Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hand infections are common, with diverse etiologies. It is important to have a high index of suspicion to allow expeditious diagnosis and treatment in order to prevent morbidity and maximize outcomes.
A thorough understanding of hand anatomy and the pathophysiology of hand infections is necessary to adequately provide treatment and improve functional outcomes.
The treatment of hand infections includes the combination of early diagnosis, empiric broad-spectrum antibiotics which is later tailored to culture data, and operative intervention.
Patients should be followed closely as hand infections can rapidly progress or spread to deeper tissues. If no clinical response is noted within 24–48 hours of initial intervention, the treatment plan should be reassessed.
A multidisciplinary team including physicians from the emergency department, radiology, infectious diseases, and hand surgery as well as hand therapists are important for global care of the patient with a hand infection.
Hand infections encompass a diverse array of diagnoses from paronychia involving the fingertip to necrotizing fasciitis of the hand and forearm. The etiology of infections is equally diverse; however, most are the result of direct inoculation of bacteria from penetrating trauma and lacerations. If not identified and treated expeditiously, these infections can result in significant morbidity.
The purpose of this chapter is to review the basic principles, evaluation, and management of patients presenting with infections based on anatomic location (fingertip, finger, hand, wrist, joints, and bone). We will also discuss atypical infections, and infection mimickers such as gout and pyoderma gangrenosum. A multidisciplinary team, including specialists from infectious disease, radiology, emergency medicine, primary care, and hand surgery, is necessary to effectively diagnose and manage infections of the hand.
Skin and soft-tissue infections account for 1.7% of all emergency department visits in the US. Further, hand infections remain one of the few surgical emergencies for hand surgeons and account for up to 35% of patients admitted to hand surgery services. The fingertip is the most common site for hand infections followed by the subcutaneous tissue of the dorsum and palm, tendon, joint and bone. The most frequent cause of major hand infections is a neglected wound with either a delayed presentation and/or appropriate initial treatment.
Numerous factors influence the development and severity of hand infections. The body is capable of preventing an infection with contamination of less than 10 5 bacterial organisms per gram of tissue. Higher concentrations of bacteria overwhelm phagocytic cells (polymorphonuclear cells and macrophages) and acute phase antibacterial proteins (lysozyme, C-reactive protein, interferon, and complement) to produce infection. Factors that impact the severity of infection include the anatomic location, virulence of the organism, viability and vascularity of the surrounding soft tissue, timing of intervention, and health status of the patient.
Immunocompromised patients are more vulnerable to and suffer increased morbidity from infection. Malnutrition, immunosuppression, immunodeficiency, alcohol or intravenous drug abuse, autoimmune disorders, systemic steroid use, and diabetes impair the immune response and increase risk of infection. These compromised hosts also have increased polymicrobial infections and opportunistic infections. Patients with weakened immunity may have attenuated clinical signs and symptoms which can lead to delayed recognition of infection and increased severity at presentation. Thus, it is important to have a high index of suspicion for infection when evaluating an immunocompromised patient with “hand pain”.
The treatment for hand infections dates back to the Golden Age of Greece and there have been many contributions to our understanding of and ability to treat infections over time. Hippocrates, a Greek physician, is often referred to as the “true father of hand surgery”. He was born in 460 BCE and authored works that described the treatment of wound infections in addition to the treatment of fractures, joints, and dislocations. His treatment principles were practiced and popularized in Greece and continue to hold true today. For example, in the treatment of infections, Hippocrates is quoted as saying that the dressing should be kept loose “so as not to intercept the pus but allow it to flow away freely”.
Although not clearly delineated in the literature with regards to hand surgery, a few important steps in the evolution of medicine and surgery have certainly impacted our current understanding and treatment of hand infections. In 1846, the first surgical procedure was performed using sulfur ether inhalational anesthesia at Massachusetts General Hospital. The development of “painless” surgery could then be used for the treatment of hand infections with surgical drainage. Contributing to the understanding of the basis of infection and its treatment in the mid-1800s, Louis Pasteur used heat to remove undesirable microorganisms, which was later termed “pasteurization”. This concept was recognized and utilized in the surgical arenas thereafter.
A momentous leap in the treatment of hand infections occurred when the relationship between hand anatomy and infection was established. In 1905, Allen Kanavel published his work on fascial and synovial spaces of the hand. Kanavel used injection studies to define the fascial spaces of the hand and described their patterns of communication. Based on his findings, he identified the appropriate location of surgical incisions which are still utilized today. A few years later, Kanavel also characterized infections as to their findings on exam. For example, he described the classic signs of flexor tenosynovitis, now referred to as Kanavel's cardinal signs, as well as advocated for thorough surgical debridement and drainage of established infections.
Finally, the introduction of antibiotics revolutionized the treatment of all infections. In 1929, Alexander Fleming identified a contaminant on a culture plate that inhibited growth of Staphylococcus . Years later this substance was purified and produced as the drug penicillin. Penicillin use became widespread in the 1940s and its positive impact on clinical results were evident. Although penicillin resistance was found early, alternative antibiotics have continued to be discovered and their importance in our current treatment algorithm for hand infections has not wavered.
Staphylococcus and Streptococcus species are the most common organisms to cause hand infection . S. aureus is particularly virulent, producing leukocidin, a neutrophil toxin. S. aureus has been reported to cause up to 80% of hand infections. Although gram-positive organisms are most common, gram-negative, fungal, mycobacterial organisms and viruses are also culprits, especially in polymicrobial infections. Methicillin-resistant S. aureus (MRSA) infections, both nosocomial and community acquired, have increased in prevalence over the past few decades. In the US, community-acquired MRSA is now responsible for the majority of hand infections. Risk factors for community-acquired MRSA include crowded living conditions such as day care, the homeless, inmates, athletes with shared clothing or sporting equipment, and military personnel. Empiric antibiotic coverage for presumptive MRSA infection is recommended based on the local prevalence of MRSA.
Although S. aureus is the most common culprit of hand infections, it is helpful to consider the etiology of the infection and associate it with the possible offending microbial organism. Human bites, or “fight bites”, are notorious sources of hand infections. Although S. aureus and alpha-hemolytic Streptococcus are usually isolated from these wounds, Eikenella corrodens is also found. Neisseria gonorrhea , a gram-negative diplococcus, should be considered in the young, sexually active patient with a hand infection without a clear nidus of infection. Domestic animal bites are usually polymicrobial, but are often associated with Pasteurella multocida . Fungal or mycobacterial organisms should be suspected in the presence of chronic, indolent infections. Atypical mycobacteria such as Mycobacterium marinum are associated with injuries from fishing, fish tanks, and swimming pools. Sporothrix schenckii and Enterobacter agglomerans infections occur following contamination with soil or plant material such as rose thorns.
Appropriate antibiotic coverage should be chosen based on the severity of infection and the exposure history. Ideally, antibiotics would be initiated after Gram stain and cultures are obtained. In cases of severe infections, a multidisciplinary approach including an infection specialist is recommended to adequately treat the patient and optimize outcomes. Current antibiotic recommendations for common organisms are listed in Table 15.1 .
| Organism | Antibiotic | Additional information |
|---|---|---|
| Methicillin-sensitive Staphylococcus aureus | Cephalexin, amoxicillin-clavulanate (orally) | |
| Methicillin-resistant Staphylococcus aureus |
|
|
| Vancomycin-resistant enterococci | Daptomycin, linezolid (orally or IV), tigecycline (IV), quinupristin/dalfopristin (IV) | |
| Gram negative |
|
|
| Pseudomonas |
|
|
| Anaerobic infections |
|
|
| Vibrio vulnificus |
|
|
| Nocardia | Trimethoprim/sulfamethoxazole. If sulfa allergy: imipenem, ceftriaxone, amikacin | 6 months of treatment in immune-suppressed patients |
| Sporothrix schenckii |
|
|
| Mycobacterium marinum |
|
|
| Aeromonas hydrophilia |
|
|
| Cutaneous anthrax |
|
Treatment for 60 days to treat any remaining spores |
| Tularemia | Gentamicin and doxycycline |
Early recognition and intervention improve outcomes.
Identify risk factors: Immunocompromised? Diabetes? Steroid use?
Obtain baseline lab work, radiographs, and blood cultures.
Obtain wound cultures and start empiric antibiotics. Cover for MRSA if local prevalence is high.
Once an area of fluctuance and/or abscess is identified, surgical intervention with incision, drainage, irrigation and debridement should be performed.
Plan for multiple washouts (every 24–48 hours) until infection is controlled.
Immobilize the extremity for tissue rest and elevation.
Once tolerable, begin aggressive hand therapy to maximize return of function.
Pain, erythema, edema, fluctuance, and tenderness are prominent features of an existing hand infection. Systemic signs are often rare. Early recognition and intervention can greatly improve outcomes.
When evaluating a patient with a possible hand infection, it is important to perform a thorough medical history to identify risk factors. Handedness, occupation, immunization history (e.g. tetanus), smoking, drug or alcohol abuse history, and previous surgeries or trauma are important details to obtain. Prior personal or family history of MRSA infections is suggestive of another MRSA infection. On physical exam, it is important to assess the entire extremity for lymphangitic spread, indicating clinically advanced infection. A head-to-toe examination should also be performed to identify other sources or concomitant sites of infection.
Routine laboratory studies such as the white blood cell count (WBC) and the erythrocyte sedimentation rate (ESR) are often normal in the evaluation of a hand infection. When elevations do occur, they are usually associated with more severe cases. Measurement of the acute-phase reactant C-reactive protein (CRP) can be helpful when monitoring treatment response, especially in patients with osteomyelitis. The CRP level can elevate in response to a variety of stressors or clinical conditions such as surgery or trauma. Thus, it is sensitive, but nonspecific. In cases requiring long-term parenteral antibiotics, i.e. osteomyelitis, flexor tenosynovitis, or necrotizing fasciitis, blood cultures should be obtained. These should be negative prior to any long-term indwelling line being placed.
Radiographic imaging is important in the assessment of hand infections. Plain radiographs should be taken with any presenting hand infection to rule out the presence of a foreign body or subcutaneous emphysema. They will also allow for assessment of the underlying bone and joints, providing either diagnostic information or a baseline from which to compare in the future as radiographic evidence of osteomyelitis occurs 2–3 weeks after the onset of infection. Ultrasound and magnetic resonance imaging (MRI) are also useful tools for the diagnosis and treatment of musculoskeletal infections. Ultrasound can diagnose early suppurative flexor tenosynovitis, localize foreign bodies and/or focal fluid collections. MRI is useful for early detection of osteomyelitis and can be used for evaluation of cellulitis, abscess formation, and necrotizing fasciitis. For the diagnosis of osteomyelitis in the presence of hardware, a tagged 99 mTc-labeled white blood cell radionuclide scan with bone marrow imaging can be performed. This study avoids the confounder of artifact or scatter seen on computed tomography (CT) or MRI.
Early or superficial infections, including cellulitis, may respond to nonsurgical intervention. Antibiotics, immobilization, and elevation should be initiated. Patients should be followed closely as the infection can rapidly progress or spread to deeper tissues necessitating operative management. Further, if no clinical response is noted following nonoperative treatment, deeper involvement should be suspected. Once an area of fluctuance and/or abscess is identified, surgical intervention with incision, drainage, irrigation, and debridement should be performed. Ideally, cultures would be obtained prior to the administration of antibiotics. Fluid should be sent for Gram stain, aerobic and anaerobic cultures, and sensitivities. Fungal stains, fungal cultures, and mycobacterial cultures should be sent if suspicion is high or if the patient is immunocompromised.
In the following section we review the basic principles, evaluation, and management of specific upper extremity infections according to anatomic location. A comprehensive understanding of hand anatomy including the intricate synovial connections and spaces are essential for adequate treatment and improved surgical outcomes.
Assess for abscess formation deep to the nail plate that may require removal of part of or the complete nail.
Incise away from the nail plate to avoid inadvertent injury to the germinal matrix.
Be sure to leave a small drain or gauze wick to prevent premature closure of the eponychium.
Rule out herpetic whitlow at the time of presentation.
Paronychia accounts for 30–50% of all hand infections, making it the single most common infection in the hand. This infection is most commonly caused by Staphylococcus aureus followed by Streptococcus and Pseudomonas . Paronychias originate from either the proximal nail fold or the paronychium (skin fold on either lateral side of the nail plate). The infection typically begins unilaterally or just proximal to the nail. Untreated, the paronychia can expand around the nail, which is termed the “runaround” infection. The infection may also spread deep between the nail plate and the nail bed. Acute bacterial infection follows disruption of the barrier between the nail plate and the surrounding nail folds such as may occur with manicures, hangnails, or nail biting.
Early paronychia presents with pain, redness, and swelling ( Fig. 15.1 ). As the infection progresses, gross purulence may collect around, or deep to, the nail plate. Extension toward the palmar fingertip may result in a felon. Before developing an associated abscess, the developing paronychia is treated with oral antibiotics and warm soapy soaks.

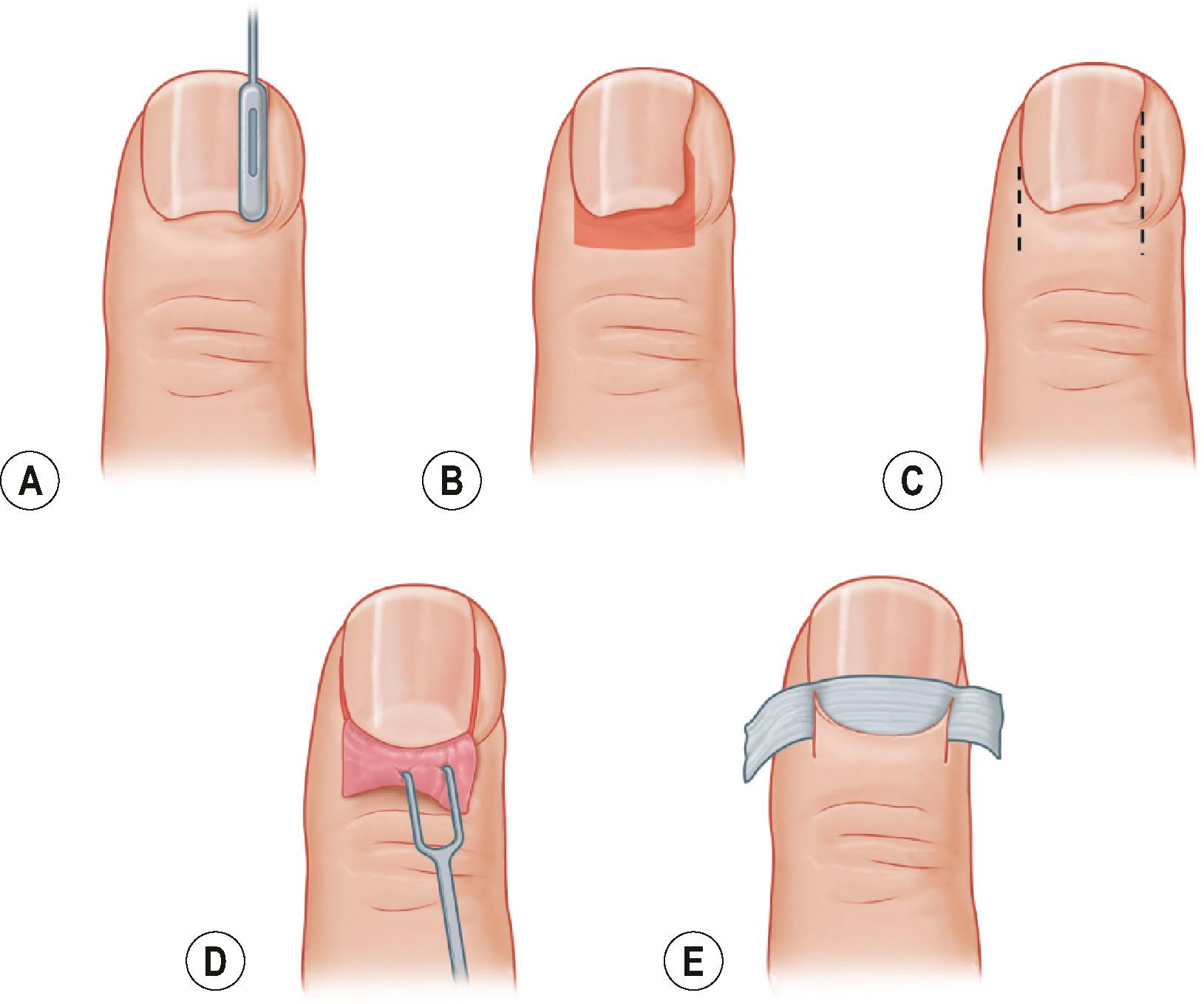
After developing an abscess, drainage is required. Small abscesses with thin skin coverings can be unroofed and cultured. However, in many of the cases referred for hand specialty care, formal surgical decompression is required. This decompression is performed with a digital block and a small elastic digit tourniquet. The authors recommend first elevating the involved proximal or lateral nail fold from the nail plate. If purulence has accumulated deep to the nail plate, then at least part of the nail is removed. Skin incisions are made parallel to the lateral nail folds if required. Paronychia involving the proximal nail fold may be incised transversely over the most superficial portion of the abscess or decompressed with incisions extending proximally from the corners of the nail fold ( Fig. 15.2 ). In cases in which skin incisions are required, we leave a thin plastic drain or cotton gauze wick to allow passive egress of fluid. Patients are allowed to remove the drain/wick and dressing 1–2 days after surgery and continue soapy water soaks twice a day until all wounds are sealed and dry.
Chronic paronychia is a distinct entity most commonly found in patients with prolonged exposure of the fingertips to a wet environment – i.e., bartenders, swimmers, dishwashers, food-handlers, nurses – and has been associated with previous diagnoses of diabetes and psoriasis. By definition, a paronychia is chronic after being present for at least 6 weeks. Candida albicans is the primary pathogen responsible for chronic paronychia, although gram-positive cocci, gram-negative rods, and mycobacteria have all been implicated by culture data from the subungual space. Patients with chronic paronychia present with thickened, indurated, and erythematous tissue proximal to the nail plate ( Fig. 15.3 ). Nail plates may become thickened and discolored. The eponychial fold may retract. The pain associated with chronic paronychia is less impressive than that reported during acute paronychia infection. Chronic paronychia may involve multiple fingertips.

Treatment for chronic paronychia is frequently surgical but a trial of topical antifungal cream (2% ketoconazole or 2% miconazole) or oral antifungal medication (itraconazole or fluconazole) may be attempted. In the authors’ experience, this may take months to obtain results and these medications are prescribed by a dermatologist. Eponychial marsupialization is the surgical treatment for chronic paronychia ( Fig. 15.4 ). Performed with a digital block and tourniquet at the base of the finger, a 3–5mm-wide crescent-shaped portion of skin is removed starting 1 mm proximal to the eponychial fold. Although marsupialization has been described to various depths, the authors have removed the entire dermal layer but left the roof of the germinal matrix intact. Removing the deformed nail plate has reduced recurrence of chronic paronychia. The wounds are left open for healing via secondary intention. Soft gauze dressings are changed once or twice a day until the wounds have healed. Patients are also started on a course of antibiotics, which are de-escalated based on intraoperative cultures. In our experience, marsupialization has been effective but changing the patient's occupational or leisure activities to minimize prolonged exposure of the fingertips to liquids is important to prevent recurrence.
Paronychia must be differentiated from herpetic whitlow at the time of presentation. Herpetic whitlow is a viral infection caused by herpes simplex type 1 (60% of cases) or 2 (40% of cases). It is caused from a viral inoculation of the host via infected body fluids. The virus invades the dermis and subcutaneous tissue and symptoms begin 2–14 days after exposure. Symptoms of this infection include a painful, burning or tingling sensation of the affected digit followed by erythema, edema, and the development of 1–3 mm grouped vesicles over the next 7–10 days ( Fig. 15.5 ). The infection is usually self-limiting with resolution within 3 weeks. Herpetic whitlow is characterized by a primary infection followed by a latent period in which the virus enters the cutaneous nerve endings and migrates to the peripheral ganglia. Recurrences can be induced with physiologic or psychological stress, fever, and sun exposure. Unroofing the vesicles may allow for a definitive diagnosis, usually with culture and Tzanck smear, but deeper debridement risks secondary bacterial infection or more disseminated herpetic infection. Other potential mimics of paronychia include pemphigus vulgaris, drug-induced paronychia associated with isotretinoin, and swelling secondary to trauma; such diagnoses may be considered in the setting of refractory paronychia.

Protect neurovascular bundles should a midaxial approach be indicated.
Surgical decompression requires blunt dissection of all pulp septae to adequately evacuate the infection regardless of incision used.
Avoid violation of the flexor tendon sheath to prevent iatrogenic flexor tenosynovitis.
Postoperative management should include the use of antibiotics, gauze wick to allow for subsequent drainage, soaks, and early range of motion.
A felon is an infection in the subcutaneous pulp space of the fingertip. Staphylococcus aureus remains the most common causative organism. Felon infections have been demonstrated to be increasingly secondary to community-acquired MRSA, and polymicrobial infections have been described.
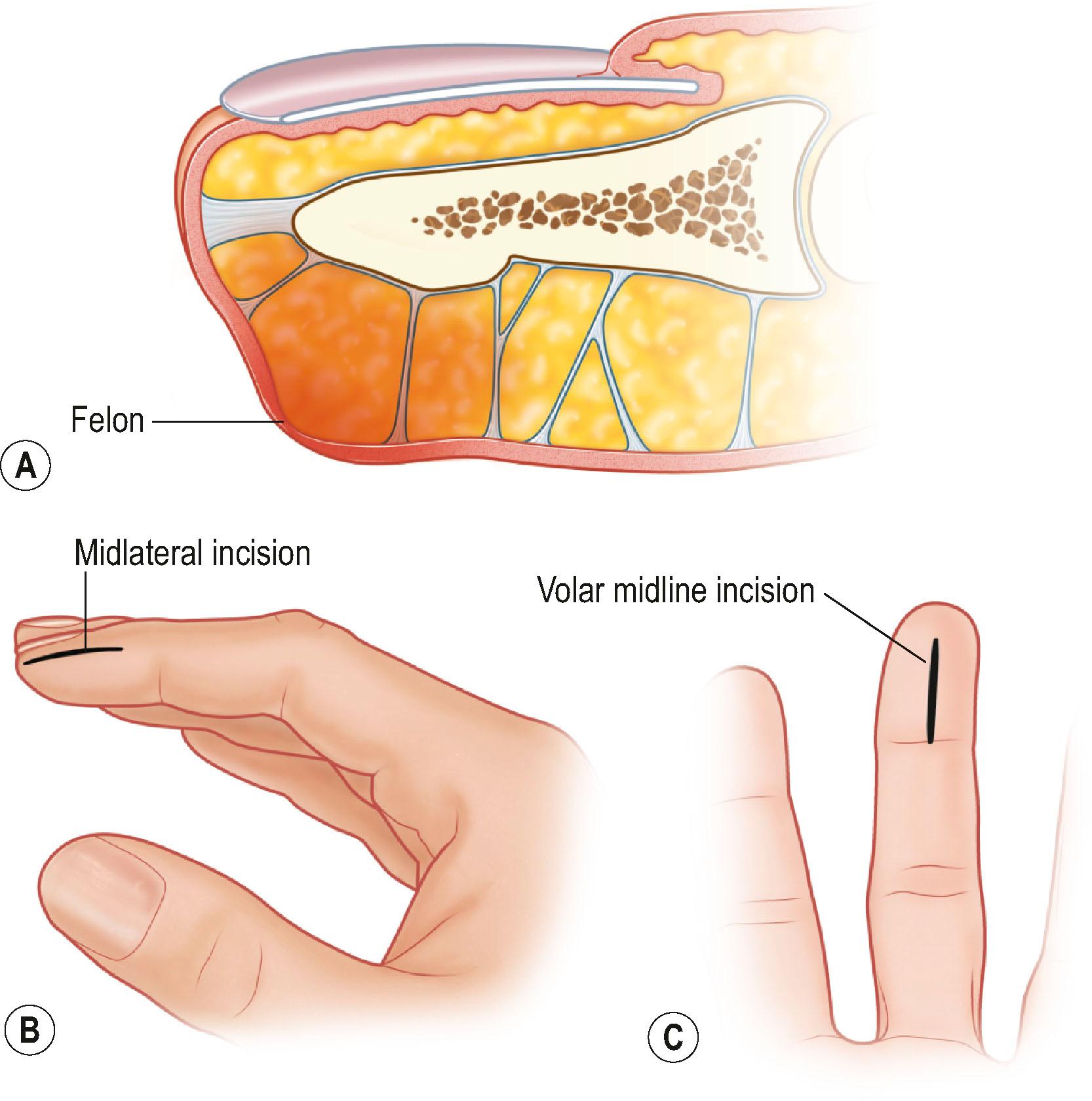
A felon behaves like a deep space infection forming an abscess because it is confined within the matrix of vertical fibrous septa in the pulp space. Felons most commonly follow penetrating trauma to the fingertip. Patients present with painful swollen fingertips that are exquisitely tender over the pulp space ( Fig. 15.6 ). The swelling and pain should be confined to the pulp space distal to the distal interphalangeal flexion crease. When not treated, the felon may progress to cause tissue necrosis in the pulp space, or seed infection into the distal phalanx (osteomyelitis and/or tendon rupture), adjacent interphalangeal joints (septic arthritis), or the flexor tendon sheath (tenosynovitis). Failure to identify osteomyelitis may result in recurrent infection, and subsequent reoperation or amputation, so plain radiographs should be considered at the time of presentation.

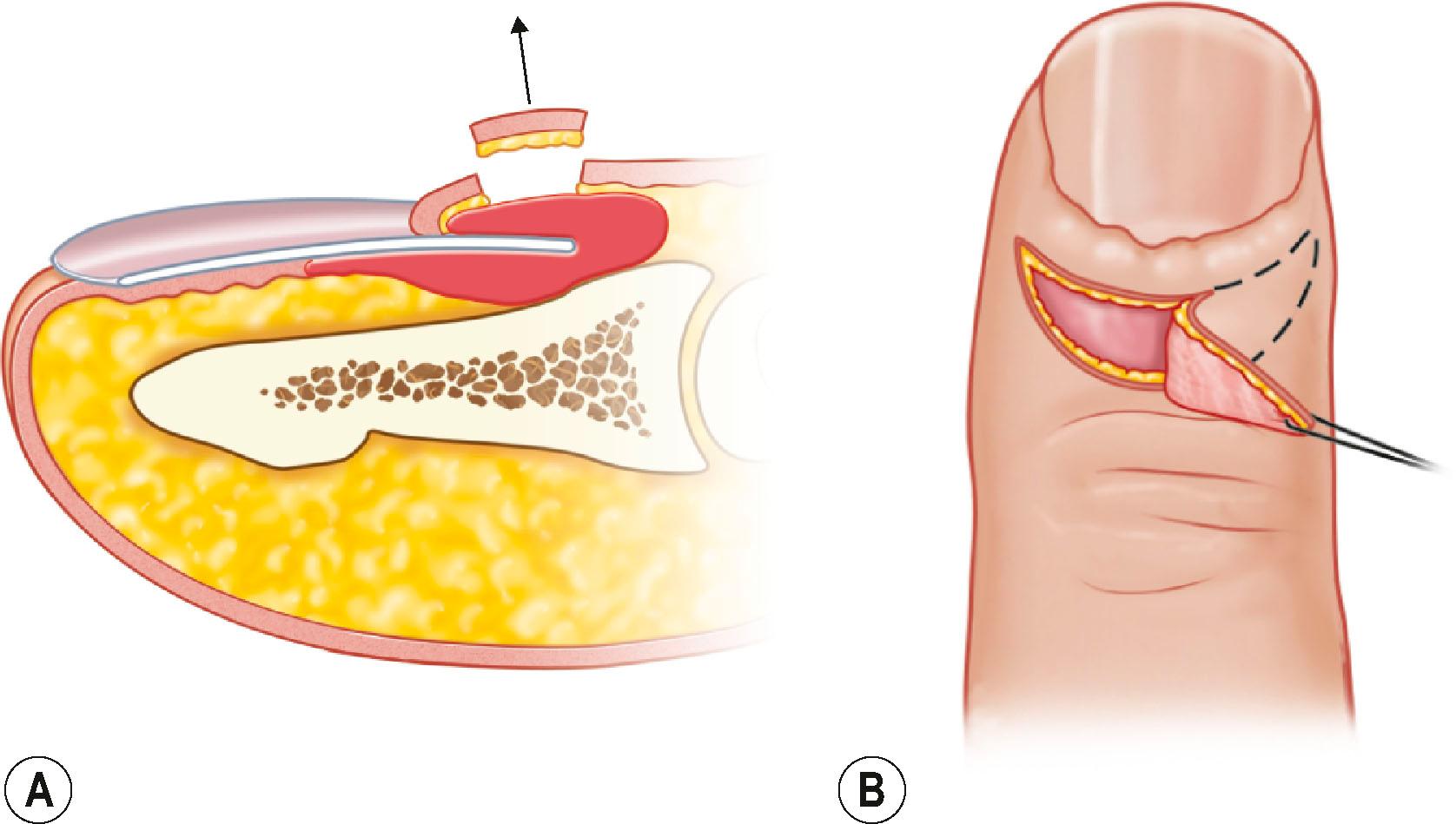
With the exception of the rare pulp space infection presenting prior to abscess formation, felons require surgical decompression. Similar to paronychia, various surgical approaches are described; however, so-called fish-mouth incisions risk devascularizing the pulp, leading to further tissue necrosis, and therefore should be avoided ( Fig. 15.7 ). A longitudinal incision in the pulp space is an approach that minimizes risk to the digital neurovascular structures. Alternatively, a midaxial incision may be used (typically radial side of small finger and thumb, ulnar side of index, long, and ring fingers to minimize the chance of painful pinch or resting the hand on a painful scar). Regardless of the skin incision, blunt dissection with a tenotomy scissor or hemostat is required to disrupt the fascial bands in the pulp space to ensure complete decompression. Nonviable tissue is debrided and the wound is irrigated. A small plastic drain or cotton gauze wick is left in the wound and dressing changes with soapy water soaks and drain/wick removal commence the following day. Most cases may resolve in 3–4 weeks with appropriate management; however, pulp instability may persist for 6 months to 1 year, and if encountered, pulp deformity and atrophy may be a permanent sequela.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here