Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vascular malformations are likely the single most misdiagnosed entity in the vascular system. Essentially, vascular malformations are errors in vasculogenesis with the particular characteristics of the lesion determined by the vessel in the vascular system that is involved. As a result, these malformations can include arteries, veins, lymphatic vessels, or capillaries. These lesions occur in about 1.5% of the population and over 90% are present at birth. Venous malformations are the most common vascular anomalies. Although these lesions can have mass effect on adjacent structures, they are not tumors.
An organized, histologically based classification system was initially presented by Mullikan, Glowacki, and colleagues in 1992, and a more recently modified classification system was adopted in 2014 by the International Society for the Study of Vascular Anomalies (ISSVA). The classification system clearly separates tumors (e.g., hemangiomas) from the vascular spaces that characterize a vascular malformation ( Table 25.1 ).
| Vascular Anomalies | ||||
|---|---|---|---|---|
| Vascular Tumors | Vascular Malformations | |||
| Benign | Locally Aggressive | Malignant | Simple | Combined |
| Infantile hemangioma | Kaposiform hemangioendothelioma | Angiosarcoma | Capillary malformation (CM) | CVM, CLM |
| Congenital hemangioma | Retiform hemangioendothelioma | Epithelioid hemangioendothelioma | Lymphatic malformation (LM) | LVM, CLVM |
| Tufted hemangioma | PILA, Dabska tumor | Venous malformation (VM) | CAVM | |
| Spindle-cell hemangioma | Composite hemanigoendothioma | Arteriovenous malformation (AVM) | CLAVM | |
| Epithelioid hemangioma | Kaposi sarcoma | Arteriovenous fistula | ||
| Pyogenic granuloma | ||||
Hemangiomas are childhood masses characterized histologically by high endothelial cell turnover and by cell markers (GLUT-1, merosin, Lewis Y) that are traditionally found only in human placental tissue and that display phasicity characterized by a rapid proliferative phase, plateau phase, and slow involutional phase. The proper nomenclature for these lesions is infantile hemangioma. Infantile hemangiomas are benign vascular tumors that are not usually present at the time of birth but instead become evident within the first 2 to 3 weeks of life. They are the most common, benign tumor of infancy. There is a subgroup of hemangiomas that present fully formed at birth known as congenital hemangiomas. These congenital hemangiomas (as opposed to infantile hemangiomas) do not exhibit the expected accelerated postnatal growth. Some congenital hemangiomas involute quickly over the first year of life and are called rapidly involuting congenital hemangiomas (RICHs), whereas some may persist indefinitely without treatment and are called noninvoluting congenital hemangiomas (NICHs).
The majority of infantile hemangiomas are localized and, although disconcerting to parents and care providers, are nonthreatenting. For these lesions, observation and routine monitoring by the pediatrician or dermatologist are acceptable treatment options. A minority of infantile hemangiomas can, however, cause significant morbidity. These require early recognition, timely referral to a specialist, and prompt intervention to minimize complications. Worrisome presentations include multiple hemangiomas and sensitive locations such as beard distribution, periocular, perioral, nasal tip, large regions of the face and neck, and the lumbosacral spine region. In general, larger hemangiomas located on the face are more likely to require treatment. One of the strongest indications for the use of the laser is the presence of ulceration. Other symptoms necessitating therapeutic intervention include congestive heart failure, airway obstruction, dysphagia, infection, failure to thrive, external auditory canal occlusion, visual axis impairment, and severe facial deformity.
Hemangiomas in adults are not hemangiomas; a hemangioma is a childhood-only birthmark. If a vascular birthmark was not present in the childhood stage, then it is not a hemangioma. Hemangiomas are not arteriovenous malformations (AVMs), and vice versa. Although there is arterial inflow that identifies both these lesions, hemangiomas demonstrate typical tumor vascularity with a central arterial pedicle, and there is fairly minimal, if any, shunting identified in the outflow vessels. An AVM, on the other hand, may have significant venous shunting, with resultant low-resistance arterial inflow and arterialized pulsatility in the venous outflow vessels. Venous enlargement is also common in AVMs, resulting from the pressurized, shunted, arterial flow into the nidus.
Muscular skeletal hemangiomas are not hemangiomas. They are venous malformations that occur in the muscle. With the correct clinical history, a properly performed magnetic resonance imaging (MRI) examination should be almost pathognomonic. Vertebral body hemangiomas are also not hemangiomas; they are venous malformations that occur in bone. Review of the literature demonstrates numerous studies showing “increased vascularity” of these lesions. However, the increased vascularity is from the venous pooling in the lesion and not from arterial hypertrophy and neovascularity. Liver hemangiomas are not hemangiomas; they are venous malformations occurring in the liver.
Vascular malformations are malformed or dysplastic embryologic spaces that are characterized by normal endothelial cell turnover and abnormal vascular anatomy characterized by the dysplastic vessels involved. All vascular malformations can be placed into one of three groups: low flow, high flow, and combined.
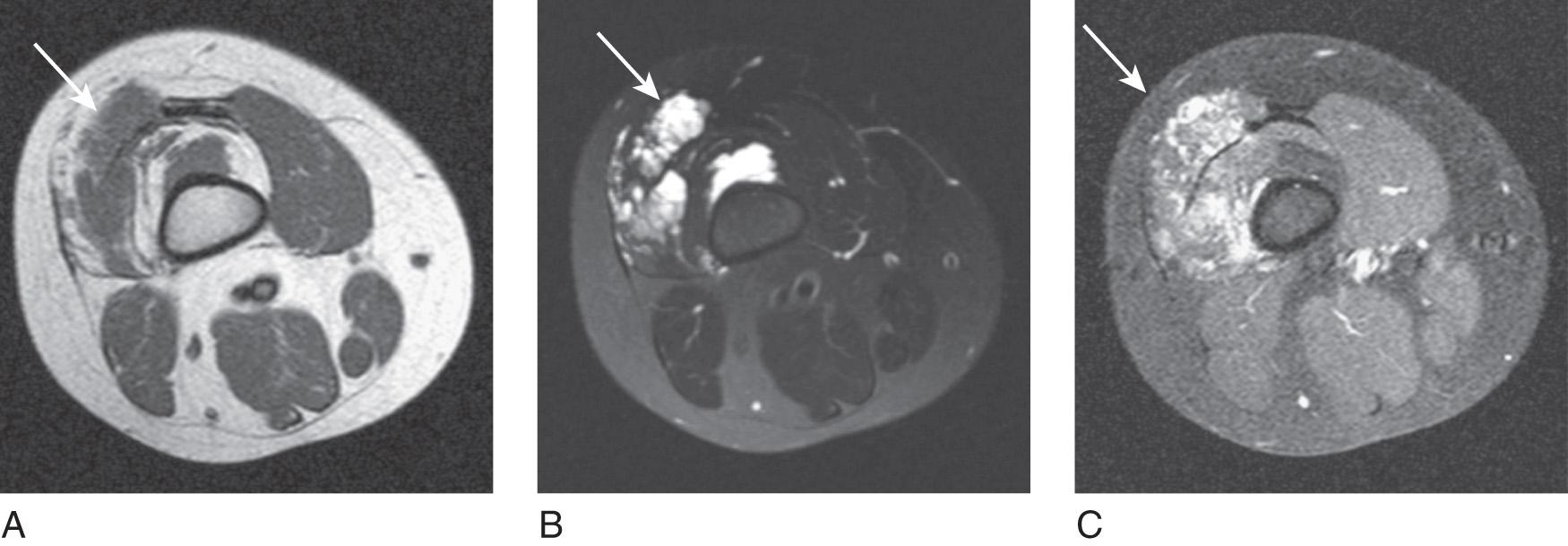
Low-flow venous malformations are the most common form of vascular malformation; simplified, they are a number of tortuous vascular channels. They will be evident at birth and will grow with the child. These are common birthmarks present at birth, although they can be clinically occult if deep in location and usually do not become symptomatic until late childhood/early adolescence. Deep subcutaneous or intramuscular venous malformations often manifest with only local swelling and pain. The diagnosis can be difficult because extremity varicosities may be the only visible sign, especially in deep venous malformations. Superficial venous malformations can be seen with bluish-purple skin discoloration. Venous malformations can be divided into truncal and extratruncal lesions. On physical examination, these lesions are soft and easily compressible and will often demonstrate engorgement, especially when the affected extremity is placed in a dependent position. Extratruncal lesions occur from remnants of primitive vessels early in development and are usually dysplastic and diffusely infiltrative. They commonly involve the deep soft tissue structures, but patients may have constant pain. Truncal venous malformations occur in differentiated and later-stage vascular structures and patients may have an impressive cutaneous manifestation with limb swelling and varicosities. Diffuse malformations involve multiple areas or regions and are usually part of a syndrome such as Klippel-Trenaunay syndrome. Diagnosis of venous malformations can usually be made by clinical examination. However, imaging studies, such as MRI, are performed to evaluate the extent and guide treatment. On MRI, venous malformations are T1 isointense to muscle and T2 hyperintense and demonstrate late enhancement ( Fig. 25.1 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here