Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hand dominance
Location: medial, lateral, anterior, or posterior
Type of pain: radiating, numbness/tingling, stiffness, mechanical symptoms (locking/catching)
Duration of symptoms
Mechanism of injury
Pain modifiers
Activity related: gripping, lifting, pushing, throwing, punching
History of previous injuries
Recent changes in technique or training regimen
Treatments rendered and response
Inspection
Compare with uninjured side
Skin changes
Swelling
Ecchymosis
Muscle atrophy/hypertrophy
Carrying angle (cubitus valgus/varus)
Normal 10–20 degrees valgus, often greater in females
Neurovascular examination
Sensation
Median, ulnar, radial, medial, and lateral antebrachial cutaneous (LABC) nerves
Two-point discrimination at fingertips (≤5 mm is normal)
Motor
Median, ulnar, and radial nerves
Ulnar nerve subluxation, irritability
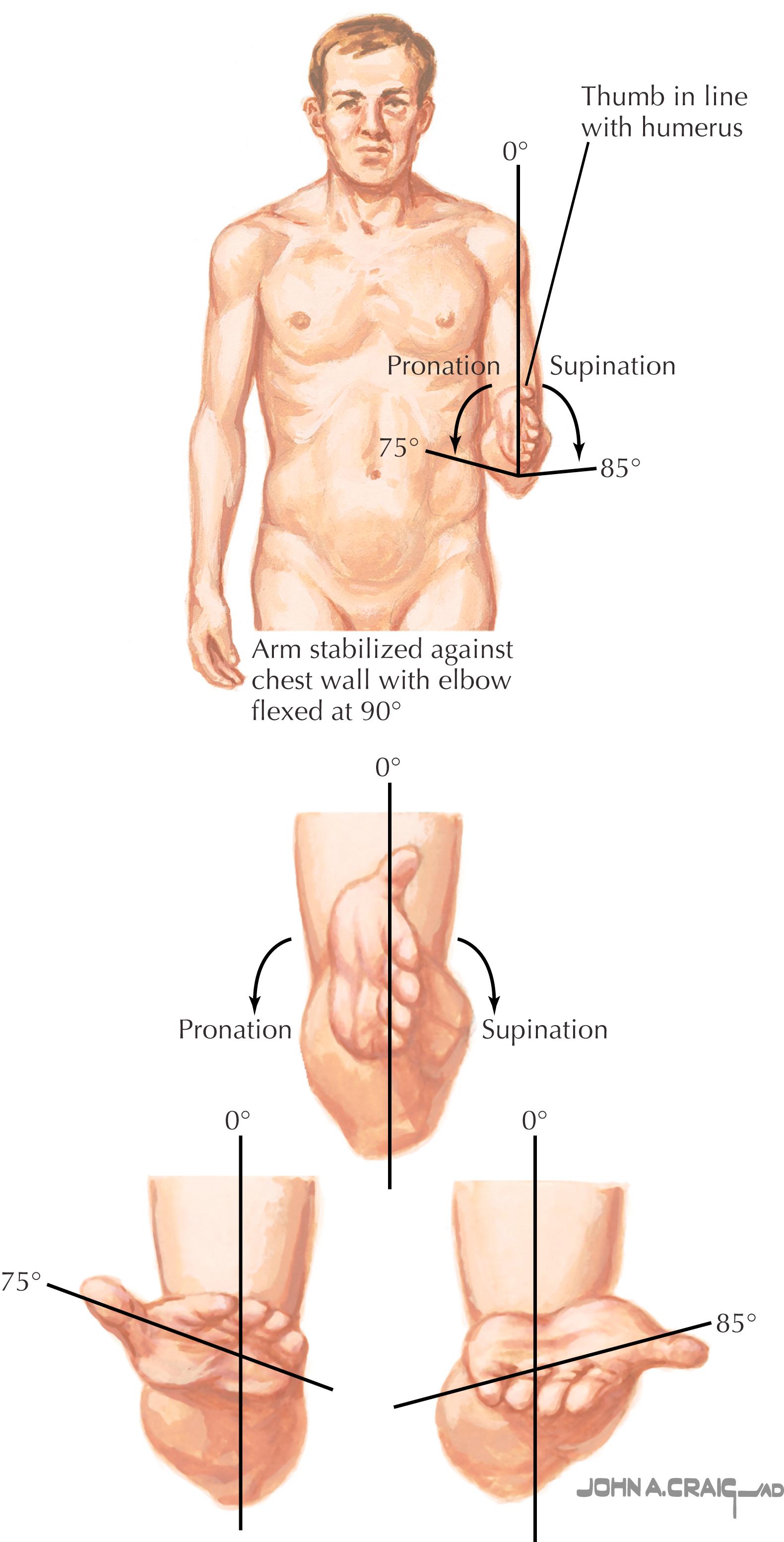
Range of motion (ROM) ( Fig. 50.1 )
Elbow flexion/extension
Forearm pronation/supination
Palpation:
Tenderness of key anatomic structures
Manual strength testing
Stability
Valgus–varus laxity
Posterolateral rotary laxity
Ulnar collateral ligament laxity
Provocative maneuvers
Radiographs: Anteroposterior (AP) and lateral
Special views:
Forty-five-degree flexion (capitellum)
Oblique (radial head)
Axial projections (olecranon fossa or gun-sight, Jones)
Gravity/manual stress
Computed tomography (CT) scan: Articular congruity, loose bodies, fracture dislocation, osteophytes/exostosis, tendon calcification, heterotopic ossification
Magnetic resonance imaging (MRI) ± magnetic resonance arthrogram (MRA): Soft tissue mass, ligament attenuation/rupture, chondral defect, loose bodies
Arthroscopy (diagnostic): Loose bodies, chondral lesions, synovitis
Electromyogram (EMG)/nerve conduction study (NCS): Nerve compression
Ultrasound: Dynamic evaluation for ligament laxity or ulnar nerve instability
Description: Traumatic avulsion of the distal bicep tendon from the bicipital tuberosity of the proximal radius
Mechanism of injury: Eccentric muscle contraction against an extension load on a flexed elbow
Presentation: Less than 10% of biceps ruptures occur at the elbow. Most often occur in males (90%), dominant extremity (80%), in ages 30–50. Risk factors: smoking, anabolic steroids, and mechanical attrition. Often an acute pop or tearing sensation in the proximal forearm or antecubital fossa with an eccentric contraction, with subsequent pain and weakness. Tears may be complete or partial (radial sided).
Physical examination: Tenderness to palpation in the antecubital fossa, acute swelling, and ecchymosis are common. Palpable tendon defect in complete tears indicates tendon retraction (“Popeye sign”), though may not occur because of adhesion to the lacertus fibrosus. Pain and weakness with supination (40%–50% loss) and flexion.
Hook test: Flex the elbow to 90 degrees in full supination, and insert a finger from the lateral side into the antecubital fossa to palpate for a cordlike structure
Biceps squeeze test: Rest the elbow on patient’s lap in slight pronation and midflexion, firmly squeeze the biceps muscle belly and observe for supination
Differential diagnosis: Biceps tendonitis, bicipital-radial bursitis, LABC nerve entrapment
Diagnostics: Primarily a clinical diagnosis
Radiographs: Rule out associated elbow injuries and evaluate for irregularities around the radial tuberosity
Ultrasound: Demonstrates extent of injury; cost-effective but user dependent
MRI: Should be performed with the patient prone, shoulder abducted overhead, elbow flexed to 90 degrees, and forearm fully supinated; identify complete vs. partial tear and amount of retraction
Treatment:
Nonsurgical: Activity modification, rest for low-grade partial tears
Surgical: Complete or high-grade partial tears; acute repair superior to nonsurgical treatment; grafting may be required in chronic cases; one- and two-incision repair techniques described; concern for heterotopic bone formation/radioulnar synostosis with the two-incision technique; most common complication with either approach is LABC nerve palsy (15%–40%), higher with the one-incision technique (most resolve within 6 months)
Prognosis and return to sport: A season-ending injury; patients surgically treated early can be expected to have near-full return of power and function; return to sport 4–6 months; re-rupture rate of 5%.
Description: Compression of the median nerve at the elbow with resultant nerve irritation ( Fig. 50.2 )
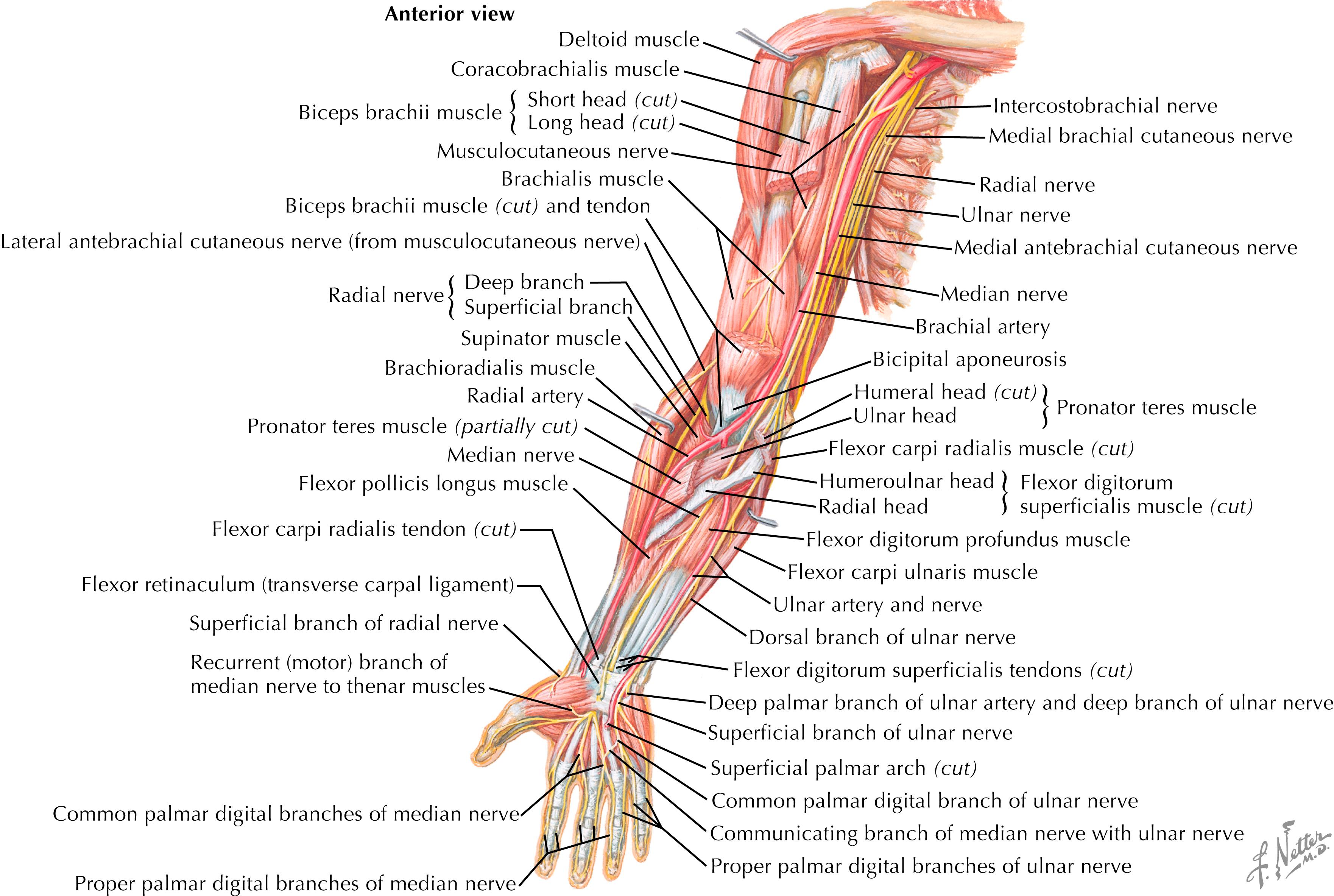
Mechanism of injury: No specific mechanism of injury has been associated; four possible sites of compression have been identified: beneath the ligament of Struthers in patients with a supracondylar process; an accessory head of the flexor pollicis longus (Gantzer muscle); lacertus fibrosus; tendinous arch of the flexor digitorum superficialis (FDS) (“sublimis bridge”)
Presentation: Similar to carpal tunnel syndrome with paresthesias in the volar radial three and a half digits and volar forearm/wrist pain; distinguished from carpal tunnel syndrome by decreased sensation over the thenar eminence in the distribution of the palmar cutaneous branch of the median nerve. Symptom severity may increase with activity such as weightlifting, competitive driving, and underarm pitching. Nighttime symptoms are less common than those in carpal tunnel syndrome.
Physical examination: Symptoms recreated with resisted pronation/supination or resisted middle finger proximal interphalangeal (PIP) flexion, caused by compression of FDS heads; may have a positive Tinel sign over volar forearm
Pronator compression test: Apply pressure for 30 seconds to the proximal edge of pronator muscle belly, which reproduces pain and paresthesias
Differential diagnosis: Carpal tunnel syndrome, cervical spine or brachial plexus nerve compression, flexor–pronator tendonitis, biceps tendonitis
Diagnostics:
Radiographs: Often normal but can reveal a supracondylar process (5 cm proximal to the medial epicondyle; 1% of population)
EMG/NCS: Help rule out other sites of compression; however, are often nondiagnostic
Treatment:
Nonsurgical: Activity modification, forearm flexor stretching, and nonsteroidal anti-inflammatory drugs (NSAIDs)
Surgical: Complete decompression of the median nerve throughout its course in the proximal forearm after failed conservative treatment: release of the ligament of Struthers, lacertus fibrosus, deep head of the pronator teres, and the FDS arch
Prognosis and return to sport: Early active range of motion (ROM), full return to activity by 6–8 weeks, and return to sport dependent upon restoration of strength and ROM.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here