Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Clinical liver transplantation stems from the pioneering work of Professor Thomas Starlz in Denver, Colorado, where he attempted the first human liver transplantation on March 1, 1963. The recipient was a 3-year-old child with biliary atresia, who unfortunately died in the operating room with overwhelming intraabdominal bleeding. A few other attempts followed shortly after, but, in view of dismal results, the transplantation program was stopped and surgeons concentrated on the best strategies to solve the problems that they were encountering. Four years later, on July 23, 1967, the first successful liver transplantation was performed on a 19-month-old girl with liver cancer, who survived over a year. Pediatric liver transplantation, therefore, is positioned at the very birth of the hepatic transplantation surgical specialty, which now has become the standard treatment worldwide for a large range of serious or end-stage liver diseases in adults and children.
At the present time, the need for adult liver transplantation outnumbers greatly the need for pediatric liver transplantation. In the United Kingdom, the ratio between adult and pediatric liver transplants is around 9:1, and data from the National Health Service Blood and Transplant Annual Liver Transplant Report 2018 3 showed that out of 6830 deceased donor first liver-only transplantations done between 2008 and 2018, 6500 (90%) were performed in adult and 669 (10%) in pediatric patients. Importantly, the process of liver transplantation differs between adult and pediatric recipients; in this chapter, we will highlight the most important differences.
At the onset of the development of pediatrics as a specialty, pediatricians were taught to treat the child as a whole entity, and specialties and subspecialties were not encouraged or considered useful. Pediatric gastroenterology started to separate from adult gastroenterology around the 1960s in recognition of the fact that children’s hepatic and gastrointestinal clinical problems had a peculiar nature and complexity. The discovery of metabolic liver diseases, bile acid synthesis defects, cryptogenic neonatal hepatitis syndromes, and the development of the Kasai portoenterostomy procedure for the treatment of biliary atresia, a condition up until then considered untreatable, were all factors that contributed to the foundation of the subspecialty of pediatric hepatology in the 1970s. The first two centers recognized for the diagnosis and management of pediatric liver disease were in Paris, led by Professor Daniel Alagille, and in London, led by Professor Alex Mowat. In the early 1980s, at King’s College Hospital, Mowat introduced the first supraregional tertiary referral center for pediatric hepatology. This rapidly became a world-class clinical and research unit, attracting fellows from all over the world and nurturing the development of similar units worldwide.
Also, in the early 1980s, the advent of new immunosuppression strategies upgraded liver transplantation from an experimental procedure to a therapeutic option. At that time, pediatric liver transplantation was only performed by Starzl in Pittsburgh. Pediatric liver transplantations started in the United Kingdom in 1983 initiated by the collaboration between Calne’s Transplant Unit in Cambridge and Williams’ and Mowat’s Liver Unit at King’s College Hospital in London. This collaboration laid the basis for the standardization of the procedure, indications, and care of pediatric patients.
Indications for liver transplantation in adults and children differ ( Table 2.1 ), and pediatric multidisciplinary teams should be involved throughout the child’s care, from the initial diagnosis and management to the preparation to transplantation when necessary.
| Cause | Pediatric | Adult |
|---|---|---|
| Cholestatic disorders |
|
|
| Metabolic liver disease, with cirrhosis |
|
|
| Metabolic liver disease, without cirrhosis |
|
|
| Chronic hepatitis |
|
|
| Acute liver failure |
|
|
| Liver tumors |
|
|
| Other causes |
|
|
In children, the main indication for liver transplantation is extrahepatic biliary atresia (~ 50% of cases). , Pre-transplantation management includes performing a Kasai portoenterostomy to try to restore biliary drainage from the liver. As a consequence, if children with biliary atresia come to liver transplantation, their abdomen presents adhesions that complicate the procedure and need to be carefully considered in the planning of surgery.
Although usually rare, metabolic liver diseases causing cirrhosis in children (see Table 2.1 ) are frequent indications for pediatric liver transplantation. In addition, there is a subgroup of noncirrhotic metabolic diseases that cause serious systemic problems, corrected by the grafting of a normal liver (see Chapter 40 ). Pediatric metabolic physicians are an essential part of the multidisciplinary medical team aiming at optimizing the patients’ therapeutic pathway, which might lead to liver transplantation or to defining a contraindication for this procedure. The possibility of using auxiliary liver transplantation to correct the metabolic defect in these noncirrhotic conditions underscores an important aspect of the different approaches to pediatric liver transplantation when compared with their adult counterparts (see Chapters 14 and 47 ).
Primary tumors of the liver (e.g., hepatocellular carcinoma) remain one of the most important indications for adult liver transplantation. Strict criteria are followed in these patients for inclusion on the transplantation waiting list, based on the number and size of the malignant lesions (Milan Criteria) ; such strict criteria limit this surgical option to only a minority of patients at the time of detection. In children, the most common malignant liver disease is hepatoblastoma. The therapeutic approach to its unresectable presentation is almost the opposite of the strategy applied to primary liver malignancies in adults because in hepatoblastoma, transplantation is indicated on the basis of a large tumor size and an anatomy that precludes the possibility of safe and radical resection. This approach has been made possible by very effective chemotherapy. In the modern era, pre– and post–liver transplantation chemotherapy, using the PRETEXT system, has contributed to achieving 70% to 80% survival in these patients. Their survival before the advent of effective chemotherapy and transplantation was as low as 2%.
Another condition in which there are profound differences between the adult and pediatric populations is acute liver failure. Not only the etiology (see Table 2.1 ) but also the indications for liver transplantation differ. In children, acute liver failure is not as clearly defined as in adults, and several possible causes are recognized, not all correctable by liver transplantation. The King’s College Hospital criteria to select patients with acute liver failure for liver transplantation have been used for about 30 years worldwide, despite a relative limited sensitivity. According to these criteria, pediatric age at presentation is deemed to be associated with a worse prognosis. In children, a poor prognosis is predicted by an international normalized ratio greater than 4, severe metabolic acidosis, cardiovascular instability, a rapidly shrinking liver, and the presence of renal failure and encephalopathy; the latter sign, however, is frequently a late event and often difficult to diagnose.
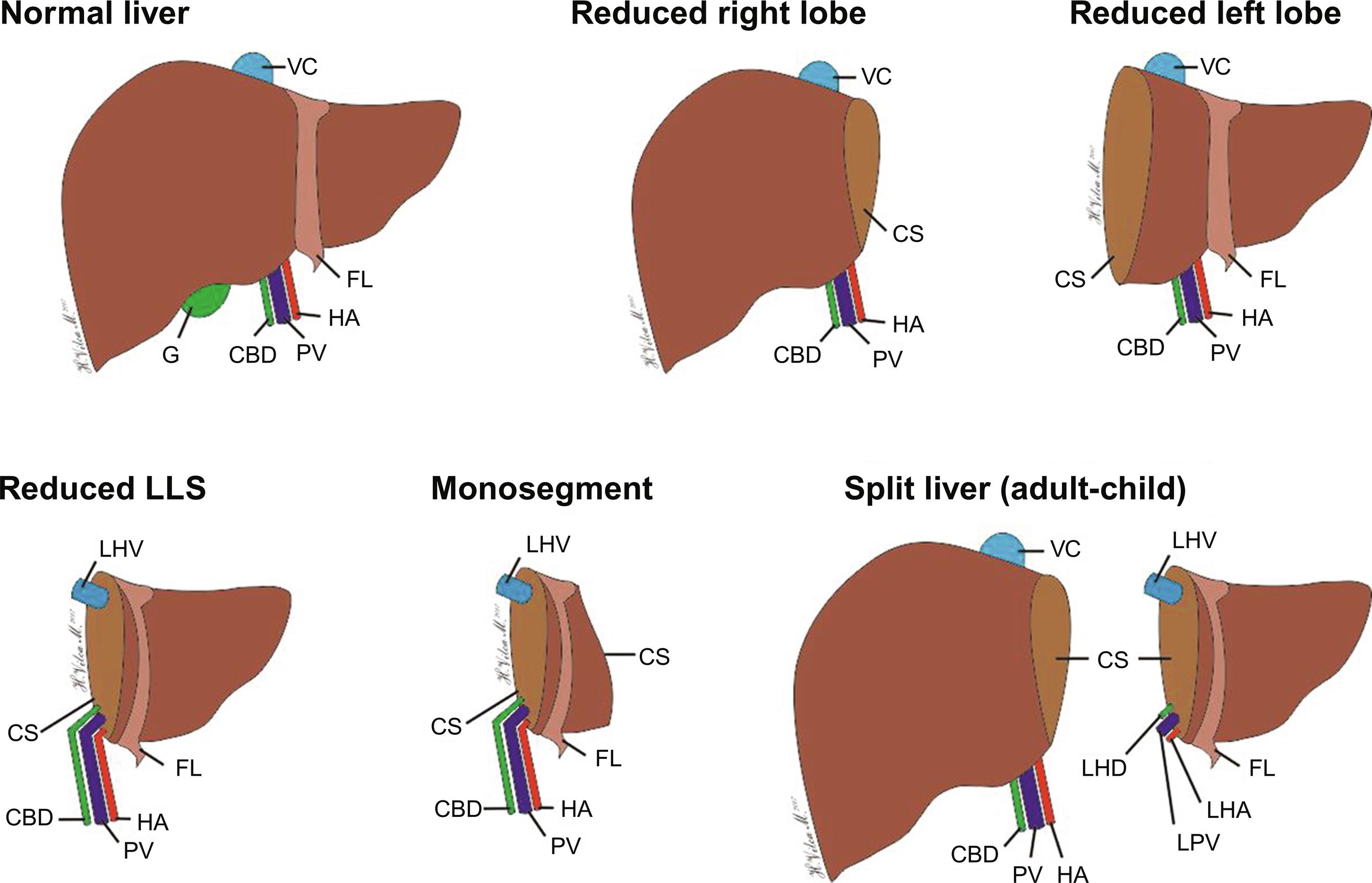
Once the patient has been accepted for liver transplantation, the waiting time for adults and children is one of the most challenging phases of the whole transplantation process. Most of the liver grafts come from cadaveric donors. In the past, a close size match between donor and recipient was deemed necessary, particularly for pediatric recipients, leading to lengthy waiting times and increased mortality on the waiting list. The advent of liver graft reduction techniques and the possibility to divide the liver graft for two patients (split liver transplantation) have reduced the waiting time for children ( Fig. 2.1 ).
A further surgical strategy that has increased the number of liver grafts for children was the introduction of live liver donation, with the donor usually being one of the parents. Today, this procedure has become a routine surgical option in experienced liver transplantation centers. Live donors have been also used for adult-to-adult liver transplantation, despite the potentially increased morbidity and even mortality for the donors.
To date, partial grafts have been used more frequently than size-matched organs in children, considerably decreasing the waiting time. In a recent UK report, the median wait time for pediatric recipients was 80 days versus 134 days for adult recipients; the percentage of living donors was 20% in children and 1% in adults.
The minimum age considered safe for a pediatric liver donor is 1 month, because careful handling of very fragile tissues becomes more challenging as the age of the donor decreases. The surgical procedure for organ retrieval for children should be performed by experienced retrieval teams, using magnifying loupes and perfusing the graft with a cold preservation solution only, through the aorta, followed by portal perfusion of the liver on the bench after hepatectomy. In adult recipients, matching with the donor blood group is very important and affects the waiting time to obtain the right match. In pediatric recipients younger than 1 year, the liver grafts from an incompatible blood group can be safely used in the absence of high titers of anti-A or anti-B antibodies (see Chapter 9 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here