Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Describe the landmarks of the thoracic cavity
Define the relational landmarks of the heart
Discuss the function of the pericardial sac
Differentiate the three layers of the heart wall
Describe the anatomic landmarks of the cardiac chambers, valves, and interventricular septum
The cardiovascular system delivers oxygenated blood to tissues in the body and removes waste products from these tissues. The heart pumps blood to all the organs and tissues of the body. The autonomic nervous system controls how the heart pumps, and the vascular network (arteries and veins) carries blood throughout the body, keeps the heart filled with blood, and maintains blood pressure.
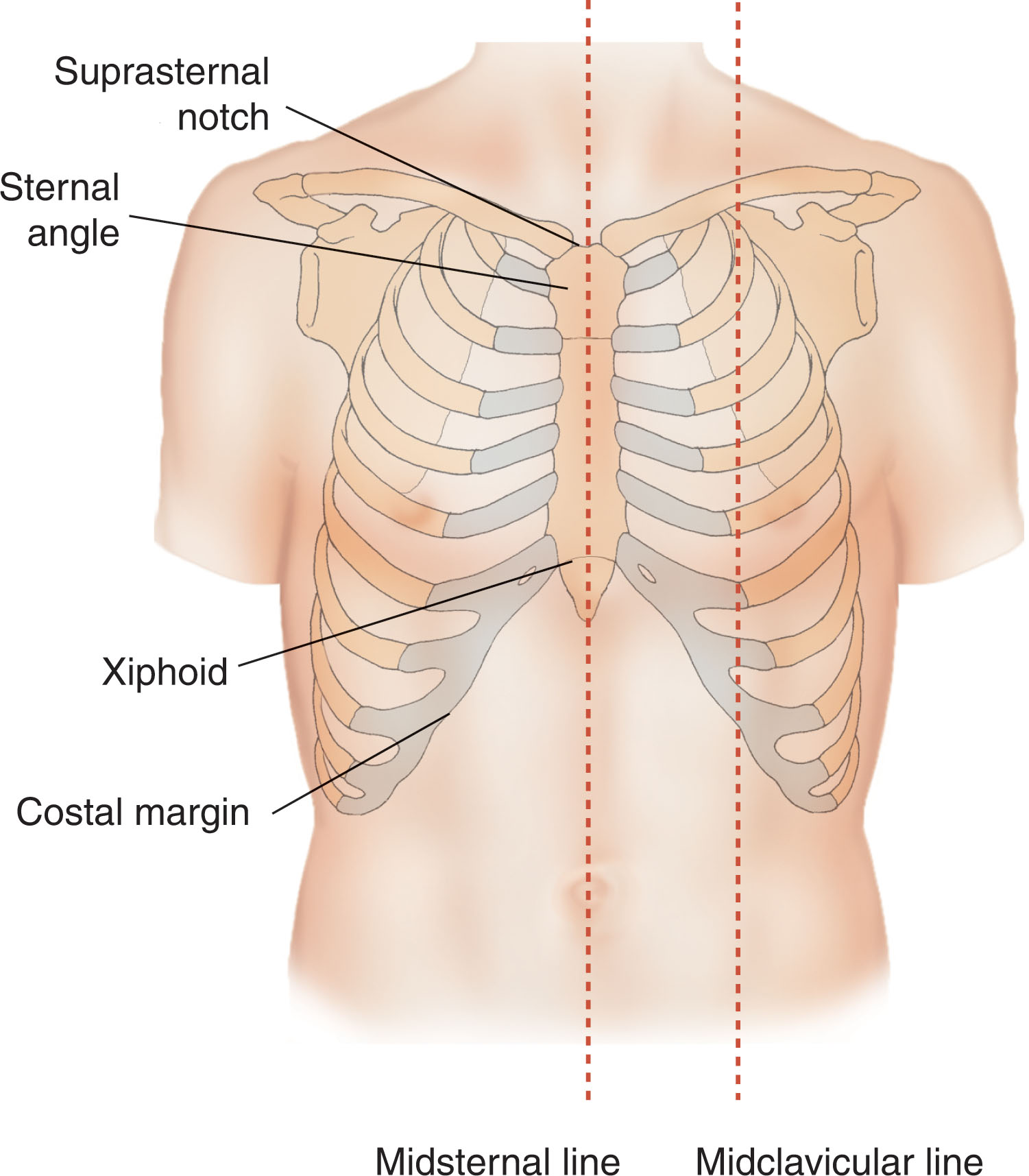
The thorax constitutes the upper part of the body between the neck and the diaphragm. There are eight external landmarks of the thorax ( Fig. 30.1 ). The costal margin is the lower boundary of the thorax; it is formed by the cartilages of the seventh through tenth ribs and the ends of the eleventh and twelfth cartilages. The midaxillary line runs vertically from a point midway between the anterior and posterior axillary folds. The midclavicular line is a vertical line from the midpoint of the clavicle. The midsternal line lies in the median plane over the sternum. The sternal angle is the angle between the manubrium and the body of the sternum; it is also known as the angle of Louis. The suprasternal notch is the superior margin of the manubrium sterni, lying opposite the lower border of the body of the second thoracic vertebra. The xiphisternal joint is the junction between the xiphoid and the sternum. The final external landmark of the thorax is the xiphoid , the lowest point of the sternum.
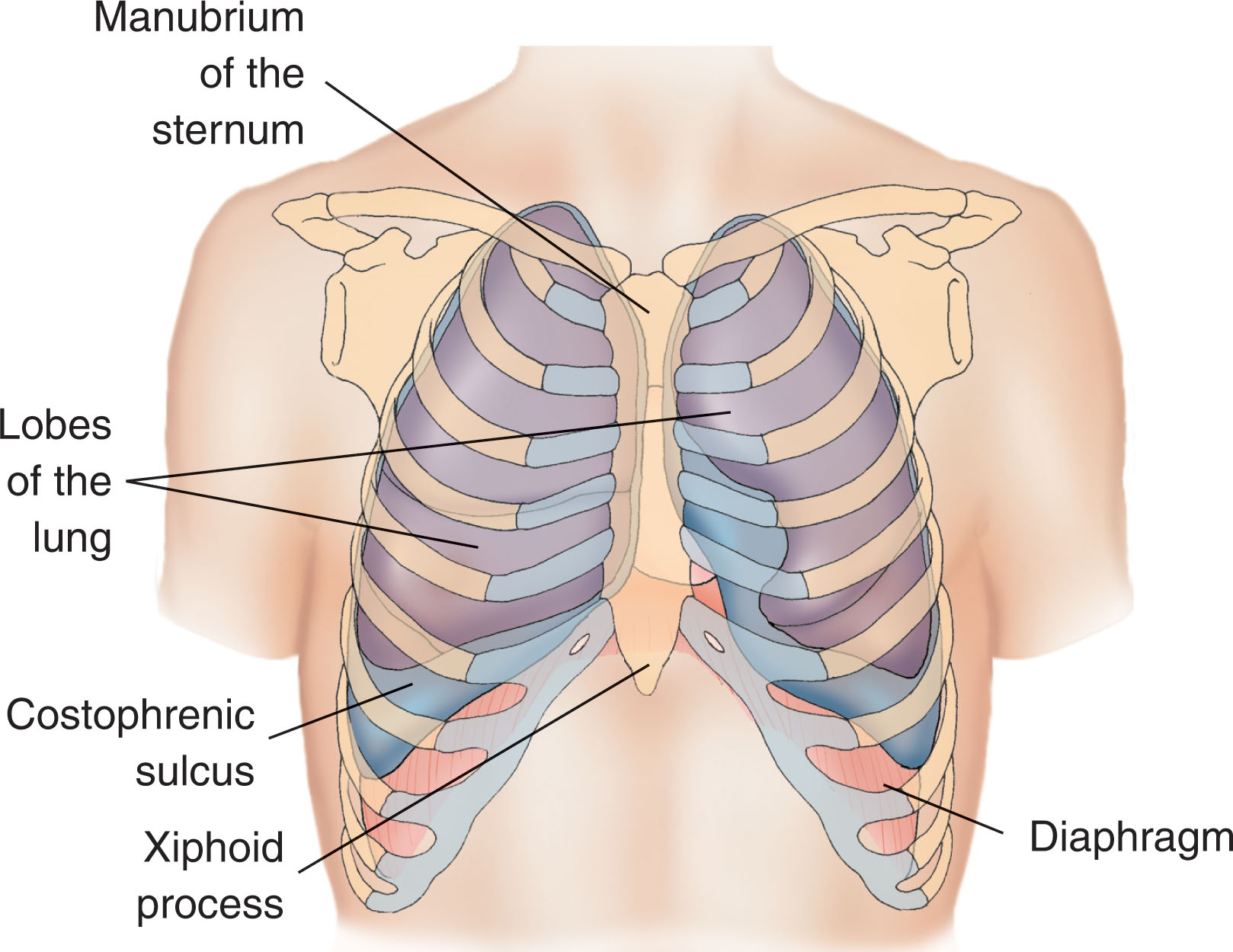
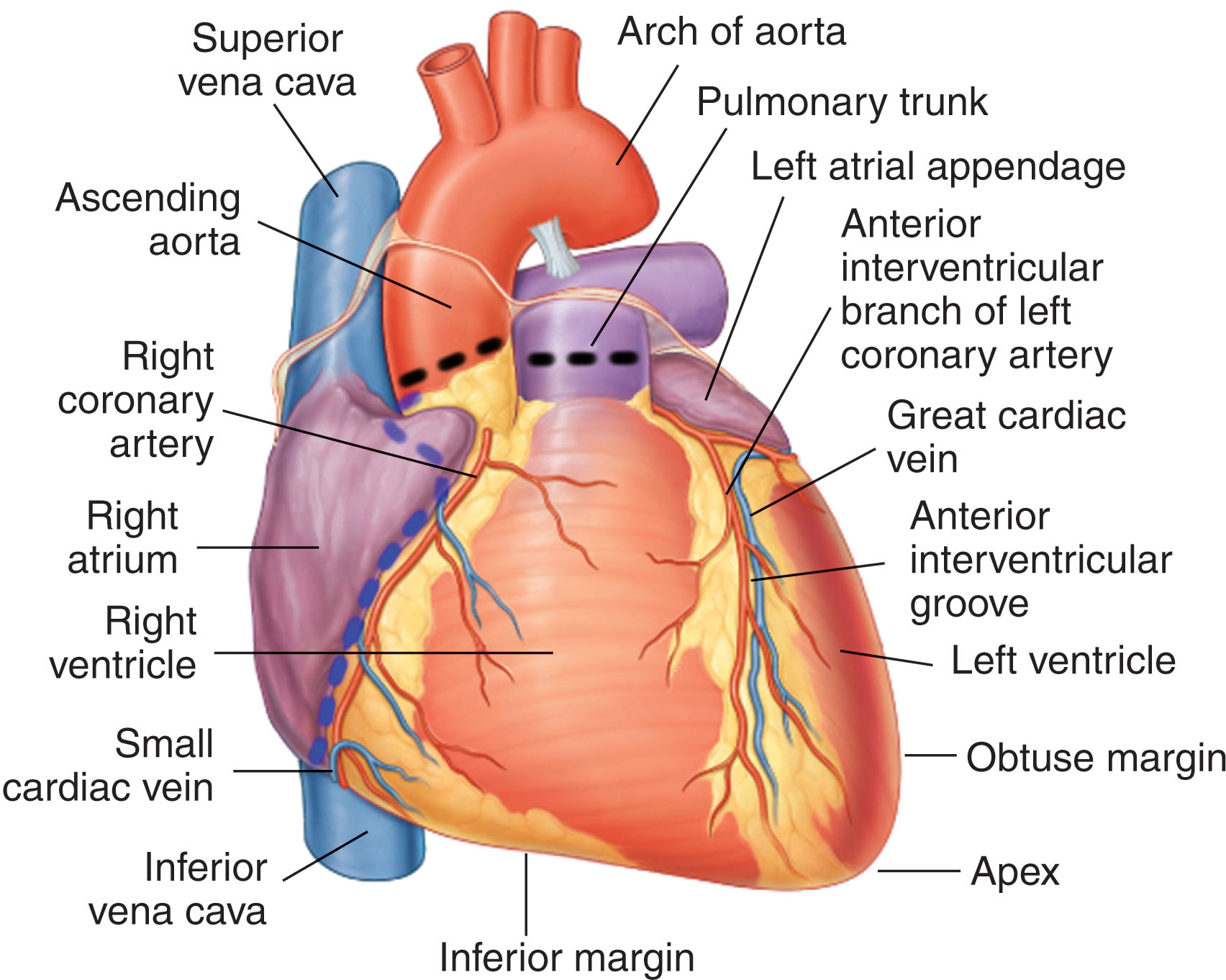
The thoracic cavity lies within the thorax and is separated from the abdominal cavity by the diaphragm ( Fig. 30.2 ). The diaphragm reaches upward as high as the midaxillary level of the seventh rib. The mediastinum is the medial portion of the thorax, and the pleurae and lungs are the lateral components.
Superiorly, the upper thoracic cavity gives access to the root of the neck. It is bounded by the upper part of the sternum, the first ribs, and the body of the first thoracic vertebra.
Anteriorly, the sternum consists of the manubrium, the corpus sterni (body), and the xiphoid process. The junction between the manubrium and the body of the sternum is a prominent ridge; together they form the angle of Louis. This palpable landmark is important in locating the superior mediastinum or the second rib cartilages, which articulate with the sternum at this point.
The greater part of the thoracic cavity is occupied by the two lungs, which are enclosed by the pleural sac. To understand the pleural sac, imagine a deflated plastic bag covering your fist. Your fist should be enveloped by both sides of the bag to simulate the pleural sac. The internal layer, or visceral pleura, is adherent to each lobe of the lung. The external layer, or parietal pleura, is adherent to the inner surface of the chest wall (costal pleura), diaphragm (diaphragmatic pleura), and mediastinum (mediastinal pleura). The two layers become continuous with each other by a “cuff” of pleura that surrounds the structures at the hilum of the lung.
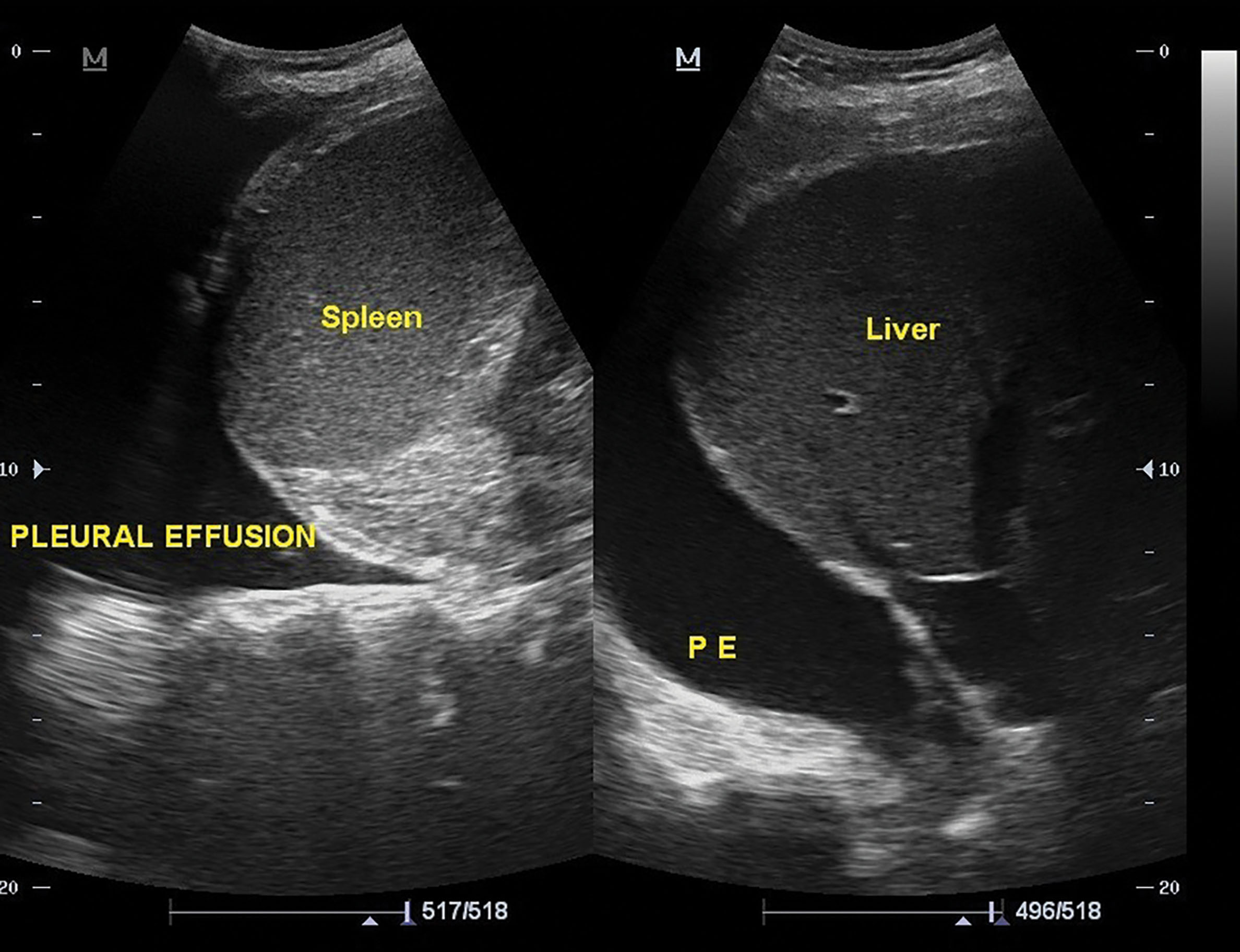
The costophrenic sinus is the pleural reflection between the costal and diaphragmatic portions of the parietal pleura. This space lies lower than the edge of the lung and, in most cases, is never occupied by the lung. When pleural fluid accumulates, its most common location is in the costophrenic sinus. On a radiographic examination, the costophrenic angle is blunted by the presence of pleural effusion.
The mediastinum is the median partition of the thoracic cavity. The mediastinum is a movable, thick structure and extends superiorly to the thoracic inlet and the root of the neck and inferiorly to the diaphragm. It extends anteriorly to the sternum and posteriorly to the twelfth thoracic vertebra. Within the mediastinum are found the remains of the thymus, the heart and great vessels, the trachea and esophagus, the thoracic duct and lymph nodes, the vagus and phrenic nerves, and the sympathetic trunks.
The mediastinum may be divided into a superior and inferior mediastinum by an imaginary plane from the sternal angle to the lower body of the fourth thoracic vertebra ( Box 30.1 ). The inferior mediastinum is subdivided into three parts: (1) middle, which contains the pericardium and the heart; (2) anterior, which is a space between the pericardium and sternum; and (3) posterior, which lies between the pericardium and vertebral column.
The evaluation of the lungs with ultrasound is primarily based on the interpretation of artifacts produced at the pleural surface. Most of these artifacts relate to the interaction of ultrasound and air. Although ultrasound can be used to interpret the characteristics of the surface of an air interface, it cannot penetrate gas; therefore, pathology lying deep to air cannot be visualized with ultrasound. With the exception of the mediastinal reflections, ultrasound can be used to explore most of the pleural surface of the lungs. There is frequently an overlap in the sonographic appearance of differing conditions, and integration with the clinical picture is important.
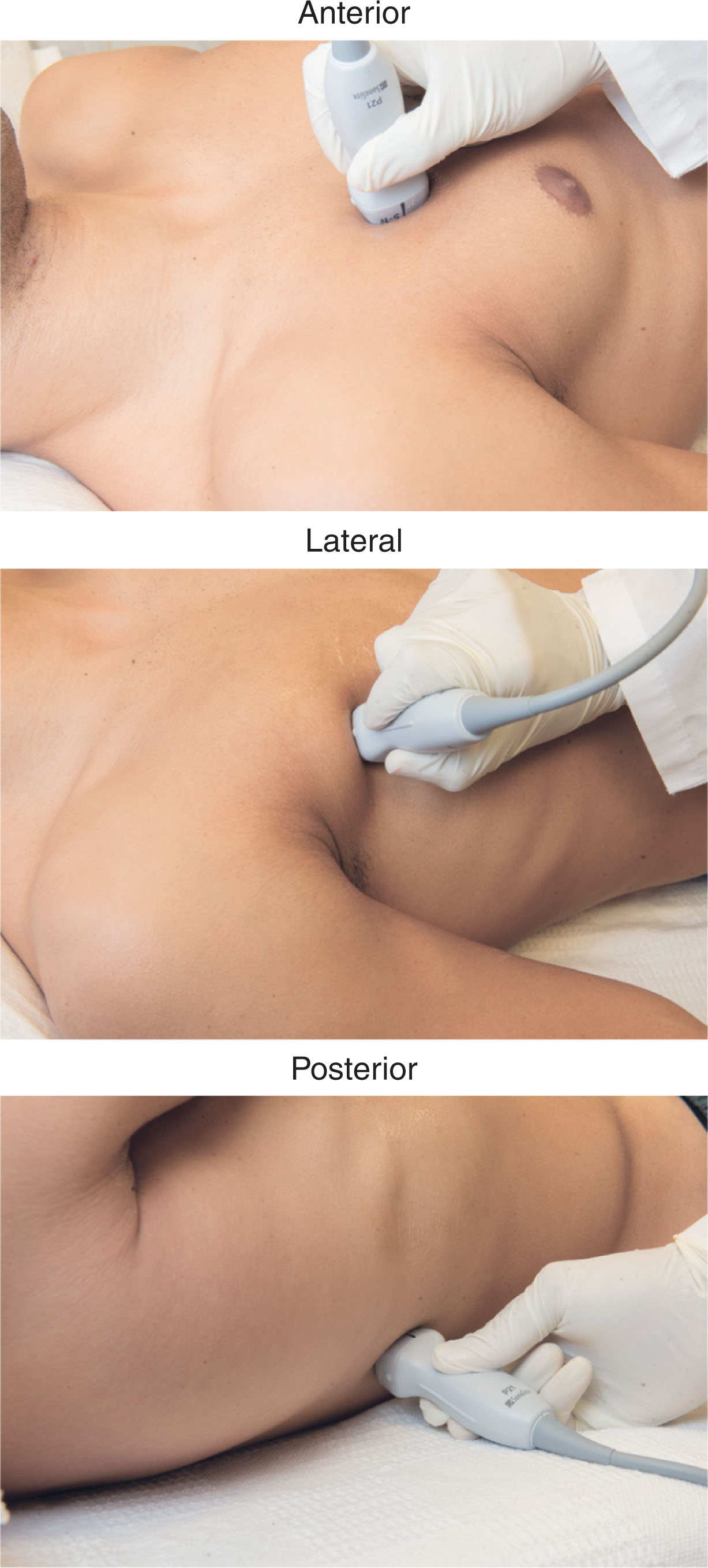
In trauma cases the patient is supine, which is convenient for the detection of a pneumothorax where free pleural air gathers at the most apical point of the thoracic cavity. The detection of a hemothorax—which is more dependent—is challenging, with a posterolateral approach required using the liver or spleen as an acoustic window. Intubated patients are generally supine for the anterior, lateral, and posterior approach—with the patient rolled to one side or other. The conscious patients in acute respiratory distress usually sit up to optimize their ventilators. Access to the entire chest wall is possible with this approach. If the patient is not acutely distressed and is sitting on a chair or stool, maximal chest wall accessibility is possible. Ask the patient to hug themselves or put their arms out forward to move the scapula around the chest wall to help access the upper posterior lung.
The probes utilized to evaluate the lungs include the curvilinear (for good penetration with low frequency), the linear (for pleural surface detail with high frequency; Fig. 30.3 ), or the phased array transducer (for visualization of the pleural surface and the pleural fluid).
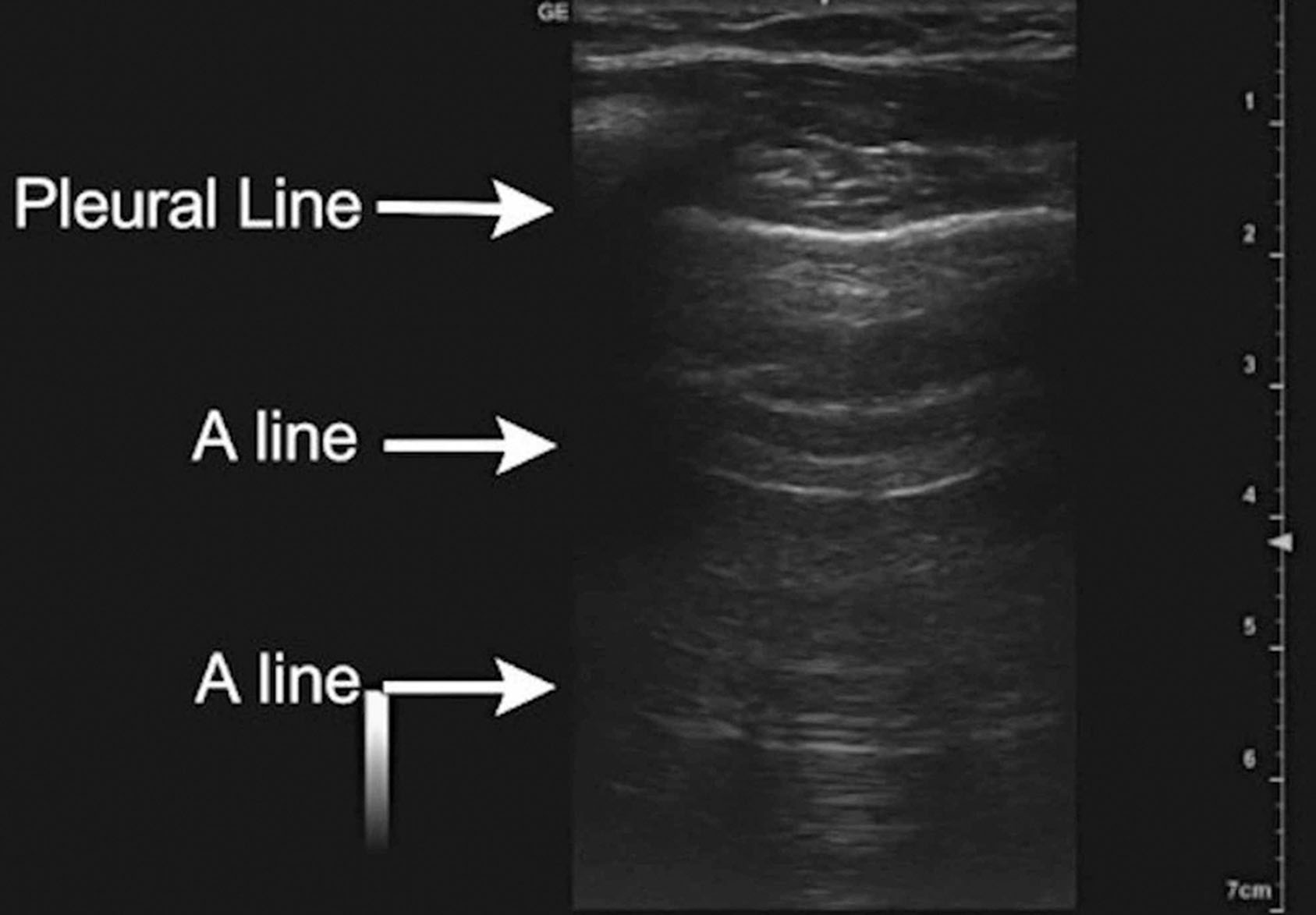
Ultrasound evaluation of the pleural line to look for lung sliding ( Fig. 30.4 ) or lung pulse is done by looking for movement at the pleural line. Vertical artifacts below the pleural lining may represent comet tails or B-lines ( Fig. 30.5 ). Horizontal artifacts below the pleural line may be seen when the pleural line is perpendicular to the line of interrogation of the ultrasound beam ( Fig. 30.6 ).
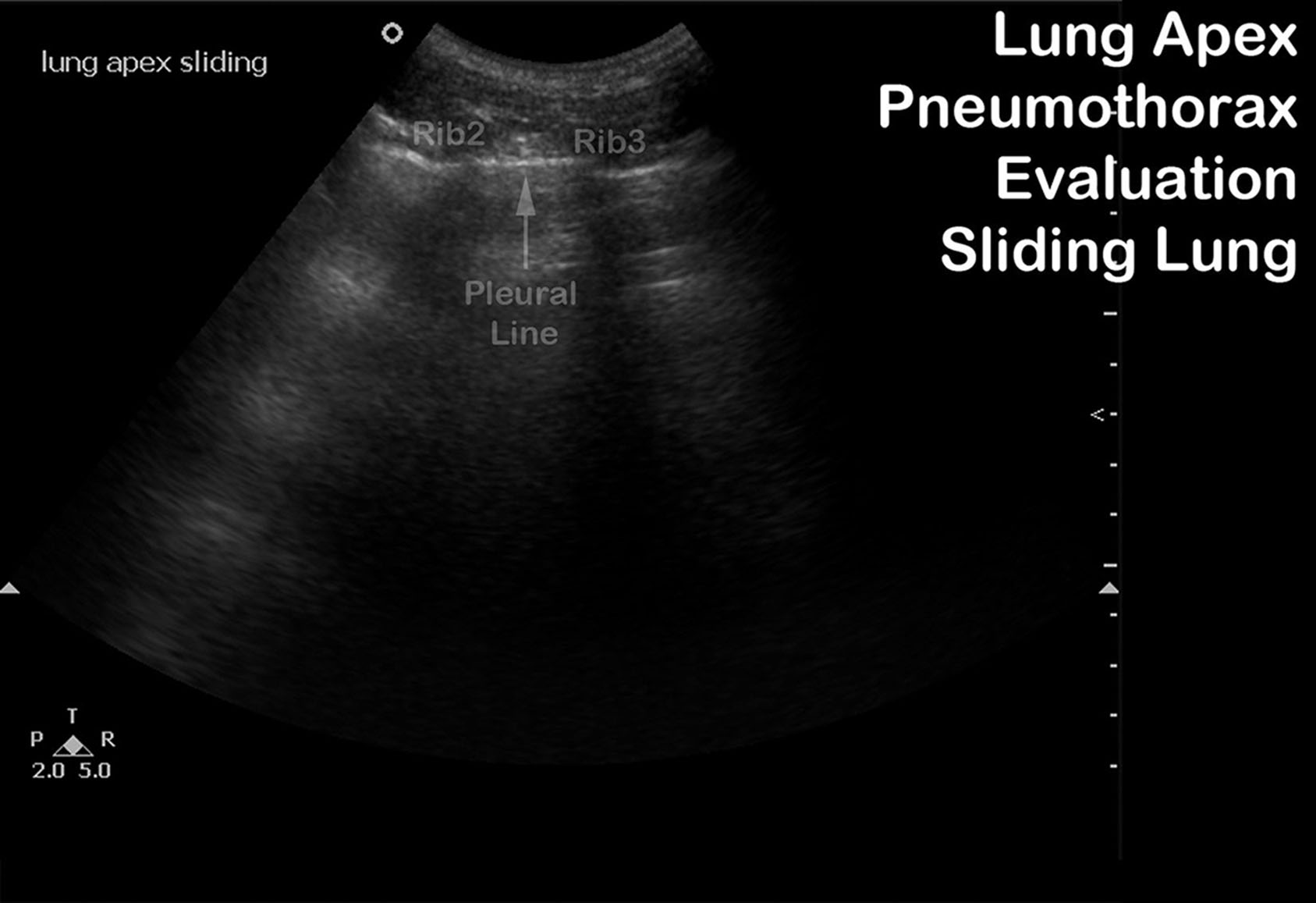
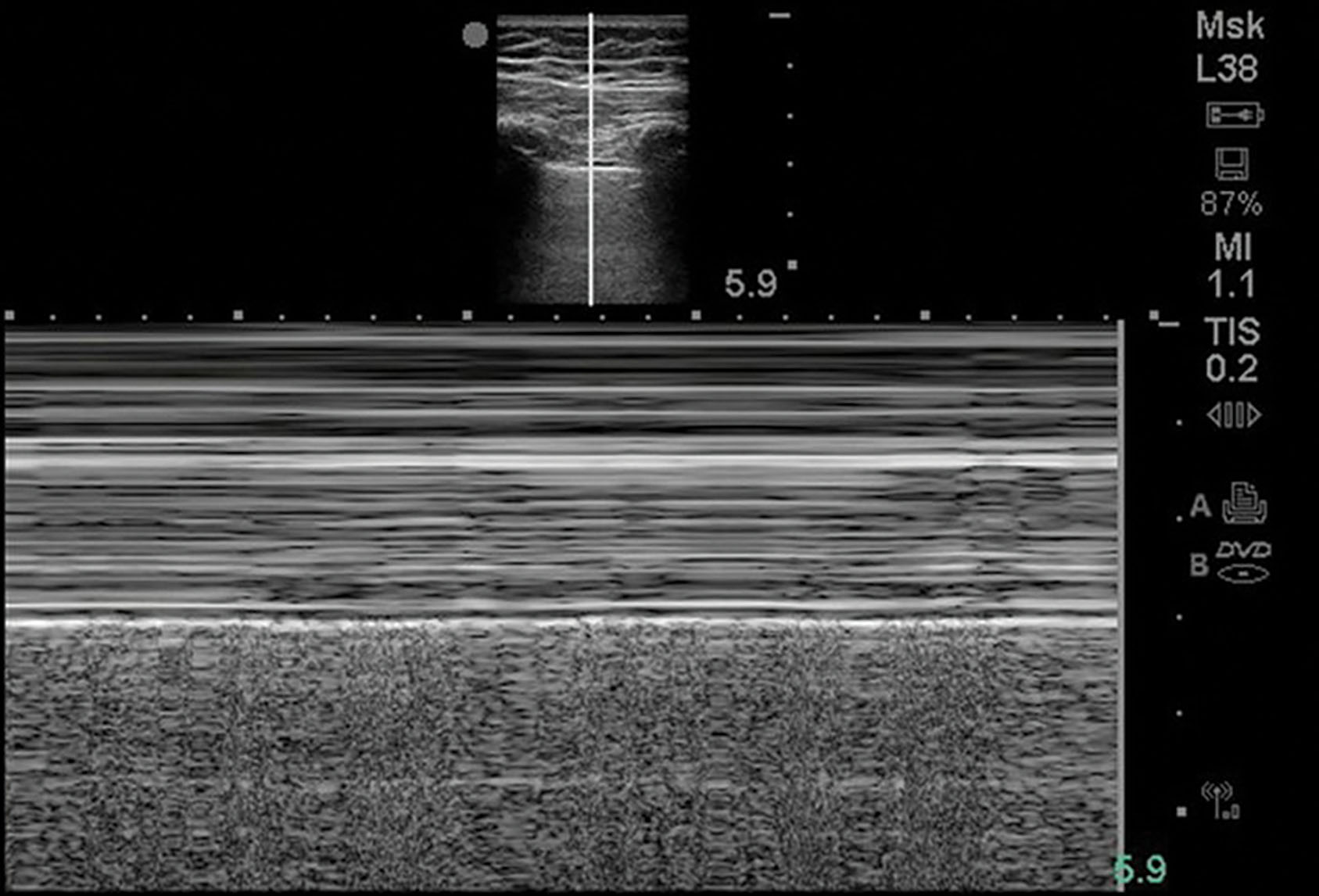
Lung that is normally aerated has a characteristic pattern of air artifact designated as A-lines ( Fig. 30.7 ). These A-lines indicate air, whether physiologic of pathologic. A-lines are horizontally oriented hyperechoic lines seen deep to the pleural line. They represent reverberation artifacts from the ultrasound reflection between the pleural surface and the outer surface of the chest wall. Therefore, their depth is a multiplicative of the distance between the skin surface and the pleural line.
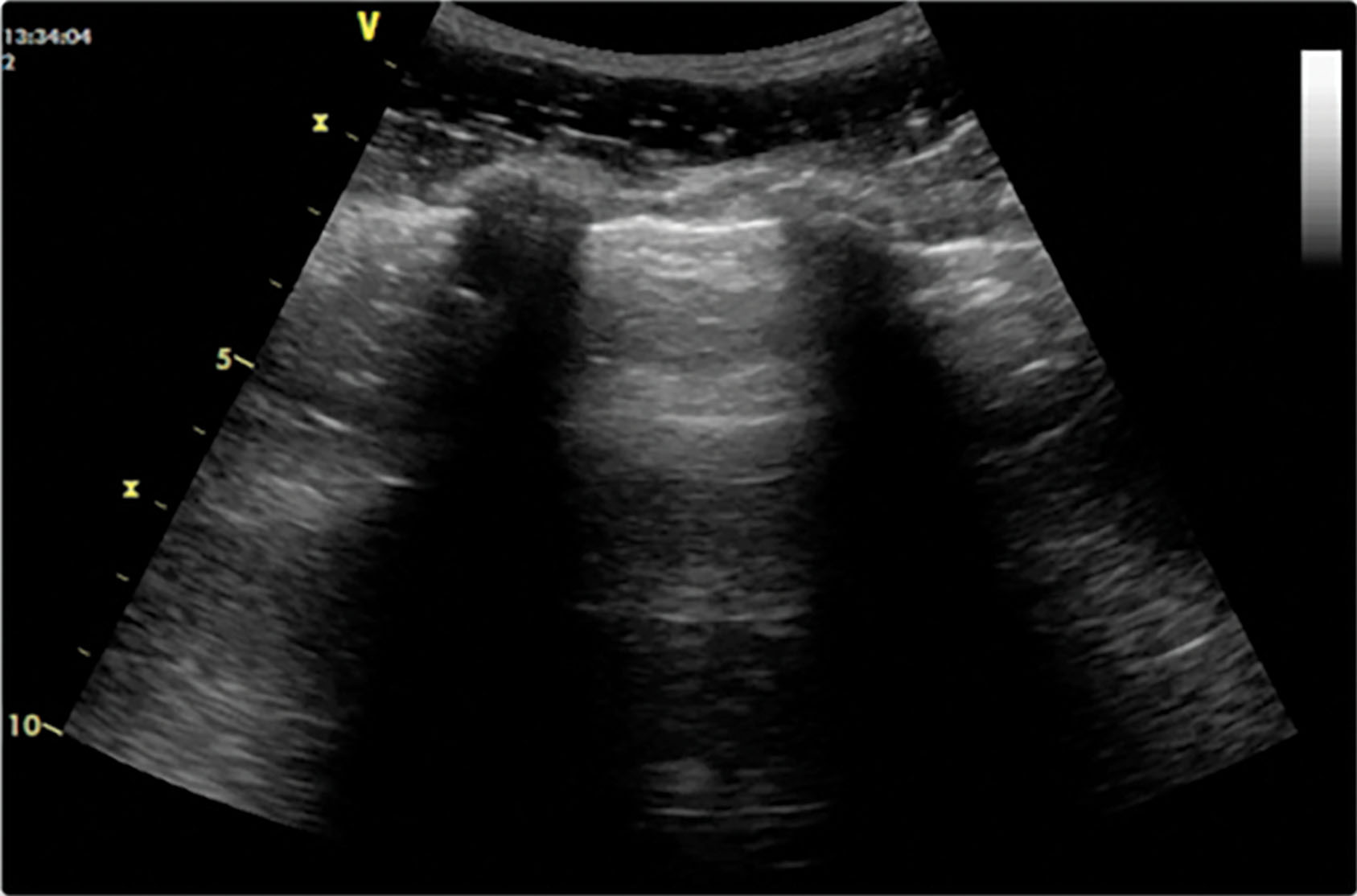
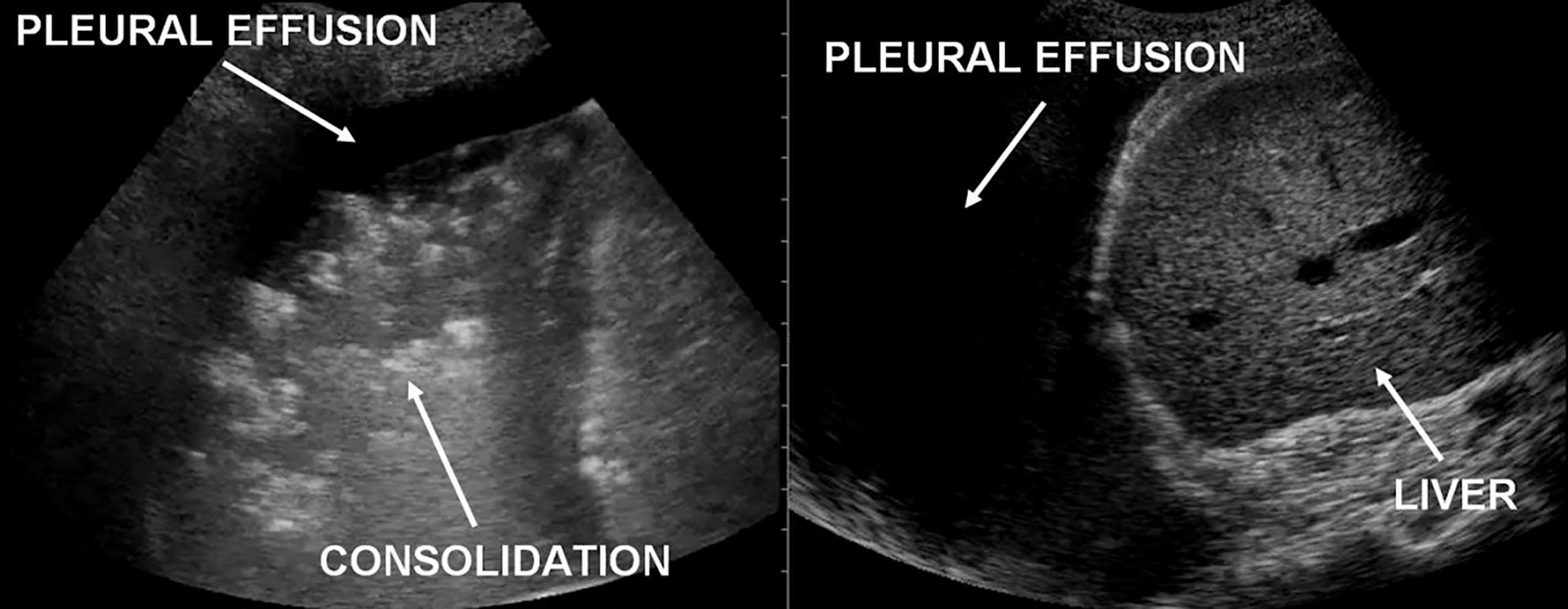
In the presence of a pleural effusion, the costophrenic angle is filled with fluid that allows the ultrasound to reach the spine ( Fig. 30.8 ). A loculated effusion may not involve the costophrenic angle and requires scanning multiple zones ( Fig. 30.9 ).
The heart lies obliquely in the chest, posterior to the sternum, with the greater portion of its muscular mass lying slightly to the left of midline. The heart is protected within the chest by the sternum and rib cage anteriorly and the vertebral column and rib cage posteriorly. The other structures within the thoracic cavity in close approximation to the heart are the lungs, esophagus, and descending thoracic aorta.
Contrary to most simplified anatomic illustrations, the heart is not situated with its right chambers lying to the right and its left chambers to the left. It may be better considered as an anteroposterior structure, with its right-side chambers located more anterior than its left-side chambers. As we look at the embryologic development, the heart forms as a tubular right-to-left structure. However, as development continues, the right side becomes more ventral and the left side remains dorsal.
In addition, another change in axis causes the apex (or the inferior surface of the heart) to tilt anteriorly. The final development of the heart presents the right atrium anterior to the left atrium and to the right of the sternum, whereas the right ventricle presents anterior to the left ventricle and slightly to the left of the sternum. The left atrium becomes the most posterior chamber to the left of the sternum, whereas the left ventricle swings its posterior axis slightly toward the anterior chest wall.
The heart has three surfaces: sternocostal (anterior), diaphragmatic (inferior or apex), and base (posterior) ( Fig. 30.10 ). The right atrium forms the right border of the heart to the right of the sternum. The vertical atrioventricular groove separates these two structures.
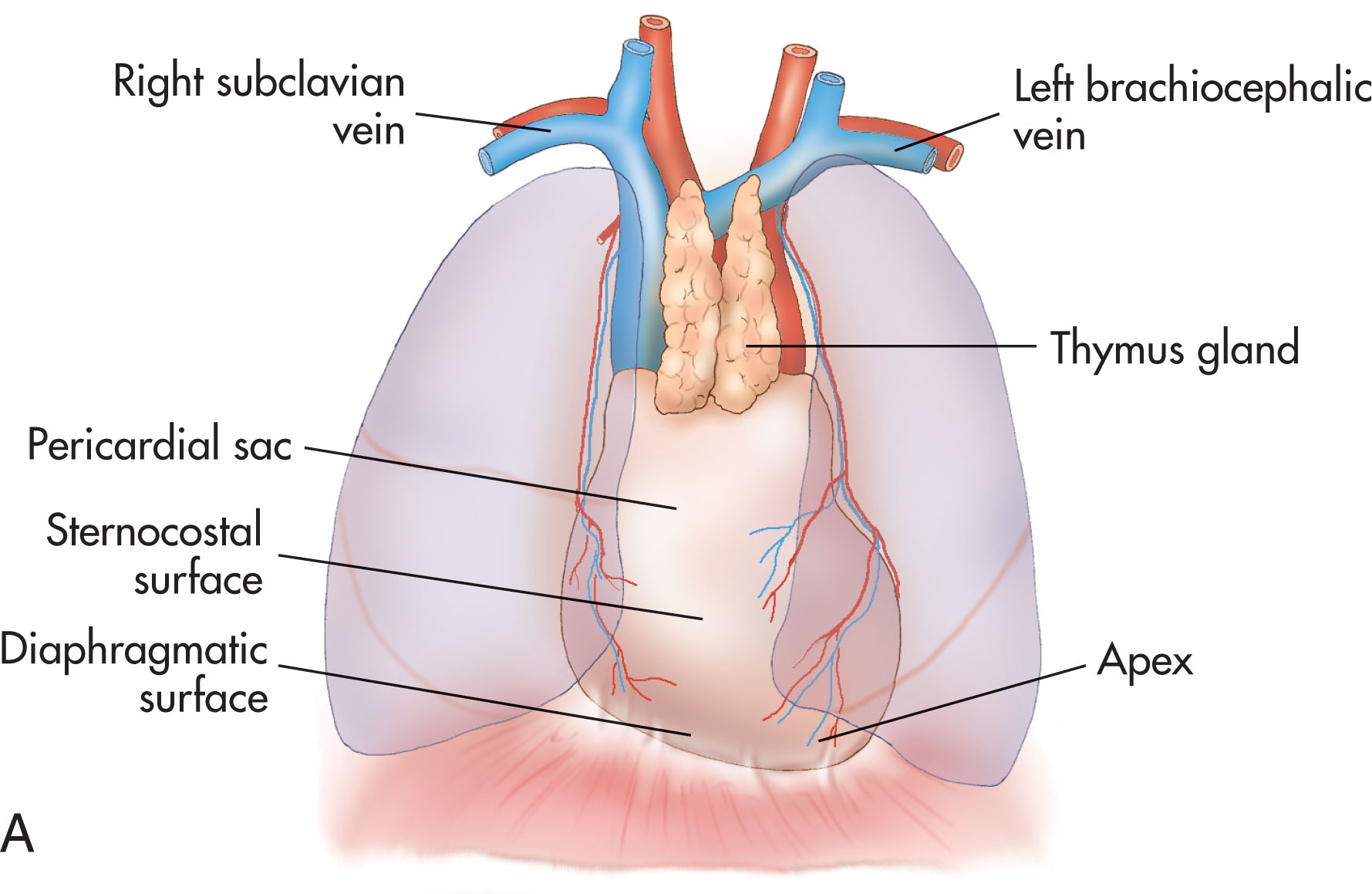
The left border is formed by the left ventricle and left atrial appendage. The right and left ventricles are separated by the anterior interventricular groove ( Fig. 30.11 ). The diaphragmatic surface of the heart is formed principally by the right and left ventricles, separated by the posterior interventricular groove. A small part of the inferior surface of the right atrium also forms this surface.
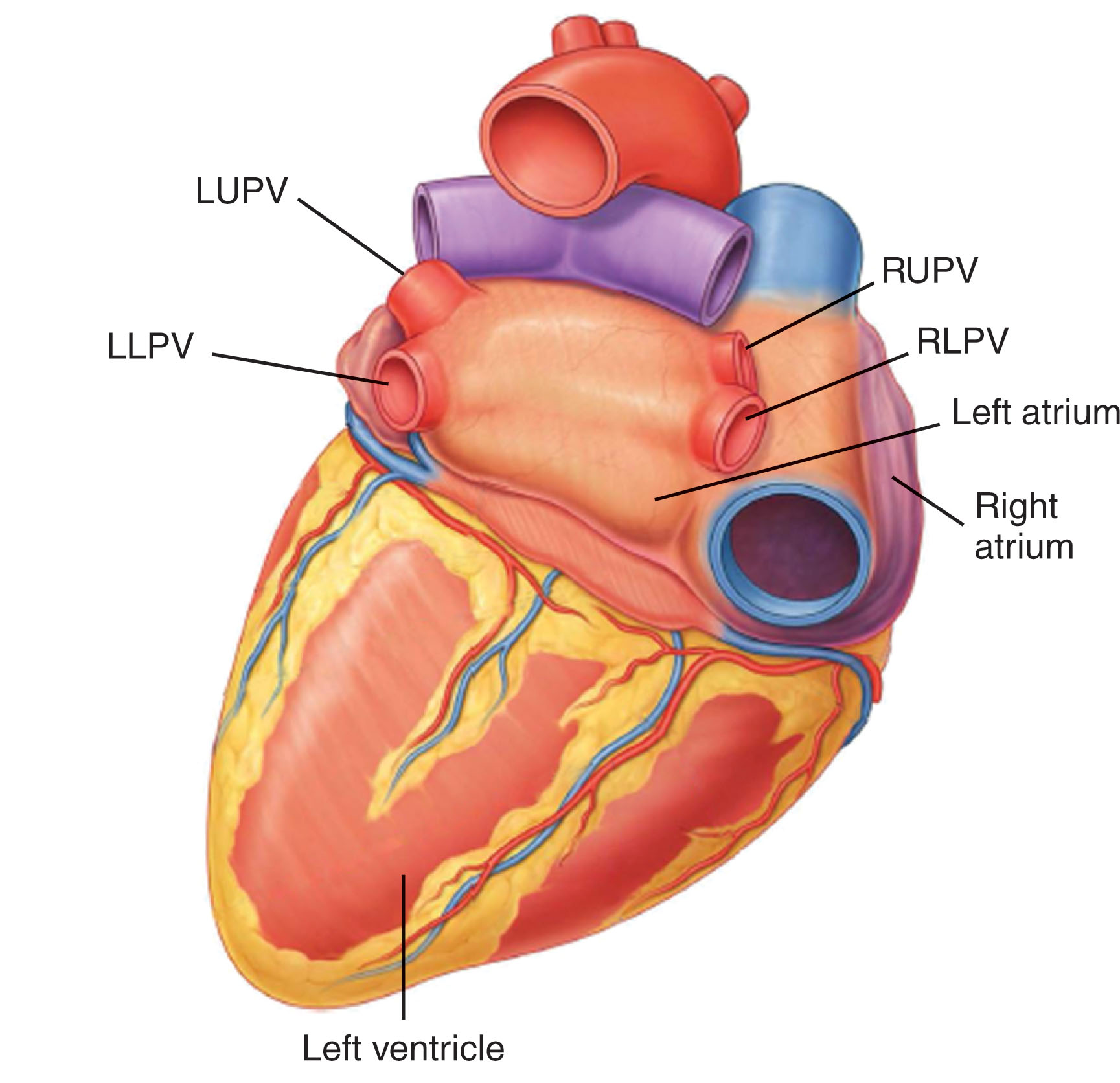
The base of the heart is formed by the left atrium, into which the four pulmonary veins enter from the lungs. The right atrium contributes a small part to this posterior surface ( Fig. 30.12 ). The left ventricle forms the apex of the heart, which can be palpated at the level of the fifth intercostal space, about 9 cm from the midline.
The heart and roots of the great vessels lie within the pericardial sac (see Fig. 30.10 ). Like the pleura of the lungs, the pericardium is a double sac. The fibrous pericardium limits the movement of the heart by attaching to the central tendon of the diaphragm below and the outer coat of the great vessels above. The sternopericardial ligaments attach to it in the front. The serous pericardium is divided into parietal and visceral layers. The parietal layer lines the fibrous pericardium and is reflected around the roots of the great vessels to become continuous with the visceral layer of serous pericardium. The visceral layer is closely applied to the heart and is often called the epicardium . The slit between the parietal and visceral layers is the pericardial cavity. This cavity normally contains a small amount of fluid that lubricates the heart as it moves.
The pericardial sac protects the heart against friction. If the serous pericardium becomes inflamed, pericarditis will develop, or if too much pericardial fluid, fibrin, or pus develops in the pericardial space, the visceral and parietal layers may adhere to one another.
The pericardial sac does not totally encompass the heart. On the posterior left atrial surface of the heart, the reflection of serous pericardium around the pulmonary veins forms the recess of the oblique sinus. This may be an important landmark in the echocardiographic separation of pericardial effusion from pleural effusion. The transverse sinus lies between the reflection of serous pericardium around the aorta and pulmonary arteries and between the reflections around the pulmonary veins.
The chambers of the heart are lined by the endocardium, myocardium, and epicardium. ( Fig. 30.13 ) The endocardium is the intimal lining of the heart and is continuous with the intima of the vessels connecting to it. The endocardium is similar to the intima of blood vessels. It also forms the valves that lie between the filling (atria) and pumping (ventricle) chambers of the heart and along each base of the two great arterial trunks leaving the heart (the aorta and pulmonary artery).
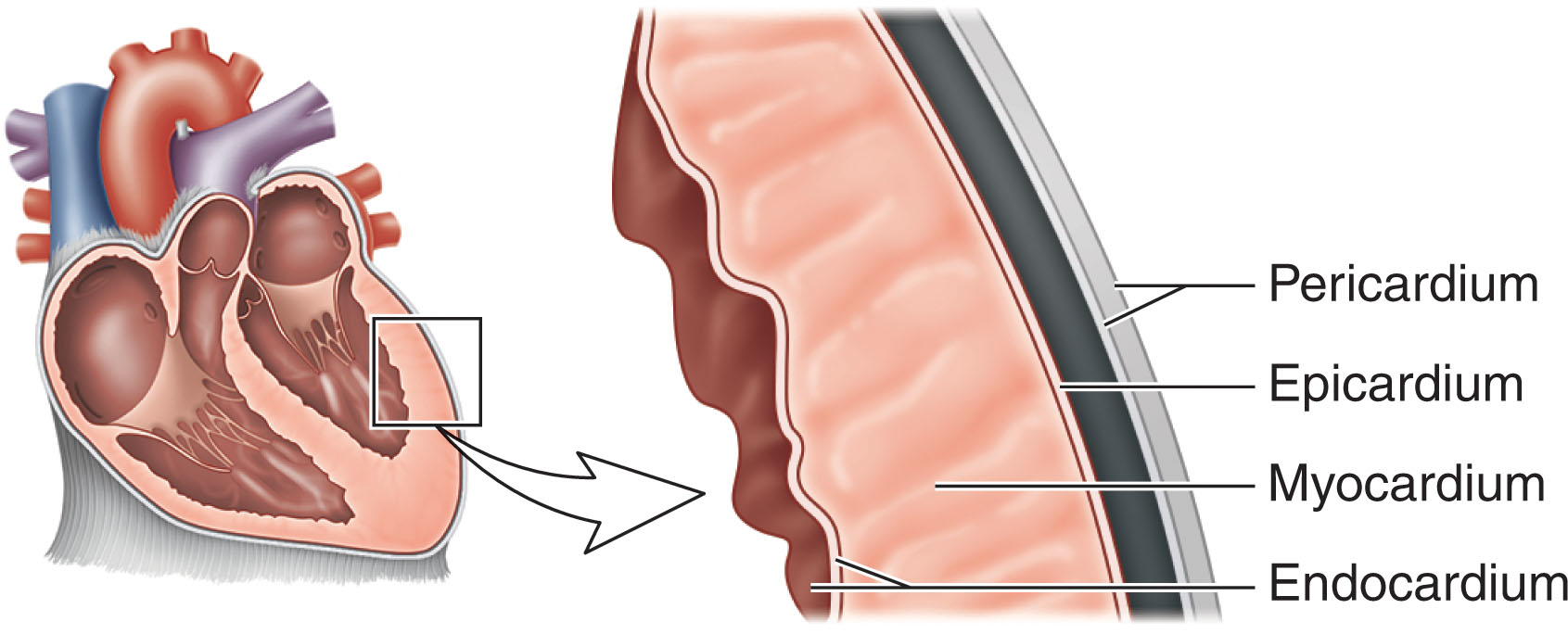
The muscular part of the heart, the myocardium , is a special type of muscle found only in the heart and great vessels. This cardiac muscle is equivalent to the media of a blood vessel. The cardiac muscle is complex compared with other muscular fibers. Although it is striated like voluntary muscle, the fibers of the cardiac muscle branch and anastomose so that it is impossible to determine the limits of a fiber. The myocardium of both ventricles is one continuous muscle mass, as is the myocardium of both atria. Because of this continuity, an impulse for contraction originating in the atrium can spread throughout the atrial musculature; similarly, an impulse originating in a ventricle can spread throughout the ventricular musculature. A special bundle of fibers connects the atria to the ventricles. The unique feature of cardiac muscle is the ability to possess intrinsic rhythmic contractility. It is this rhythmicity that keeps the heart contracting, with nerve impulses modifying rather than initiating the heartbeat.
Because the atria work at low pressures, the musculature of the atria is thin compared with the ventricular wall mass. The primary purpose of the atria is to act as filling chambers that drive the blood into the relaxed ventricular cavity. In contrast, the myocardium of the ventricles is much thicker than that of the atria. The left ventricle has the greatest muscle mass, because it must pump blood to all of the body, whereas the right ventricle needs only enough pressure to pump the blood to the lungs.
The outside layer of the heart is the epicardium , or the visceral layer of the serous pericardium. The outer surface of the epicardium is a single layer of mesothelial cells continuous with the serous (inner) surface of the pericardium.
The right atrium forms the right border of the heart ( Fig. 30.14 ). The superior vena cava enters the upper posterior border, and the inferior vena cava enters the lower posterolateral border. The posterior wall of the right atrium is directly related to the pulmonary veins (which flow from the lungs to empty into the left atrium). The medial wall of the right atrium is formed by the interatrial septum. The septum angles slightly posterior and to the patient’s right, so the atrium lies in front and to the right of the left atrium. The central ovale portion of the septum is thin and fibrous. Just superior and in front of the opening of the inferior vena cava lies a shallow depression, the fossa ovalis. Its borders are the limbus fossae ovalis and the primitive septum primum. The foramen ovale lies under the most superior part of the limbus fossae. The limbus fossae ovalis is the remainder of the atrial septum and forms a ridge around the fossa ovalis.
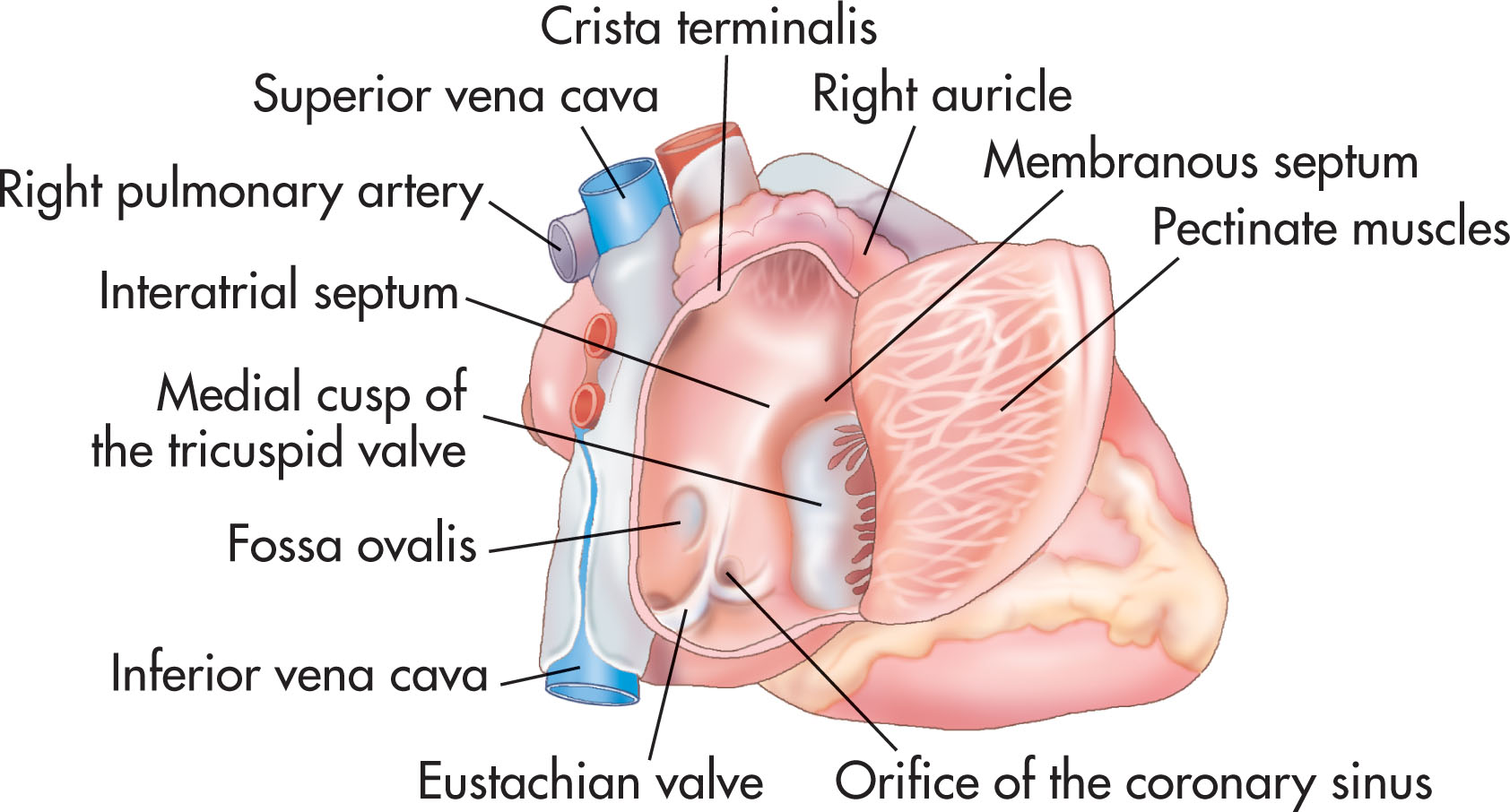
The atrioventricular part of the membranous septum separates the right atrium and left ventricle. Atrial septal defects can occur in this area, causing blood to flow from the high-pressured left ventricle into the right atrial cavity.
The anterior and lateral walls of the right atrium are ridged by the pectinate muscles. The superior portion of the right atrium, the right atrial appendage, contains the most prominent pectinate muscles. The posterior and medial walls are smooth, probably because of the continual flow of blood from the inferior and superior venae cavae and coronary sinus.
The inferior vena cava is guarded by a fold of tissue called the eustachian valve, and the coronary sinus is guarded by the thebesian valve.
The coronary sinus drains the blood supply from the heart wall. It is bordered by the fossa ovalis and the tricuspid valve.
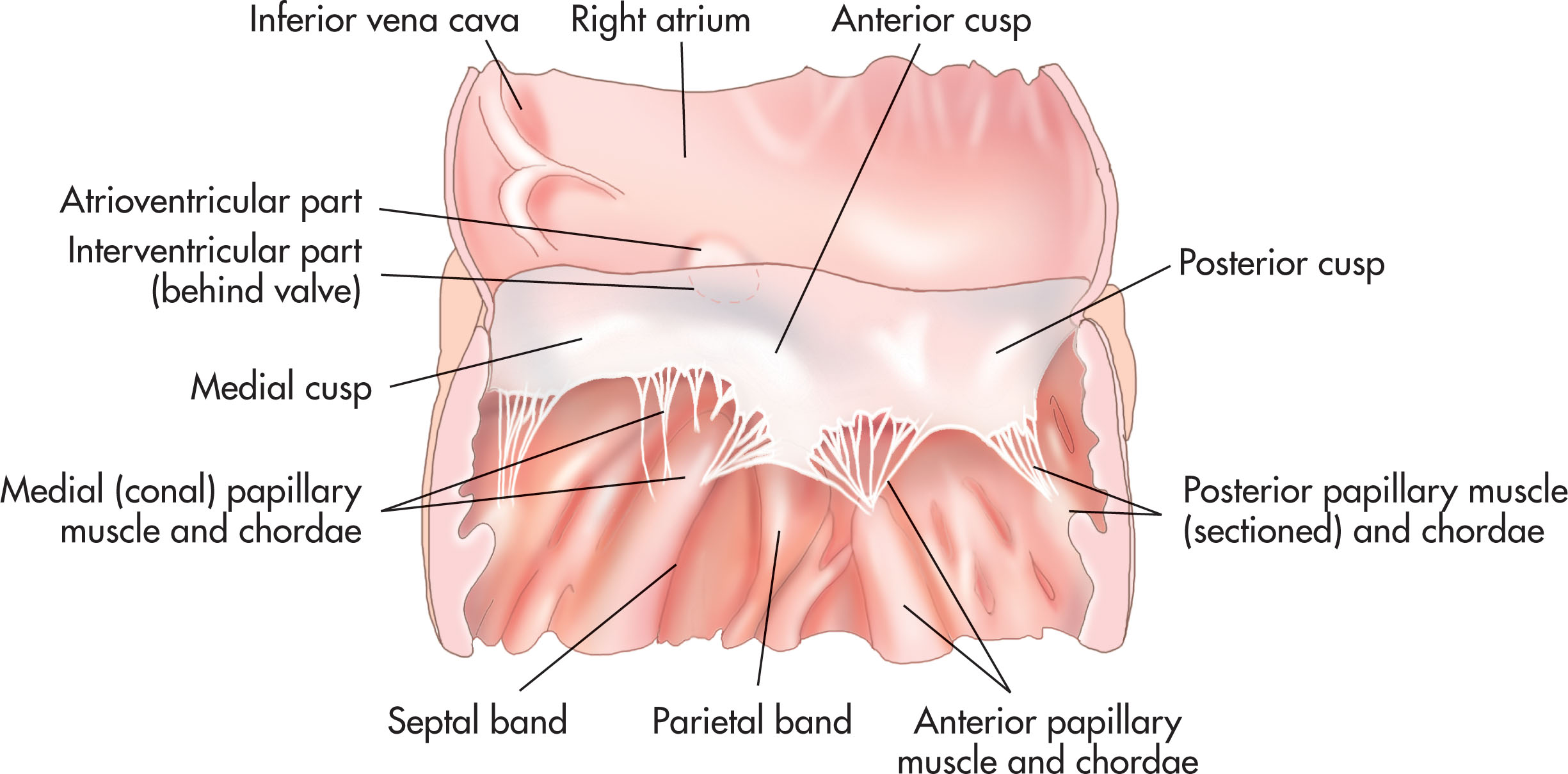
The tricuspid valve separates the right atrium from the right ventricle. It has three leaflets: anterior, septal, and inferior (or mural) ( Fig. 30.15 ). The septal leaflet may be underdeveloped in association with such conditions as ostium primum defect or ventricular septal defect. The leaflets are attached by their base to the fibrous atrioventricular ring. The chordae tendineae attach the leaflets to the papillary muscles. As these muscles contract with ventricular contraction, the leaflets are pulled together to prevent their being pulled into the atrial cavity. The septal and anterior leaflets are connected to the same papillary muscle, which helps in this process.
The base of the right ventricle lies on the diaphragm, and the roof is occupied by the crista supraventricularis, which lies between the tricuspid and pulmonary orifices ( Fig. 30.16 ). The right ventricle is essentially divided into two parts: the posteroinferior inflow portion (containing the tricuspid valve) and the anterosuperior outflow portion (containing the origin of the pulmonary trunk). The demarcation between these two parts is several prominent bands: the parietal band, supraventricular crest, septal band, and moderator band (see Fig. 30.16 ). Together, these bands form an almost circular orifice that normally is wide and forms no impediment to flow.
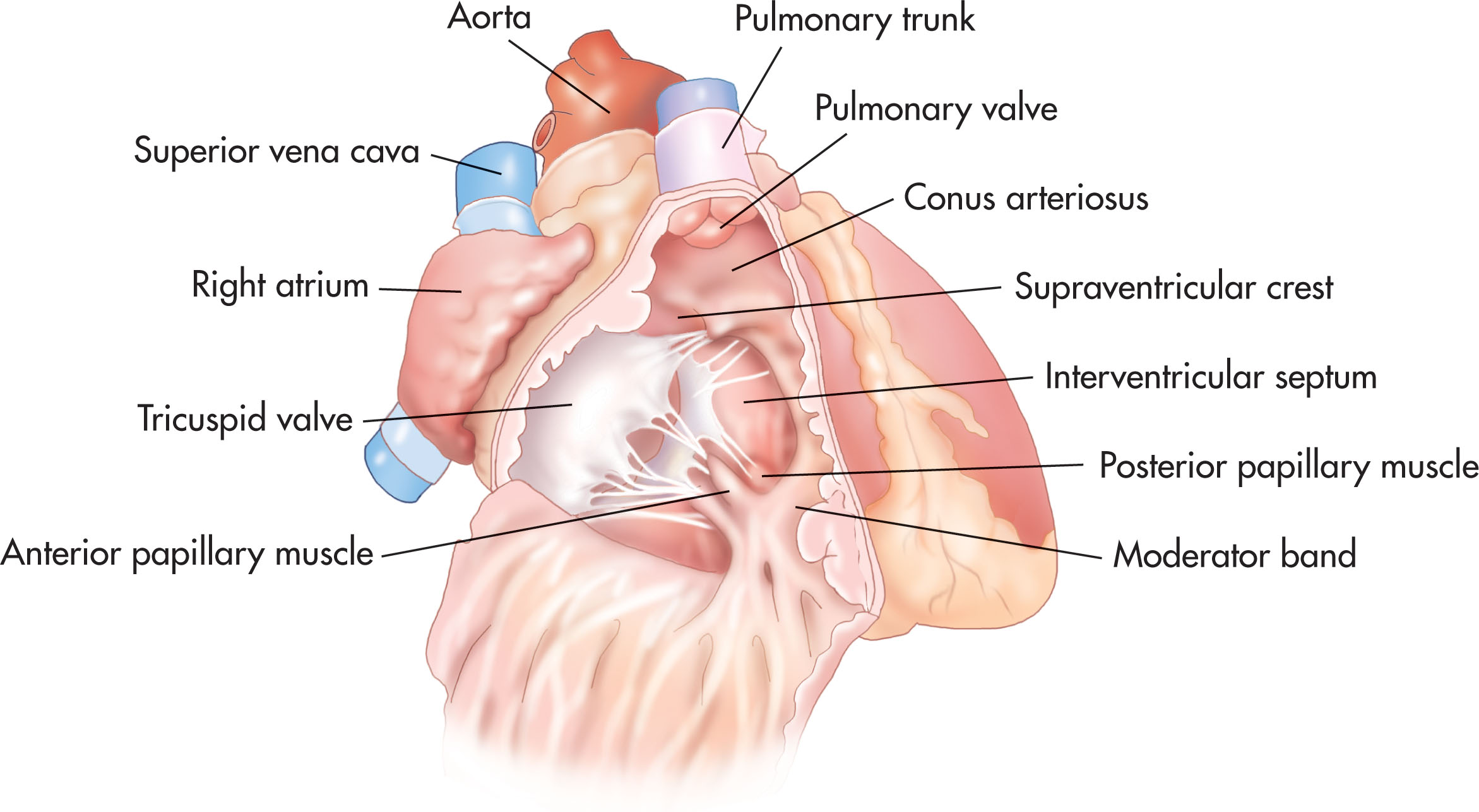
The inflow tract of the right ventricle is short and heavily trabeculated. It extends from the tricuspid valve and merges into the trabecular zone. This zone is the body of the right ventricle. The trabeculae carneae enclose an elongated ovoid opening. The inflow tract unites with the outflow tract, which extends to the pulmonary valve. The outflow portion of the right ventricle, or infundibulum, is smooth walled and contains few trabeculae.
The right ventricle has two walls: an anterior wall (corresponding to the sternocostal surface) and a posterior wall (formed by the ventricular septum).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here