Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The oral cavity and oropharyngeal region represent the upper portion of the digestive tract; in addition, the oropharynx constitutes a portion of the upper respiratory tract. The oropharynx and hypopharynx share many of the diseases of the two adjacent digestive tract organs—oral cavity and esophagus—whereas the nasopharynx shares them with the two other components of the upper respiratory tract, that is, the nasal cavity and paranasal sinuses.
For the purposes of the topographic characterization of lesions that occur in this area (particularly squamous cell carcinoma), the oral cavity and oropharyngeal region is divided into the following regions: (1) lip , including only the vermilion surface and comprising an upper and lower lip joined at the commissures of the mouth; (2) floor of the mouth , a U-shaped area bounded by the lower gingiva and the oral tongue; (3) oral tongue , defined as the portion of the tongue anterior to the circumvallate papillae; (4) buccal mucosa , which covers the inner surface of the cheeks and lips; (5) gingiva (alveolar ridge), the mucosa covering the mandible or maxilla from the gingivobuccal gutter to the origin of the mobile mucosa; (6) retromolar trigone , a small triangular surface behind the third molar covering the ascending ramus of the mandible; (7) hard palate , a semilunar area located between the upper alveolar ridge and the mucous membrane covering the palatine process of the maxillary bones; (8) base of the tongue , bound anteriorly by the circumvallate papillae, laterally by the glossotonsillar sulci, and posteriorly by the valleculae; (9) tonsillar area , which includes the anterior and posterior tonsillar pillars and the tonsillar fossa; (10) soft palate ; and (11) pharyngeal walls.
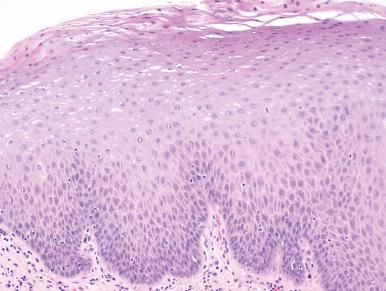
The surface epithelium of this region is of stratified squamous type throughout, with greater depth than the epithelium of the skin. It lacks hair follicles and sweat glands but may contain scattered sebaceous glands, melanocytes, and Merkel cells. It keratinizes in the areas most exposed to mastication (gingivae, hard palate, and dorsum of tongue) but not in others. The lamina propria is composed of loose connective tissue and contains mucous and serous glands of minor salivary gland type. Minor but distinctive variations exist among the various areas of this region.
The oral cavity and oropharynx are the sites of numerous diseases, both congenital and acquired, affecting a large variety of tissues and systems. Only those that occur commonly enough to be of interest to the surgical pathologist are discussed here. For a more thorough discussion of these diseases and the rarer diseases, the reader is referred to specialized textbooks on the subject.
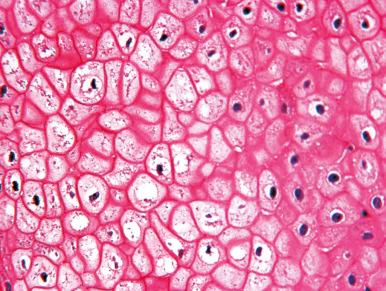
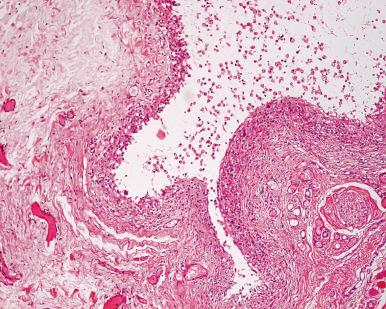
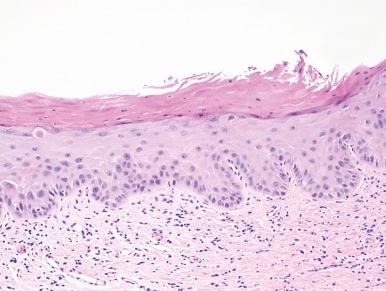
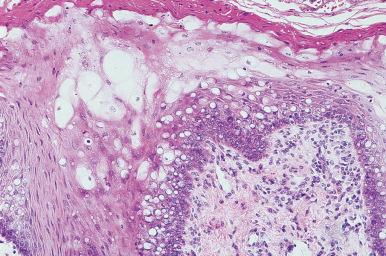
Dermoid cysts are seen in the midline of the floor of the mouth. Although present at birth, they may become evident only later when secondarily inflamed. They are lined by squamous epithelium and contain skin adnexa. Heterotopic gastric or intestinal epithelium has been reported in the tongue and floor of the mouth, sometimes resulting in cystic formations. Minute cysts of odontogenic origin are commonly seen in the alveolar and palatal mucosa of newborns and older infants; they need not be biopsied. Nodules of heterotopic nerve tissue in the palate or parapharyngeal space, mainly composed of glial elements and ependyma-lined clefts, have been reported as glial choristomas ; in rare cases, a neoplasm may arise from them. White sponge nevus, an autosomal dominantly inherited disease, is characterized by large white plaques in the oral mucosa with preferential involvement of the buccal mucosa ( Fig. 4.1 ). Mutations of the keratin 4 or 13 genes, which are expressed in the malpighian layer of the mucosa, is responsible for the clinical and histologic abnormalities. Microscopically there is striking intracellular glycogen accumulation throughout the malpighian layer with overlying parakeratosis ( Fig. 4.2 ). Fordyce granule refers to the presence of normal sebaceous glands inside the oral cavity, a very common occurrence. Sometimes these glands undergo hyperplastic changes and appear as discrete nodules. The entity lingual thyroid is discussed in Chapter 8 .

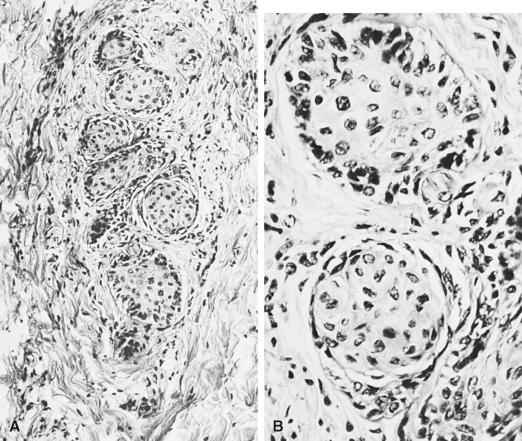
Although it does not represent a congenital anomaly, the occurrence of epithelial nests in intraoral sensory nerve endings should be mentioned here. Their importance relates to the fact that pathologists unaware of their existence might easily confuse them with perineurial invasion by squamous cell carcinoma. These formations are normally occurring neuroepithelial structures of alleged receptor function, known by anatomists as the organ of Chievitz , Chievitz paraparotid organ, and juxtaoral organ ( Fig. 4.3 ). They lie deep to the internal pterygoid muscle near the pterygomandibular raphe and are associated with small branches from the buccal nerve. These structures can undergo nodular hyperplasia.
Chronic inflammatory lesions of nonspecific type are produced in the oral cavity by ill-fitting denture, ragged, sharp teeth, and poor dental hygiene. Removal of the offending agent allows the pathologic process to subside. Microscopically, a combination of hyperplastic epithelium (including pseudoepitheliomatous hyperplasia), fibrous tissue, and inflammatory cells in varying proportions is seen. In a classic article, Bhaskar et al. described 341 such cases, all associated with the use of dentures, under the term inflammatory papillary hyperplasia ; 82.7% of the lesions were located in the palate. Localized overgrowth of the epithelium with or without ulceration is frequent, and it is not rare to see large pseudotumors made up of fibrous tissue and chronic inflammatory cells, among which plasma cells may be prominent. Lesions in which the fibrous proliferation predominates are sometimes referred to, somewhat inaccurately, as irritation fibromas . Scattered stellate and multinucleated giant cells can be seen throughout the fibrous tissue, in which case the term giant cell fibroma has been used.
Geographic tongue (benign migratory glossitis, glossitis migrans) is a relatively common condition (affecting 1%–2% of the population) of unknown cause, which is usually asymptomatic. Most patients are adults, but it has also been seen in children. It often occurs in association with fissured tongue. Clinically, it appears as an erythematous flat zone on the dorsum of the tongue resulting from loss of the filiform papillae ( Fig. 4.4 ). The microscopic appearance is that of a psoriasiform process; there is acanthosis with migration of neutrophils throughout the epithelium to form microabscesses near the surface, accompanied by a mild inflammatory infiltrate in the lamina propria.

Tuberculosis is a rare lesion within the oral cavity. It is usually seen on the tongue as a painful ulcer, but it also may occur on the buccal mucosa. It nearly always is associated with advanced pulmonary disease. Microscopically, there are typical tubercles.
Syphilis may produce a gumma in the tongue or palate appearing as a painless indurated mass. Microscopically, there are granulomas with giant cells, numerous plasma cells, and prominent vascular changes.
Histoplasmosis can occur anywhere in the oral cavity and can closely simulate squamous cell carcinoma on clinical examination. Indurated ulcers, nodular lesions, or verrucous masses can be present. The usual microscopic appearance is that of a granuloma, although sometimes only a nonspecific inflammatory reaction is seen. Special stains (Gomori methenamine silver or periodic acid–Schiff [PAS]–Gridley) are necessary for the identification of the fungi.
Crohn disease can involve the oral cavity and pharynx, sometimes as the initial manifestation. Oral lesions develop in about 6% of patients with Crohn disease at some stage of this disorder. The most common locations are lips, gingiva, vestibular sulci, and buccal mucosa. The lesions can manifest as edema, ulcers, or in the form of a polypoid papulous hyperplastic mucosa. Microscopically, there are edema, dilation of lymph vessels, chronic inflammation, scattered giant cells, and, rarely, noncaseating granulomas.
Sarcoidosis may affect the oral mucosa, gingiva, tongue, hard palate, and major salivary glands. Random biopsy of the lower lip has been successfully used to support a diagnosis of sarcoidosis; in a series of 75 consecutive patients, noncaseating granulomas were found by this procedure in 58%.
Melkersson–Rosenthal syndrome is composed of the triad of orofacial swelling, peripheral facial nerve paralysis, and plicated tongue. Cheilitis granulomatosa is probably an abortive variant of this syndrome, the etiology and pathogenesis of which remain obscure. Microscopically, there is a granulomatous inflammation primarily involving the stroma of the lip ( Fig. 4.5 ). The differential diagnosis includes sarcoidosis and Crohn disease.
Granulomatous tonsillitis is occasionally found in specimens of tonsillectomy performed because of chronic recurrent tonsillar enlargement; in most cases, no specific organism is recovered, and the course is benign.
Waldeyer ring lymphoid hyperplasia is a common symptomatic complication of HIV infection. Characteristically, the process is accompanied by a scattering of multinucleated giant cells adjacent to the tonsillary crypt of surface epithelium. These cells, which harbor significant amounts of HIV, exhibit histiocytic markers and probably belong to the accessory immune system.
Granulomatosis with polyangiitis (Wegener) may manifest in the oral cavity as a red to purple hyperplastic gingiva; in about 5% of the cases this is the first manifestation of the disease. On microscopic examination, there are epithelioid histiocytes, giant cells, eosinophils, pseudoepitheliomatous hyperplasia, and, in rare cases, vasculitis.
Behçet disease affects primarily skin, oral mucosa, and eyes and is characterized microscopically by a leukocytoclastic vasculitis. Cytomegalovirus infection can manifest in the oral cavity as an ulcerated lesion.
Tongue ulceration with eosinophilia (eosinophilic ulcer; ulcerative eosinophilic granuloma; traumatic ulcerative granuloma with stromal eosinophilia [TUGSE], Riga–Fede disease) may mimic carcinoma clinically. Microscopically, it shows a polymorphic inflammatory infiltrate rich in eosinophils, extending into the submucosa, muscle, and minor salivary glands ( Fig. 4.6 ). The initiating event is presumably traumatic (crush injury to the tongue muscle), hence its alternative designation as traumatic (ulcerative) granuloma . Some cases have shown T-cell receptor rearrangement and/or CD30 immunoreactivity, but the clinical behavior is benign.
Chronic graft-versus-host disease (GVHD) frequently involves the oral cavity and presents with xerostomia if the salivary glands are involved as well as with lichen planus-like lesions involving the buccal mucosa and tongue. Histologically, the mucosal lesions demonstrate intracellular edema with basal cell degeneration, scattered dyskeratotic cells, and a lichenoid chronic inflammatory infiltrate.
Pulse granuloma, an odd lesion also known by a variety of synonyms, is discussed in Chapter 5 .
Leukoedema presents as a diffuse opalescent lesion of the cheek mucosa that can extend to the lips; microscopically, the main alteration is vacuolization or intracellular edema of the malpighian cells, a change of a probably degenerative nature.
Diffuse fibrous hyperplasia of the gingiva has been traditionally described as a complication of diphenylhydantoin (Dilantin) therapy, but most cases seen today are genetically inherited, idiopathic, or associated with other drugs, such as cyclosporin A. The gingival thickening can be so extreme as to necessitate surgical removal.
Oral submucosal fibrosis , as seen mainly in Indians and Pakistanis, is a reactive process characterized microscopically by subepithelial fibrosis and chronic inflammation, accompanied by hyalinization and loss of vascularity. The overlying epithelium may be either atrophic or hyperplastic and is often hyperkeratotic. The pathogenesis is unknown. The disease is thought to predispose the patient to the development of squamous cell carcinoma.
Mucous cyst (mucocele) , when applied to a lesion of the oral cavity, has been used for two different processes. The first and more common is referred to as extravasation mucocele and represents a focus of stromal reaction to spillage of mucus from a traumatically injured minor salivary gland. It is often seen in young individuals, the lower lip being the classic location, and the microscopic pattern is that of granulation tissue surrounding one or more spaces containing mucin ( Fig. 4.7 ). Sometimes the cysts are very superficial and simulate vesicobullous diseases clinically.
The second type, named retention mucocele , occurs most often in older patients and in other locations in the oral cavity, such as the floor of the mouth and the inside of the cheek. Microscopically, a mucus-filled cyst completely lined by cylindric, cuboidal, or flattened epithelial cells is seen.
An anatomic variant of either extravasation or retention mucocele is known as ranula when it occurs as a blue-domed cyst in a sublingual location, and as plunging ranula when it extends into the neck above the hyoid bone.
Oral focal mucinosis is the oral counterpart of the more common cutaneous focal mucinosis ; this condition is located in oral cavity sites other than the lip and lacks the granulation tissue wall and inflammatory cells consistently seen in extravasation mucocele.
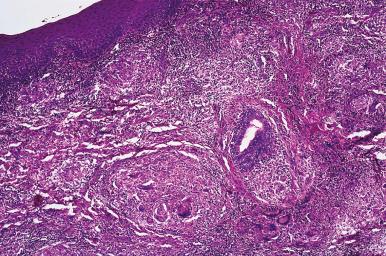
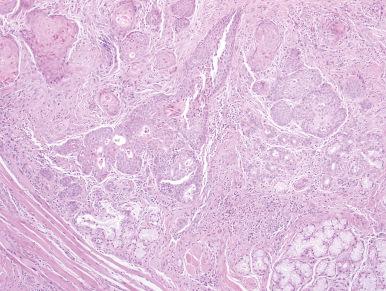
Necrotizing sialometaplasia is a reactive condition involving minor or—less commonly—major salivary glands; its importance lies in the fact that it can be confused histologically with squamous cell or mucoepidermoid carcinoma. The disease usually presents as an ulcerating lesion of the hard palate characterized by vascular proliferation, prominent inflammatory infiltrate, and partial necrosis of salivary glands, associated with regeneration and squamous metaplasia of the adjacent ducts and acini. Cases also have been described in the nasal cavity, gingiva, lip, hypopharynx, and maxillary sinus. The morphologic changes are somewhat similar to those seen in this region after radiation therapy. The pathogenesis is probably ischemic, and some cases have been seen as a complication of vasculitis and other primary vascular disorders. The lobular configuration that these lesions exhibit on low-power examination is an important sign in the differential diagnosis with squamous cell carcinoma ( Fig. 4.8 ). The presence of calponin-positive myoepithelial cells is a supporting diagnostic feature.
Amyloidosis of the tongue may be an isolated event (localized amyloidosis) but is often involved as a manifestation of systemic amyloidosis. Only in a small proportion of cases are the deposits extensive enough to result in clinically evident disease in the form of diffuse macroglossia or a localized tumor. Patients with lingual amyloidosis should be worked up for systemic disease; 15% of those with systemic disease will have underlying multiple myeloma.
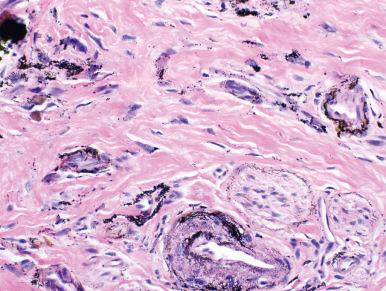
Amalgam tattoos result from amalgam alloys being inadvertently deposited in subepithelial connective tissues of the gingiva, buccal mucosa, and/or alveolar ridge. They appear as blue-black macules ranging from 1 to 20 mm. They are typically biopsied to rule out melanocytic lesions. Histologically, fine golden-brown or black granules are deposited on connective tissue fibers and around vessels and nerves ( Fig. 4.9 ). Larger particles can be seen in foreign body giant cells.
Dermatologic disorders of various types can involve the oral cavity, including lichen planus (but beware of lichenoid dysplasia, see next section), lupus erythematosus , and pemphigus vulgaris .
It has been rightly pointed out that the lesions grouped under this generic term “continue to be among the most widely discussed, reclassified, and semantically tortured conditions in the medical literature.” Part of the problem resides in the fact that different clinical and pathologic terms have been introduced haphazardly over the years and that the correlations between them—although certainly present, as will be shown later—are less than perfect. Among the clinical terms, leukoplakia remains the most widely used. It has been defined as “a white patch or plaque, not less than 5 mm in diameter, that cannot be removed by rubbing and cannot be classified as any other diagnosable disease,” and it implies nothing about the histologic appearance. It is equivalent to the term keratosis as used more often at other sites (such as larynx) and is sometimes subclassified (always on clinical grounds) as homogeneous, nonhomogeneous (speckled; nodular; erythroleukoplakia), erythroplakia (which is red rather than white), and proliferative verrucous leukoplakia. The most common location of leukoplakia, as defined previously, are the buccal gingival gutter and tongue.
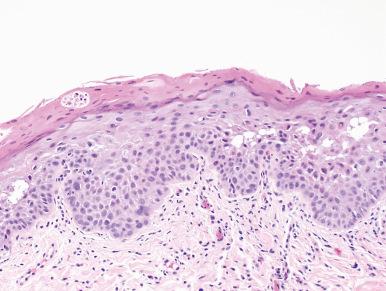
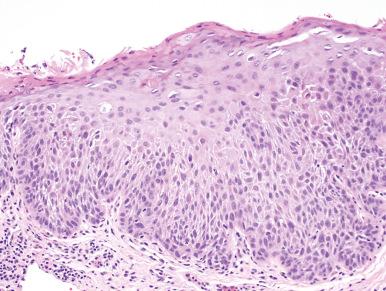
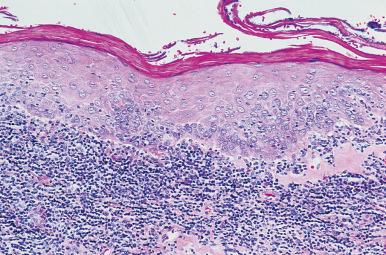
At the histopathologic level, terms such as keratosis, squamous hyperplasia, and verrucous hyperplasia have been used interchangeably, the choice depending on minor architectural differences but mainly on personal preference. When dysplasia is present, this is added to the diagnosis and the changes are graded as mild , moderate , and severe , the latter merging with squamous cell carcinoma in situ (CIS) and therefore often grouped with it, as it is at other sites ( Figs. 4.10–4.13 ). The microscopic criteria for the diagnosis of severe dysplasia/CIS are the same as for other mucosal membranes: epithelial disarray with full-thickness atypia, no flattening or horizontal elongation of the surface layer, and a basement membrane that appears intact in routinely stained sections.
The atypical proliferative changes characteristically involve the surface epithelium, but they can also extend to the ducts of minor salivary glands. When the dysplastic changes are accompanied by hyperkeratosis, prominent granular layer, irregular basal layer, sawtoothed rete pegs, and bandlike lymphocytic infiltrate, the condition is referred to as lichenoid dysplasia ( Fig. 4.14 ). Because of the often subtle degree of the dysplastic changes, this condition is frequently underdiagnosed as lichen planus, a mistake that may have serious consequences.
The alternative terminology that has been proposed for this group of lesions is that of oral intraepithelial neoplasia ( OIN ), grade I (equivalent to mild dysplasia), grade II (equivalent to moderate dysplasia), and grade III (equivalent to severe dysplasia/CIS). Until the latter terminology is widely adopted (and there is no sign that it will happen soon), our preference is to use keratosis as the generic term, to qualify it if indicated and—most importantly—to indicate the presence and degree of dysplasia, according to the scheme in Table 4.1 . It should be acknowledged that, no matter what terminology is used, the determination is subjective and marred by a marked degree of interobserver variability.
| GENERIC TERM | QUALIFIERS | DYSPLASIA |
|---|---|---|
| Keratosis | Papillary | Absent |
| Lichenoid | Mild | |
| Verrucous | Moderate | |
| Proliferative verrucous | Severe/CIS | |
Examples:
|
||
At the immunohistochemical level, the main distinction between keratosis without and with dysplasia is a quantitative one: whereas in the former the expressions of keratin 19, p53, and proliferation-related antigens (such as Ki-67) are all limited to the basal layer, in the latter they are also expressed in suprabasal cells. A similar distinction is appreciated with p16 INK4A , the protein product of a tumor suppressor gene. Of these markers, Ki-67 (MIB-1) seems the most consistent and therefore the most useful for the identification and grading of the dysplasia. DNA ploidy studies have shown that about one-third of “leukoplakic” lesions are hyperploid or aneuploid but that the relationship of this parameter with the grade of dysplasia is poor. Overexpression of p53 has been found in only a small minority of dysplasias, in keeping with the known late occurrence of this event in the carcinogenesis chain. In summary, no immunohistochemical marker, or set of markers, is adequate in making a diagnosis of dysplasia or grading dysplasia but, in conjunction with the morphology, can be useful as an adjunctive measure in making these distinctions.
In terms of clinicopathologic correlations, severe dysplastic changes are much more likely to be present in lesions with the clinical appearance of erythroplakia than those of homogeneous leukoplakia, with erythroleukoplakia occupying an intermediate position. Thus, of 158 “early” asymptomatic squamous cell carcinomas studied by Mashberg et al., 143 (90.5%) had red velvety (“erythroplastic”) components, whereas only 10 (9.8%) had white components; only four lesions were solely white, and there was no color distinction between in situ and invasive carcinoma. The presence of induration almost guaranteed the presence of stromal invasion.
There is also a correlation between the location of the leukoplakia and the chance of finding dysplastic changes microscopically; the probability of dysplasia is much higher for lesions located in the floor of the mouth.
The most important issue concerning this group of lesions is the likelihood of them evolving into invasive carcinomas of either squamous or verrucous type. There is no question that this prediction is more accurate when made on the basis of the severity of the dysplasia as judged microscopically than when attempted on the basis of clinical features. If all cases fitting the clinical definition of leukoplakia are included, the incidence of subsequent malignancy is very low. Pindborg et al. followed 248 patients with oral leukoplakia (mostly of the speckled type) for 1–10 years and found that only 4.4% developed squamous cell carcinoma. In Einhorn and Wersäll's series of 782 patients with a mean follow-up of 11.7 years, the incidence of invasive carcinoma was 2.4% after 10 years and 4% after 20 years. Most other series quote figures ranging from less than 1% to 6%.
From a microscopic standpoint, the implicit assumption is that the greater the atypia, the higher the premalignant potential. It is, however, important to remember that some squamous cell carcinomas of the mouth present without any evidence of adjacent or preceding dysplasia and that a lesion with the features of severe dysplasia/CIS may simply be the peripheral expression of an invasive carcinoma that has not been properly sampled.
There is hope that some special procedure will eventually allow a more accurate and reproducible prediction of the premalignant potential of these lesions.
Actinic cheilitis is the equivalent in the lip vermilion of actinic keratosis of the skin on morphologic, pathogenetic, and behavioral grounds; it should therefore not be equated with the leukoplakic–dysplastic conditions within the oral cavity previously discussed. An increased prevalence of dysplastic and malignant lip lesions has been documented in renal transplant recipients and other immunosuppressed individuals.
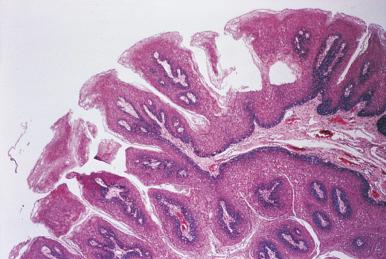
The oral cavity can be the site of a variety of human papilloma virus (HPV)-related lesions, some of which are microscopically and behaviorally analogous to those located in the genital tract. These include focal epithelial hyperplasia (Heck disease), verruca vulgaris , condyloma acuminatum , and the relatively common squamous papilloma ( Fig. 4.15 ).
Heck disease presents clinically as a well-circumscribed, sessile, pale elevation of the buccal mucosa. Microscopically, the most prominent feature is the presence of balloon cells in the malpighian layers. The balloon cells often demonstrate irregular nuclear karyorrhectic degeneration resembling mitotic figures (mitosoid bodies) that are suggestive of the diagnosis. This disorder is more common among Native Americans and Eskimos.
The verrucae, condylomas, and papillomas often exhibit koilocytosis as a sign of cytopathic effect.
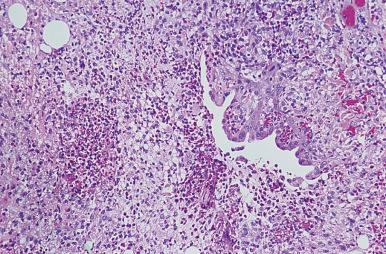
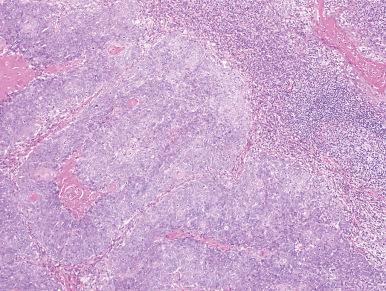
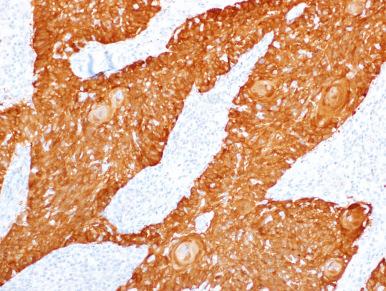
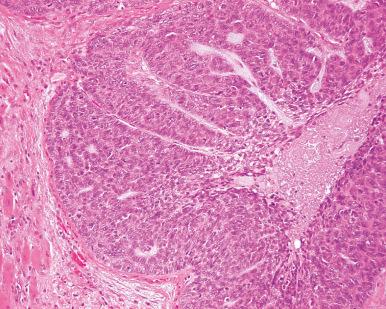
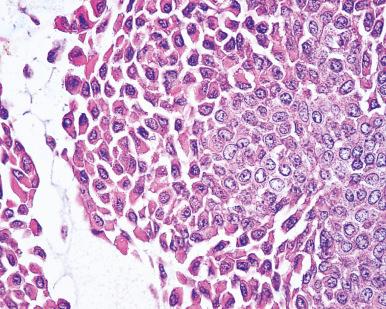
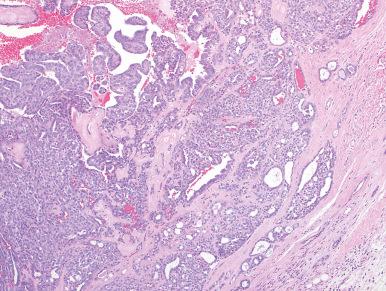
An etiologic role for HPV has also been suggested for verrucous carcinoma and squamous cell carcinoma, including some of its precursors (high-grade dysplasia/CIS) and variants, but these are inconsistent findings. The benign oral lesions are statistically associated with HPV types 2, 4, 6, 11, 13, and 32, and the malignant ones with HPV types 16, 18, and 33. Among the carcinomas, those with the highest incidence of HPV detection are the poorly differentiated nonkeratinizing squamous cell carcinomas of the oropharynx (palatine and lingual tonsil) seen in sexually active young individuals ( Fig. 4.16 ). Parenthetically, many of the latter tumors express p16 protein, a surrogate marker for high-risk HPV infection ( Fig. 4.17 ). HPV-positive oropharyngeal cancers are also more likely to exhibit a “basaloid” morphology and to have cystic lymph node metastasis. It is important to recognize these cancers as they are associated with a favorable response to chemoradiation therapy and are associated with a much improved survival compared with conventional squamous cell carcinoma of the head and neck.
Not all squamous papillomas of the oral cavity are virally induced. Some may be the result of mechanical irritation, and others (although possibly viral related) are genetically determined, such as those occurring as a component of Cowden syndrome.
Hairy leukoplakia was originally thought to be associated with HPV but is now believed to be due to Epstein–Barr virus (EBV) lytic infection. This lesion develops in patients with HIV infection and is characteristically located along the lateral edges of the tongue. Microscopically, it shows parakeratosis, acanthosis, and intranuclear inclusions in keratinocytes, associated with ballooned or ground-glass cytoplasm ( Fig. 4.18 ). There is a high incidence of superinfection by Candida organisms.
Practically speaking, cancer of the oral cavity mucosa is synonymous with squamous cell (epidermoid) carcinoma. Known predisposing factors vary according to the location of the tumor. Most carcinomas of the oral cavity are strongly associated with tobacco use, and there is a synergistic effect with alcohol. For carcinoma of the lip, they include sunlight, fair complexion, and—to less extent—smoking and mechanical irritation. Transplant recipients and HIV-positive patients are also at an increased risk, presumably as a result of immunosuppression. This risk is greater among younger patients. Interestingly, carcinomas developing in HIV-positive individuals are only infrequently associated with HPV infection.
Oropharyngeal carcinomas have been related mainly to tobacco and alcohol, but also to syphilis, oral sepsis, iron deficiency, oral candidiasis, and Fanconi anemia. Currently, most oropharyngeal squamous cell carcinomas are now known to be related to infection with high-risk HPV. Most cases occur in men over the age of 50, although the relative incidence among women and younger patients seems to be increasing.
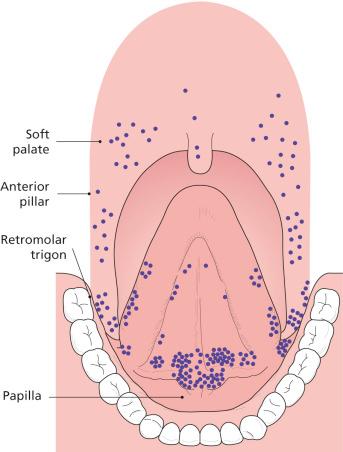
In a large series from the M.D. Anderson Cancer Center in Houston, Texas, the location of squamous cell carcinomas within the oral cavity was listed as follows: lip, 45%; tongue, 16%; floor of mouth, 12%; buccal mucosa, 10%; lower gingiva, 12%; and upper gingiva and hard palate, 5%. Of the lip tumors, over 90% involved the lower lip. In a careful study of early asymptomatic squamous cell carcinomas of the oral cavity proper, Mashberg and Meyers found that the overwhelming majority of them occurred in three locations: floor of the mouth (especially at the papilla at the Wharton duct exit), soft palate–anterior pillar–retromolar complex, and ventrolateral aspect of the mobile portion of the tongue ( Fig. 4.19 ). These “high-risk areas” have in common a lining of thin nonkeratinized squamous epithelium, with short or absent rete ridges and a narrow lamina propria.
Multiplicity of tumors is common; in such cases, the tongue is one of the most commonly affected sites. Patients with carcinoma of the oral cavity have a 100-fold probability of developing a second primary tumor in the region. The chances of this occurrence are particularly high when the carcinoma is associated with dysplastic changes elsewhere in the oral cavity, which are the morphologic indicators of the important biologic phenomenon known as field cancerization .
The analysis of the karyotype and pattern of TP53 mutation in these multiple tumors has shown that in some cases they are clonally related (taken to indicate that they represent metastases from a single lesion), whereas others—probably the majority—are truly multiple primary tumors.
Intraoral squamous cell carcinomas range widely in their degree of differentiation. Histologic evidence of squamous differentiation is typically manifest as intercellular bridges and/or squamous pearls. Those located at the base of the tongue or in the tonsil tend to be undifferentiated and solid with less prominent evidence of keratinization, thereby creating diagnostic confusions with large cell malignant lymphoma. Perineurial and vascular invasion are common. The epithelium adjacent to the invasive tumor often shows dysplastic changes of various degrees, all the way to CIS. Some variations in the microscopic appearance of this tumor exist. A few squamous cell carcinomas are massively infiltrated with mature eosinophils, a feature that may create diagnostic difficulties and that is said to be associated with an improved prognosis.
Immunohistochemically, these tumors are invariably positive for keratin. In the study by Suo et al., all cases expressed CK8 and 19, most expressed 5/6 and 13 (the latter only in the metastases), and none expressed CK20.
For the special features of the tonsillar tumors associated with cystic metastases in cervical lymph nodes, see under “ Spread and Metastases . ”
The most common oncogene alterations identified in oral squamous cell carcinoma involve p16 (approximately 80% of the cases), p53 (50%, with mutation being more common in smokers), cyclin D1 (30%), p63 (30%), phosphatase and tensin homolog (PTEN) (10%), Rb (<10%), and epidermal growth factor receptor (EGFR, <10%). The critically altered pathways include p53 (inactivation by mutation, HPV-16 E6 protein inhibition, or aberrations of other genes in the pathway), EGFR (frequent overexpression through gene amplification, transcriptional activation or mutation in ligand-binding domain), signal transducer and activator of transcription 3 (STAT3) and vascular endothelial growth factor receptor (VEGFR). There are ongoing clinical trials on the usefulness of drugs that specifically target these pathways, such as EGFR inhibitor and VEGF or VEGFR inhibitor.
Evaluation of these changes has led to the proposal of a model of molecular progression, which is conceptually appealing but which should be viewed only as a working hypothesis.
Gene expression profiling studies have identified transcriptional signatures in oral squamous cell carcinomas that are said to predict the overall survival, recurrence-free survival, and likelihood of lymph node metastasis.
Dentists have the best opportunity to discover early lesions of the oral cavity, especially those in “hidden” sites such as the posterolateral tongue. It is their responsibility to examine the oral cavity carefully and to refer patients with suspicious lesions for proper evaluation and possible biopsy. The diagnosis is usually obvious in a well-taken sample. A biopsy specimen that is often much more difficult to interpret is the one taken from an abnormal-appearing mucosa sometime after irradiation therapy has been completed for an invasive squamous cell carcinoma. Under these circumstances, it is better to refrain from making a diagnosis of carcinoma unless there is definite stromal invasion, because from a cytologic standpoint it is often challenging to distinguish residual CIS from radiation atypia. Generally speaking, it is better to wait a minimum of 4–8 weeks after completion of the therapy before taking a new biopsy.
Fine-needle aspiration is a very convenient and efficient way to confirm the presence of cervical lymph node metastases. As mentioned, p16 immunohistochemistry is helpful in supporting the diagnosis of metastatic oropharyngeal squamous cell carcinoma if positive.
The main role of frozen section in oropharyngeal squamous cell carcinoma is in the evaluation of surgical margins. A good correlation has been found between presence or closeness of the tumor at the margin and the probability of local recurrence and mortality.
The pattern of direct spread of oropharyngeal carcinoma is dictated by the anatomic features of the primary site. Carcinoma of the lip invades adjacent skin, the orbicular muscle, and—when advanced—the buccal mucosa, the adjacent mandible, and the mental nerve. Tumors of the floor of the mouth penetrate early beneath the mucosa into the sublingual gland, into the midline muscles, and extend toward the gingiva and mandible. Tumors of the oral tongue, which usually arise on the lateral surfaces and ventral side, tend to remain localized for long periods but eventually invade the floor of the mouth, mandible, and root of the tongue, resulting in fixation of the organ. Tumors of the buccal mucosa invade the underlying muscles and may eventually penetrate into the skin. Tumors of gingiva extend quickly into the periosteum, the adjacent buccal mucosa, and the floor of mouth. Tumors of the hard palate may spread into the underlying bone, but extension into the maxillary antrum is very rare. Tumors of the retromolar trigone spread to adjacent buccal mucosa, anterior tonsillar pillar, maxilla, pterygomandibular space, medial pterygoid muscle (resulting in trismus), and buccinator muscle.
Invasion of the mandible usually involves the body of the bone, from which it may spread to the ramus; direct invasion of the latter structure may also occur, particularly after radiation therapy. Metastases occur primarily by the lymphatic route, the distribution of lymph node involvement depending on the location of the primary tumor. The more anterior the tumor, the lower the position of the cervical nodal metastasis. Carcinomas of the base of the tongue and oropharynx tend to metastasize to the upper cervical (jugulodigastric; level II) lymph nodes. These metastases are notoriously cystic and frequently present before the identification of the primary carcinoma.
Metastases to the posterior triangle region (level V) are rare; they occur in only 6% of the oropharyngeal tumors and 1% of the oral tumors. Features of the primary tumor associated with the likelihood of nodal metastases in the neck are location (higher for the posterior portion of the tongue and oropharynx, intermediate for the anterior portion of the tongue, and lower for the lip, floor of mouth, cheek mucosa, hard palate, and gingiva), poor microscopic differentiation, and depth of invasion. Lip carcinomas associated with metastases tend to be wide, deep, not well differentiated, and accompanied by an inflammatory and desmoplastic response.
Occasionally, the cervical node metastases from these squamous cell carcinomas undergo cystic degeneration. This, plus the well-differentiated nature of the lesion, may easily lead to a mistaken diagnosis of branchial cyst with malignant transformation (“branchial carcinoma”). The occult primary lesion is often located in the lingual or palatine (faucial) tonsil, and it may take 10 years or more for it to be detected. Another peculiar morphologic pattern that squamous cell carcinoma can exhibit when metastasizing to cervical nodes is that of an extensive foreign body giant cell reaction around clumps of keratin, without viable tumor cells; this is particularly common if the tumor has been previously irradiated.
The two pillars of therapy for oropharyngeal carcinoma are surgery and radiation therapy, used either singly or in combination. For most early stage lesions, the results of irradiation and surgery are very similar, so that the final decision as to which to use often depends on factors such as functional and cosmetic results, the patient's general status, and the physician's bias. Advanced cases are treated by a combination of radiation therapy and chemotherapy. Most other sites are treated with primary surgery for resectable cases with adjuvant radiation therapy with or without concomitant chemotherapy. Patients with unresectable tumors can be treated with radiation or chemoradiation therapy with palliative intent.
The treatment of metastatic squamous cell carcinoma to the cervical lymph nodes without detectable primary is largely dependent on the specific location of the lymphadenopathy.
Listed below are the most important prognostic determinants in carcinomas of the oral cavity.
Location . The overall 5-year survival rates are about 90% for carcinomas of the lower lip; 60% for tumors of the anterior tongue; 40% for tumors of the posterior tongue, floor of mouth, tonsil, gingiva, and hard palate; and 20%–30% for tumors of the soft palate. However, these figures are heavily influenced by, and largely dependent upon, the tumor stage. HPV-related oropharyngeal squamous cell carcinomas are associated with a favorable outcome compared with conventional head and neck squamous cell carcinoma.
Stage . As usual, this parameter is of the utmost significance. Thus, the recurrence-free 5-year survival rates for “mucosal cancer” of this region in a series of over 3000 cases were: stage I, 91.0%; stage II, 77.2%; stage III, 61.2%; stage IVA, 32.4%; stage IVB, 25.3%; stage IVC, 3.6%.
Grade . This parameter has proved to be of independent prognostic value. It has been noted that grading of the deep invasive margins of the tumor provides better prognostic information than grading of the entire tumor.
Depth of invasion . This is an important factor, at least in some locations. This feature is incorporated into the staging systems and often dictates whether a lymph node dissection will be performed, especially for oral cavity carcinomas.
Tumor size . This feature does not correlate closely with clinical outcome, except for the very small tumors.
Tissue eosinophilia . Intense infiltration of the carcinoma by eosinophils is said to be a favorable prognostic factor.
Lymph node involvement . Naturally, presence of lymph node metastases is an important prognostic criterion and, as such, it is a key feature of the staging system. Extracapsular spread (i.e., spread of the metastases beyond the lymph node capsule) is an indicator of a further decrease in survival rates being associated with higher rates of locoregional failure.
High-risk HPV . HPV-16 and -18 positivity in squamous cell carcinomas of the oral cavity and other head and neck sites has been recognized to be a powerful indicator of improved survival. In a recently completed study, it was confirmed that tumor HPV status is a strong and independent prognostic factor for survival among patients with oropharyngeal cancer. This survival advantage is tempered in those individuals who smoke.
P21 gene . Overexpression of this gene (the product of which is the downstream regulatory protein of TP53 ) was found to be an independent indicator of unfavorable prognosis in lingual squamous cell carcinoma.
p16 . Overexpression of p16 was found by Kato et al. to be a favorable prognostic factor in oropharyngeal carcinoma. This is related to the fact that p16 is a surrogate marker for high-risk HPV, a known favorable prognostic factor.
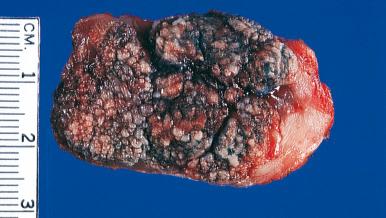
Verrucous carcinoma (Ackerman tumor) is a variant of well-differentiated squamous cell carcinoma endowed with enough clinical, pathologic, and behavioral peculiarities to justify its being regarded as a specific tumor entity. The oral cavity is its classic location, but this lesion also has been reported in the larynx, nasal cavity, esophagus, penis, anorectal region, vulva, vagina, uterine cervix, and skin (particularly in the sole of the foot). Within the oral cavity, the most common sites are the buccal mucosa and lower gingiva. Most patients are elderly males, and there is a close connection with the use of tobacco, especially chewing or snuff dipping. Grossly, it presents as a large, fungating, soft papillary growth that tends to become infected and slowly invades contiguous structures ( Fig. 4.20 ). It may grow through the soft tissues of the cheek, penetrate into the mandible or maxilla, and invade perineurial spaces. Regional lymph node metastases are exceedingly rare and are presumably related to an undetected well-differentiated conventional squamous cell component. Distant metastases have not been reported.
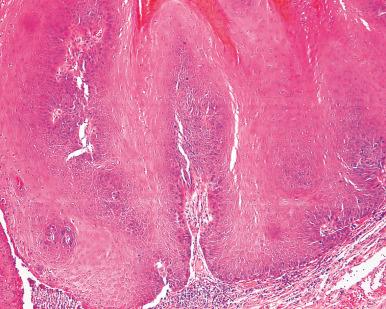
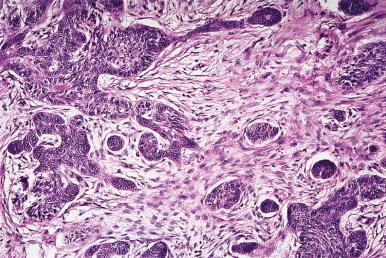
The microscopic diagnosis of verrucous carcinoma may be difficult because of its well-differentiated character. A superficial biopsy will show only hyperkeratosis, acanthosis, and benign-appearing papillomatosis. Sections of an adequate biopsy show swollen, rounded, and voluminous rete pegs that extend into the deeper tissues ( Fig. 4.21 ). Additional features include parakeratin plugs (invaginations) and a band of lymphoplasmacytic inflammation at the advancing front. The most important differential feature with squamous cell carcinoma is the good cytologic differentiation throughout the tumor. Dr. Lauren Ackerman, who first described the entity, used to express this fact by stating: “If a lesion looks cytologically like carcinoma, it is not verrucous carcinoma.” Significantly, in about one-fifth of the cases, cytologically identifiable foci of squamous cell carcinoma occur within a lesion that looks otherwise like a verrucous carcinoma, hence the importance of thorough sampling. These hybrid ( verrucous–squamous ) tumors are said to be associated with a higher recurrence rate than pure verrucous carcinomas.
Resection is the treatment of choice. If surgery is inadequate, the tumor will recur. Radiation therapy is not recommended, since it may alter the nature of the tumor to a highly malignant, rapidly metastasizing, poorly differentiated squamous cell carcinoma. This has occurred in as many as 30% of the cases in some series, the average postirradiation interval being 6 months.
It is likely that most of the cases reported in the past as oral florid papillomatosis represent early and noninvasive stages of verrucous carcinoma. Along the same lines, the similar if not identical conditions known as verrucous hyperplasia , proliferative verrucous leukoplakia , verrucous keratosis , and leukoplakia verrucosa can be regarded as precursor lesions of verrucous carcinoma, from which they are distinguished by the fact that the verrucous process is superficial to the adjacent squamous epithelium.
Carcinomas of surface epithelial origin other than squamous cell carcinoma of either the conventional or verrucous carcinoma types include the following:
Adenoid (pseudoglandular) squamous cell carcinoma . This tumor exhibits a pseudoglandular or alveolar appearance because of acantholysis. Most examples are located in the lip and, like their more common cutaneous counterparts, are associated with, and probably induced by, actinic radiation; however, a few have been seen in the gingiva or tongue, where an actinic pathogenesis cannot be invoked.
Adenosquamous carcinoma . In contrast to the type listed previously, the rare adenosquamous carcinoma shows areas of squamous differentiation admixed with others having true glandular differentiation. Some of these cases may be of minor salivary gland derivation, but they are substantially different from mucoepidermoid carcinomas.
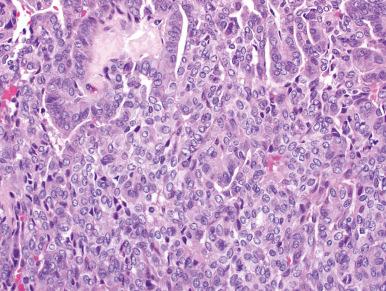
Basaloid squamous cell carcinoma . This is an aggressive variant of squamous cell carcinoma that has a predilection for the upper aerodigestive tract (oral cavity, oropharynx, esophagus, and larynx) but also occurs in other sites such as lung. In basaloid carcinoma, areas with obvious squamous differentiation are admixed with solid tumor islands composed of undifferentiated basaloid cells that exhibit peripheral palisading and a thick basement membrane ( Fig. 4.22 ). Small cystic spaces containing mucoid or hyaline material are present, resulting in a resemblance to adenoid cystic carcinoma. The prominence of basal lamina material is one of the most striking attributes of this tumor at both the ultrastructural and immunohistochemical level. Immunoreactivity for high-molecular-weight keratin (detected with the 34βE12 antibody) and p63 is a consistent feature of this tumor. Occasional examples have a spindle cell component. The differential diagnosis includes minor salivary gland tumors (particularly adenoid cystic carcinoma) and peripheral ameloblastoma.
Adenoid cystic carcinoma shows a lower nuclear grade and exhibits focal glandular differentiation, whereas basaloid squamous cell carcinoma shows squamous differentiation. Both adenoid cystic carcinoma and basaloid squamous cell carcinoma are immunoreactive for 34βE12 and p63.
HPV-16 is detectable in the large majority of oropharyngeal basaloid squamous cell carcinomas, but only in few of those arising in other sites. The absence of HPV-16 in these tumors is associated with a decreased overall survival.
Papillary squamous cell carcinoma. This is an uncommon variant in the oral cavity. It is seen most frequently in the oropharynx and larynx of elderly individuals and shows a frequent association with HPV infection. Papillary squamous cell carcinoma of the oral cavity and oropharynx is associated with a good prognosis.
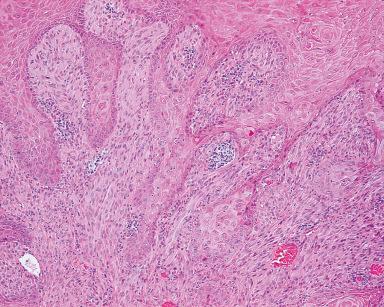
Spindle cell (sarcomatoid) carcinoma . This may appear as an ulcerated and infiltrative mass or as a polypoid growth in the lip, tongue, or other portions of the oral cavity. Sometimes the sarcoma-like formation blends with areas of obvious squamous cell carcinoma or represents the recurrence of what originally was an obvious squamous cell carcinoma ( Fig. 4.23 ). Other tumors are associated with squamous CIS or severe dysplasia. These findings, plus a wealth of electron microscopic, immunohistochemical, and molecular data, indicate that the sarcoma-like component represents a metaplastic change of an originally epithelial neoplasm. Immunostains helpful in the distinction between sarcomatoid carcinoma and sarcoma (in the sense of favoring the former if positive) are keratin 5/6, epithelial membrane antigen (EMA), membranous epithelial cadherin, and nuclear p63. Unfortunately, even a broad panel of epithelial immunohistochemical markers will be negative in a significant percentage of cases.
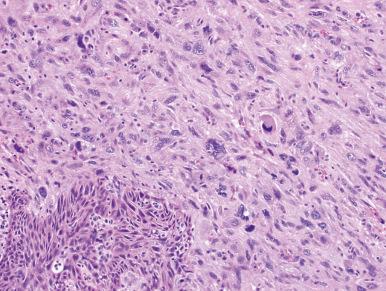
The sarcoma-like component may look like an undifferentiated pleomorphic sarcoma or fibrosarcoma of soft tissue or it may show evidence of specific mesenchymal differentiation, particularly along muscle lines. The nodal and distal metastases of this tumor may be purely carcinomatous, have a mixed appearance as in the primary neoplasm, or, in rare cases, be entirely composed of sarcoma-like elements. The prognosis is closely related to the stage and depth of invasion and is not significantly different from ordinary squamous cell carcinoma of equivalent stage and thickness.
Small cell carcinoma . The appearance is similar to that of the homonymous lung carcinoma. It may be pure or associated with a squamous component and its behavior is very aggressive.
Lymphoepithelioma-like carcinoma . A tumor microscopically similar to the lymphoepithelioma of the nasopharynx and tonsil is occasionally found in the oral cavity or oropharynx.
NUT (midline) carcinoma . This newly recognized type of carcinoma is defined by a molecular genetic alteration, but its diagnosis can be suspected on the basis of its clinicopathologic features. Clinically it affects midlines structures, particularly those in the head and neck areas. Most of the initial reported cases were in children and young adults, but they were subsequently seen in all age groups. The most typical morphologic pattern is represented by foci of undifferentiated carcinoma showing islands of keratinization, with a sharp interphase between the two , accentuated by the immunohistochemical profile (CK8/18 positive in the undifferentiated areas and CK5/6 or p63 positive in the keratinizing areas). Prior to its recognition, this tumor was usually interpreted as sinonasal undifferentiated carcinomas, poorly differentiated squamous cell carcinoma, small cell carcinomas, or the basaloid squamous cell carcinomas.
At the molecular level, the tumor is defined by rearrangement of the NUT gene on chromosome 15q14. The diagnosis is confirmed by documenting nuclear expression of NUT in the nuclei of the undifferentiated cells by immunohistochemistry (with the C52 monoclonal antibody) or by detecting the chromosome translocation BRD4-NUT or one of its variants (such as BRD3-NUT ) by fluorescent in situ hybridization or reverse transcriptase-polymerase chain reaction (RT-PCR). This tumor runs an extremely aggressive clinical course but has been found to respond well to the chemotherapeutic regimen used for Ewing sarcoma/primitive neuroectodermal tumor (PNET).
Minor salivary glands, present in practically all compartments of the oral cavity, participate in many of the diseases affecting their major counterparts, a feature that can be exploited for diagnostic purposes. Thus biopsy of the lower lip has shown involvement of the minor salivary glands in cases of cystic fibrosis and Sjögren syndrome and has also been used to diagnose end-stage chronic GVHD .
Adenomatoid hyperplasia is a term used for a localized hyperplastic process of minor salivary glands appearing clinically as a nodule, usually in the hard palate but occasionally in the retromolar area.
Intraoral minor salivary glands can give rise to a variety of benign and malignant tumors. The hard palate is the most common location, but similar tumors also occur in the soft palate, cheek, tonsil, floor of the mouth, tongue, lip (usually the upper), gingiva, and jaw. It is important to remember that tumors arising in the deep lobe of the parotid gland may present as primary intraoral masses. With a few exceptions, minor salivary gland tumors are morphologically analogous to those located in the major glands ; however, they differ from the latter in their relative incidence and, to some extent, in their natural history.
Pleomorphic adenomas (benign mixed tumor), which constitute over 75% of all parotid neoplasms, make up about half of the salivary gland tumors of the palate but are otherwise similar to major salivary gland pleomorphic adenomas. They may be overdiagnosed as malignant because of increased cellularity, nuclear atypia in the often predominant myoepithelial component (see under “Myoepithelioma”), or pseudoepitheliomatous hyperplasia of the overlying mucosa.
Adenoid cystic carcinoma, mucoepidermoid carcinoma , and polymorphous low-grade adenocarcinoma (see later section) comprise the large majority of intraoral malignant salivary gland tumors, in contrast to the more even distribution of tumor types seen in the parotid gland. Rare cases of acinic cell carcinoma and of epithelial–myoepithelial carcinoma (to be distinguished from pure myoepithelioma, see later ) have also been described. The prognosis of adenoid cystic carcinoma is said to be better when the tumor is located in the palate than when arising in the parotid or submandibular gland, but this may be at least partially due to the inclusion among the palatal tumors of some cases of polymorphous low-grade adenocarcinomas. The prognostic difference among the various morphologic subtypes of this tumor, which has been noted for the major salivary gland, seems to apply also to this location. Of the salivary gland tumors located in the lip, about 80% are benign. Among the malignant types, adenoid cystic carcinoma and mucoepidermoid carcinoma are the most frequent.
Some types of salivary gland tumor occur predominantly or, in some instances, almost exclusively in the minor salivary glands of the oral cavity. They include the following:
Canalicular adenoma . This tumor, characterized by a canalicular pattern of growth ( Fig. 4.24 ), has a predilection for the upper lip, buccal mucosa, and palate (often at the junction between the hard and soft regions), where it is sometimes confused with adenoid cystic carcinoma. In contrast to adenoid cystic carcinoma, canalicular adenomas are diffusely positive for S-100 and demonstrate only focal and weak p63 staining if positive.
Myoepithelioma . This lesion, composed of hyaline or plasmacytoid cells, usually involves the hard palate ( Fig. 4.25 ). The differential diagnosis includes plasmacytoma, oncocytoma, and even skeletal muscle neoplasms. Despite its high cellularity and the occasional presence of atypical hyperchromatic nuclei and intravascular tumor cells, the behavior is generally benign.
Sialadenoma papilliferum . This is a papillary tumor of the oral cavity, usually located in the hard palate or buccal mucosa and characterized microscopically by a biphasic composition. An exophytic mass of well-differentiated squamous epithelium is seen covering a glandular component consisting of cleft-like cystic spaces lined by cuboidal or columnar epithelium; some of these glands may contain oncocytic cells, and others may exhibit squamous metaplasia. The stroma is usually rich in plasma cells. The appearance is reminiscent of both Warthin tumor of the parotid gland and papillary syringocystadenoma of skin, both at the light and electron microscopic level.
Inverted ductal papilloma . This tumor has a pattern of growth similar to that of inverted papilloma of the nasal cavity. It appears clinically as a small submucosal mass in the oral cavity of adults. Microscopically, there are complex invaginations formed by well-differentiated, predominantly squamous epithelium–associated microcysts, occasional mucous cells, and a lining of columnar cells. The behavior is benign.
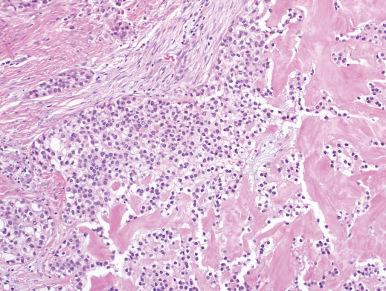
Clear cell carcinoma. This is a low-grade carcinoma that predominantly occurs in intraoral minor salivary glands of adults. The palate is most frequently involved, but all oral sites can be involved such as alveolar ridge, tongue, tonsil, floor of mouth, and buccal mucosa. Microscopically, they are composed of sheets or nodules of large polygonal cells with abundant cytoplasmic glycogen and lacking in atypia or mitotic activity ( Fig. 4.26 ). The stroma can be hyalinized and paucicelluar or composed of a cellular spindled myofibroblastic stroma. The cells are positive for keratin and p63 with variable S-100 staining. They may be associated with recurrence and regional lymph node metastasis, but they rarely metastasize distantly or result in death. Recently these tumors have been shown to have a consistent EWSR1-ATF1 fusion.
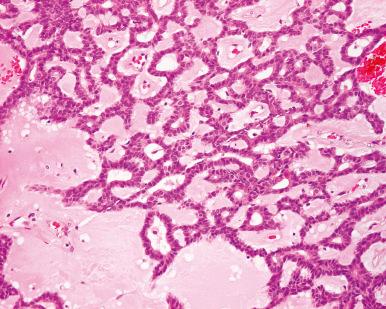
Polymorphous low-grade adenocarcinoma. This is the currently preferred term for a low-grade malignant tumor that has also been called low-grade papillary adenocarcinoma , terminal duct carcinoma , and lobular carcinoma. Adult females are most commonly affected. The palate is the most common location, but all intraoral sites can be involved. Polymorphous low-grade adenocarcinoma is the second most common type of salivary gland carcinoma in this location following adenoid cystic carcinoma. Microscopically, there is uniformity of cell type but a marked variation in architectural patterns, which is responsible for the various names that this tumor has received. Tubular, cribriform, papillary, solid, and fascicular formations may appear, with frequent combinations and transitions ( Figs. 4.27 and 4.28 ). The tumor nuclei are typically oval with pale chromatin and occasional nuclear grooves imparting a resemblance to papillary thyroid carcinoma. The periphery of the tumor has invasive features, sometimes in an Indian-file pattern, which has led to a strained analogy with invasive lobular carcinoma of the breast. Perineurial invasion is also common and may have a targetoid appearance. Mitotic activity is inconspicuous. Extensive S-100 protein immunoreactivity is present, suggesting possible derivation from intercalated ducts. They are often p63 positive, but the staining is focal and of variable intensity. C-kit is often positive in polymorphous low-grade adenocarcinoma, limiting its utility in the differential diagnosis. The differential diagnosis includes benign mixed tumor, canalicular adenoma, basal cell adenoma (all of which lack infiltrative features), and in particular adenoid cystic carcinoma. However, the last lacks the plump and columnar cells of polymorphous low-grade adenocarcinoma, as well as its papillary and fascicular growth patterns. In addition, adenoid cystic carcinomas are not diffusely S-100 positive and have diffuse strong p63 staining in the myoepithelial/basal cell component. The behavior of this tumor is that of a low-grade malignancy. In one series of 69 cases, recurrences developed in 12% and regional lymph node metastases in 10%, but there were no distant metastases, and there was only one tumor-related death. In another series, consisting of 164 cases, 97.6% of the patients were either alive or had died of other diseases. Tumors with a conspicuous papillary component are associated with a higher incidence of lymph node metastases. Rarely, polymorphous low-grade adenocarcinoma may undergo transformation to a high-grade tumor. A majority of polymorphous low-grade adenocarcinomas have recently been shown to have PRKD1 activating mutations.
The recently described cribriform adenocarcinoma of minor salivary glands (cribriform adenocarcinoma of the tongue) is mentioned here despite its obscure histogenesis and also because its differential diagnosis includes several types of salivary gland tumor. Morphologically, it resembles the solid and follicular variants of papillary thyroid carcinoma (to the point of raising the possibility of an origin from the thyroglossal duct anlage), but thyroglobulin stains are negative. Some consider this a variant of polymorphous low-grade adenocarcinoma due to significant histologic and immunophenotypic overlap. This is supported by recent molecular evidence demonstrating translocations involving the PRKD1 gene and the related PRKD2 and PRKD3 genes. In contrast to polymorphous low-grade adenocarcinoma, cribriform adenocarcinoma of minor salivary glands most often arises in the tongue base and more often presents with cervical lymph node metastasis. Despite this latter fact, they are associated with an overall favorable prognosis.
The treatment of minor salivary gland tumors is primarily surgical. It has been emphasized that the first excision should be the most definitive and comprehensive and that treatment of recurrent disease is rarely curative. Postoperative irradiation is generally recommended for all high-grade malignancies, including adenoid cystic carcinoma.
Peripheral ameloblastoma is a tumor of the oral cavity, not involving bone but exhibiting microscopic features of ameloblastic differentiation ( Fig. 4.29 ). As a matter of fact, its appearance is indistinguishable from that of ameloblastoma of the jaw (see Chapter 5 ). Most of the reported cases have occurred in the gingiva, and several have been published in the past as basal cell carcinomas. A desmoplastic variety has been described. Theoretically, peripheral ameloblastomas could arise from remnants of the dental lamina within the gingiva (“rests of Serres”) or from surface epithelium that has retained the capacity to differentiate along odontogenic structures. They are more indolent than their counterparts in the jaw and are generally cured by local excision.
Ephelis and lentigo (melanotic macules) can present as solitary lesions of the oral cavity, usually the lower lip. They are more common in females and are characterized microscopically by hyperpigmentation of the basal layer, associated in the case of lentigo with elongation of the rete ridges. The term melanoacanthoma has been used when the melanocytic proliferation extends above the basal layer and is found intimately admixed with the keratinocytes. Multiple pigmented macules of the lip are one of the components of the Peutz–Jeghers syndrome and Carney complex. The presence of pigmented patches within the oral cavity (usually located in the hard palate or gingiva) is known as melanosis .
Melanocytic nevi may involve the lips and, in rare cases, the inside of the oral cavity. In one series, there were 3 junctional, 30 compound, 32 submucosal (equivalent of the cutaneous intradermal), and 6 blue nevi.
Spitz nevus may involve the tongue and be associated with pseudoepitheliomatous hyperplasia of the overlying squamous epithelium, to a degree that may simulate both malignant melanoma and squamous cell carcinoma ( Fig. 4.30 ).
Malignant melanoma of the oral cavity is particularly common in people of Japanese and black African origin. The hard palate and gingiva are the most common locations. Both pigmented and amelanotic varieties occur. Some of the tumors have desmoplastic features, especially when occurring in the lower lip. These are often underdiagnosed because of their scarce cellularity and sometimes less than prominent atypia. The diagnosis should be suspected in the presence of a spindle cell proliferation in the lamina propria with a fascicular pattern of growth, particularly if accompanied by prominent clusters of lymphocytes in the peripheral portion. The diagnosis is supported by the S-100 protein positivity; however, this is usually accompanied by negativity for Melan-A and HMB-45. Conventional melanoma, by contrast, is usually positive for all three markers.
Oral “melanosis” adjacent to the area of invasive melanoma is found in about 30% of the cases; in most instances, there is some degree of atypia in this intraepithelial component. Lymph node and distant metastases are common, and the prognosis is extremely poor. The histologic parameters used for predicting prognosis of cutaneous melanomas do not apply as well.
Benign nodules made of mature small lymphocytes, with or without an admixture of histiocytes, are not uncommon in the oral cavity. They may represent enlarged buccal lymph nodes or hypertrophic buccal tonsils, or may be associated with cystic glandular structures (“lymphoepithelial cysts”) . The most prominent of these benign lymphoid proliferations occur in the palatine tonsils and are designated lymphoid polyps or pseudolymphomas , but it is better to avoid the latter term.
Malignant lymphoma most commonly occurs in the Waldeyer ring, particularly in the palatine and lingual tonsil, but it can also develop in the gingival area, buccal mucosa, palate, or lips. Most patients are in their sixth or seventh decade, but cases have been reported in younger patients and even in children. The typical clinical presentation is that of a soft, bulky mass covered by normal or ulcerated mucosa. Microscopically, most cases are of B-lineage and follicular center cell origin, of large size and with a generally diffuse pattern of growth. In about 40% of the cases, there is evidence of disease outside the oral cavity, particularly in the cervical lymph nodes and gastrointestinal tract. A high proportion of the latter represent cases of marginal zone lymphoma. T-cell lymphomas can also occur in this location (including mycosis fungoides ), as well as anaplastic large cell lymphomas.
As for malignant lymphomas elsewhere, clinical staging and microscopic typing are the two most important prognostic factors.
Plasmacytomas can occur in the soft tissues of the oral cavity, although not so commonly as in the upper air passages. It is important to distinguish them from the more common plasma cell granulomas of reactive nature, including so-called mucous membrane plasmacytosis or plasma cell mucositis. These disorders are composed of mature plasma cells, have a mixture of other inflammatory cells, and are associated with fibrosis. Immunohistochemical staining for immunoglobulin light chains may help in this differential diagnosis as plasmacytomas will demonstrate a monoclonal population of either kappa- or lambda-expressing cells.
Hodgkin disease presenting initially in the oral cavity is extremely rare, but several reported cases are on record. Most of them were located in the Waldeyer ring, and there was a predilection for the lymphocyte-rich classical subtype.
Leukemia of acute myelocytic or myelomonocytic type is associated with gingival involvement in about 4% of the cases, with or without concomitant skin involvement. In rare cases, oral cavity disease is the first manifestation of extramedullary myeloid sarcoma.
Langerhans cell histiocytosis can involve the oral cavity, either as an isolated focus or as an expression of multisystem disease. Although most often found in the gingiva, the lesions can also affect the hard palate.
Follicular dendritic cell tumors (dendritic reticulum cell tumors) and histiocytic sarcomas have been observed in the palate and tonsil. These are fully discussed in Chapter 37 .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here