Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Lichenoid skin eruptions are a subcategory of papulosquamous skin disease. While most papulosquamous eruptions present with scaling papules, lichenoid eruptions differ in that the scale is often subtle, and the papules tend to remain small and discrete. On occasion, confluent plaques may form.
The term lichenoid has at least three commonly accepted applications/definitions:
Originally, “lichenoid” referred to a clinical resemblance of such eruptions to lichens (the latter a composite organism of algae or cyanobacteria living among filaments of fungus).
Lichen planus (LP) is the prototypical disease in this category, and eruptions sharing clinical features with LP may be described as “lichenoid.”
“Lichenoid” also refers to a histologic reaction pattern with as a “bandlike” infiltrate of mononuclear inflammatory cells (chiefly lymphocytes) subjacent to the dermoepidermal junction.
LP is a relatively common disorder, accounting for about 1% of all patient visits to dermatology clinics. The disease most often affects middle-aged adults. Although LP is thought to have no consistent gender predilection, some studies have found women to be more often affected. A recent meta-analysis regarding the incidence of oral LP found an overall age-standardized prevalence of 1.27% (0.96% in men and 1.57% in women).
Gorouhi F, Davari P, Fzel N. Cutaneous and mucosal lichen planus: a comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. ScientificWorldJournal. 2014;30:742826. (free text online.)
LP may affect both the skin and mucosa. Examination of both areas is essential when the diagnosis of LP is suspected. The frequency of involvement for these areas is somewhat controversial. In general, patients with mucosal disease may not demonstrate skin lesions, but 50% or more of patients with cutaneous disease will demonstrate mucosal lesions. Flexural areas, such as the wrists and ankles, are often involved. Other sites of preferential involvement include the neck, buttocks, sacrum, anogenital region, penis, and buccal or vaginal mucosa.
LP is a disease characterized by “P-words”:
P lentiful
P ruritic
P olished
P urple
P olygonal
P lanar
P apules and p laques
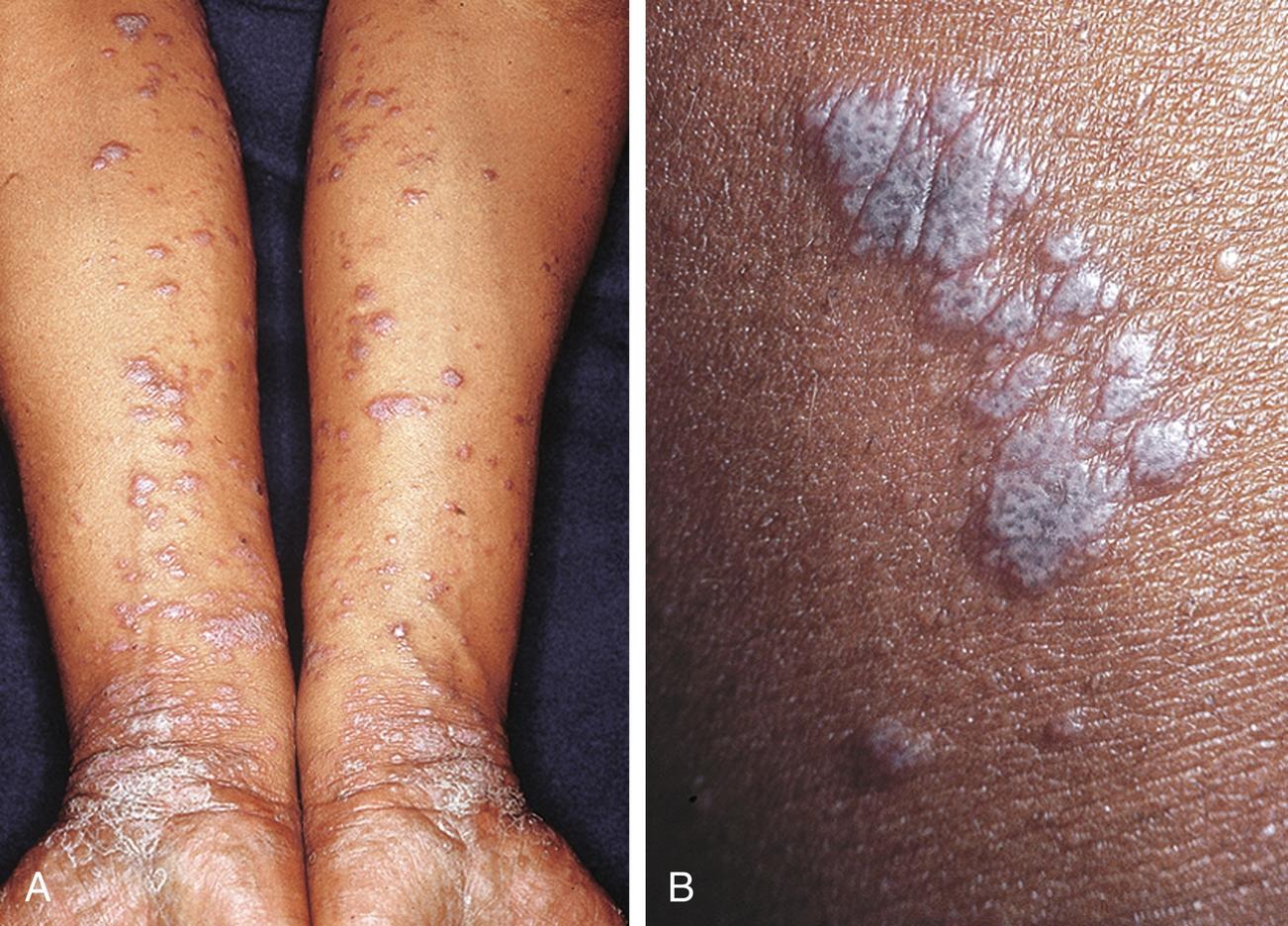
Primary lesions of the skin are 1- to 5-mm, flat-topped, violaceous, shiny papules ( Fig. 12.1 ). While papules are often clustered, individual lesions tend to be discrete, with angulated (polygonal) borders. Wickham’s stria, a lacy white network present on the surface of the papules, is often of great diagnostic value.
Mucosal lesions of LP differ from cutaneous lesions through demonstration of Wickham’s stria in the absence of a papular component. A white, reticulated, “netlike” pattern is often present upon the buccal mucosa, the tongue, or other mucosal surfaces ( Fig. 12.2 ). Other forms of mucosal LP may be ulcerative. Some experts believe that some cases of oral LP may be associated with mercury-containing dental amalgams, but the evidence is not conclusive. Still, others believe such cases represent a separate category of disease, more aptly termed a mercury-associated lichenoid stomatitis. The rate of malignant transformation in oral LP is low (< 2%).

Giuliani M, Troiano G, Cordaro M, et al. Rate of malignant transformation of oral lichen planus: a systematic review. Oral Dis. 2019;25:693–709. https://doi.org/10.1111/odi.12885 .
The isomorphic response (Koebner phenomenon) refers to the development of new lesions at sites of external trauma. This phenomenon is characteristic of both LP and psoriasis, among other rarer conditions. In LP, linear aggregates of papules may be induced by scratching or rubbing ( Fig. 12.3 ).

The cause of LP is unknown. Etiologic hypotheses include hypersensitivity reactions, viral infection (particularly hepatitis C), or autoimmune mechanisms. Case reports have linked LP to viral hepatitis, neurologic disease, and severe psychic trauma. Other autoimmune diseases such as vitiligo, inflammatory bowel disease, and autoimmune thyroiditis are seen with increased frequency in those with LP. Lichenoid eruptions (otherwise identical to idiopathic LP) may be a reaction to drugs or as a manifestation of graft-versus-host disease (GVHD) following allogeneic bone marrow transplantation. Oral disease and, to a lesser degree, cutaneous LP have been associated with hypersensitivity to dental amalgams. Most LP occurs in otherwise healthy people without an identifiable cause.
Tziotzios C, Lee JYW, Brier T, et al. Lichen planus and lichenoid dermatoses: clinical overview and molecular basis. J Am Acad Dermatol . 2018;79(5):789–804. https://doi.org/10.1016/j.jaad.2018.02.010 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here