Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The femoral artery is a direct continuation of the external iliac artery, which courses from the inguinal ligament to the adductor canal (subsartorial or Hunter’s canal), where it exits as the popliteal artery. The common femoral artery lies at a point midway between the anterior superior iliac spine and the pubic symphysis. Proximally, the femoral vessels course through the femoral triangle, the borders of which are composed of the inguinal ligament superiorly, the sartorius muscle laterally, and the adductor longus medially. The femoral artery starts superficially and progresses deep and medially together with the femoral vein, which is located medial to the artery.
The proximal common femoral artery and vein are wrapped in the femoral sheath, which is a continuation of the iliac, pectineal, and transversalis endoabdominal fascia. The femoral sheath contains three compartments: the lateral compartment contains the femoral artery, the middle (or intermediate) compartment contains the femoral vein, and the most medial compartment is the femoral canal, which accommodates the passage of lymphatics.
The common femoral artery is the most proximal portion of the femoral artery arising posterior to the inguinal ligament. Branches of the common femoral artery include the superficial circumflex iliac, superficial epigastric, and superficial external pudendal arteries.
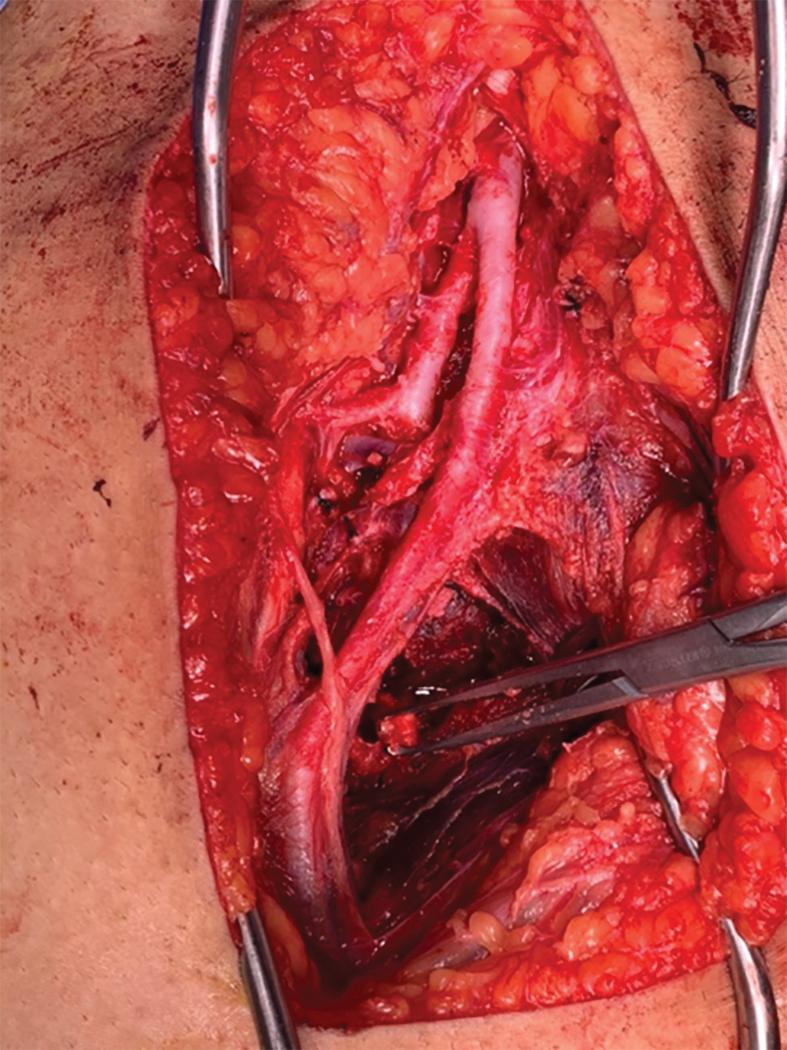
Approximately 4 cm below the inguinal ligament, the common femoral artery bifurcates into the profunda (deep) femoral artery and the superficial femoral artery (SFA) ( Fig. 1 ). The profunda femoral artery arises from the posterolateral aspect of the common femoral artery and courses deep into the thigh muscles where it receives numerous collaterals from branches of the hypogastric artery. Within 2 to 3 cm of its origin, the profunda femoral artery bifurcates into the medial and lateral circumflex arteries.
The SFA is a continuation of the common femoral artery and courses from an anterior location to a posterior medial position as it proceeds distally in the thigh where it transitions to the popliteal artery at the opening of the adductor magnus or Hunter’s canal. The descending genicular artery forms a collateral anastomosis with genicular arteries of the popliteal artery and is the only significant branch of the SFA.
The femoral vein is a continuation of the popliteal vein and receives drainage from two major tributaries, the deep femoral vein and the greater saphenous vein. The latter enters the femoral sheath via the fossa ovalis in the fascia lata, piercing the femoral sheath on its anterior aspect. The femoral vein ends at the inferior edge of the inguinal ligament where it becomes the external iliac vein.
The femoral nerve courses lateral to the femoral artery outside of the femoral sheath. The nerve divides into both anterior and posterior divisions, which contain branches that innervate the anterior compartment of the thigh.
Femoral vessel injuries account for 70% of all arterial trauma, and young males are disproportionately affected by these injuries. Although the vast majority of studies examining extremity vascular injuries have been performed in adult patient populations, several recent civilian and military studies in the pediatric population have reported an incidence of 0.68% to 3.5%.
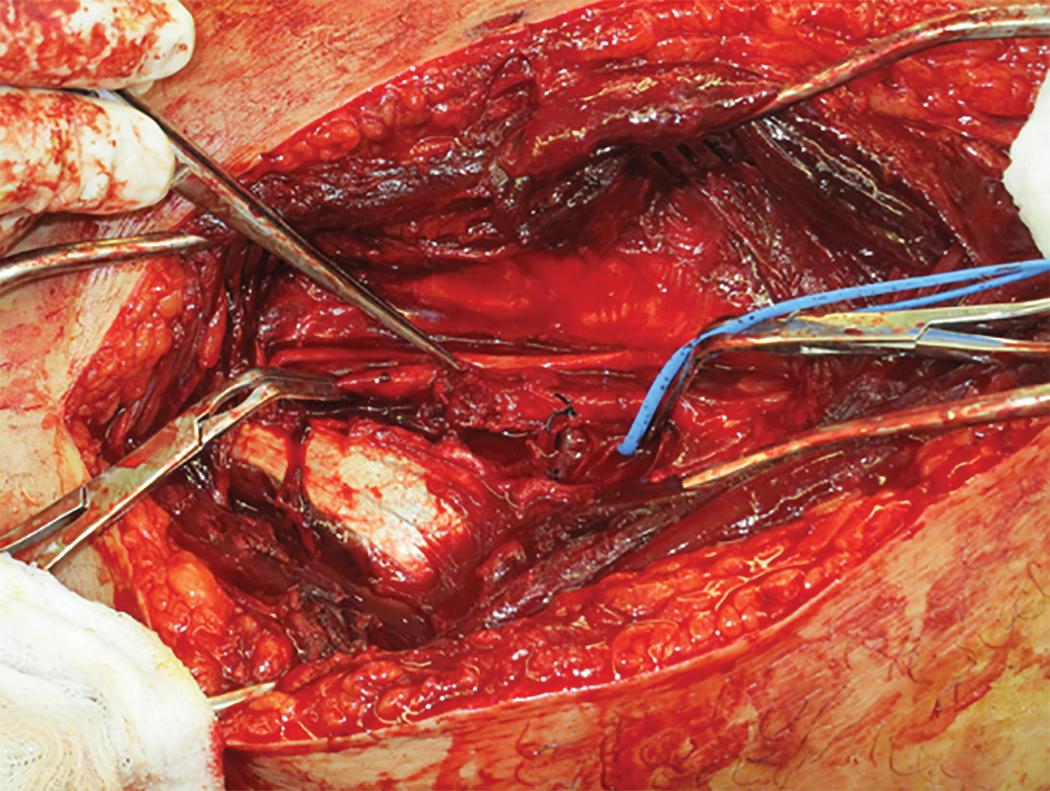
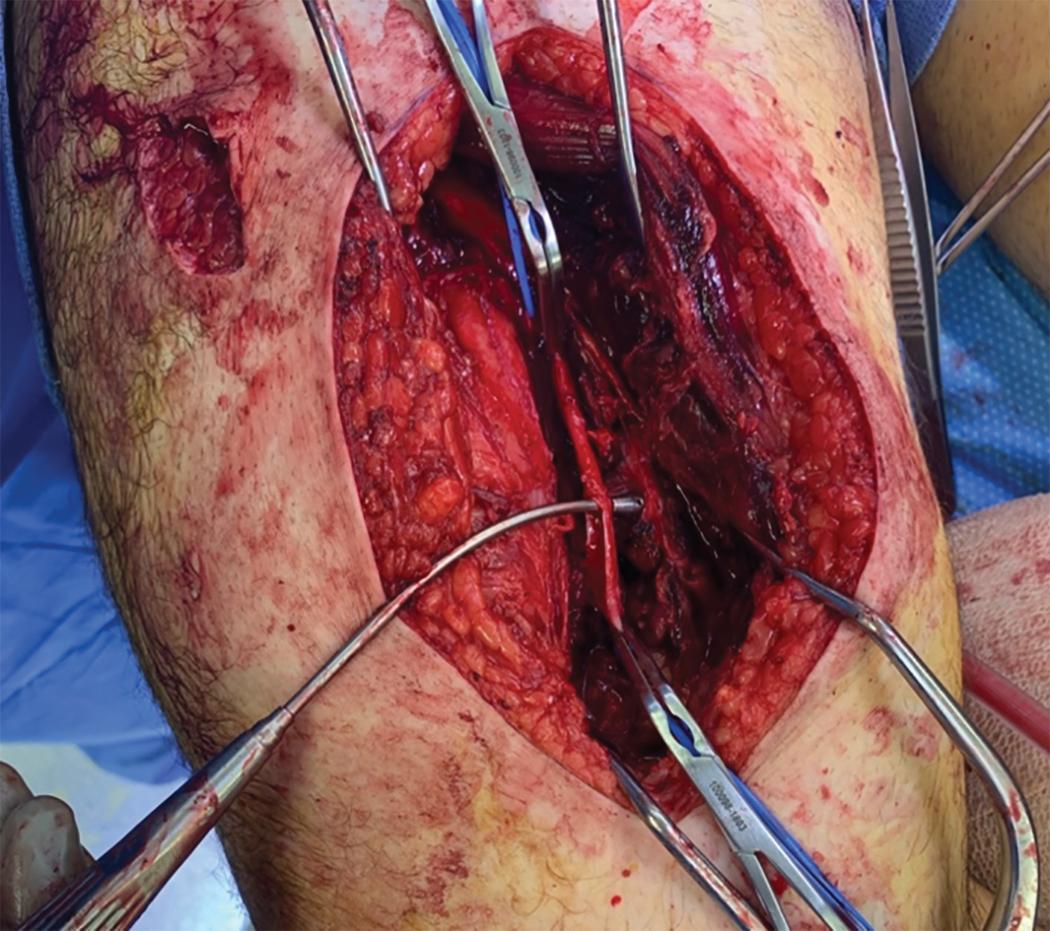
Penetrating mechanisms account for the vast majority of femoral vessel injuries (>80%), and high-velocity gunshot wounds ( Fig. 2 ) are much more common than stab wounds ( Fig. 3 ). Due to the kinetic energy and cavitation associated with ballistic injuries, significant soft tissue and bony injuries usually accompany femoral vessel injuries.
Blunt mechanisms are uncommon and may account for up to 12% to 14% of all femoral vessel injuries. Anterior dislocation of the hip is a rare but potential etiology for blunt injury to the proximal femoral vessels, whereas distal femur fractures may be associated with superficial femoral or supragenicular popliteal artery injuries. In comparison with upper extremity vascular injuries, in which the brachial artery is the most commonly injured vessel, lower extremity vascular injuries occur more commonly and are associated with a higher incidence of adverse outcomes including amputation and death. The type of injury often dictates the clinical presentation ( Table 1 ).
| Type of Injury | Clinical Presentation |
|---|---|
| Partial laceration | Decreased pulse, hematoma, hemorrhage |
| Transection | Absent distal pulses, ischemia |
| Contusion | Initial examination may be normal |
| May progress to thrombosis | |
| Pseudoaneurysm | Initial examination may be normal |
| Bruit, thrill, or decreased pulses | |
| Arteriovenous fistula | Same as pseudoaneurysm |
| External compression | Decreased pulses |
| Return of pulses with fracture reduction |
The incidence of femoral vessel injury is well documented in the civilian trauma literature. Feliciano et al reported a 65% incidence of femoral artery injuries in a series of 220 lower extremity vascular injuries, which parallels recent military data. Other civilian series report an incidence of 26% to 56%.
Femoral vessel injuries are the most common vascular injuries reported in the American wartime experience. The incidence of injuries has increased with each conflict ( Table 2 ). During World War I when limited attempts were made to repair femoral vessel injuries, the incidence of these injuries ranged from 22% to 31%. A similar incidence of 21% was reported during World War II with an amputation rate of 53%. Ligation remained the treatment of choice for these injuries prior to the Korean conflict, in which an incidence of 31% was reported. A 35% incidence of femoral vessel injuries was reported during the Vietnam War. The incidence of femoral vessel injuries during the conflicts in Iraq and Afghanistan has been consistent with previous military experience ranging from 17% to 38%.
| Conflict | Authors (Year) | Total Injuries | Femoral Vessels | Incidence (%) |
|---|---|---|---|---|
| World War I | Makins (1919) | 1191 | 366 | 30.5 |
| World War II | DeBakey and Simeone (1946) | 2471 | 517 | 20.9 |
| Korea | Hughes (1970) | 304 | 95 | 31 |
| Vietnam | Rich (1970) | 1000 | 351 | 35 |
| Iraq | Michael (2007) | 192 (arterial only) | 41 | 21.3 |
| Iraq | Woodward (2007) | 513 | 100 | 19.5 |
| Iraq and Afghanistan | Jasmeet (2011) | 1570 | 268 | 17 |
| Iraq and Afghanistan | Sharrock (2019) | 597 | 225 | 37.7 |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here