Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Atrioventricular (AV) nodal reentrant tachycardia (AVNRT) was originally proposed to result from reentry confined within the compact AV node. Now, however, AVNRT is thought to involve the AV node, at least two atrionodal connections, and a component of the atrial and/or coronary sinus (CS) myocardium. Much of our current understanding about the components of the reentrant circuits has evolved from the development of ablation procedures in which one of the atrionodal connections, remote from the compact AV node, is destroyed, eliminating AVNRT without producing AV block.
The multiple forms of AVNRT use two of the atrionodal connections (AV nodal pathways) for the anterograde and retrograde limbs of the reentrant circuit. Traditionally, variants of AVNRT have been distinguished based on the site of earliest retrograde atrial activation ( Fig. 72.1 ) and the relative duration of the A-H and H-A intervals into three patterns: Slow/Fast, Fast/Slow, and Slow/Slow AVNRT. Slow/Fast AVNRT was identified by earliest retrograde atrial activation recorded at the interatrial septum behind the tendon of Todaro (ToT), with long A-H and short H-A intervals. Slow/Slow and Fast/Slow AVNRT were distinguished from Slow/Fast AVNRT by recognizing earliest retrograde activation at the inferior triangle of Koch (ToK) or CS. Slow/Slow and Fast/Slow AVNRT were then differentiated by the relative duration of the A-H and H-A intervals. In our experience of 734 patients referred for catheter ablation of AVNRT, by this definition 515 patients (77%) had Slow/Fast AVNRT, 80 patients (11%) had Slow/Slow AVNRT, and 89 patients (12%) had Fast/Slow AVNRT.
Because more is now known about the anatomic substrate for the various forms of AVNRT, the different forms of AVNRT can be distinguished anatomically by the atrionodal connections that form the anterograde and retrograde pathways used in the tachycardia and labeled with the name of the atrionodal connection used for the anterograde pathway/retrograde pathway. (For a more complete bibliography of the development of the understanding of this topic, see Lockwood et al. )
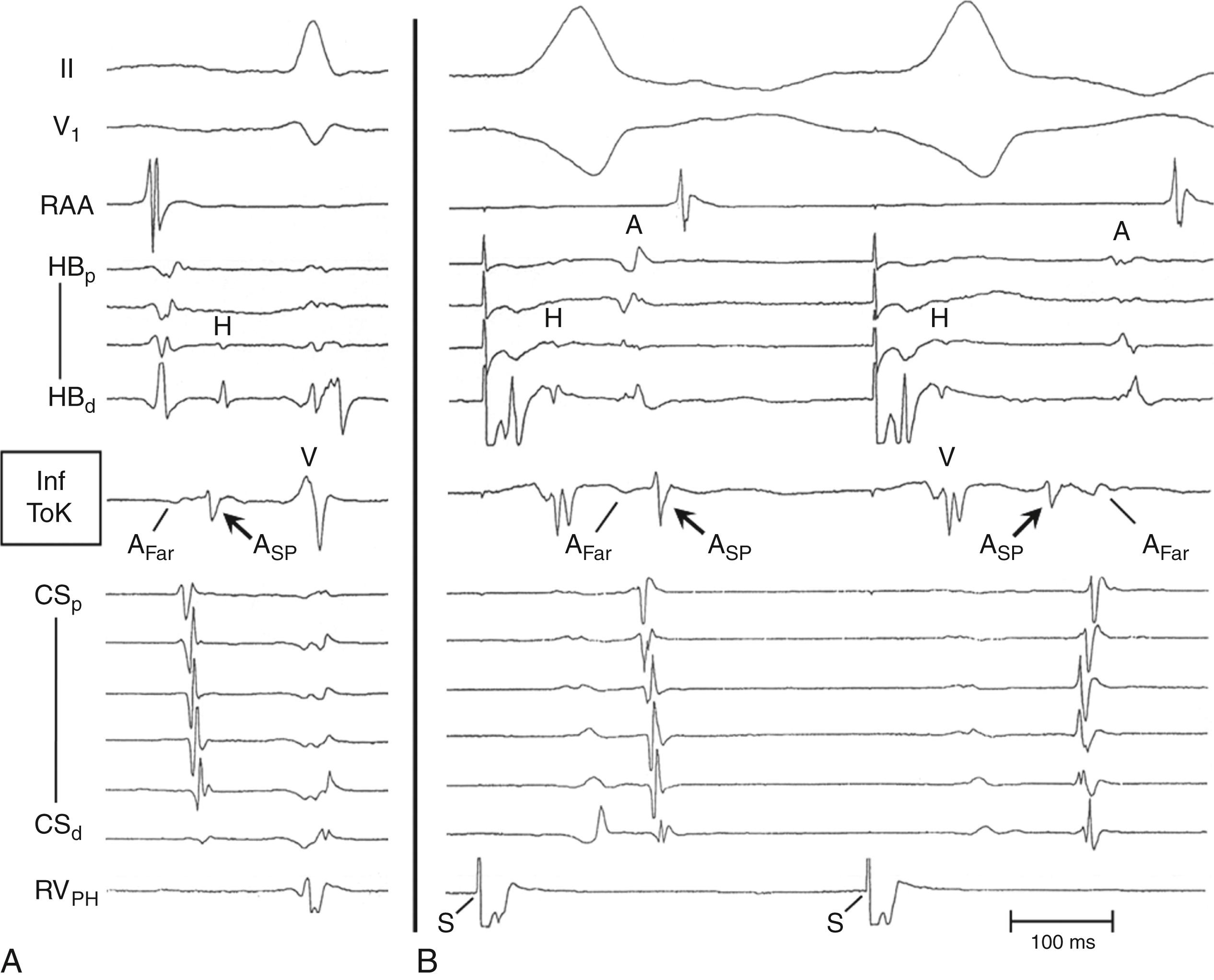
Evidence that the fast pathway (FP) and slow pathways (SPs) involved in the reentrant circuits of AVNRT represent conduction over different atrionodal connections, rather than functional longitudinal dissociation within the compact AV node, includes the following: (1) different sites of earliest atrial activation during retrograde conduction over the FP and each of the SPs, as originally described by Sung et al. ( Fig. 72.2 ); (2) the ability of a late extrastimulus delivered to the atrium outside the compact AV node to advance the timing in an anterograde SP (advancing or sometimes delaying the next His bundle potential) and reset the various forms of AVNRT ; and (3) the selective elimination of FP or SP conduction by catheter or surgical ablation in the atrium, remote from the compact AV node. The atrial connections of the FP and SPs can be identified by locating the site of earliest atrial activation during selective retrograde conduction over each pathway. These sites are located away from the compact AV node (see Fig. 72.1 ).
During retrograde FP conduction, right atrial (RA) mapping using closely spaced electrodes (1 mm edge to edge) records earliest RA activation posterior to the ToT at a level approximately 10 to 15 mm inferior to the level recording the proximal His bundle potential ( Fig. 72.3 ; see also Fig. 72.1 ). The position posterior to the ToT is confirmed radiographically by leftward deviation of the mapping catheter in the left anterior oblique (LAO) projection (RA septum in Fig. 72.3B ), indicating that the mapping catheter was not constrained by the tricuspid annulus (TA) and ToT. If the mapping catheter had been positioned across the ToT, the catheter would have been oriented parallel to the His bundle catheter.
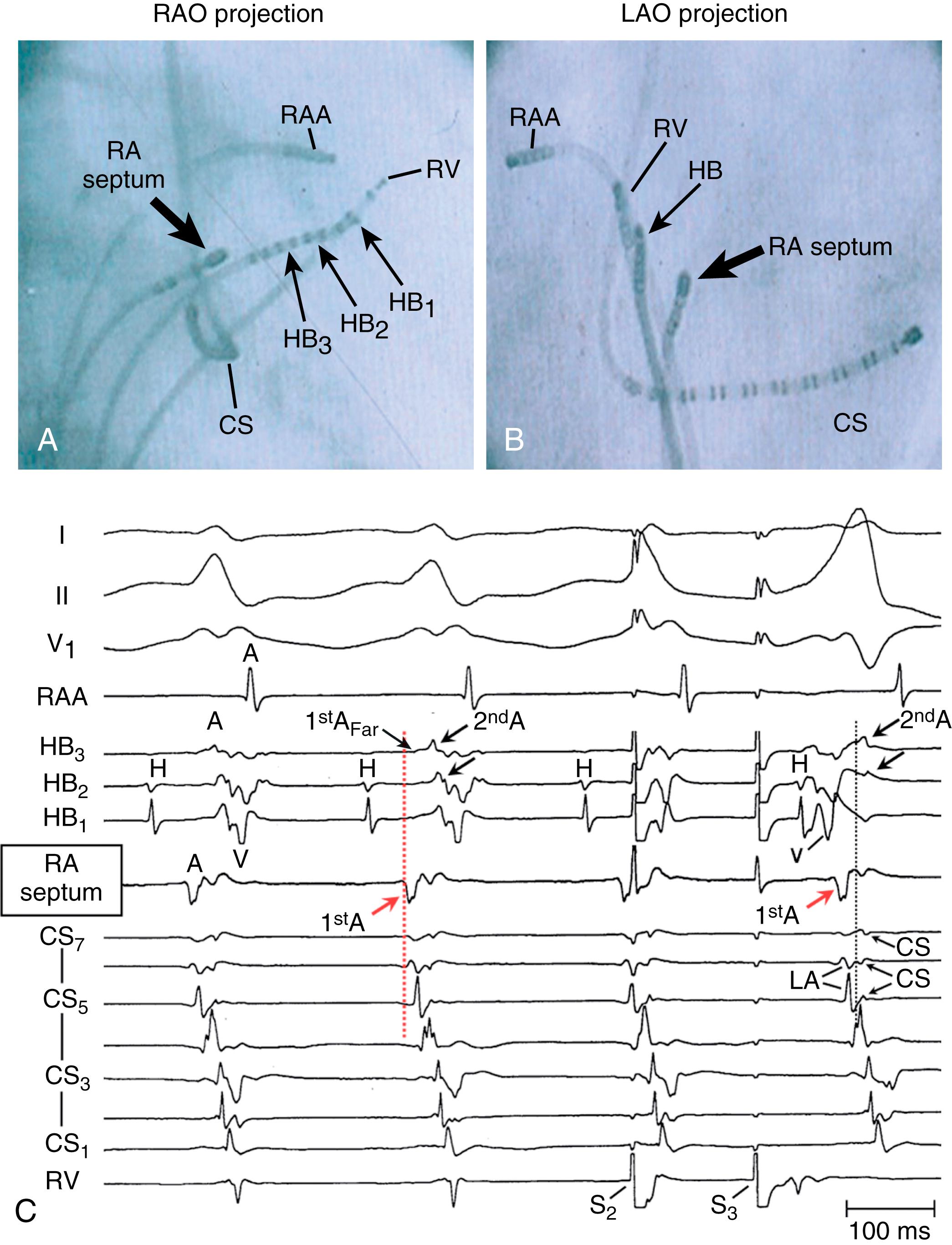
During retrograde FP conduction (ventricular pacing or Slow/Fast AVNRT), RA activation, beginning posterior to the ToT (outside the ToK), propagates away in the posterior, superior, and inferior directions (green arrows 2 in Fig. 72.4A ). Activation propagating inferiorly along the posterior aspect of the eustachian ridge (ER) produces an early far-field atrial potential recorded from the inferior aspect of the ToK (A Far in Fig. 72.5C ). Atrial activation within the ToK (adjacent to the TA) occurs relatively late and proceeds in an inferior-to-superior direction, beginning just outside the CS ostium (blue arrows 6 in Fig. 72.4A and ASP [slow pathways] potential in Fig. 72.5C ), producing a second late atrial potential near the apex of the ToK, occurring 50 to 115 ms after the earliest atrial activation (see second A in Figs. 72.3C and 72.6 ). The two wavefronts, propagating in opposite directions on either side of the ToT (green arrow and blue arrow 6 in Fig. 72.4A ), suggest conduction block across the ToT and ER. The timing of the second atrial potential (see Fig. 72.6 ) near the apex of the ToK is later than the timing of atrial activation in the inferior ToK (A SP potential recorded between the CS ostium and the TA), which is later than the timing of activation within the proximal CS (see Fig. 72.3C and 72.5 ). This suggests that the tissue within the ToK is activated by the CS myocardium (brown arrows in Fig. 72.4A ).
![Fig. 72.4, (A) Proposed pattern of atrial activation during retrograde conduction over the fast pathway (FP). Retrograde FP conduction ( dotted red arrows 1 ) activates the right and left atrium at the interatrial septum, posterior to the tendon of Todaro (ToT) outside the triangle of Koch (ToK). Right atrial activation propagates away in the posterior, superior, and inferior directions (RA activation , green arrows 2 ). This results in superior-to-inferior right atrial activation along the eustachian ridge (ER) outside the ToK. This right atrial wavefront is unable to cross the ER and ToT to enter the ToK, presumably because of conduction block at the ER ( short perpendicular green line ). Left atrial activation propagates inferiorly ( green arrows 3 in left anterior oblique [LAO] projection) and activates the coronary sinus (CS) myocardium, 1 to 3 cm from the ostium ( brown arrows ). The reentrant impulse propagates along the CS myocardium to the CS ostium ( brown arrows 4 ) where it activates the inferior ToK ( brown arrow 5 ), producing the A SP potential, with activation proceeding in the inferior-to-superior direction along the inferior ToK ( blue arrows 6 ). (B) Postulated pattern of activation during retrograde conduction over the rightward inferior extension (RIE) of the atrioventricular (AV) node. Retrograde conduction over the RIE ( blue arrows ) activates the myocardium between the inferoseptal tricuspid annulus (TA) and the CS ostium (inferior ToK) to produce the retrograde A SP potential ( blue arrow 2 ) and then activates the CS at the floor of the ostium ( brown arrows 3 ). Activation in the ToK does not cross the ER to the right atrium ( perpendicular green line ) but proceeds leftward along the CS myocardium ( brown arrows in LAO projection) to activate the left atrium. Left atrial activation propagates rapidly in the leftward direction ( solid green arrow 4 in LAO projection) but must reverse direction to propagate in the septal direction ( dotted green line 5 ). The reversal of direction produces late left atrial activation at the left atrial inferoseptal region and a second potential in proximal CS electrograms (recorded from the CS roof). This septal left atrial wavefront activates the interatrial septum ( dotted green line 6 ), which is followed by activation of the right atrium posterior to the ToT and ER ( green arrows 7 ), which produces a late far-field potential recorded from the inferior ToK. (C) Postulated pattern of activation during retrograde conduction over the leftward inferior extension (LIE) of the AV node. It is unknown whether retrograde conduction over the LIE ( purple arrows ) initially activates the left atrial myocardium close to the inferoseptal mitral annulus (MA ; top purple arrowhead in LAO projection) or the CS myocardium at the roof of the proximal CS ( lower purple arrowhead in LAO projection). During retrograde conduction over the LIE, CS activation ( brown arrows ) is recorded earliest at the CS roof, 1.5 to 4 cm from the ostium. (D) Postulated pattern of activation during retrograde conduction over the inferolateral left atrial SP (IL-LA) and the anterior superior SP (AS). Retrograde conduction over the IL-LA SP ( orange arrows ) activates the left atrium close to the inferolateral MA at the 4:30 to 5:00 o’clock position, as viewed in the LAO projection ( green arrows ). Right atrial mapping during retrograde conduction over the AS ( pink arrows ) records earliest activation at the anterior-superior aspect of the septum or medial right atrial free-wall. FO, Fossa ovalis; IVC, inferior vena cava. Fig. 72.4, (A) Proposed pattern of atrial activation during retrograde conduction over the fast pathway (FP). Retrograde FP conduction ( dotted red arrows 1 ) activates the right and left atrium at the interatrial septum, posterior to the tendon of Todaro (ToT) outside the triangle of Koch (ToK). Right atrial activation propagates away in the posterior, superior, and inferior directions (RA activation , green arrows 2 ). This results in superior-to-inferior right atrial activation along the eustachian ridge (ER) outside the ToK. This right atrial wavefront is unable to cross the ER and ToT to enter the ToK, presumably because of conduction block at the ER ( short perpendicular green line ). Left atrial activation propagates inferiorly ( green arrows 3 in left anterior oblique [LAO] projection) and activates the coronary sinus (CS) myocardium, 1 to 3 cm from the ostium ( brown arrows ). The reentrant impulse propagates along the CS myocardium to the CS ostium ( brown arrows 4 ) where it activates the inferior ToK ( brown arrow 5 ), producing the A SP potential, with activation proceeding in the inferior-to-superior direction along the inferior ToK ( blue arrows 6 ). (B) Postulated pattern of activation during retrograde conduction over the rightward inferior extension (RIE) of the atrioventricular (AV) node. Retrograde conduction over the RIE ( blue arrows ) activates the myocardium between the inferoseptal tricuspid annulus (TA) and the CS ostium (inferior ToK) to produce the retrograde A SP potential ( blue arrow 2 ) and then activates the CS at the floor of the ostium ( brown arrows 3 ). Activation in the ToK does not cross the ER to the right atrium ( perpendicular green line ) but proceeds leftward along the CS myocardium ( brown arrows in LAO projection) to activate the left atrium. Left atrial activation propagates rapidly in the leftward direction ( solid green arrow 4 in LAO projection) but must reverse direction to propagate in the septal direction ( dotted green line 5 ). The reversal of direction produces late left atrial activation at the left atrial inferoseptal region and a second potential in proximal CS electrograms (recorded from the CS roof). This septal left atrial wavefront activates the interatrial septum ( dotted green line 6 ), which is followed by activation of the right atrium posterior to the ToT and ER ( green arrows 7 ), which produces a late far-field potential recorded from the inferior ToK. (C) Postulated pattern of activation during retrograde conduction over the leftward inferior extension (LIE) of the AV node. It is unknown whether retrograde conduction over the LIE ( purple arrows ) initially activates the left atrial myocardium close to the inferoseptal mitral annulus (MA ; top purple arrowhead in LAO projection) or the CS myocardium at the roof of the proximal CS ( lower purple arrowhead in LAO projection). During retrograde conduction over the LIE, CS activation ( brown arrows ) is recorded earliest at the CS roof, 1.5 to 4 cm from the ostium. (D) Postulated pattern of activation during retrograde conduction over the inferolateral left atrial SP (IL-LA) and the anterior superior SP (AS). Retrograde conduction over the IL-LA SP ( orange arrows ) activates the left atrium close to the inferolateral MA at the 4:30 to 5:00 o’clock position, as viewed in the LAO projection ( green arrows ). Right atrial mapping during retrograde conduction over the AS ( pink arrows ) records earliest activation at the anterior-superior aspect of the septum or medial right atrial free-wall. FO, Fossa ovalis; IVC, inferior vena cava.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/AtrioventricularNodalReentrantTachycardia/2_3s20B978032375745400072X.jpg)
If only the second of the two potentials is recorded on the His bundle electrogram during Slow/Fast AVNRT (see Figs. 72.3C and 72.6 ), this may lead to the erroneous impression that activation is earlier at the inferior ToK or in the CS (retrograde SP conduction) and may suggest the incorrect diagnosis of Slow/Slow AVNRT. This error can be avoided by mapping behind the ToT, along the TA, and in the CS to identify the true site of earliest activation during AVNRT (see the first A in Figs. 72.3 and 72.6B ).
Animal studies suggest that the FP may be formed by transitional cells (with action potentials having features intermediate between those of atrial cells and AV nodal cells), which begin on both sides of the atrial septum, cross the right and left sides of the ToT, and insert into the AV bundle distal to much of the compact AV node, relatively close to the His bundle. As a result, retrograde conduction over the FP results in almost simultaneous activation of both the left and right sides of the interatrial septum. , The left atrial (LA) wavefront propagates around the inferior mitral annulus in the counterclockwise direction, as viewed in the LAO projection (green arrows 3 in Fig. 72.4A ), activating the CS myocardium at the roof, approximately 1 cm from the CS ostium. CS activation propagates in both lateral and septal directions (brown arrows 4 in Fig. 72.4A ). The septally oriented CS wavefront activates the inferior ToK (brown arrows 5 in Fig. 72.4A ), resulting in activation in the superior direction in the ToK (blue arrow 6 and A SP potential in Fig. 72.4A ).
A study in isolated perfused canine hearts found that anterograde conduction block in the FP occurred posterior to the ToT. As the atrial pacing rate was increased, block occurred at progressively more proximal locations (i.e., closer to the anterior limbus of the fossa ovalis). Anterograde FP block may therefore occur outside the ToK, which may prevent retrograde invasion of the SP, allowing anterograde conduction over one of the SPs and thus facilitating initiation of Slow/Fast AVNRT and possibly other forms, such as Slow/Slow AVNRT.
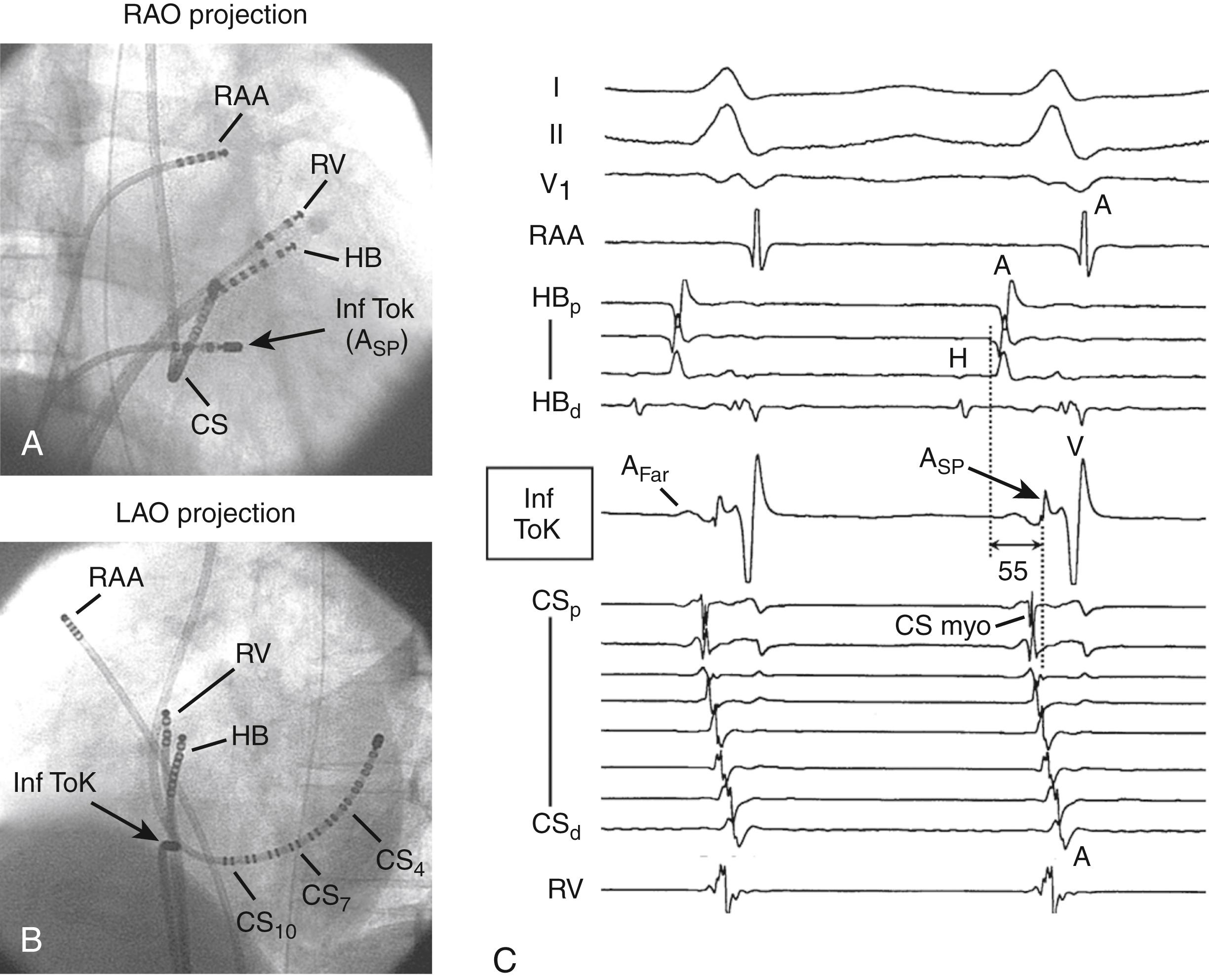
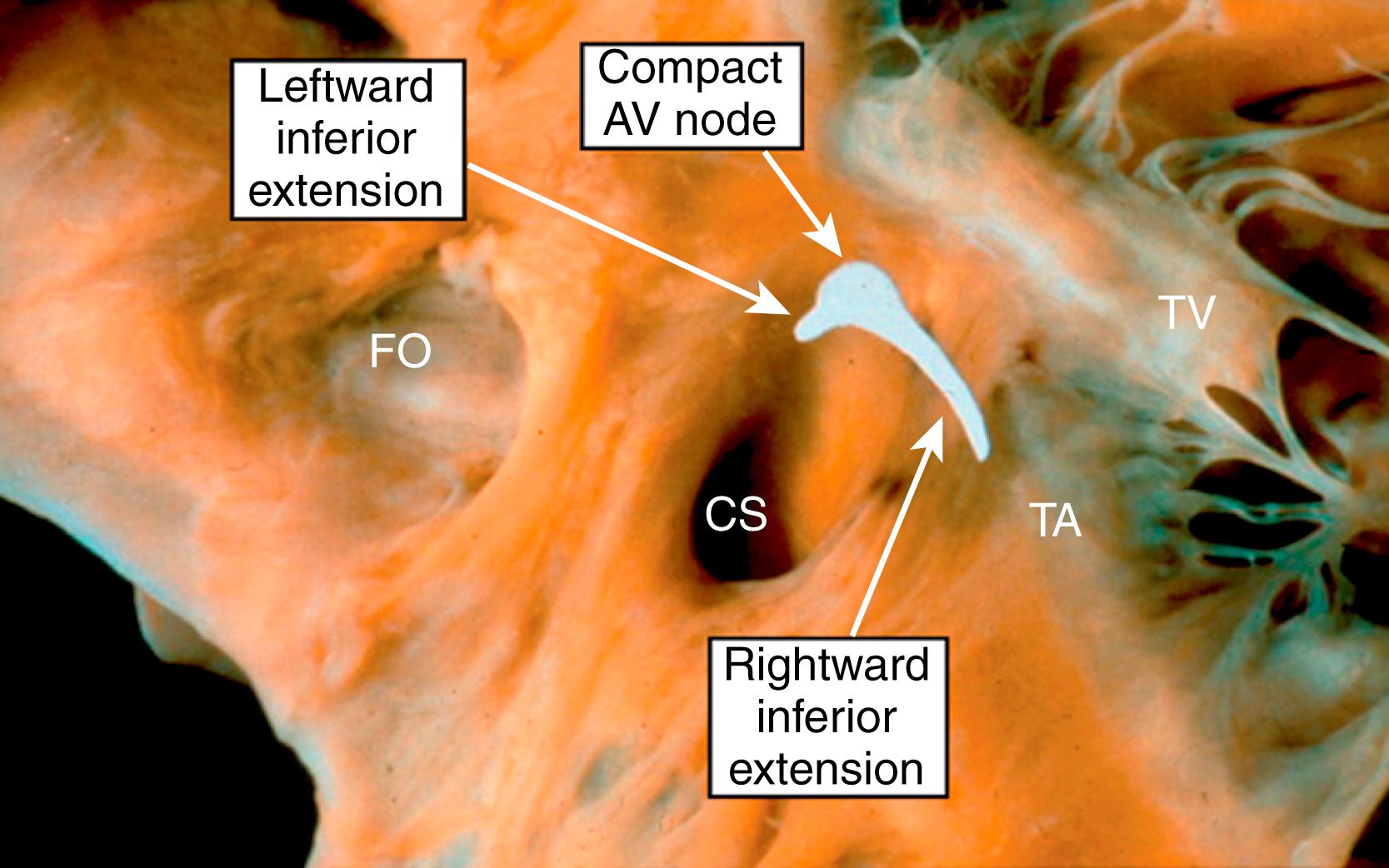
At least four atrionodal connections other than the FP participate in various forms of AVNRT; these atrionodal connections have generally been labeled as SPs. The SP most commonly used in either the anterograde or retrograde direction is formed by the rightward inferior extension (RIE) of the AV node ( Fig. 72.7 ). Detailed mapping during retrograde conduction over the RIE suggests that this structure extends over a long length (blue arrows in Fig. 72.4B ) and connects selectively to the floor of the CS ostium to connect with the LA via the CS myocardium (brown arrows 3 in Fig. 72.4B ). The ER forms a complete line of block to prevent the RA from being activated from the ToK (green line in RAO projection of Fig. 72.4B ). The earliest retrograde high-frequency potential (A SP potential) is recorded at the inferior ToK between the TA and the CS ostium (second complex in Figs. 72.2B and 72.8B , blue arrow 2 in Fig. 72.4B ). Activation is then recorded at the floor of the CS ostium (brown arrow 3 in Fig. 72.4B and CS myo arrow in CS floor p electrogram in Fig. 72.8B ). The CS myocardium propagates the impulse leftward and superiorly, activating the LA myocardium approximately 2 to 3 cm from the CS ostium. LA activation proceeds rapidly leftward (green arrow 4 in Fig. 72.4B ), while slowly reversing direction (because of transverse conduction across the atrial fibers) to propagate rightward toward the septum (dotted green line 5 in Fig. 72.4B ). Activation then propagates across the interatrial septum to activate the RA behind the ToT (green arrows 6 and 7 in Fig. 72.4B ). RA activation proceeds superiorly (behind the ToT) to create the late atrial potential in the His bundle electrogram and inferiorly (behind the ER and CS ostium) to create the late, far-field potential recorded at the inferior ToK (A Far in the second complex of Figs. 72.2B and 72.8B ). Late RA extrastimuli advance the atrial potential behind the ToT, without advancing the A SP potential, supporting the presence of conduction block across the ToT and ER.
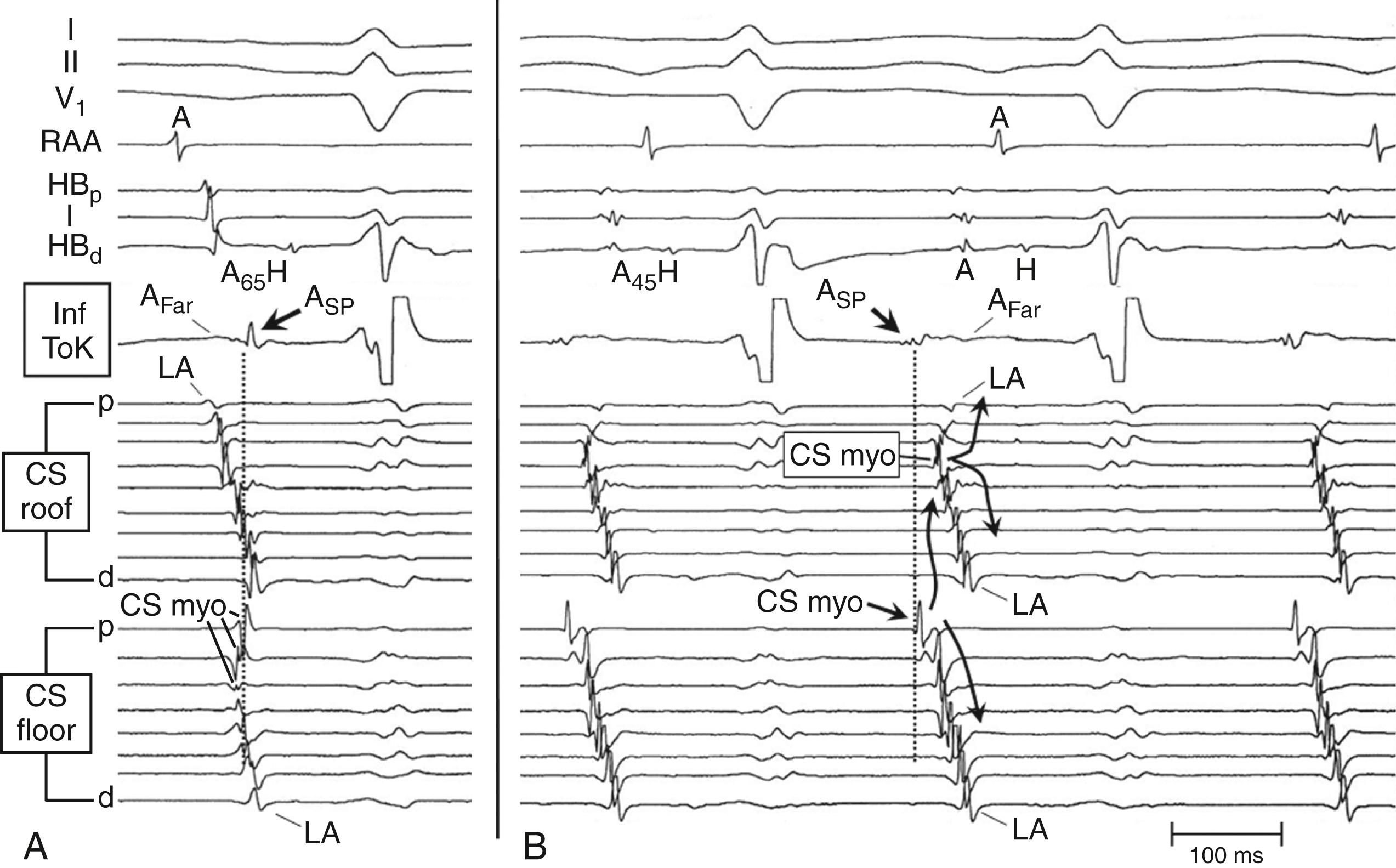
Conduction block across the ER may also account for the late timing of activation within the ToK during sinus rhythm (A SP potential in Figs. 72.2A and 72.8A ). The two most likely explanations for the late A SP potential during sinus rhythm are that the inferior ToK is activated by either (1) the CS musculature, which is activated from the LA ( Fig. 72.9A ) or (2) the crista terminalis (see Fig. 72.9B ). Observations that the CS myocardium propagates in a distal-to-proximal direction in the proximal 1 to 2 cm of the CS (CS myo in Fig. 72.8A ) and that the A SP potential is recorded after CS activation in the proximal CS (see Figs. 72.2A and 72.8A ) suggest that the inferior ToK is activated from the CS myocardium (see Fig. 72.9A ).
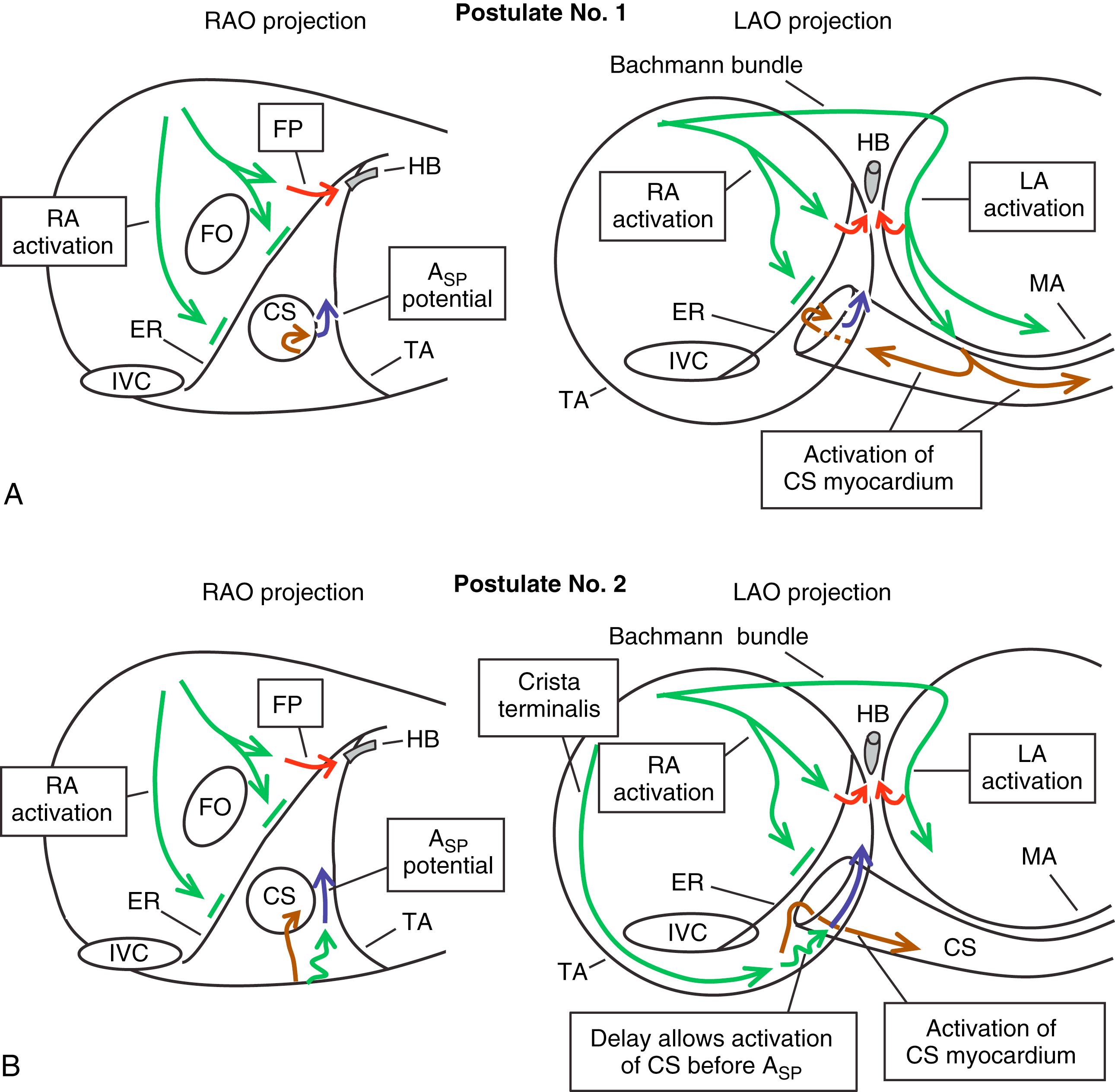
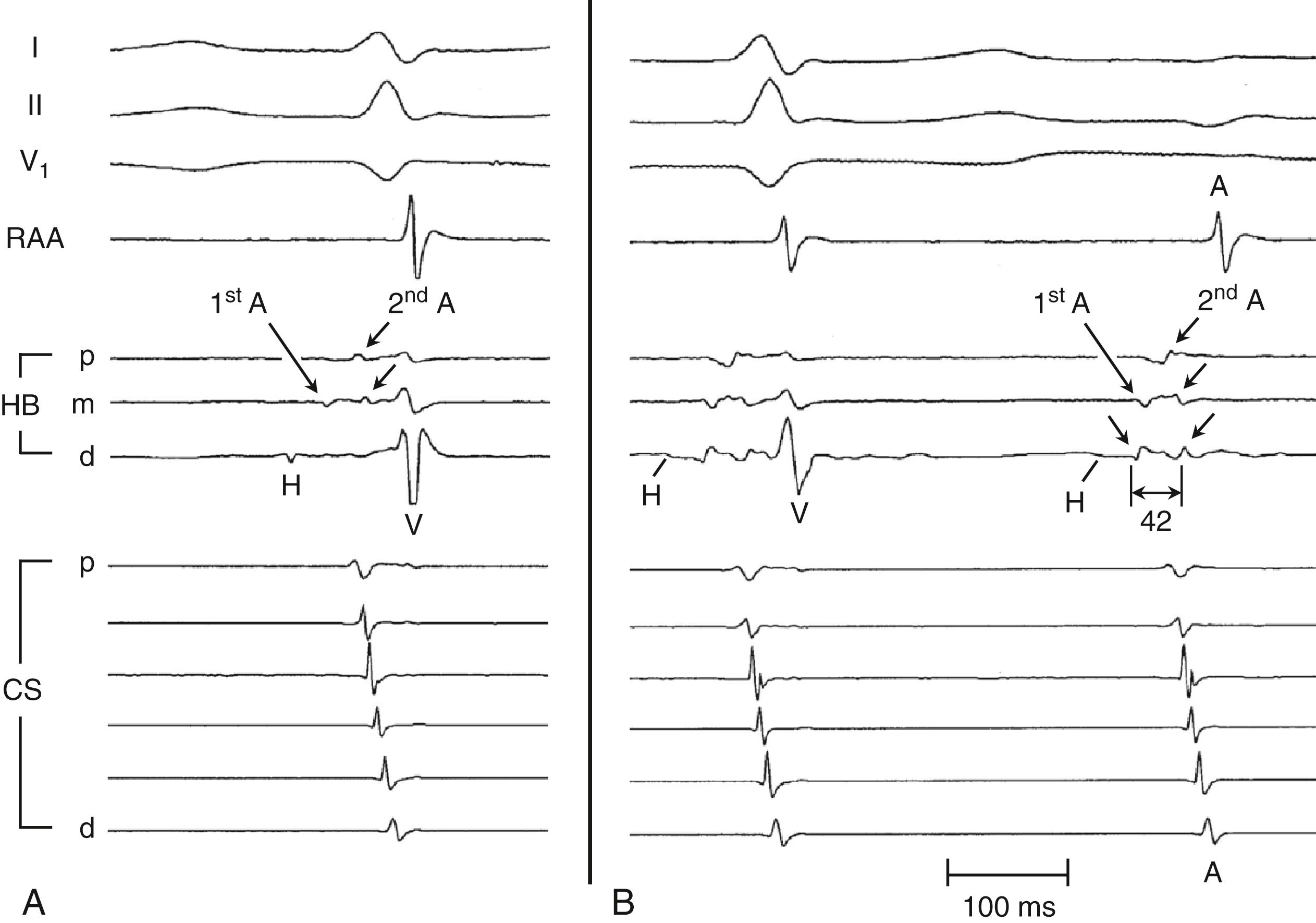
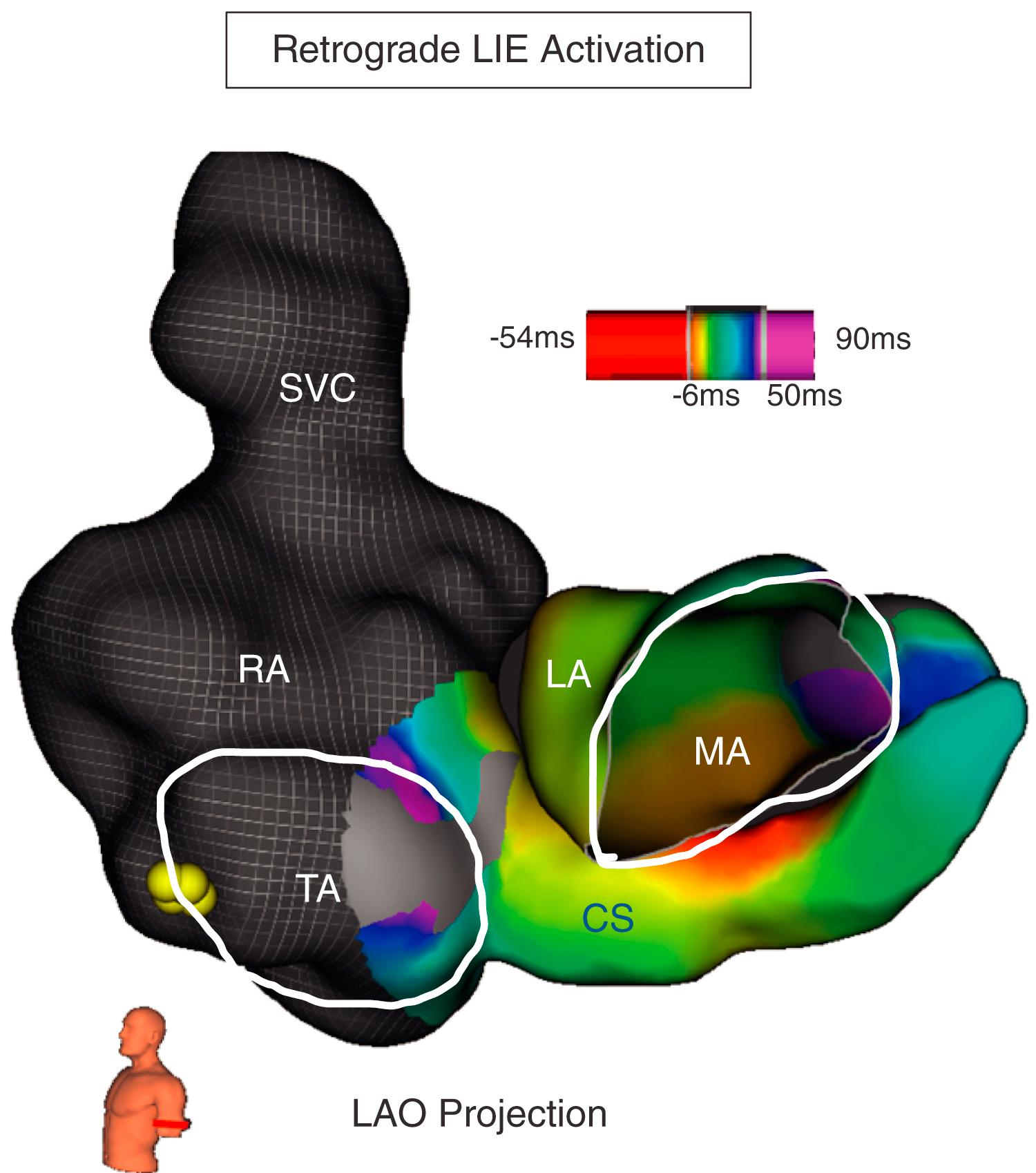
The leftward inferior extension (LIE) of the AV node is the second most commonly observed SP. During retrograde conduction over the LIE, earliest activation is recorded at the roof of the CS, 1 to 3 cm from the ostium ( Figs. 72.10, 72.11B ; see also Fig. 72.4C ) and the first beat (see Fig. 72.11B ). Activation is also early at the inferior paraseptal LA near the mitral annulus (see Fig. 72.10 ). The LIE can often be ablated from the roof of the CS but may require ablation from the inferior or inferior paraseptal LA.
![Fig. 72.11, Comparison of the H-A interval during tachycardia and during ventricular pacing for Slow/Fast atrioventricular nodal reentrant tachycardia (AVNRT) and Slow/Slow (rightward inferior extension [RIE]/leftward inferior extension [LIE]) AVNRT. Fig. 72.11, Comparison of the H-A interval during tachycardia and during ventricular pacing for Slow/Fast atrioventricular nodal reentrant tachycardia (AVNRT) and Slow/Slow (rightward inferior extension [RIE]/leftward inferior extension [LIE]) AVNRT.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/AtrioventricularNodalReentrantTachycardia/9_3s20B978032375745400072X.jpg)
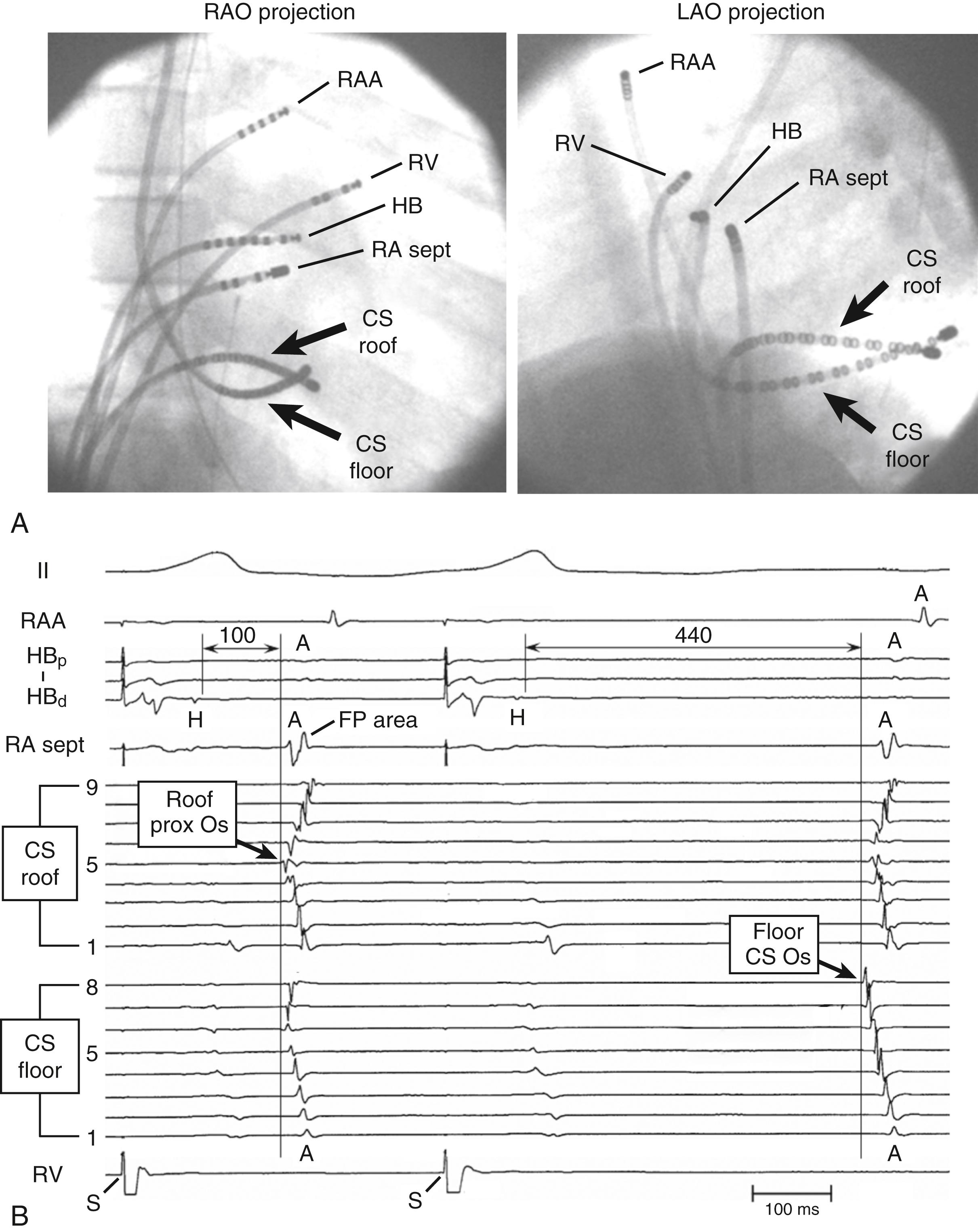
Evidence of conduction over more than one SP includes the observation of multiple, abrupt increases of 50 ms or more (“jumps”) in the A 2 to H 2 interval in some patients during atrial extrastimulus testing. Additionally, during programmed ventricular stimulation, two distinct retrograde atrial activation sequences with different H-A intervals are sometimes seen, representing retrograde conduction over two separate SPs (RIE and LIE). The two retrograde SPs can best be distinguished by recording simultaneously from the roof and floor of the CS, generally using a closely spaced multielectrode catheter on the CS floor (internal jugular or subclavian venous access) and a mapping/ablation catheter along the CS roof or, for research or teaching, two multielectrode CS catheters, one via the internal jugular or subclavian venous access positioned along the floor of the CS and the other via femoral venous access positioned along the roof of the CS ( Fig. 72.12 ). Evidence of conduction over more than one SP is also often observed in the response to ablation. For example, in patients with Slow/Fast AVNRT using the RIE as the anterograde SP (RIE/FP Slow/Fast AVNRT), ablation along a line between the inferoseptal TA and the CS ostium often eliminates conduction over the RIE and eliminates the tachycardia. Nevertheless, atrial extrastimulus testing continues to show a jump in the A 2 -H 2 interval (often with a single Slow/Fast nodal reentrant atrial echo beat) in approximately 75% of patients, consistent with conduction over the LIE or another SP.
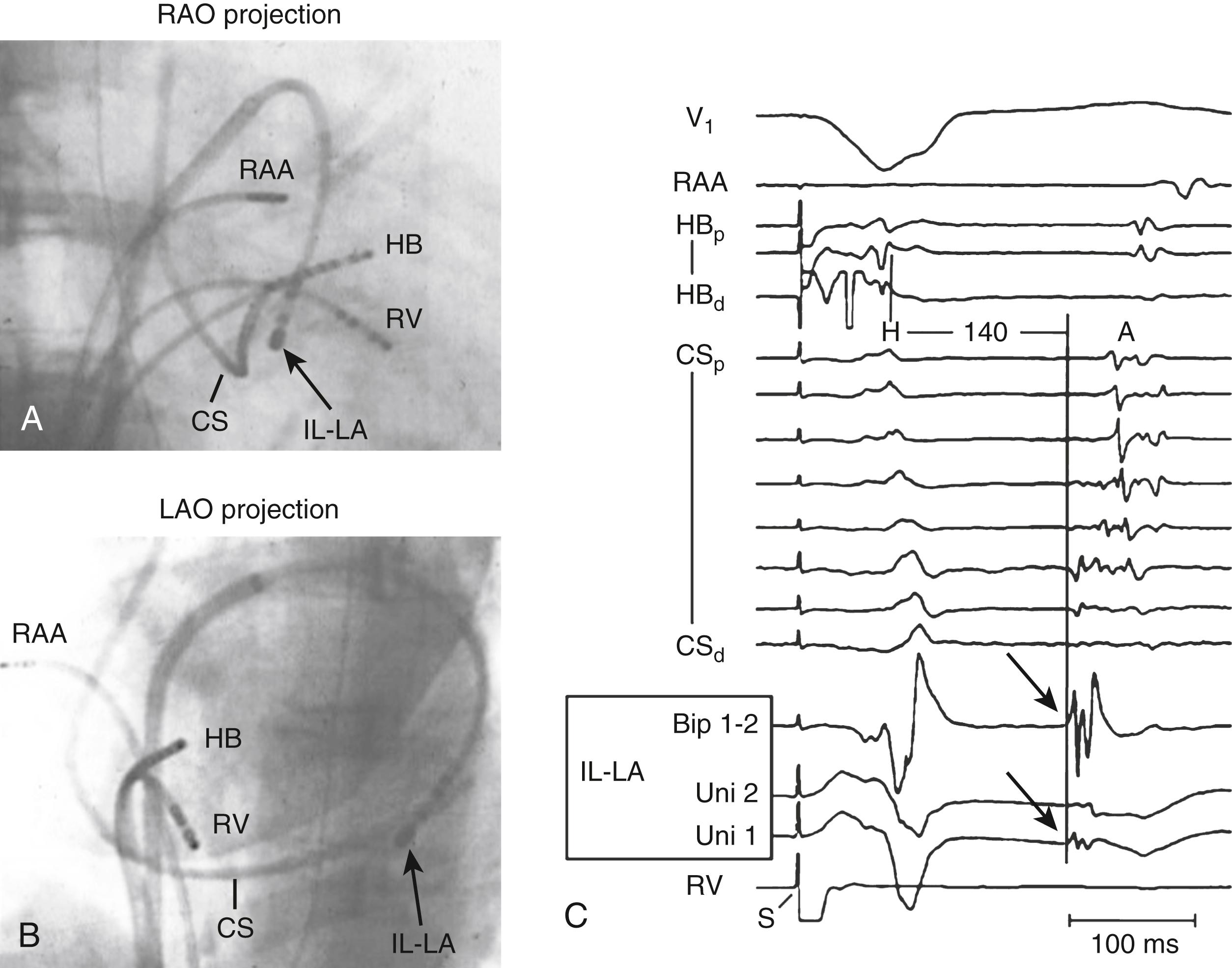
We are aware of the existence of at least two other SPs. Retrograde conduction over the inferolateral left atrial (IL-LA) SP is infrequently seen and, in our experience, only in patients who use this SP for retrograde conduction during Slow/Slow and Fast/Slow AVNRT. Earliest retrograde atrial activation over the IL-LA SP is located at the basal inferolateral LA at 4:30 to 5 o’clock position in the LAO projection ( Fig 72.13 ; see also Fig. 72.1 and green arrows in Fig. 72.4D ). More often, this SP is recognized when it forms the anterograde limb of Slow/Fast AVNRT (IL-LA/FP Slow/Fast AVNRT), being identified when the basal inferolateral LA is the site where the latest atrial extrastimulus is able to penetrate the anterograde SP and reset the tachycardia.
Retrograde conduction over the anterior-superior SP results in earliest atrial activation on the septum, posterior to the ToT, and 2 to 4 mm superior to the site recording the most proximal His bundle potential (see Fig. 72.1 and pink arrows in Fig. 72.4D ). This site is 1.5 to 2 cm superior to the site where earliest retrograde FP activation is recorded. There may be additional SPs that have not been described.
The atrionodal connections that form the FP and one or more of the SPs are typically present in normal hearts. In a series of 200 consecutive patients in our laboratory who underwent radiofrequency catheter ablation of an accessory pathway (without a history of AVNRT or inducible AVNRT during the procedure), evidence of dual-AV nodal pathway physiology in either the anterograde or retrograde direction was present in 168 (84%). The ability to demonstrate anterograde or retrograde SP conduction in a high percentage of patients was probably related to heavy sedation or general anesthesia, which depressed anterograde and retrograde FP conduction. Small doses of isoproterenol (0.25–0.5 μg/min) enhanced FP conduction to a greater extent than SP conduction and often obscured anterograde and retrograde SP conduction. These low doses of isoproterenol in heavily sedated or anesthetized patients probably mimic the usual sympathetic tone in nonsedated patients undergoing electrophysiologic studies, which explains the low incidence of dual-pathway physiology previously described in nonsedated patients without AVNRT. Other reasons may include a similar conduction time over the FP and an SP just before block in the FP (smooth transition). During ventricular stimulation, there is no specific value of H-A interval that identifies retrograde SP conduction. Nevertheless, the transition from retrograde FP conduction to retrograde SP conduction is easy to recognize because of the shift in retrograde atrial activation sequence (see Fig. 72.2B ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here