Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]()
![]() Access video and video lecture content for this chapter online at Elsevier eBooks+
Access video and video lecture content for this chapter online at Elsevier eBooks+
With increasing societal acceptance and insurance coverage of gender affirmation surgery (GAS), plastic surgeons are caring for more transgender and gender diverse (TGD) people. This chapter will provide a succinct overview of the TGD population along with the assessment, perioperative management, and basic technical aspects of the most performed GAS procedures. Due to the complexity and heterogeneity of approaches to facial feminization and masculinizing genital surgery, the discussion will focus less on technical details and more on a conceptual framework.
A brief overview of terminology used in this chapter and definitions are outlined in Box 39.1 . It is of utmost importance to realize that the TGD community is very diverse, and many may not need or seek GAS, in fact, some may not even experience gender dysphoria despite gender incongruence. Those who come to see a plastic surgeon are generally seeking GAS and evaluation should include whether or not they have met the World Professional Association for Transgender Health (WPATH) Standards of Care (SOC), Version 8 (SOC8) guidelines ( Table 39.1 ). The guidelines are there to support individuals seeking affirming care with the intent of transitioning and affirming their gender. They are based on the most recent evidence-based data available and are periodically updated. Some insurance providers still follow SOC7 criteria ( Table 39.2 ![]() ). At its core, it emphasizes the importance of a multidisciplinary approach, including medical and mental health requirements that need to be met prior to being eligible for GAS. The SOC are what most insurance providers use and surgeons performing GAS should document met criteria.
). At its core, it emphasizes the importance of a multidisciplinary approach, including medical and mental health requirements that need to be met prior to being eligible for GAS. The SOC are what most insurance providers use and surgeons performing GAS should document met criteria.
| Term | Definition |
|---|---|
| Cisgender | People whose gender identity corresponds to the sex they were assigned at birth. |
| Gender affirmation | Being recognized or affirmed in a person’s gender identity. It is usually conceptualized as having social, psychological, medical, and legal dimensions. |
| Gender-affirming surgery | A term used to describe surgery to change primary and/or secondary sex characteristics to affirm a person’s gender identity. |
| Gender diverse | A term used to describe people with gender identities and/or expressions that are different from social and cultural expectations attributed to their sex assigned at birth. |
| Gender dysphoria | A state of distress that may be experienced because a person’s gender identity differs from that which is physically and/or socially attributed to their sex assigned at birth. Gender dysphoria is a diagnostic term in the DSM-5 denoting an incongruence between sex assigned at birth and experienced gender accompanied by distress. |
| Gender identity | A person’s deeply felt, internal, intrinsic sense of their own gender. |
| Gender incongruence | A marked and persistent incongruence between an individual’s experienced gender and the assigned sex at birth. ICD-11 classification under conditions related to sexual health. |
| Sex assigned at birth | A person’s status as male, female, or intersex based on physical characteristics, usually based on appearance of the external genitalia. |
| Transgender | Umbrella term used to describe people whose gender identities and/or expressions are not what is typically expected for the sex they were assigned at birth. |
| Criteria | Facial surgery | Breast augmentation | Mastectomy | Gonadectomy | Genital surgery |
|---|---|---|---|---|---|
| Letter from health care professional with competencies in the assessment of TGD individuals | 1 | 1 | 1 | 1 | 1 |
| Gender incongruence marked and sustained | ✓ | ✓ | ✓ | ✓ | ✓ |
| Demonstrates capacity to consent for the specific gender-affirming surgical intervention | ✓ | ✓ | ✓ | ✓ | ✓ |
| Meets diagnostic criteria for gender incongruence in regions where diagnosis is necessary to access health care | ✓ | ✓ | ✓ | ✓ | ✓ |
| Fertility counseling | ✓ | ✓ | |||
| Other causes for gender incongruence identified and excluded | ✓ | ✓ | ✓ | ✓ | ✓ |
| Mental health and physical conditions that could negatively impact the outcome of gender-affirming surgical intervention have been assessed as well controlled | ✓ | ✓ | ✓ | ✓ | ✓ |
| Stable on their gender-affirming hormonal treatment (at least 6 months or longer if required for surgical results) a | ✓ | ✓ | ✓ | ✓ | ✓ |
a Unless hormone therapy is not desired or is medically contraindicated.
| Criteria | Facial surgery | Breast augmentation | Mastectomy | Genital surgery |
|---|---|---|---|---|
| Letters from mental health providers trained in transgender health | 0 Letters | 1 Letter | 1 Letter | 2 Letters |
| Persistent, well-documented gender dysphoria | ✓ | ✓ | ✓ | |
| Capacity to make a fully informed decision and consent to treatment | ✓ | ✓ | ✓ | ✓ |
| Age of majority in a given country | ✓ | ✓ | ✓ | ✓ |
| Well-controlled medical or mental health comorbidities, if present | ✓ | ✓ | ✓ | ✓ |
| 12 continuous months of hormone therapy as appropriate for patient’s gender goals (unless medically contraindicated or patient unable to take hormones) | ✓ | ✓ | ||
| 12 continuous months of social transition | ✓ a |
a Only for genital reconstruction and not surgical castration/surgical removal of sexual organs.
Due to the historic and current discrimination and transphobia that many TGD individuals experience, we recommend healthcare professionals approach each interaction in an affirmative manner. Misgendering or perceived microaggressions can have a substantial impact on an individual’s comfort and mental health. Using the correct pronouns and names, which may differ from legal name, as well as creating a welcoming environment for this population is vital.
Prior to undertaking any GAS, individuals undergo a readiness evaluation by a qualified medical professional with experience working with TGD individuals and capacity to diagnose gender incongruence. This includes evaluation and management of expectations, developing coping strategies, determination of need for active perioperative mental health support, and evaluating adequate perioperative social support. If significant mental health conditions are present, they should be optimized. It must be recognized that some mental health conditions are because of or aggravated by the presence of gender dysphoria, and are less likely to improve significantly without access to GAS. If an individual receives exogenous hormones the prescribing healthcare professional should establish adequate hormone levels and duration prior to GAS. Especially for complex genital procedures, it is important to have a cohesive multidisciplinary team including mental health, primary care, and hormone providers, as well as social workers to provide optimum patient care.
Common hormone therapies as well as their potential main side effects are listed in Table 39.3 . While it is common for those assigned female at birth (AFAB) to be on testosterone and those assigned male at birth (AMAB) to be on estrogen and/or anti-androgens, there are individuals who will not be on hormones either due to medical contraindications or due to their individual gender identity. Some, despite gonadectomy, may take the hormone associated with their birth sex for medical reasons. Moreover, there is ongoing controversy around the management of estrogen during the perioperative period for GAS. While there are some data that suggest continuation of estrogen is safe, these data are not robust enough to fully delineate standardized protocols.
| Therapy | Main side effects |
|---|---|
| Estrogens | Deep venous thrombosis (transdermal administration may lessen these risks) |
| Progesterone | Increased cardiac and cancer risks |
| Anti-androgens (i.e., spironolactone) | Potential effects on electrolytes |
| Testosterone | Polycythemia and lipid alterations |
Some surgeons will stop all estrogen 2–4 weeks prior to surgery, others will reduce the dose, and some will continue it. It is generally accepted to continue testosterone perioperatively.
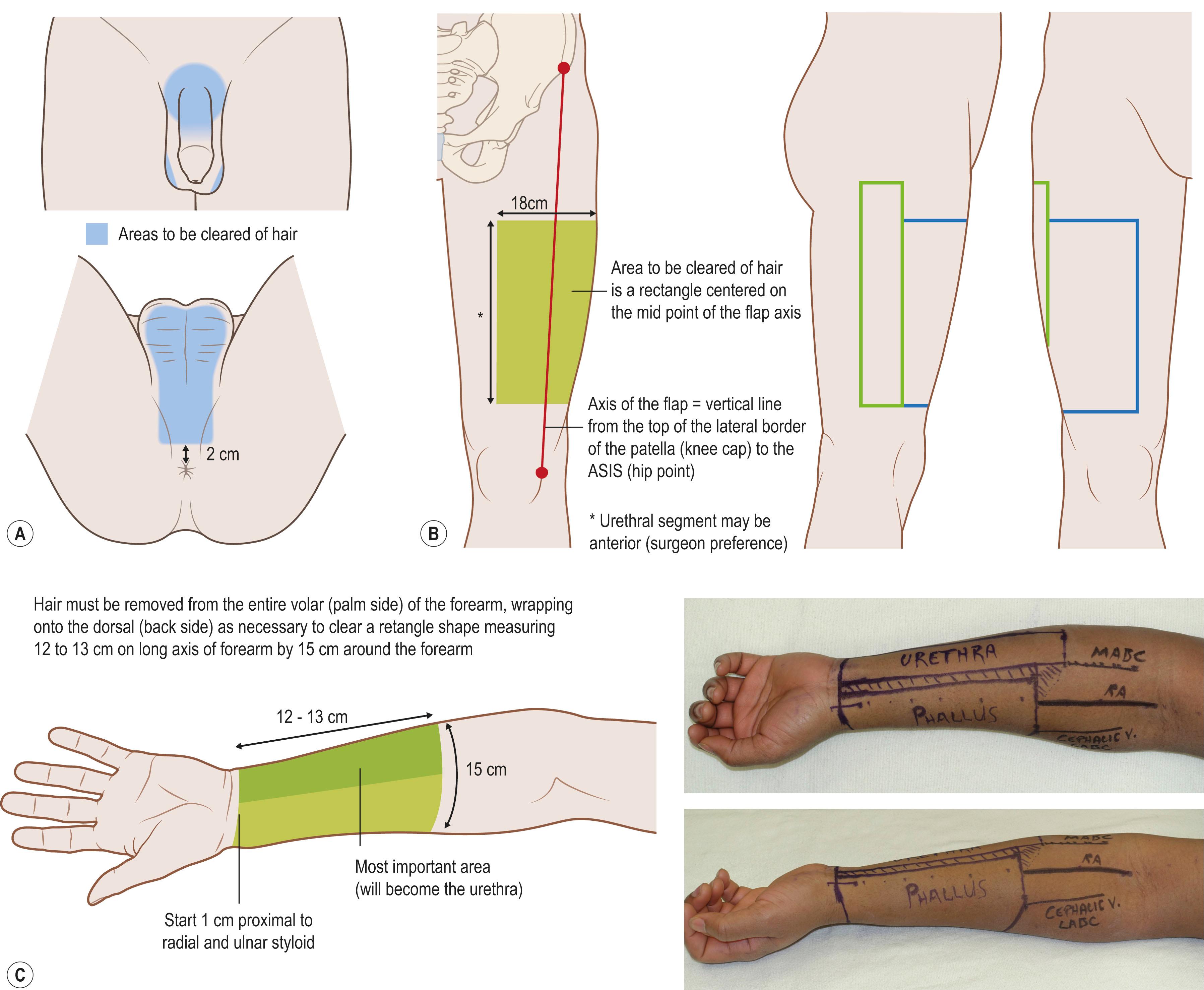
Because intraurethral or intravaginal hair is morbid and there are no effective treatments, most surgeons performing vaginoplasty and phalloplasty require hair removal prior to surgery. The choice of laser hair removal or electrolysis should be individualized depending on the patient’s hair color and density. Diagrams illustrating hair removal patterns are shown in Fig. 39.1 . For facial surgery, hair removal is not a requirement but is an important adjunct.
For chest GAS, TGD individuals present with varying requests. Most frequently, a chest masculinizing procedure is desired with the goal of obtaining a chest without a breast mound or skin redundancy, and the nipple–areolar complex (NAC) in a more lateralized position and of smaller dimensions. Although limited scar options with or without skin excision (periareolar, circumareolar, extended circumareolar) may be appropriate in selected patients, the majority of patients will require a simple mastectomy including skin resection with or without NAC grafting. Patients who require significant skin removal but desire a vascularized NAC may be candidates for a pedicled “buttonhole” mastectomy. Lastly, a subset of patients may desire some degree of breast mound and choose a wise pattern breast reduction. In this section we will focus on decision-making and the most frequently offered surgeries: Double incision with or without NAC graft, periareolar and circumareolar mastectomy.
In addition to criteria from the WPATH SOC8, a full assessment of risk factors for breast pathology is essential for each patient. In patients of appropriate age, screening mammography should be completed within a year prior to surgery. If a genetic breast cancer predisposition is suspected or if imaging is suggestive of a potential malignant lesion, then further work-up by a qualified breast oncologist is important. If that referral recommends an oncologic mastectomy, then a combined procedure with plastic surgery for chest contouring can be considered. Patient expectations and goals should be discussed along with evaluation of the breasts and chest.
The Fischer grading scale is useful to inform surgical approach to gender-affirming mastectomy ( Fig. 39.2 ). Skin laxity and quality, degree of ptosis and glandular volume are the components that need assessment ( Table 39.4 ). Algorithm 39.1 is recommended for determining the type of mastectomy.
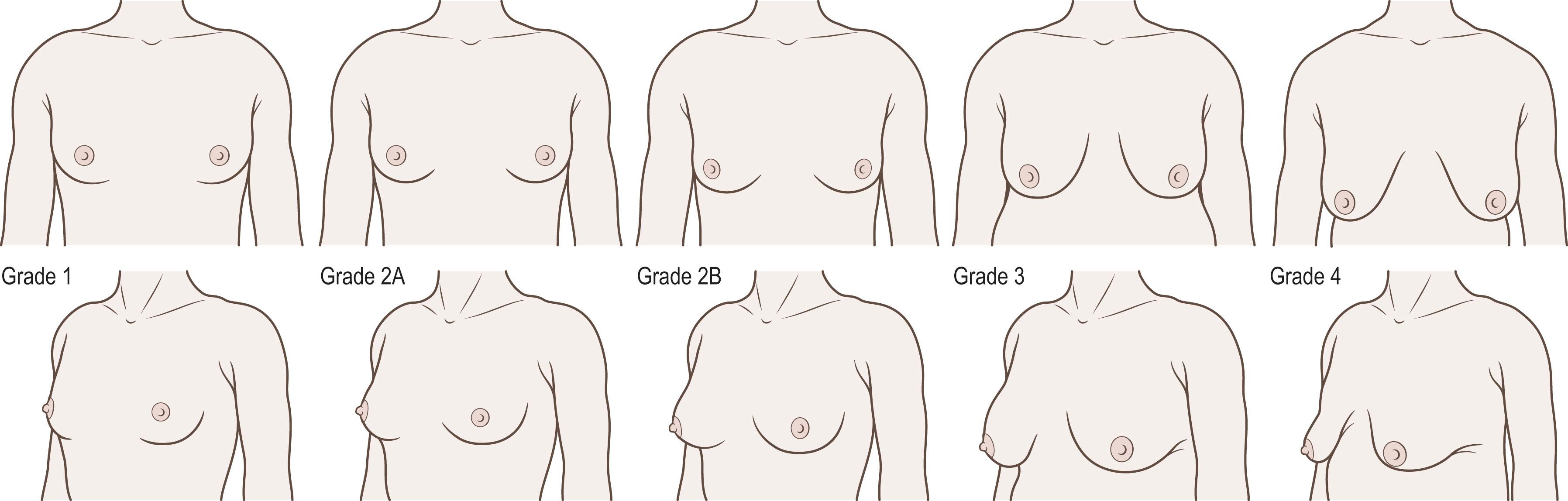
| Fischer Grade | Skin laxity | Degree of ptosis | Glandular tissue volume |
|---|---|---|---|
| Grade 1 | No laxity | NAC above IMF | Minimal |
| Grade 2A Grade 2B |
Little to no laxity Increased laxity |
NAC above IMF NAC at or below IMF |
Moderate Moderate |
| Grade 3 | Irrespective | NAC below IMF | Significant |
| Grade 4 | Significant | NAC below IMF | Deflated breast |
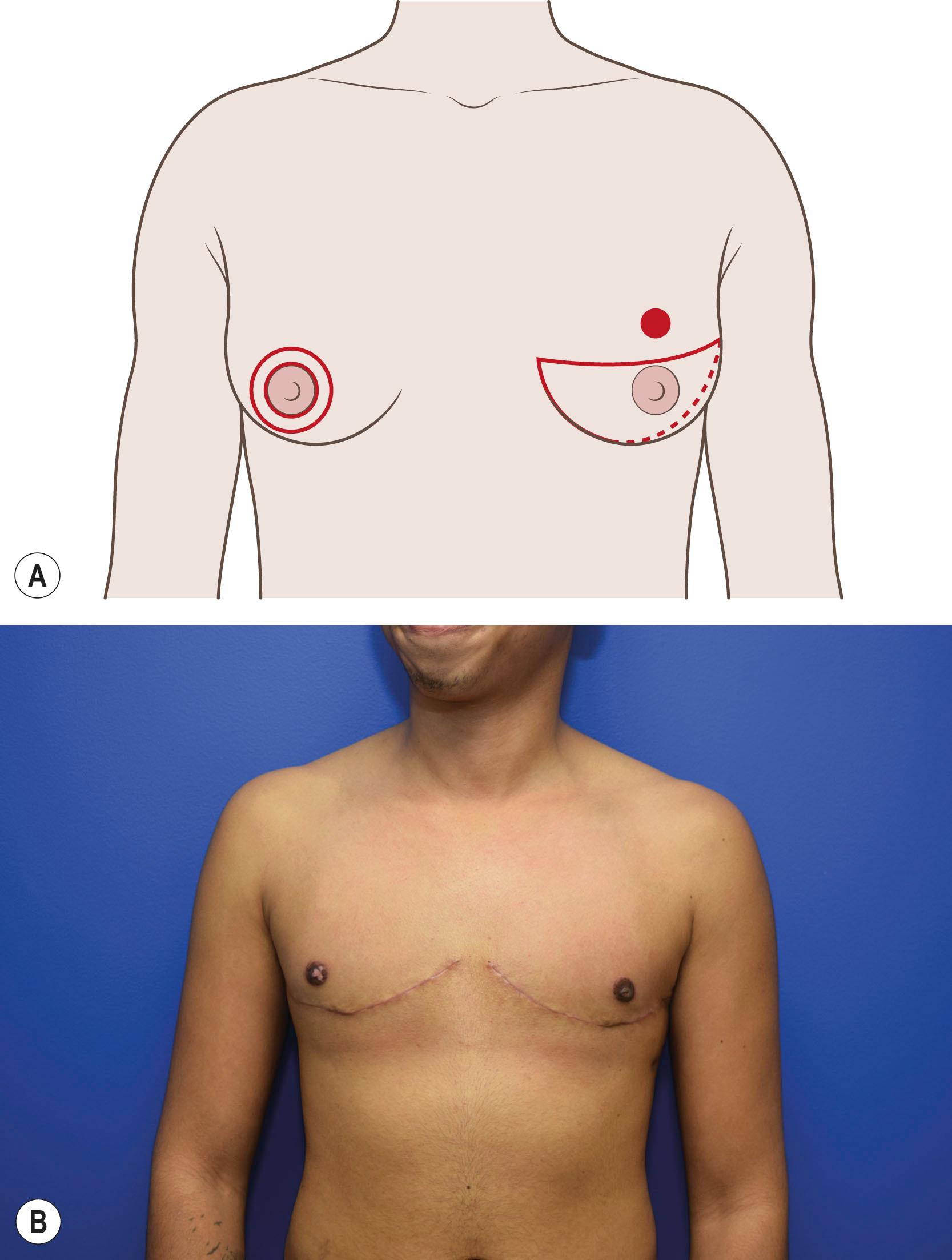
DIFNG is the most performed chest contouring procedure for two principal reasons. First, most patients present with significant excess of both breast volume and skin, and many, even those with modest breast volume, can develop significant ptosis and skin laxity due to prolonged breast binding. In addition, DIFNG has consistently been found to have lower revision rates compared with other approaches. Preoperative markings will vary by patient and surgeon, but the goal is to achieve a final incision that is gently curved and ideally mirrors the border of the pectoralis major. If there is excess axillary subcutaneous adiposity, the excision can be extended laterally to allow for contouring of this area. Liposuction, while a viable adjunct, does not contour this area as well as direct excision in most cases. To avoid midline skin excess, some surgeons allow a single incision that crosses midline; others will avoid this in favor of a minor revision later. The approximate NAC position is placed at the lateral two-thirds of the clavicle and a finger breadth above the planned incision along the pectoralis border and can be adjusted per patient preference ( ![]() and Fig. 39.3A ). If using the inferior pedicle technique, the 6-8 cm pedicle can be drawn within the planned transverse incisions.
and Fig. 39.3A ). If using the inferior pedicle technique, the 6-8 cm pedicle can be drawn within the planned transverse incisions.
In the operating room, the planned FNG is sized in a smaller oval shape (~2 × 3 cm) and removed full thickness and thinned appropriately. The superior chest flap is elevated just above the breast capsule, but can be made thicker to approximate the upper abdominal subcutaneous thickness. Once tension-free closure is confirmed, the inferior incision is made, and the breast is removed above the pectoralis fascia. The IMF is released, and the incision is closed in layers over a drain. If needed the patient can be sat up for confirmation of NAC placement. The planned placement position for the NAC is de-epithelialized and the FNG secured with a bolster. ![]() shows this surgical approach.
shows this surgical approach.
If the inferior pedicle “buttonhole” technique is used, then the planned pedicle is de-epithelialized and raised in the plane just above the breast capsule. In this approach, pedicle length and tension may limit options for NAC positioning.
In the circumareolar technique, the new NAC is sized as above, but not removed. The remainder of the old NAC is de-epithelialized and a full-thickness incision is made from 3 o’clock to 9 o’clock (see Fig. 39.3A ). A lateral incision can be made to allow for ease of mastectomy. The mastectomy is performed through this incision with 1–2 cm of tissue left below the NAC for perfusion. Once the breast is removed it is important to generously release circumferential attachments including the inframammary fold (IMF) to allow for redraping of the tissue; this assists in avoiding a postoperative “ghost breast” deformity. The incision is closed in layers including a pursestring suture to resize the NAC. In the periareolar technique, the mastectomy is completed through an incision on the NAC from 3 o’clock to 9 o’clock, and the NAC is not resized. Usually, this approach is only suitable for a Fischer grade 1.
Bolsters and drains are generally kept for 5 days postoperatively and compression is continued for 3–6 weeks. The most common complications include hematoma (5–12% with up to 5–10% requiring acute reoperation), seroma (2–5%) and nipple necrosis (2–5%). Hematoma rates are higher in minimal scar approaches. Pigmentation changes in grafted NACs can occur. Revision rates vary depending on study (10–40%) but generally DIFNG technique is less likely to require revisions. Common secondary surgeries include scar revision, dog-ear excision, and liposuction to address contour irregularities or residual tissue excess. Patient satisfaction is very high after these procedures. Surgical outcomes are shown in Fig. 39.3B . Surgeons and patients need to be aware that chest GAS is not an oncologic resection, and the mastectomy specimens should be screened for detection of occult cancer by a pathologist. No evidence-based guidelines for chest cancer screening post-gender mastectomy are available, but self-examination plus a yearly clinical breast examination is the most common recommendation.
Techniques for breast augmentation are not significantly different than those in cisgender women, but there are important considerations in a chest that has been exposed to testosterone in adolescence and exogenous estrogen later in life. Limited skin expansion, proportionally shorter nipple-to-IMF distance, wider sternum, lateralized NAC position and more developed pectoralis muscle all factor into preoperative decision-making and choice of implant.
Except for rare circumstances patients should be on well-controlled exogenous hormone therapy for at least 12 months to allow for maximal breast development prior to surgery. Perioperative hormone management should be decided based on the surgeon’s assessment of data. Previous silicone injections can impact candidacy and outcomes. Assessment of risk factors for breast pathology and a thorough discussion of the risks of implants, including breast implant-associated anaplastic large cell lymphoma, breast-implant-associated squamous cell carcinoma, and breast implant associated illness, is mandatory.
In evaluating the breasts, the thickness of the superior pole should be assessed via a pinch test. If the thickness is >1.5 cm, a subglandular approach can be considered. Pectoralis hypertrophy can blunt breast definition and cause animation deformity if a subpectoral approach is used. Due to often wider breast base width many require wider implants leading to larger volumes, especially if a moderate profile implant is desired. Once sizing is complete and the base width of the planned implant is known, then the anticipated extent of IMF lowering can be calculated. When lowering the IMF, some suggest the nipple-to-IMF distance should be equal to half of base width of implant. Ideally the implant is centered around the NAC. In patients with a wide chest and associated base width this may limit medial cleavage. If this is important to the patient a more medial placement can be offered but will lead to lateral displacement of the NAC relative to the implant. If amenable, a larger implant with a lower profile can be chosen to both give lateral and medial fullness while retaining the NAC in a more central location. Radial scoring of the breast parenchyma or a submuscular placement with judicious release of the medial pectoral fibers can allow for accommodation of a larger implant. If the IMF is lowered, Scarpa’s fascia should be secured to the underlying chest wall to prevent implant malposition. Techniques in breast augmentation are illustrated in Algorithm 39.2 . For patients desiring to avoid alloplastic implants, autologous breast construction, especially with fat-grafting, can be considered.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here