Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgment: The author and editors wish to acknowledge and thank John K. Stanley, MD, who contributed this chapter for the sixth edition. This work is built on his foundation as well as the seventh edition.
A pain-free, stable wrist joint is essential for normal function of the hand. Pain arising from a traumatized, arthritic, or unstable wrist will, through the unconscious spinal reflex, inhibit the function of the forearm musculature and result in weakness. Intermittent pain and instability result in an unreliable grasp that can fail capriciously and without warning. In addition to pain and instability, the problems of restricted range of motion and deformity may be added, which may have an adverse impact on function.
Primary osteoarthritis of the wrist is a relatively uncommon cause of wrist pain and is exemplified by degenerative changes at the scaphotrapeziotrapezoid (STT) joint. More commonly, arthritis ensues after trauma, instability and dislocations, crystalline deposition, or inflammatory processes. Less commonly, etiologies include cerebral palsy, penetrating wounds, hemophilia, infection, avascular necrosis of the carpus, or chondrolysis. On occasion, bone lesions, such as giant cell tumors of the distal radius or synovial chondromatosis of the wrist, can be a source of pain and may require excision and/or wrist reconstruction.
A variety of surgical procedures are available for the management of the painful, unstable, degenerate, or stiff wrist. The choice of treatment depends on the cause and the pattern of the effects of the causative pathology and is dependent on the integrity of the articular cartilage. There are less invasive surgical options that aim to maintain motion, including partial denervation or metaphyseal decompression. The more extensively performed surgical procedures may be grouped into two principal treatment options: (1) partial or total wrist arthrodesis and (2) wrist arthroplasty.
The aim of any treatment is to provide a pain-free, stable, and functional wrist, and each patient will have a pattern of problems that guide the surgeon toward the appropriate treatment for that individual. Some patients cannot tolerate the loss of range of motion engendered by total wrist arthrodesis and will therefore press for a motion-preserving procedure. Therefore, careful assessment of the patient’s needs and requirements must be considered.
Because the normal wrist enjoys considerable range of motion, loss of any of that range of motion is perceived as creating an impairment that may give rise to a disability. However, a number of studies have been performed to examine the requirements for wrist motion for a variety of normal activities, and it is clear that most of the activities of daily living can be performed with quite a restricted range of motion of the wrist.
Palmer and colleagues suggested that the functional range of wrist motion is 30 degrees of extension, 5 degrees of flexion, 15 degrees of ulnar deviation, and 10 degrees of radial deviation; these values were derived from a study in which they evaluated 52 standardized tasks involving activities of daily living and some aspects of work. Brumfield and Champoux found that in performing 15 activities of daily living, 10 degrees of wrist flexion was required and 35 degrees of wrist extension was used. A later study by Ryu et al. evaluated a smaller number of activities of daily living and identified that there was an ideal range of motion that they described as 60 degrees of extension, 54 degrees of flexion, 17 degrees of radial deviation, and 40 degrees of ulnar deviation. They went on to state that the majority of hand placement and range-of-motion tasks that were studied in their project could be accomplished with 70% of maximum range of wrist motion—40 degrees each of wrist flexion and extension and 40 degrees of combined radial and ulnar deviation. Nelson demonstrated with use of a splint to mimic stiffness that 123 activities of daily living could be performed successfully with limited motion consisting of 5 degrees of flexion, 6 degrees of extension, 7 degrees of radial deviation, and 6 degrees of ulnar deviation. This probably represents considerable coping strategies, compensatory motion of the shoulder and elbow, and modification of activity by the individuals in the study. Their study concluded that although good range of motion is of great value, only a small arc of motion in each direction is required to maintain independence of existence. However, life involves a combination of hobbies, pastimes, and work, each of which may require a specific range of motion, and these must be considered when assessing an individual patient for treatment. Franko et al. highlighted the issues surrounding the capacity of volunteers to adapt and compromise to limitations of wrist motion. The authors found severe restriction of wrist motion with the use of splints gave rise to only a modest impairment in function of the wrist in activities of daily living. However, when some motion was allowed, there was a significant improvement in the ease of performance of the same tasks and a significant improvement in the range of tasks that could be performed. This study highlights the general need of patients to have some movement at the wrist but that individual requirements will differ. In addition, Kiran et al. demonstrated that there remains individual variability in important activities such as perineal hygiene, so the assumption that hand use is similar between patients is incorrect. Therefore, when patients seek advice and treatment for a painful, unstable wrist, it is important to identify not only the impairment that is present but also the net effect of that impairment on functional ability. Further, documentation of hand preference with important activities like hygiene will help in planning treatments. This will be unique to each individual patient and will have a great effect on the choice of a surgical procedure. With a good history one can discern the patient’s particular activities that are inhibited by the painful or unstable wrist so that the correct choice of a motion-preserving procedure, such as limited arthrodesis or arthroplasty, or a motion-ablating procedure, such as arthrodesis, can be made. Other factors, such as the patient’s age, ipsilateral shoulder and elbow pathology, and occupation may well factor into the decision-making process with regard to the choice between arthroplasty and arthrodesis. Preoperative assessment of the patient must include a detailed physical examination and a full radiographic analysis to determine bone quality, residual bone stock, and the pattern of the disease. Additional investigations may be needed to identify the underlying pathology, for example, whether the condition is due to an inflammatory or degenerative disease process, as well as identification of any comorbidity that might prejudice the outcome of any surgical procedure. Preoperative assessment should score function, disability, and pain to facilitate measurement of the outcome of the intervention. An important element of the preoperative assessment is an evaluation of the capacity of the patient’s willingness and ability to comply with the appropriate postoperative instructions and the therapy program that accompanies it, and such evaluation is essential to a successful outcome for most surgical procedures involving the wrist.
This process therefore consists of five discrete elements.
Identification of the impairment or loss of faculty. Impairment is defined as the parameters that can be measured and include range of motion, grip strength, deformity, and stability.
Assessment of pain, which by definition is a symptom and therefore no objective measurement can be made. The closest that we can approach assessment of this aspect of the patients’ problem with some degree of reliability is through a visual analog scale, and therefore a visual analog chart of the pain should be scored for pain at rest and pain with activity.
Patient-related outcome measures are an important part of the preoperative assessment. They help the patient (and surgeon) better understand the limitations, guide the treatment plan, and help realize expectations.
Presence of a disability. The effect that pain and the impairment have on an individual is defined as a disability. This identifies the areas of the activities of daily living that are affected and the areas of significant difficulty within patients’ lives that they wish to resolve.
Radiographic assessment to determine the range of surgical procedures that are possible as defined by bone stock and the pattern of degenerative changes.
Examination of the wrist is necessary to establish the baseline values of movement, strength, deformity, and stability. , In addition, visual inspection will allow the examining physician to observe local swelling, scars, evidence of current or previous infection, and the patient’s reaction to movement or provocative stress testing of the joint or joints. The associated physical signs of inflammatory joint disease may well be apparent, including multiarticular involvement, deformity, swelling, and effusion. The presence or absence of scaly patches and nail changes must be sought to rule out psoriasis. A patient with psoriasis must be warned of the Koebner phenomenon, in which acute psoriatic plaques may develop along the length of the scar engendered by the surgery. The presence of vasculitis or active rheumatoid disease may be a contraindication to surgery until the condition is controlled.
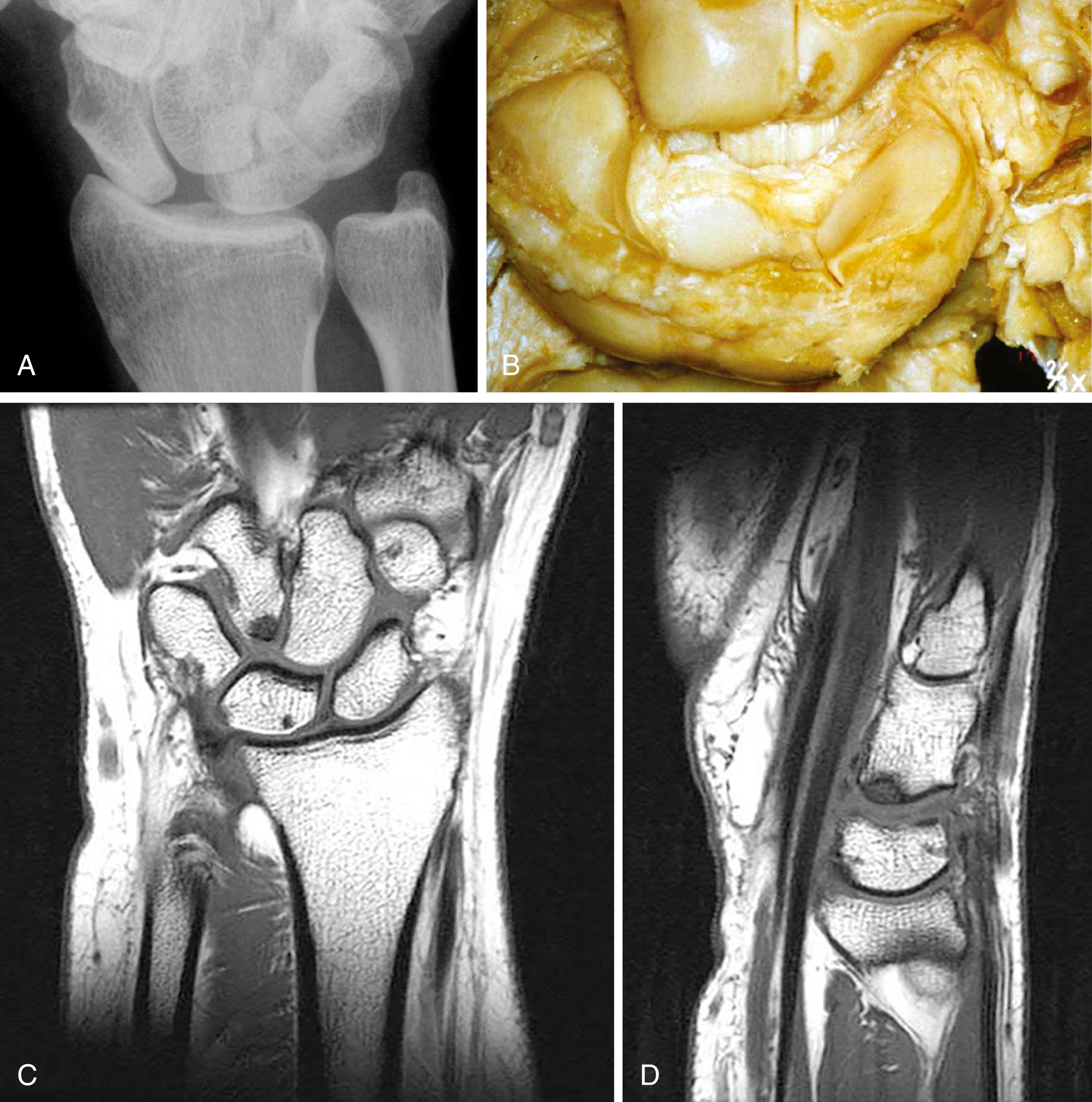
X-rays including standard posteroanterior (PA), oblique, and lateral view should be the basis for the initial radiographic examination. Gross changes can be seen on the standard PA view, performed with the shoulder held at 90 degrees of abduction, the elbow at 90 degrees of flexion, and the hand placed flat on the radiographic plate in neutral rotation. This gives a reproducible PA view in neutral rotation with the beam centered over the capitate and including the distal radioulnar joint (DRUJ). The lateral view should be performed with the 90-degrees flexed elbow at the side, again in neutral rotation. The oblique is done with the wrist in neutral rotation and the arm abducted 45 degrees. Marked changes, as seen in the scapholunate advanced collapse (SLAC) pattern of arthritis, the scaphoid nonunion advanced collapse (SNAC) pattern, and carpal coalitions, are easily identified. STT arthrosis may be associated with deposition of calcium pyrophosphate ( Fig. 12.1A and B), and in this condition the radiolunate joint may well be involved (see Fig. 12.1C ). Less obvious and more difficult to assess is arthrosis between the capitate and the lunate and between the head of the hamate and the lunate. In these circumstances, the so-called six-shot series includes a PA view of the wrist in full radial and full ulnar deviation, which is valuable in identifying elements of instability in patients with scapholunate injury. An anteroposterior (AP) grip view completes the series and can magnify carpal collapse, scapholunate diastasis, and whether there is impingement between the hamate head and the hamate facet on the lunate ( Fig. 12.2 ). The recently described “pencil-grip” PA view profiles both scapholunate joints simultaneously and demonstrates scapholunate diastasis favorably compared with other radiographic stress views.
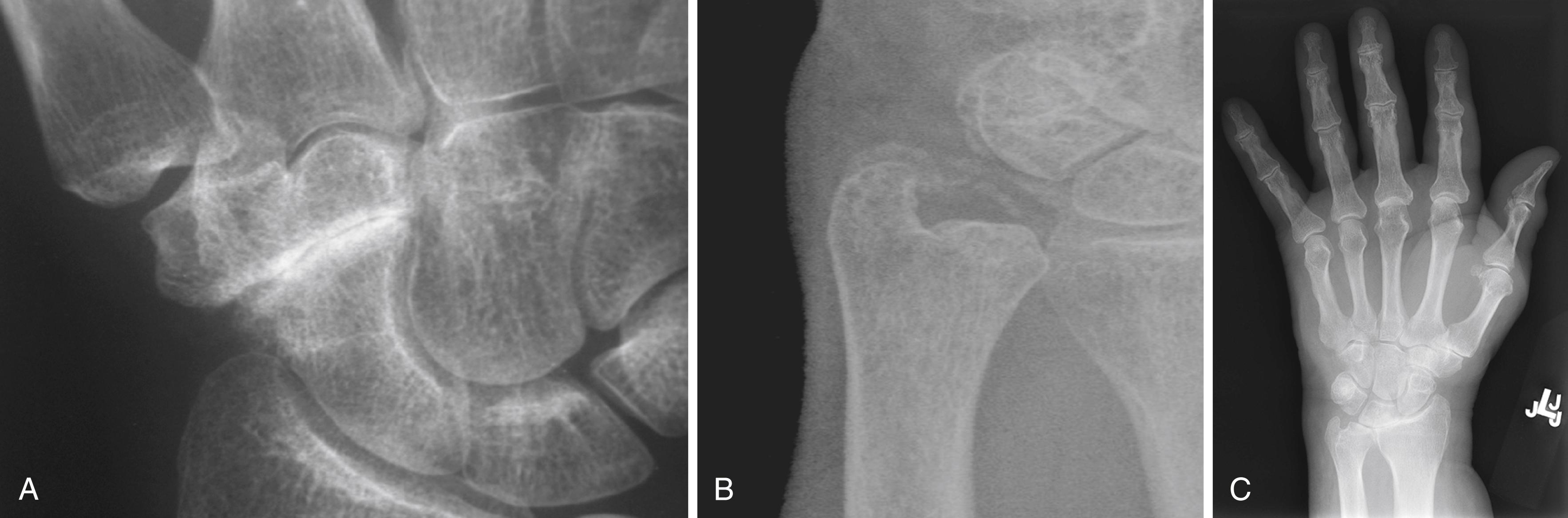
Specific x-rays are indicated by the history and examination and, if indicated, should include, for example, a pisotriquetral skyline view (a lateral view with the wrist in 10 degrees of supination) ( Fig. 12.3A ) to exclude osteoarthritis of this joint, which can coexist with other areas of arthritis in the wrist and, if not identified, can give rise to residual symptoms that may overshadow any improvement after other surgery.

Computed tomography (CT) scans and magnetic resonance imaging (MRI) may also be helpful in better evaluating patients with arthritis. CT scans will better discern the bone quality and joint disease compared with plain films (see Fig. 12.3B and C). MRI will be most helpful in confirming the vascularity of the carpus and identifying bone marrow changes, health of the articular cartilage, and ligamentous integrity. It is also helpful in delineating pathology of the soft tissues such as synovitis and tenosynovitis associated with inflammatory diseases (see Fig. 12.3D ).
In osteoarthritis, a common pattern of the progression of degenerative change has been defined by Watson and Ballet as the SLAC pattern ( Fig. 12.4 ). Similarly Vender et al described the SNAC pattern ( Fig. 12.5 ).
![Fig. 12.4, Scapholunate advanced collapse pattern of arthrosis of the wrist. Localized arthrosis of the scaphoid fossa begins at the styloid tip (stage I), proceeds to the proximal scaphoid fossa (stage II), and is followed by capitolunate arthrosis (stage III). The lunate may fall into dorsiflexion (dorsal intercalated segment instability [DISI]) and the scaphoid into flexion as seen here, but the integrity of the radiolunate articulation is preserved until late in the process. Fig. 12.4, Scapholunate advanced collapse pattern of arthrosis of the wrist. Localized arthrosis of the scaphoid fossa begins at the styloid tip (stage I), proceeds to the proximal scaphoid fossa (stage II), and is followed by capitolunate arthrosis (stage III). The lunate may fall into dorsiflexion (dorsal intercalated segment instability [DISI]) and the scaphoid into flexion as seen here, but the integrity of the radiolunate articulation is preserved until late in the process.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/WristArthrodesisandArthroplasty/3_3s20B9780323697934000122.jpg)

Because the variable picture seen in the inflammatory arthropathies such as rheumatoid arthritis (RA) does not lend itself to either of these classifications, treatment must be individualized. The following Wrightington classification of rheumatoid wrist radiographs may be useful when considering the surgical possibilities based on the pattern of joint damage and residual bone stock.
In general, in the early stages of rheumatoid disease, x-rays may show minor erosions but no significant bone loss or ligament injury and normal joint spaces. In these circumstances, simple synovectomy with disease-modifying drugs, splintage, and other measures may be all that is required ( Fig. 12.6A ).
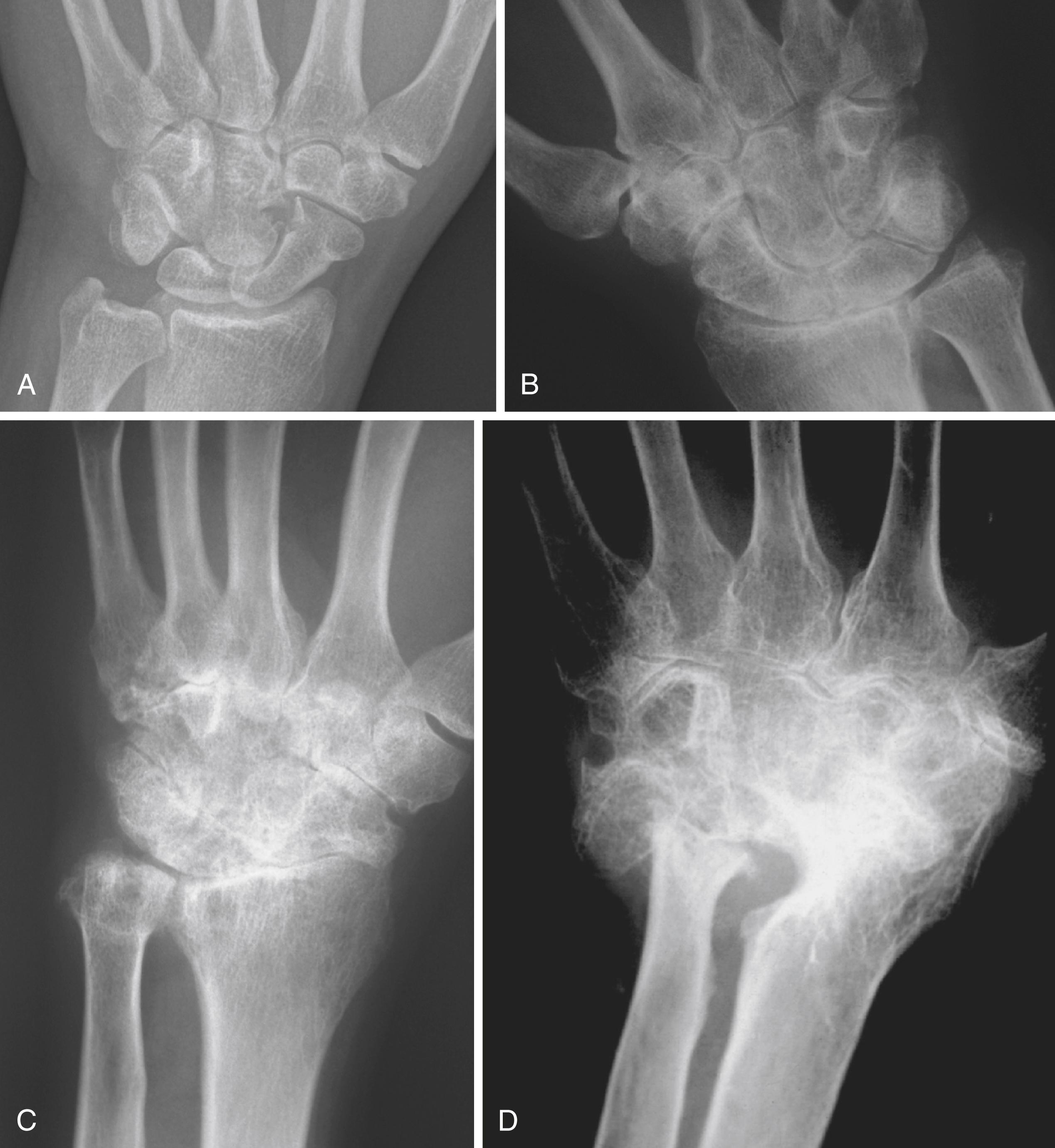
As the disease progresses, localized loss of joint space becomes apparent in the radiocarpal joint (see Fig. 12.6B ). There may be secondary changes consisting of translation and translocation of the carpus. Provided that the midcarpal joint is well preserved, these patients are suitable for radiolunate or radioscapholunate (RSL) fusion.
Progression of the disease can lead to widespread loss of the joint surface, including the midcarpal joint, but if the bone stock is preserved, the surgical choices are total wrist replacement or total wrist arthrodesis (see Fig. 12.6C ).
When the wrist has been so damaged by the disease process that bone stock has been significantly lost, the only surgical procedure that is reasonably reliable is arthrodesis, and this is often the only practical course of action. Particular attention should be paid to the lateral x-ray of the wrist; it may show significant volar subluxation of the lunate, which will give rise to some difficulties in reducing the wrist and could precipitate carpal tunnel syndrome as the wrist is relocated and realigned (see Fig. 12.6D ).
Peterson and Lipscomb, 1967: Intercarpal arthrodesis
Chamay et al., 1983: Radiolunate arthrodesis
Watson and Ballet, 1984: Surgical correction of the SLAC wrist
Pisano et al., 1991: Scaphocapitate (SC) arthrodesis
Minamikawa et al., 1992: The ideal sagittal scaphoid angle for STT and SC arthrodesis
Calandruccio et al., 2000: Lunocapitate fusion with excision of the scaphoid and triquetrum
Much effort has gone into determining the most appropriate intercarpal arthrodesis for a given condition, and there is a wide range of opinion on the best option for particular patterns of disease and the pathology. The choices are laid out in the following three sections (intercarpal arthrodesis, radiocarpal arthrodesis, and total wrist arthrodesis).
SC fusion is considered an alternative to STT fusion for stabilization of the scaphoid. Accordingly, indications include dynamic or rotatory subluxation of the scaphoid (RSS), nonunion of the scaphoid, Kienböck disease, and midcarpal instability. It is particularly advantageous with chronic scaphoid nonunion to address the instability, as well as expand the area of bone healing from distal to proximal scaphoid to capitate.
Most authors believe that there are no significant loading differences between SC and STT fusion. Watson felt that better motion is achieved with STT fusion than with SC fusion. Two cadaveric laboratory studies found essentially no differences in motion between the two. , The authors noted that after both STT and SC fusion there is diminished joint reactive force at the radiolunate and lunocapitate joints. The amount of restriction of motion very much depends on proper reduction of the scaphoid to an intermediate position of flexion with respect to the radius.
Contraindications, as in STT fusion, include any abnormality of the radioscaphoid joint that would be susceptible to increased degeneration and symptoms because of the altered or increased loading through the radioscaphoid joint after SC fusion. Similarly, STT degenerative changes would be a contraindication to SC fusion.
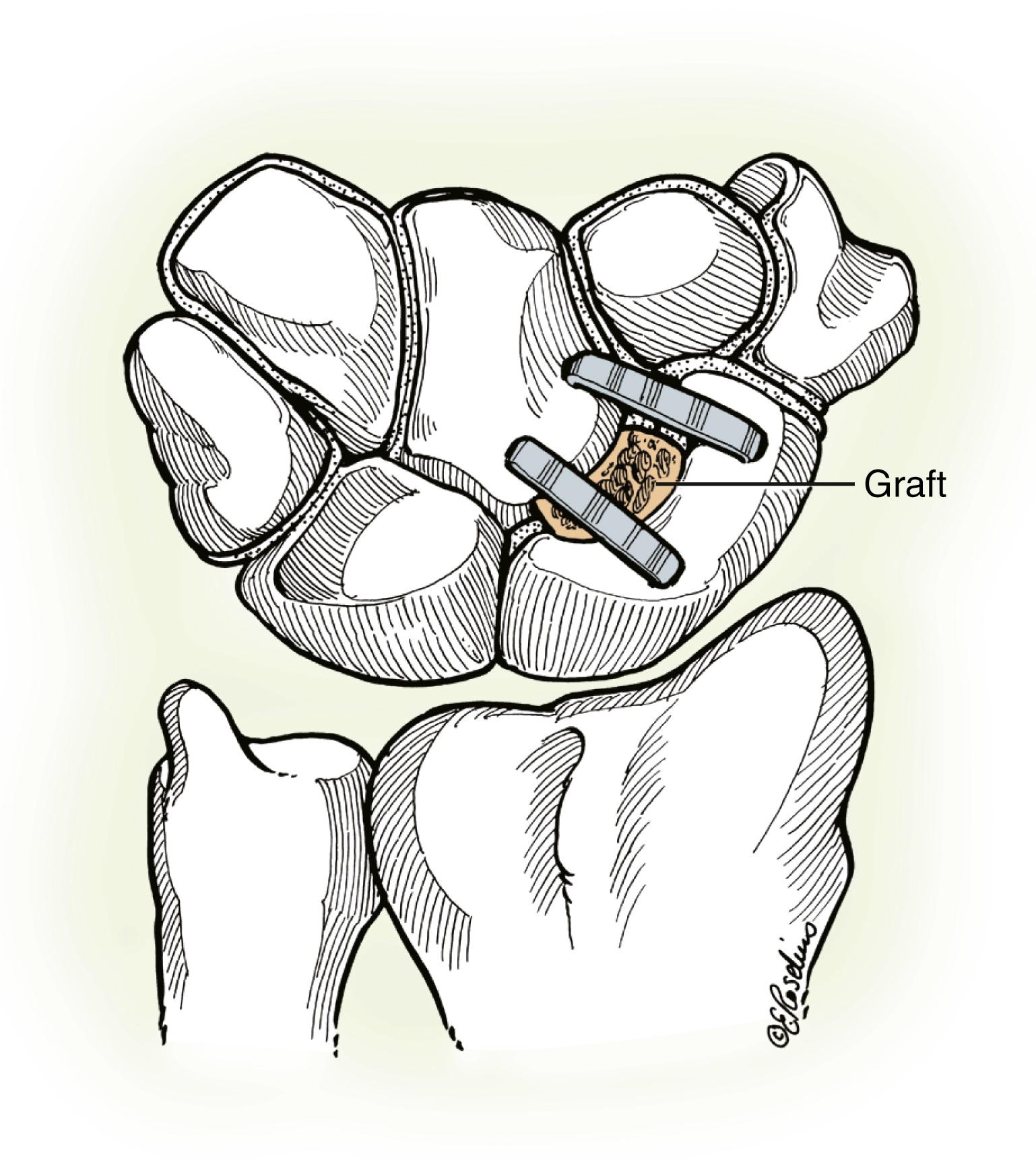
Fixation can be accomplished with Kirschner wires, staples, screws, or plate and screws ( Fig. 12.7 ). Safe hardware insertion requires identification and protection of the radial artery and the dorsal sensory radial nerve branches. Provided that normal intercarpal spacing is maintained by decorticating only the dorsal 75% of the articular surfaces and by packing the resultant space with bone graft, compression screws may be used between the scaphoid and capitate to hold the scaphoid in a 40- to 50-degree radioscaphoid angle.
The wrist is exposed through a longitudinal incision similar to that for a radiolunate fusion from the Lister tubercle to the base of the index metacarpal. The dorsal sensory radial nerve branches are identified and protected. The capsule is incised using a ligament fiber-splitting approach within the fibers of the dorsal radiocarpal and dorsal intercarpal ligaments. When necessary for exposure, this approach can be extended radially along the radiocarpal joint to better expose the radioscaphoid interval. Both the radioscaphoid and lunocapitate joints are inspected for healthy cartilage and protected. I prefer to utilize cannulated compression screws for fixation ( Fig. 12.8 ). These can be placed in a radial to ulnar direction either percutaneously or directly within the exposure of the wound, depending on the visualization and access to the radial side of the scaphoid. Care is taken to ensure that the superficial branches of the radial nerve and dorsal branch of the radial artery are safely protected. The nerve branches can be visualized just deep to the skin and protected from penetration or torsional damage by the guide pins by using a soft tissue sleeve or large metal angiocatheter needle. The artery will be deeper and should be directly visualized to ensure it is safely out of the way. Reduction of a malrotated scaphoid is required. Similarly, if the lunate is tilted dorsally, this angulation must be corrected to ensure normal alignment of the fused capitate. My preference is to not remove the lunate. I feel that the arthrodesis will offload the lunate, diminish Kienböck pain, and reduce the risk of destabilizing the wrist. For reduction, the proximal scaphoid pole is reduced into its fossa while the distal pole is elevated with a 0.062-inch Kirschner wire “joystick,” supplemented as needed with a large skin hook applied around the distal scaphoid. Correct lunocapitate posture can be restored by the application of a palmar-directed load on the capitate until the lunate is restored to its normal tilt.

The guide wires are advanced into the capitate, and reduction to a 40- to 50-degree radioscaphoid angle is confirmed by fluoroscopy with the wrist in neutral alignment. If the wires cannot be correctly positioned within the surgical exposure, they can be placed through a small transverse incision placed just distal to the radial styloid. Care must be taken to protect the dorsoradial artery and superficial branch of the radial nerve. Excessive scaphoid extension will impede radial deviation and extension. The dorsal 80% of the SC joint is then decorticated down to cancellous bone, including the dorsal apposing edges. This can be done with curettes, rongeurs, and/or a high-speed bur. Care is taken to avoid penetration of the lunocapitate joint. Cancellous bone graft is harvested through a cortical window made just proximal to the Lister tubercle and is packed into the fusion space. Upon achieving appropriate reduction of the interval and bony preparation, the guide pins are inserted. Fluoroscopy is used to confirm appropriate position of the proposed fusion and hardware placement. Screw length is measured, and a cannulated drill bit is used to overdrill the pins. I prefer to drill and place a screw in the first, prior to overdrilling the second guide pin. This maintains a point of fixation to resist rotation or loss of reduction. Care must be taken to not overcompress the normal intercarpal spacing with the compression screws. Alternatively, two staples 15 mm wide and 10 or 13 mm deep are inserted by power across the SC joint (see Fig. 12.7 ). The guidewires are removed and the capsule closed with 3-0 braided absorbable suture. The skin is closed with a 4-0 Prolene interrupted skin suture or subcuticular 3-0 monofilament polypropylene, followed by Steri-Strips. The hand and wrist are immobilized with a short-arm bulky dressing and thumb spica splint.
At 10 days, the sutures are removed and a short-arm thumb spica cast is applied. At 6 to 8 weeks, radiographs are checked, and if satisfactory, a short-arm wrist splint is applied for intermittent protection. Active range of motion is initiated. Strengthening is usually deferred until 10 to 12 weeks postoperatively.
Range of motion should approximate 50% to 60% of the opposite side. Sennwald and Ufenast reported a flexion-extension arc of 62 degrees. Viegas and associates reported range of motion 50% of the opposite side. Grip strength will be approximately 80% of the opposite side; Pisano and coworkers reported 74% of the opposite side, while Sennwald and Ufenast documented 83% of the opposite side. Nonunion rates of 6% to 28% can be expected with a 95% confidence interval.
Several studies have demonstrated encouraging outcomes with successful SC arthrodesis. , Iorio et al. reviewed their results in 10 cases of SC fusion for Kienböck disease. All patients healed with significant pain relief. While the wrist’s flexion/extension arc of motion was notably less (53 degrees), it was not significantly diminished compared with historic results of proximal row carpectomy. Another series examining 17 patients with advanced Kienböck disease treated with SC arthrodesis found similar outcomes.
Nonloaded use is allowed at 8 weeks. Full use and any exposure to sudden force should be avoided for at least 10 to 13 weeks after surgery. Patients should not expect strong, relatively symptom-free wrist performance until at least 4 months after surgery.
While some authors have reported excellent pain relief, patients are advised that complete pain relief is not predictable and that they will lose 40% to 50% of wrist motion but should still have a very functional arc. It is possible that they may experience postoperative transient tingling over the dorsoradial aspect of the wrist or hand, which will resolve over time. Although the wrist will never feel “normal,” almost all patients will feel improvement and regain 70% to 80% of grip strength. Patients are strongly advised to discontinue smoking preoperatively. Nonunion can occur in 15% of cases, and patients who smoke have a higher likelihood.
Dynamic or static RSS
Chronic scaphoid nonunion
Kienböck disease
Evaluate scaphoid stability with the scaphoid shift test (see Chapter 13 ).
Obtain a supinated anteroposterior grip radiograph to evaluate the scapholunate joint for increased gap and to be sure that the radioscaphoid and STT joints are free of degenerative changes.
Obtain a lateral radiograph to evaluate the scapholunate angle.
Obtain a hyperpronated anteroposterior radiograph to evaluate the STT joint.
Preserve the volar most cartilage surfaces between the scaphoid and lunate to maintain normal intercarpal spacing.
It is easier to reduce the scaphoid before decortication.
When using a bur, care should be taken to irrigate to avoid overheating the bone and inviting osteonecrosis.
Protect the radial sensory nerve branches and radial artery by using a small drill guide during Kirschner wire placement.
Confirm by fluoroscopy or radiographs proper reduction of the scaphoid to a 40- to 50-degree radioscaphoid angle. If the capitate is properly reduced in the sagittal plane, separate lunate reduction is not required.
Debate remains regarding whether to remove the lunate in patients with Kienböck disease; my preference has been to not remove it. Studies have demonstrated successful pain relief is achieved without excision of the lunate, and my experience has been similar.
Avoid overreduction (extension greater than 50 degrees) of the scaphoid, which will limit motion, particularly radial deviation and extension.
Avoid overcompression of the scaphocapitate interval.
The initial dressing should be bulky and noncompressive to avoid postoperative pain. Apply a short-arm thumb spica splint.
At 10 days, apply a well-molded short-arm thumb spica cast.
At 6 to 8 weeks, check radiographs and initiate active range-of-motion exercises.
Fifty percent to 60% range of motion in comparison to the opposite wrist
Eighty percent grip strength
Fifteen percent nonunion rate
Minimum 3-month recovery time before sports participation
Longer-term studies of outcome have demonstrated rates of progression of radioscaphoid arthritis between 9% and 50%, likely due to increased loading at the radiocarpal joint. , , , However, progression of radio-scaphoid (R-S) arthritis has not proven to be predictably clinically relevant. This would suggest a possible role for prophylactic radial styloidectomy, but this has not routinely been performed in the literature.
The presence of degenerative arthrosis localized to the STT joint is often associated with calcium pyrophosphate deposition disease. Primary osteoarthritis of this joint is not uncommon. Painful radial deviation and pain on gripping and when performing heavier tasks are the usual complaints of patients with STT arthritis. Failure of conservative measures including corticosteroid injection is an indication for surgical intervention. STT arthrodesis (called triscaphe arthrodesis by Watson et al. ) has also been utilized to treat selected cases of dynamic or static RSS, nonunion of the scaphoid, Kienböck disease, , scapholunate dissociation, midcarpal instability, and congenital synchondrosis of the STT joint.
Contraindications primarily include radiographic narrowing or degenerative change of the radioscaphoid joint, which will become increasingly degenerative and symptomatic after the increased load transfer associated with STT fusion. In addition, the presence of trapeziometacarpal (thumb carpometacarpal [CMC]) arthritis would likewise be considered a contraindication.
Preoperative evaluation should include radiography of the STT joint with full ulnar deviation views and full radial deviation views to identify whether the scaphoid moves. If the scaphoid is highly mobile, as characterized by considerable flexion and pronation during radial deviation, an STT fusion condemns patients to painful radioscaphoid subluxation each time they move into radial deviation. In this case one should consider some form of interpositional arthroplasty or excisional arthroplasty rather than arthrodesis. Similarly, if there is substantial gap formation at the STT joint on full ulnar deviation that closes on radial deviation, there may be chronic bone loss involving the distal pole of the scaphoid. These patients have less satisfactory results with arthrodesis and, in the author’s experience, are better served by excision of the distal pole of the scaphoid.
The STT joint is approached through a 6- to 8-cm dorsoradial curvilinear transverse dorsal wrist incision centered over the STT joint just distal to the radial styloid. The dorsal veins and dorsal branches of the superficial radial nerve are preserved. In addition, care must be taken to identify and preserve the dorsoradial artery. The radial styloid is exposed through an incision in the capsule, and the distal 5 mm is removed with a rongeur. A transverse incision in the dorsal capsule is then made, and the radioscaphoid joint is inspected. If significant degenerative disease is identified, the procedure of choice is proximal row carpectomy (if the capitate has a healthy articular surface) or scaphoid excision and four-corner fusion (if both the scaphoid fossa and head of capitate show degenerative wear).
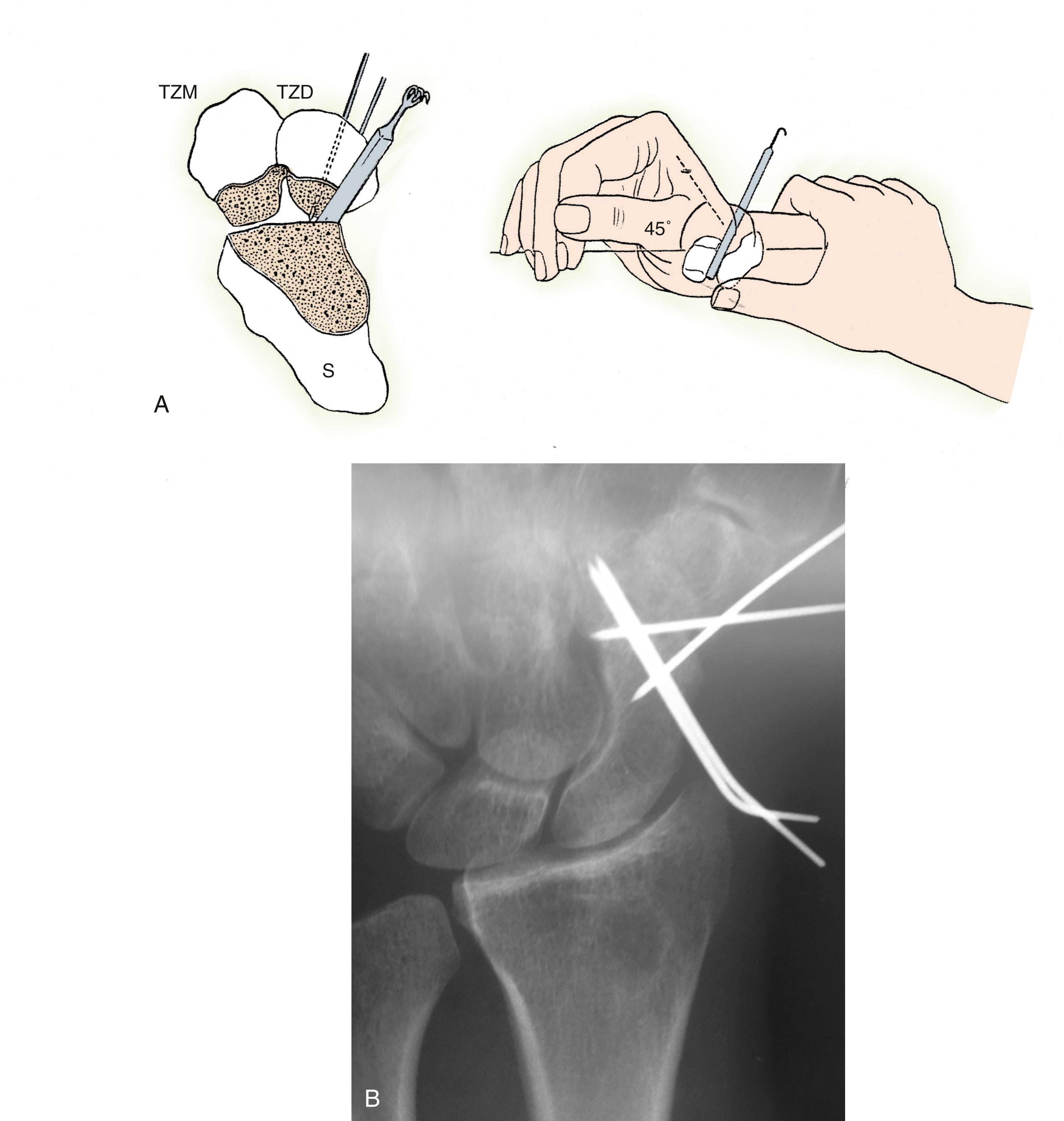
The distal aspect of the extensor retinaculum is then opened along the extensor pollicis longus (EPL) and the STT joint approached through a transverse capsular incision between the extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) tendons. The articular surfaces of the entire scapho-trapezio-trapezoid articulation are then removed with a rongeur down to bleeding cancellous bone. Only the proximal half of the trapezium-trapezoid articulation is removed to retain proper intercarpal spacing. The dorsal cortex of the trapezium and trapezoid is likewise removed to broaden the surface area for fusion. The volar lip of the scaphoid is decorticated by inserting a dental rongeur deep into the joint and levering the handle distally. Cancellous bone graft is then harvested from the distal radius at the Lister tubercle. Two 0.045-inch Kirschner wires are driven percutaneously from the distal aspect of the dorsal trapezoid proximally into the prepared space without crossing it. The first, radially positioned Kirschner wire is passed to the point of just touching the surface of the scaphoid. The second, ulnarly positioned Kirschner wire is passed proximally to the point of entering the scaphotrapezoid space. The wrist is then placed in full radial deviation and 45 degrees of dorsiflexion while the scaphoid tuberosity is reduced by the surgeon’s thumb to prevent overcorrection of the scaphoid ( Fig. 12.9A ). A 5-mm spacer, usually the handle of a small instrument, is placed into the scaphotrapezoid space to maintain the original external dimensions of the STT joint, and the radial Kirschner wire is driven into the scaphoid while avoiding the radioscaphoid joint. The spacer is then removed, and the ulnar Kirschner wire is similarly driven into the scaphoid (see Fig. 12.9B ). After pinning, the scaphoid should lie at approximately 55 degrees of flexion relative to the long axis of the radius when seen from the lateral view. This ensures optimal radioscaphoid congruity and maximizes postoperative range of motion. It is not necessary to correct any abnormal rotation of the lunate. Excessive extension of the scaphoid will limit the motion obtained after surgery. Cancellous bone is then densely packed into the spaces between the scaphoid, trapezium, and trapezoid. The pins are cut beneath the skin level, and the wrist capsule and extensor retinaculum are simply realigned without suturing. The skin incisions are closed with a single-layer subcuticular monofilament suture. The postoperative dressing consists of a bulky noncompressive wrap incorporating a long-arm thumb spica plaster splint. The hand is placed in a protected position with the wrist in slight extension and radial deviation, the forearm neutral, and the elbow at 90 degrees.
The above elbow thumb spica is maintained for the first 2 to 3 weeks postoperative. Following suture removal, a long-arm thumb spica cast is applied for 4 additional weeks. The patient is then converted to a short-arm thumb spica cast for an additional 2 to 3 weeks. Watson recommended casting the metacarpophalangeal (MCP) joints of the index and middle fingers in 80 to 90 degrees of flexion (the so-called Groucho Marx cast), but there is no evidence that this altered the nonunion rate. When radiographic union is seen, the pins are removed in the office and the patient is referred to hand therapy for full wrist mobilization. A splint may occasionally be used for an additional 1 or 2 weeks if there is any doubt about the status of bone healing.
Memory staples can simplify the fixation process and prevent complications related to Kirschner wire irritation and potential infection. After provisional fixation in the appropriate position with Kirschner wires, staples are driven across the scaphotrapezial and scaphotrapezoid joints. The provisional Kirschner wires can then be removed. Postoperative care is as outlined earlier.
Small circular plates, commonly utilized in the management of four-corner fusions, have also been designed for fixation of STT arthrodesis. The bone ends are prepared as in the above-mentioned technique and provisional Kirschner wires can be placed to hold the construct reduced. Most systems utilize reamers to inset the plate into the fusion mass.
The STT joint should be reduced and provisionally held by two guide wires and checked under fluoroscopy. Length is measured and an appropriate-length cannulated screw can be inserted over each wire.
Scaphotrapeziotrapezoid arthrosis
Kienböck disease
Scapholunate instability
Midcarpal instability
Congenital synchondrosis of the STT joint
Position the scaphoid at approximately 55 degrees of flexion.
Partial radial styloidectomy will help reduce loading at the radioscaphoid articulation.
When using a bur, care should be taken to irrigate to avoid overheating the bone and inviting osteonecrosis.
Protect the radial sensory nerve branches and radial artery by using a small drill guide during Kirschner wire placement.
Confirm by fluoroscopy or radiographs proper reduction of the scaphoid to approximately 55 degrees of radioscaphoid angle.
Avoid overcompression of the scaphotrapeziotrapezoid interval.
Time to union may be significant. Burying the Kirschner wires postoperatively can be helpful in minimizing pin irritation or pin track infections, thus minimizing the need for early pin removal.
The initial dressing should be bulky and noncompressive to avoid postoperative pain. Apply a long-arm thumb spica splint. Unlike Watson, we have not routinely included the index and long fingers in initial cast.
At 14 days postoperatively, another long-arm cast is applied.
At 4 to 6 weeks postoperatively, the patient will graduate to a short-arm cast.
Fifty percent to 60% to 80% range of motion in comparison to the opposite wrist
Eighty percent grip strength
While some have reported nonunion as rare, most surgeons agree that the nonunion rate is at least 20% and some notably higher.
Likely full use allowed at 4 months postoperatively
Full recovery will take 9 to 12 months.
Watson has reported excellent functional results and pain-free, stable wrists after STT arthrodesis. In a review of over 800 STT fusions, the average range of motion is usually 70% to 80% that of the contralateral normal wrist, and grip strength has averaged 70% to 90% that of the unaffected wrist. Long-term radiographic follow-up has revealed only rare instances of progressive radioscaphoid or intercarpal degenerative changes. However, Rogers and Watson described, more commonly, painful radial styloid-scaphoid impingement and thus concluded that styloidectomy is thus an important element of the procedure. The nonunion rate is greater than 20% ( Fig. 12.10 ). Loss of wrist range of motion is unpredictable. Recovery takes 9 to 12 months, and pain relief may not be complete.

Few authors report as successful results as have Watson and colleagues following STT arthrodesis. Kleinman and Carroll reported a 52% complication rate in 47 wrists monitored for 10 years and highlighted the need for precise positioning of the fused scaphoid.
Scapholunate arthrodesis is considered by many to be the ideal solution to scapholunate dissociation, and many recent techniques to “reassociate” the scaphoid and lunate after scapholunate ligament rupture (reduction-association of the scapholunate [RASL], “box” tendon graft reconstructions, “axis” techniques) have enjoyed considerable success by linking the two bones (see Chapter 13 ). However, because motion of the scaphoid varies from individual to individual, the results of scapholunate arthrodesis are unpredictable. In the hypermobile group of patients, the scaphoid will pronate and flex considerably with a small amount of translation. At the other extreme, the scaphoid does not flex or pronate in radial deviation. In patients with hypermobile scaphoids, scapholunate arthrodesis is contraindicated. With nonunion rates from 50% to 85%, , this procedure has not proved to be a satisfactory treatment option for scapholunate dissociation and has largely been abandoned.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here