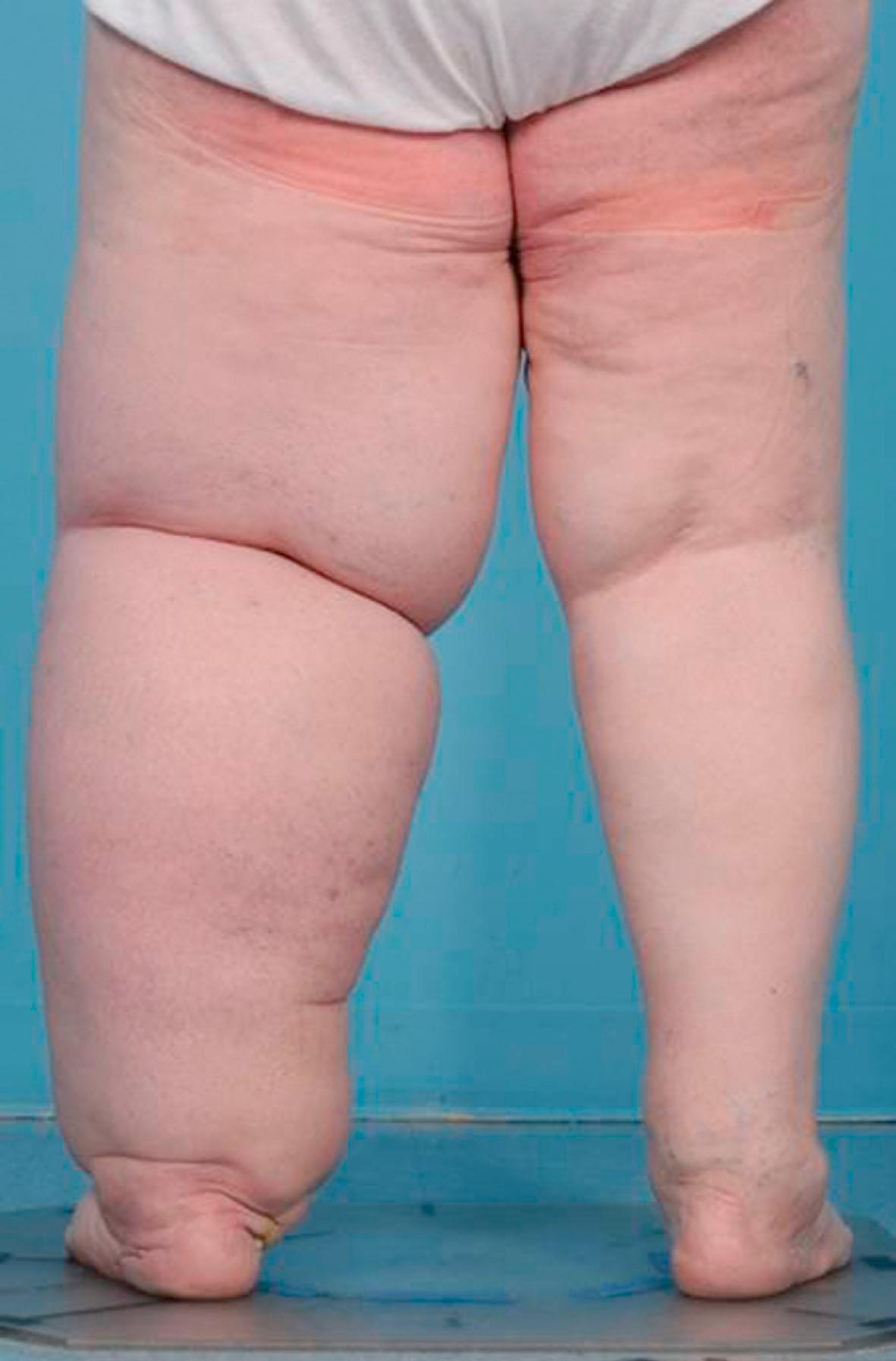
Lymphedema is a progressive disease of the lymphatic system characterized by chronic inflammation, adipose deposition, hyperkeratosis, and fibrosis. Although the precise mechanisms regulating the development of lymphedema remain unknown, a key inciting event is lymphatic dysfunction and impaired clearance of interstitial fluids. Lymphedema can develop due to genetic or developmental abnormalities of the lymphatic system (i.e., primary lymphedema) in which lymphatic vessels are absent or poorly developed. More commonly, lymphedema develops after trauma or infection of the lymphatic system (secondary lymphedema). These inciting events set off a cascade of tissue changes that in some cases ultimately result in massive accumulation of adipose tissue and the classic findings of elephantiasis ( Fig. 28.1 ).
Estimates of the incidence of lymphedema vary widely. It is estimated that 200 million patients in low-income countries suffer from lymphedema secondary to parasitic infections by Wuchereria bancrofti . This disease has a variable course, with smoldering disease in some and rapidly progressive/disabling lymphedema in others. Patients with filariasis may develop massive swelling of the limbs and genitals due to direct lymphatic obstruction by the parasites and inflammatory reactions resulting in significant morbidity and mortality.
In high-income countries, the most common cause of lymphedema is cancer treatment. Breast cancer survivors comprise the largest group of affected individuals due to the high incidence of breast cancer in these regions. It is estimated that 15–40% of all patients who undergo axillary lymph node dissection go on to develop lymphedema (ALND). The variability in rate is due, at least in part, to differences in the diagnostic criteria and the length of follow-up. Recent advances in sentinel lymph node biopsy (SLNB) have decreased the requirement for full ALND and therefore the incidence of lymphedema. However, lymphedema does develop even after SLNB in 5–7% of patients.
In addition to lymph node dissection, extensive skin resections, radiation therapy, obesity, and infections have also been identified as significant risk factors for disease development.
Lymphedema is not exclusively a disease of breast cancer survivors and occurs as a complication of treatment of most other solid tumors, with reported incidence of 16% in melanoma, 30% in sarcoma, 20% in gynecologic tumors, 10% in genitourinary tumors, and 4% in head and neck cancers. In fact, a recent meta-analysis estimated that nearly 1 in 6 patients treated for a variety of solid tumors go on to develop lymphedema. The development of lymphedema in patients with sarcomas is an interesting phenomenon since lymph nodes are rarely removed in these tumors, suggesting that widespread injury to the superficial lymphatic system (as would occur with a wide excision of a skin sarcoma in combination with radiation therapy) is sufficient to disrupt the lymphatic vasculature and lead to the development of lymphedema even when the regional lymph nodes are not injured.
Cancer survivors with lymphedema are severely impacted by the disease, suffering chronic pain and decreased ability to perform activities of daily living as well as being at high risk for developing severe infections necessitating prolonged hospitalization.
Given that the prevalence of lymphedema is expected to increase with increasing incidence of its predisposing factors such as obesity and radiation, lymphedema represents a substantial biomedical burden.
Based on both clinical and laboratory experience, this chapter overviews the cellular mechanisms that regulate the pathophysiology of lymphedema, as well as the basic principles of evaluation and management of lymphedema patients.
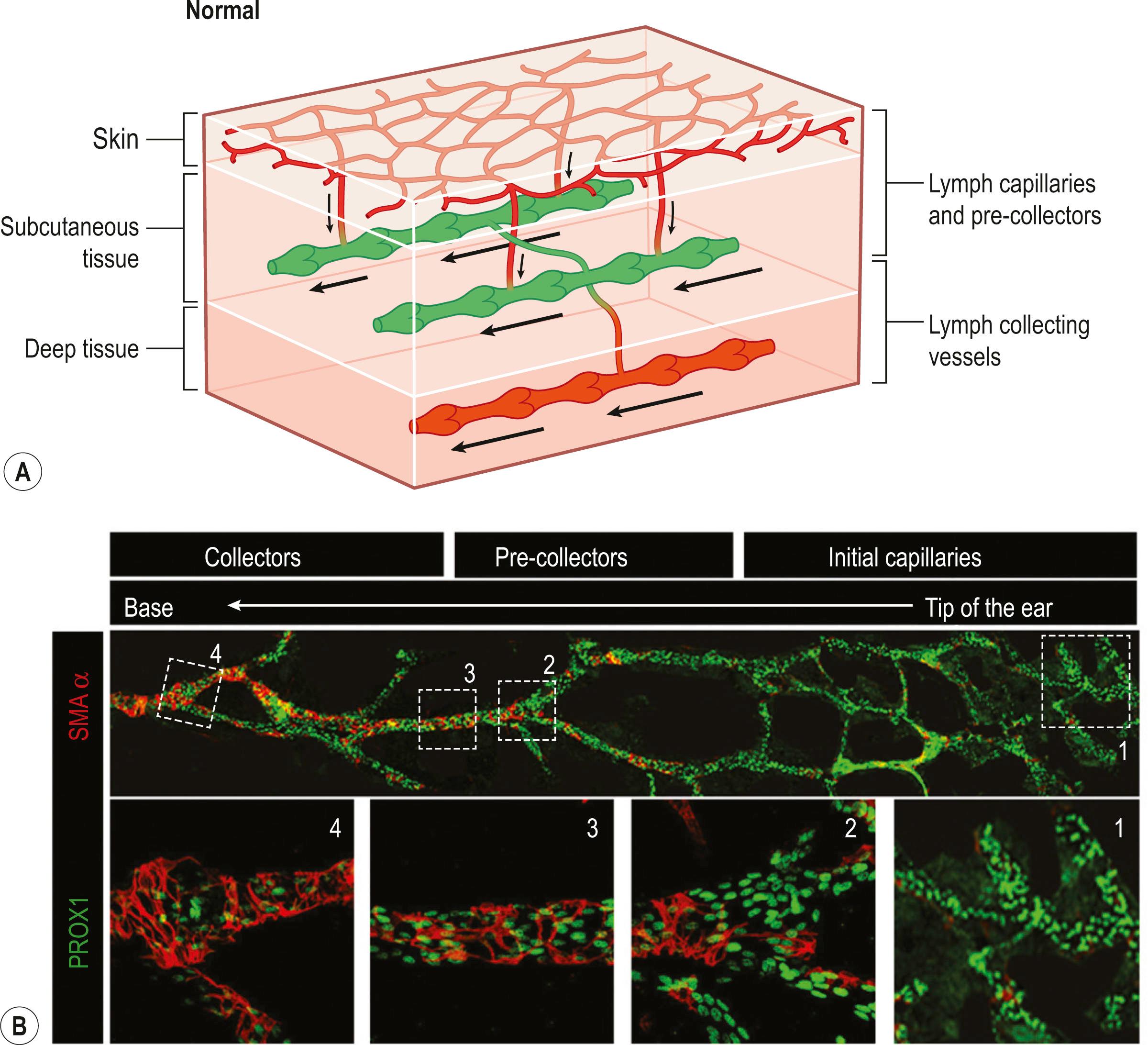
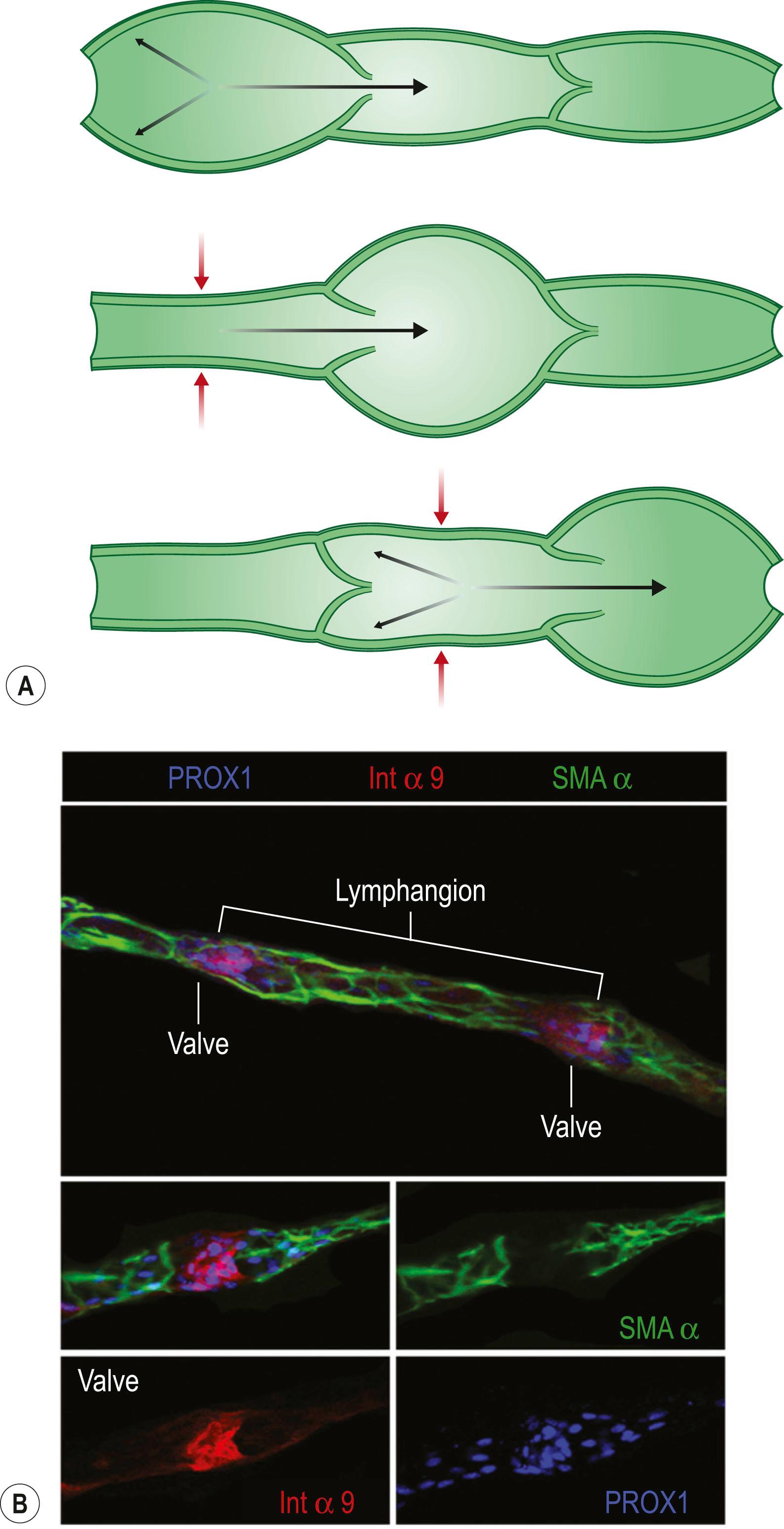
The lymphatic system plays a key role in many physiologic processes, including interstitial fluid and immune cell transport, regulation of inflammation, responses to host or foreign antigens, and fat absorption, among others. The transport of immune cells and interstitial fluid from the periphery begins in capillary lymphatics located in the dermis ( Fig. 28.2 ). These thin-walled, relatively large vessels are comprised of a single layer of lymphatic endothelial cells (LECs) with little to no basement membrane, are physically tethered to the surrounding tissues by anchoring filaments and to each other by overlapping or intercalating button-like junctions. Minute changes in tissue fluid content cause adjacent LECs to separate due to the physical connections of these cells with the surrounding tissues by anchoring filaments, thus enabling entrance of cells and interstitial fluid into the initial lymphatics. Once the interstitial fluid has entered the lymphatic system, the overlapping regions between LECs is reestablished, maintaining the fluid within the lymphatic vessel. Fluid is propelled passively to pre-collectors and collecting lymphatics located in the deeper dermis and subcutaneous tissues. The LECs in collecting vessels, in contrast to the capillary lymphatics, have continuous, “zipper like”, endothelial cell junctions that prevent fluid leak with physical changes in the microenvironment. In addition, collecting lymphatics have a basement membrane and are covered by smooth muscle cells that can contract to propel lymphatic fluid forward. Lymphatic collectors also have bicuspid valves located every 1–2 mm that ensure one-way flow of interstitial fluid blocking backflow into the capillary lymphatic system. The functional lymphatic unit is defined as a lymphangion and contains a region of collecting lymphatic vessels between two valves ( Fig. 28.3 ).
Lymphatic flow is determined by two factors. Passive compressive forces arise from external compressive forces such as muscle contractions, respiration, regional arterial pulsation, and gravity. These forces, as their name implies, passively propel interstitial fluid centrally. In normal limbs (i.e., without history of lymphatic injury), passive compressive forces such as massage or muscular contractions do not significantly increase lymphatic pressure in collecting lymphatics and do not increase flow. Active compressive forces arise from intrinsic contraction of smooth muscle cells surrounding the collecting lymphatics. These muscle cells are unique in that they have features of both smooth and striated muscles and have basal myogenic activity. Myogenic forces in the lymphatic system, similar to the heart, are responsive to preload and afterload pressure changes. In addition, the force and frequency of lymphatic pump contraction can be modulated by vasoactive substances such as histamine and substance P, among others. In general, increases in preload and afterload lead to an increase in contraction frequency and strength up to a point. Persistent increases beyond this point lead to lymphatic pump failure and vessel dilatation.
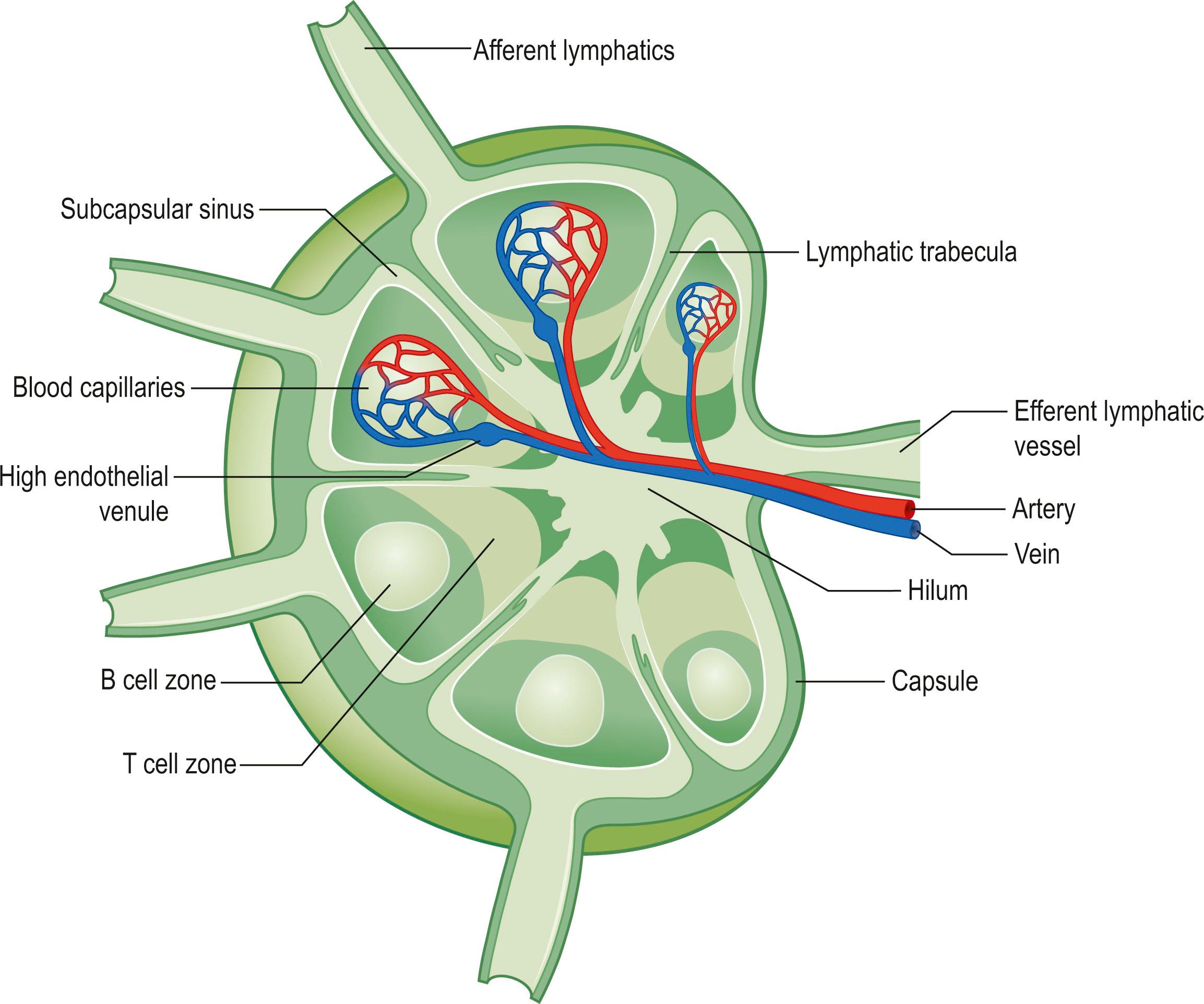
Lymph nodes filter lymphatic fluid as it is transported within the lymphatic system back to the venous circulation ( Fig. 28.4 ). Although the number of lymph nodes is somewhat variable, a typical adult has 600 lymph nodes located in various regions and clustered in areas where body parts come together or in/around intra-abdominal organs. Interstitial fluid is transported centrally by collecting lymphatics and enters the subcapsular sinus of the lymph node via afferent lymphatics. From there, the interstitial fluid (and the antigens, antigen-presenting cells, and inflammatory cells it contains) drain through lymph sinuses that surround lymph node follicles where B cells reside. Lymphatic sinuses are lined by reticular endothelial cells and antigen-presenting cells, enabling presentation and response to self/foreign antigens. Macrophages located in these regions can also phagocytose bacteria for processing and clearance. In addition, fluid exchange occurs through regional high endothelial venules that permeate the lymph node enabling hematogenous delivery of immune cells and cytokines to the lymph node. The lymphatic fluid exits the lymph node via efferent lymphatics located at the lymph node medulla progressing to the next lymph node chain or centrally for return back to the venous system.
Numerous genetic defects are associated with development of primary lymphedema ( Table 28.1 ) and germline sequence variations have been identified in at least 20 human genes. These disorders have a highly variable natural history in terms of timing of presentation and severity of symptoms. In addition, primary lymphedema may be familial with known or suspected genetic defects, may occur as a result of spontaneous mutations, or in some cases develop without a known cause. Familial forms of primary lymphedema, even within members of the same family, can have different presentation due to the penetrance of the genetic mutation or causative factors and interaction with environmental regulators. Thus, in some cases primary lymphedema may present shortly after birth (i.e., congenital lymphedema) or, more commonly, become manifest years later with progressive symptoms ( lymphedema praecox or lymphedema tarda ).
| Gene | Syndrome | Pathology | References |
|---|---|---|---|
| FLT4 (5q35) (coding region for vascular endothelial growth factor receptor 3) | Milroy disease | Primary lymphedema of the lower extremities. Upslanting “ski jump” toenails due to nail bed edema | |
| FLT4 (4q34) (coding region for vascular endothelial growth factor C) | Milroy-like lymphedema | Congenital lower limb lymphedema | |
| FOXC2 | Lymphedema-distichiasis syndrome | Lower-limb lymphedema most often presents at puberty; double row of eyelashes | |
| SOX18 | Hypotrichosis–lymphedema– telangiectasia syndrome | Lymphedema, hair loss, and small dilated blood vessels near the surface of skin | |
| GJC2 (coding for connexin 47 (CX47) | Meige’s disease | Impaired gap junction activity, increased risk of breast cancer-related lymphedema | |
| CCBE1 (18q21) (encodes for collagen and calcium binding EGF domain 1) | Hennekam syndrome | Severe lymphedema in limbs, genitalia, and face; facial anomalies; seizures, mental retardation; and stunted growth. Symptoms often present in utero | |
| KIF11 (10q24) | MCLMR syndrome | Microcephaly, congenital lower limb LE, ocular abnormalities, learning disabilities | |
| GATA2 (3q21) | Emberger syndrome | Unilateral or bilateral lower limb lymphedema; presents in childhood; severe cutaneous warts; myelodysplasia | |
| WILD syndrome | WILD syndrome (warts, immunodeficiency, lymphedema, and dysplasia) | ||
| AKT1 | Proteus syndrome | Lymphatic malformations, skeletal, cutaneous, and CNS abnormalities |
In most cases of primary lymphedema, patients present with unilateral lower extremity lymphedema (~70%) at some point between birth and age 35. The lymphatic system is poorly developed with decreased numbers of lymphatic vessels (most commonly collecting lymphatics). However, it is unclear if patients with primary lymphedema have defects of the lymphatic system at birth or if these changes develop postnatally. The current evidence suggests that in most cases some degree of lymphatic dysfunction is present at birth and that these changes gradually worsen over time. The rate at which these changes occur is variable and can be altered by environmental factors leading to differential presentation of the disease. Studying these changes has been a challenge due to our inability to serially monitor the lymphatic system noninvasively; however, recent advances with lymphatic imaging have been helpful in this regard.
Congenital lymphedemas occur more commonly in females, more commonly involve the lower extremities, and account for 10–25% of all primary lymphedemas. The degree of swelling of the limbs can be variable and, in some cases, may result in severe abnormalities in one limb and relatively mild or absent disease in the contralateral limb.
Our knowledge of the molecular mechanisms affecting lymphangiogenesis has improved substantially over the past 20 years, mainly due to the identification of regulatory molecules and markers specific to the lymphatic endothelium. Several signal transduction pathways have been described in the differentiation and growth of LECs, and differentiate lymphatics from blood vessels. The signal-transduction system for LEC growth, migration, and survival is formed by vascular endothelial growth factors (VEGF) C and D and their receptor VEGFR-3, a key signaling molecule primarily expressed by LECs. VEGF-C and VEGF-D also bind to neuropilin-2 (Nrp2), a semaphorin receptor in the nervous system that is also expressed in lymphatic capillaries. Not surprisingly, Nrp2-deficient mice have lymphatic hypoplasia.
Milroy’s disease is a familial, sex-linked disorder in which inactivating mutations occur in VEGF-R3. These mutations account for a relatively small number of patients with primary lymphedema (2–3%) and usually present shortly after birth with limb swelling and/or chylothorax. Activation of VEGF-R3 results in transmission of intracellular signals that regulate lymphatic endothelial cell differentiation, proliferation, migration, and endothelial-derived nitric oxide production. Consistent with these findings, patients with Milroy’s disease have hypoplastic lymphatic vessels with variable severity of dermal and collecting lymphatic vessel agenesis.
In contrast to congenital lymphedemas in which the disease presents shortly after birth, patients diagnosed with lymphedema praecox present with mostly unilateral lower extremity lymphedema at some point before the age of 35. The vast majority of these patients develop unilateral lower extremity lymphedema and the disease has a 4:1 female to male ratio. Additional evidence implicating a sex-hormone link with this disease is the fact that most patients begin to become symptomatic at the time of puberty. Histologic examination of patients with lymphedema praecox has shown variable pathologic findings; however, these patients often exhibit fewer capillary lymphatics and hypoplastic, low-caliber, collecting vessels.
The diagnosis of lymphedema tarda refers to patients who develop primary lymphedema after the age of 35. This disease is a diagnosis of exclusion since secondary causes of lymphedema are much more common in this age group. In addition, lymphedema tarda is an infrequent presentation of primary lymphedema and occurs most commonly in the lower extremities of women. Although the pathophysiology of this disease remains largely unknown, recent studies have shown an association with loss-of-function mutations in the FOXC2 gene.
The validity of classification schemes that categorize primary lymphedema based on the age at which symptoms present has been recently debated. This debate centers on the fact that presentation of these disorders is highly variable due to genetic and environmental factors and that this variability decreases the utility of these categories for diagnosis. As a result, recent studies have attempted to develop new classification schemes based on the presentation of disease and known genetic mutations. This approach categorizes congenital lymphedemas into five main groups: syndromic, systemic or visceral, disturbed growth, congenital onset, and late onset. The developers of this system contend that this diagnosis algorithm is more precise and as a result can be useful for developing and testing of diagnostic or therapeutic interventions. Due to the high genetic heterogeneity in primary lymphedema, a better understanding of the pathogenetic mechanisms of lymphedema along with accurate phenotyping may improve genotype–phenotype correlations and disease classification.
Secondary lymphedemas develop after injury or obstruction of the lymphatic system. For example, infections with parasites in filariasis result in chronic obstruction of lymphatic channels and subsequent immune responses that impair lymphatic function leading to progressive disease. Filariasis is caused by roundworms (most commonly Wuchereria bancrofti, Brugia malayi , and Brugia timori ) that are transmitted by mosquitos. The adult worms grow in the tissues and release larvae into the bloodstream (microfilariae) that are diagnostic for the disease. However, patients with clinical disease may be free of microfilariae in the blood, in which case the diagnosis is made either clinically, or by tissue biopsies, or serum antigen testing. Filariasis is a major cause of morbidity in low-income countries and treatment remains limited to antiparasitic medications that only kill the developing larvae rather than the adult worm.
Iatrogenic lymphatic injury in the course of cancer treatment is another major cause of secondary lymphedema. In fact, lymphedema is the most common long-term complication of cancer treatment (even more common than radiation-induced sarcomas, or chemotherapy-induced renal or cardiac failure), with the potential to develop in the course of treatment for virtually all solid tumors. Lymphedema can even develop after extirpation of head and neck tumors resulting in cosmetic deformity and functional compromise.
Secondary lymphedema in cancer survivors occurs most frequently months and sometimes years after the initial surgery ( Fig. 28.5 ). This delayed presentation together with the fact that lymphedema develops in only a subset of patients who undergo lymphadenectomy is important since these findings suggest that lymphatic injury is necessary but not sufficient for the development of the disease. Thus, additional pathological changes are needed for patients to develop lymphedema after lymph node dissection.
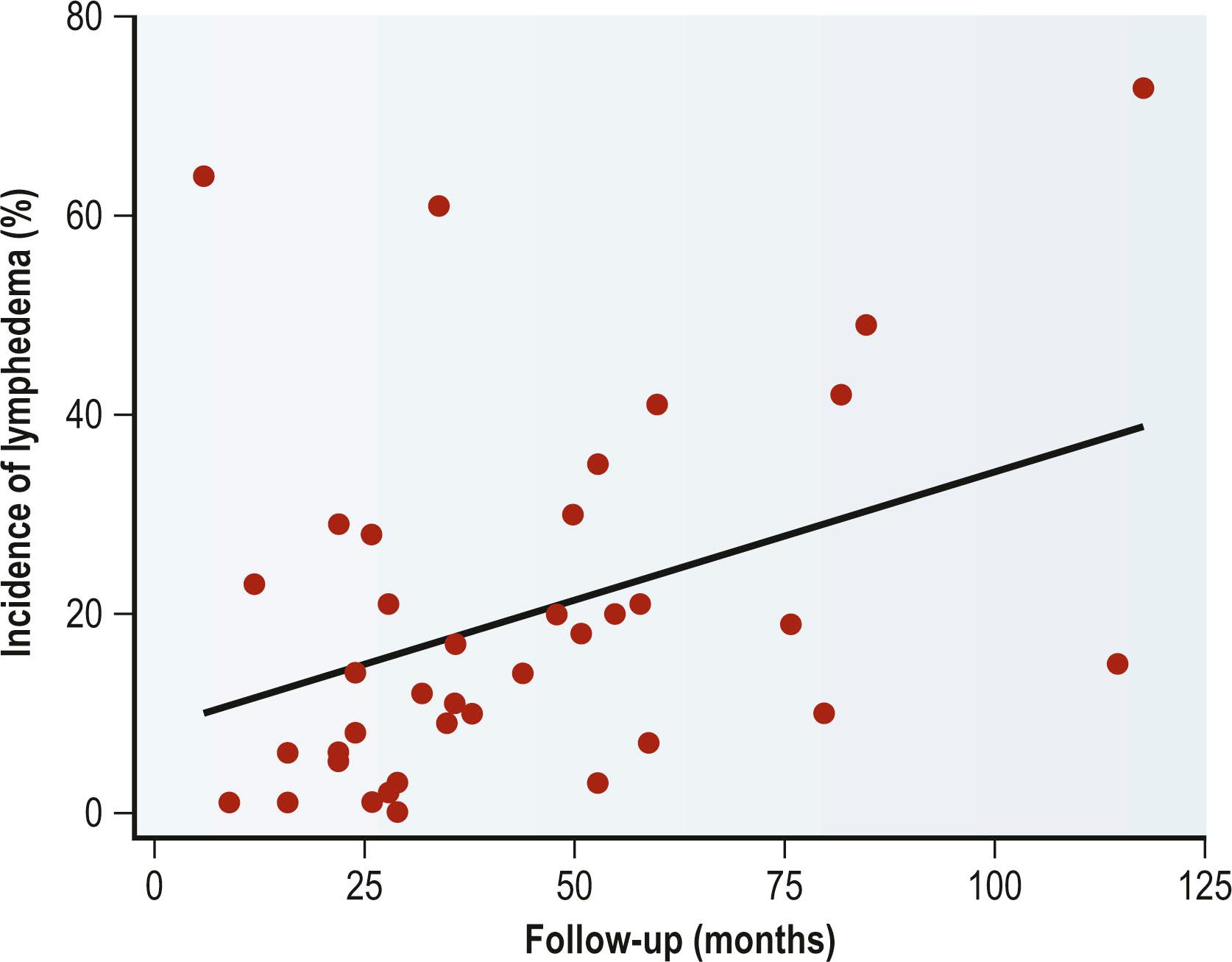
On average, secondary lymphedema in breast cancer survivors develops approximately 8 months after the initial surgery. In addition, the majority of patients (75%) are diagnosed within the first 3 years. In one unusual case report, a patient developed lymphedema after a seemingly innocuous injury 50 years after the initial lymphatic injury. Thus, in most cases the acute surgical swelling that develops after breast surgery and lymphadenectomy resolves within the first few weeks of surgery and, in most cases, never recurs. However, in some patients it recurs in a progressive and permanent manner 8–12 months later. This process appears to be accelerated somewhat in the lower extremity (perhaps due to the effect of gravity) with lymphedema developing on average 3–6 months after surgery.
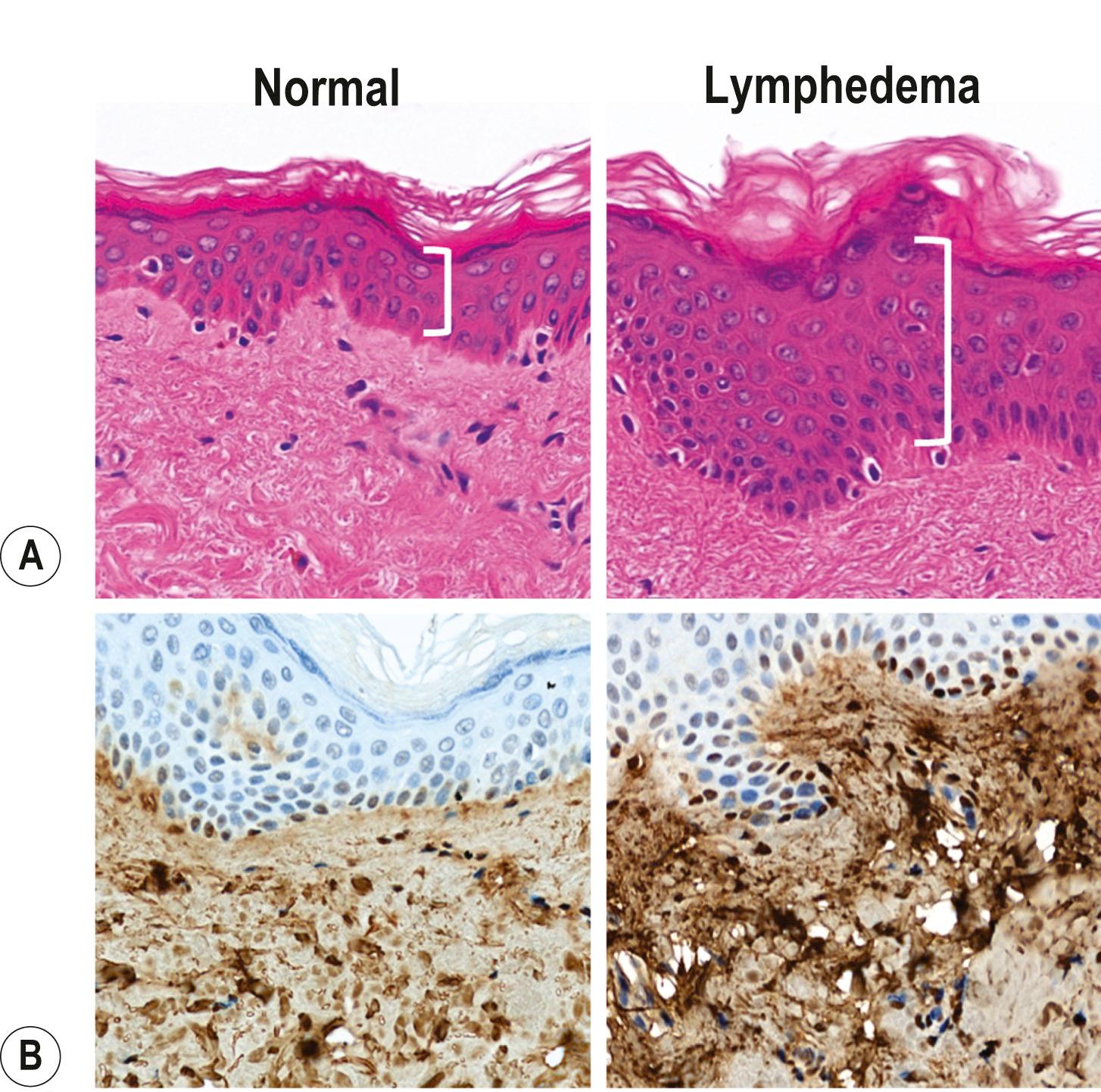
Although lymphedema is common and morbid, surprisingly little is known about the pathophysiology of this disease. The histological hallmarks of the disease are edema, fibroadipose tissue deposition, chronic inflammation, and hyperkeratosis and recent studies have begun to shed light on how lymphatic injury leads to these protean symptoms ( Fig. 28.6 ). A key concept in understanding the pathology of lymphedema is that lymphatic injury is only the initiating step and that additional pathological events are necessary for the development of lymphedema clinically. This concept is highlighted by the fact that lymphedema only develops in a subset of patients who undergo lymphadenectomy, and even in these individuals does so in a delayed fashion usually months to years after surgery.
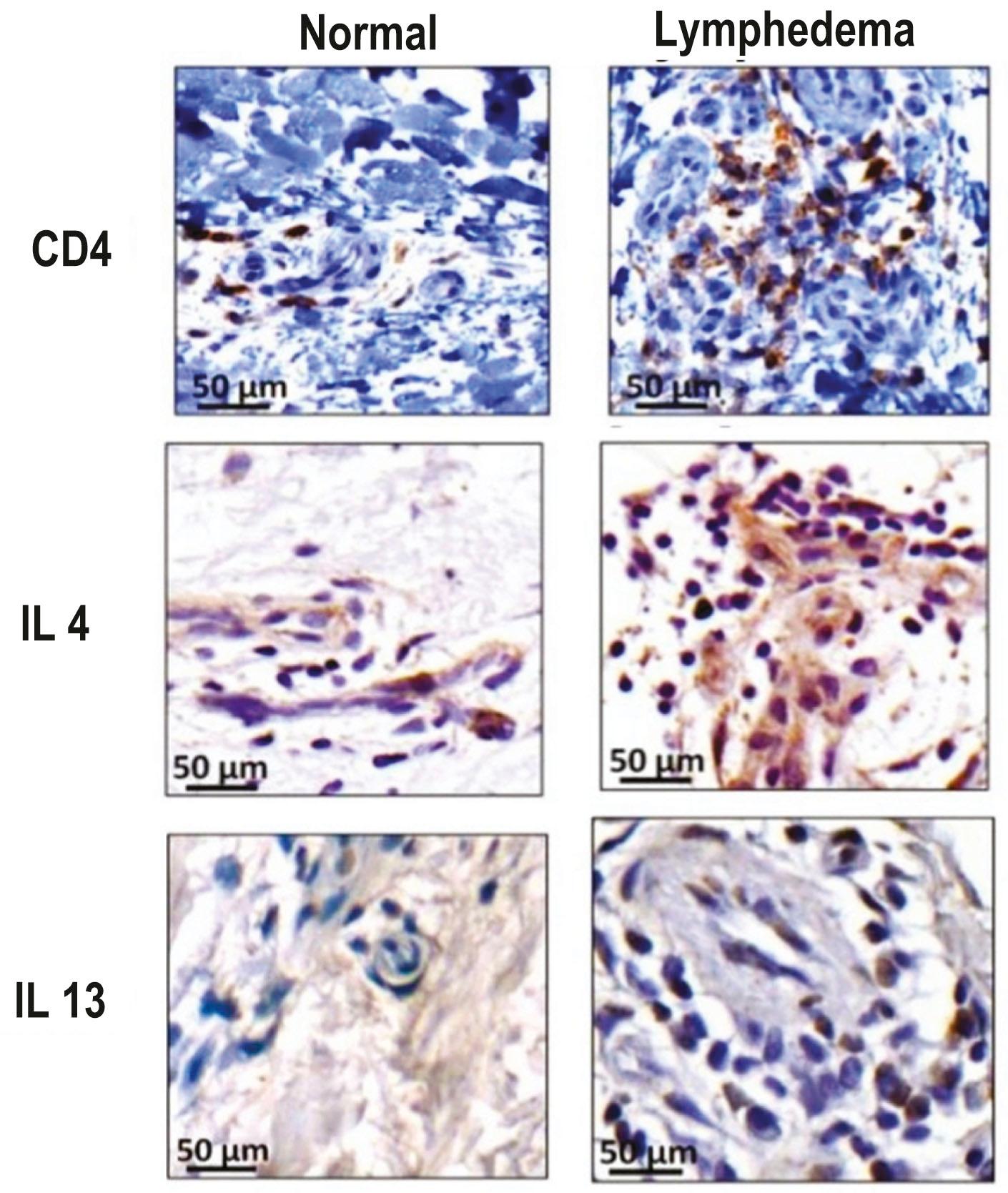
Rockson and colleagues were one of the first groups to suggest that inflammation plays a key role in lymphedema development. It was previously known that inflammation was a histological characteristic of the disease but recent studies have shown that inflammation may play a causal role. This group has not only shown that inflammation is increased in lymphedema, but also that treatment with anti-inflammatory medications decreases the severity of the disease.
Focusing on understanding the types of inflammatory reactions that occur in lymphedema, our lab has recently shown that activation and maintenance of chronic inflammatory mechanisms with resultant tissue fibrosis underlie these additional steps. We have shown that lymphedema develops after lymphatic injury in response to induced infiltration and differentiation of CD4 + cells into Th2 cells in the tissues, and that the degree of this inflammatory response correlates with the severity of lymphedema. Using antibody depletion studies and knockout mice, we have shown that CD4 + cell responses are necessary for the initiation and maintenance of lymphedema after lymphatic injury. Further, using mouse models and biopsy specimens, our group has demonstrated that Th2 cells critically influence the pathological mechanisms that translate lymphatic injury to the development of lymphedema, regulating multiple overlapping mechanisms, including lymphatic pump failure, impaired collateral vessel formation, adipose deposition and epidermal changes ( Figs. 28.7 & 28.8 ). A better understanding of these pathological processes is therefore imperative for improved diagnosis and development of targeted treatments and prevention options. Although a number of studies have analyzed lymphatic vascular changes in primary lymphedema and have identified a wide variety of defects, the remainder of this discussion will be dedicated to pathophysiological changes that occur in secondary lymphedema following cancer therapy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here