Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ultrasound guidance is the optimum technique for placing needles into soft tissue structures when they are well visualized using this imaging method. In broad terms, ultrasound is used for injections and biopsies, but both the structures to be punctured and those that must be avoided should be visible. Ultrasound imaging has particularly good resolution within the first 5 to 10 cm of soft tissue. Sound waves are blocked by bone and gas. Therefore, structures behind bone, for example in the pelvis, or behind a gas-containing viscus would not be suitable for ultrasound image guidance. Most lesions in the extremities, many in the chest and abdominal walls, and most in the neck are safe to inject under ultrasound control.
Color Doppler ultrasonography allows the detection of increased blood supply in a lesion for biopsy and permits the localization of vessels in the intended needle route.
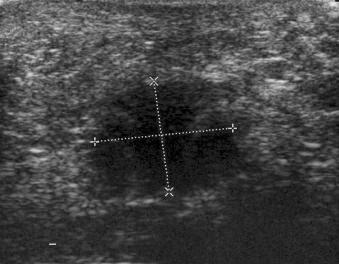
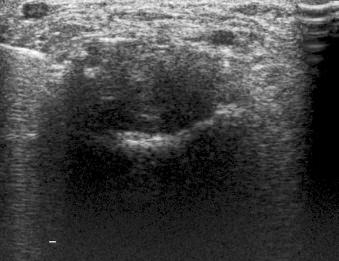
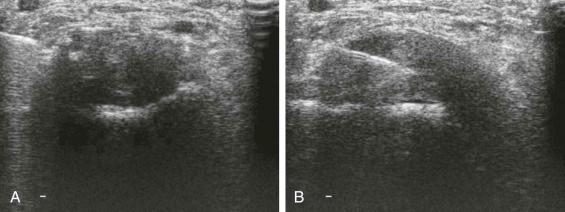
Local anesthetic and corticosteroid injections are commonly undertaken by practitioners in their clinics without any recourse to image guidance. The complications of these procedures are small, and many will be satisfied with this as normal practice. However, it has been argued that a more precise placement of the active agents into the affected area is likely to achieve better results; a more precise injection into a potential cavity rather than muscle or tendon may be less painful. Inadvertent injection into a vessel or nerve can be potentially damaging, and there is evidence that tendon rupture is more common after injections without image guidance. There will be occasions when the unguided placement of drugs does not produce the desired clinical effect. However, there is limited scientific evidence to show that image-guided injections are more effective. It is recognized that unguided injections hit the intended site far less frequently than the clinician may imagine, with the precision being quoted as 25% to 30%. Having stated this, the injection of 5 to 10 mL of drug will infiltrate a very wide area extending up to 15 cm in diameter; therefore, perhaps precise precision is not necessarily an advantage. Ultrasound-guided techniques allow injection of much smaller quantities of active agent into a more selected site ( Fig. 125-1 ; eFigs. 125-1, 125-2, and 125-3 ). Therefore, ultrasound-guided injections are definitely safer and have the potential to be less painful and more effective than injections performed without image guidance.

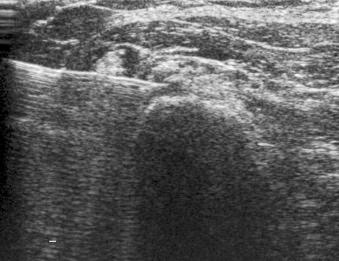
Placement of needles in a joint to instill contrast agents for MR or CT arthrography may be used as an alternative to fluoroscopic guidance. In the shoulder, this may be a more accurate method than fluoroscopy. In the hip and wrist, however, the operator should be experienced in ultrasound-guided injections because extravasation is more likely.
Removal of fluid for diagnostic and therapeutic reasons is straightforward using ultrasound guidance. The guidance and placement methods are the same as for injections. It is usually wise to use larger-bore needles for aspiration, especially in the case of ganglia in which the fluid may be very thick. Aspirated material may be sent for culture, crystal studies, and cytology depending on the suspected diagnosis.
It is tempting to aspirate ganglia, and indeed there is usually an early beneficial effect of doing so. However, the patients and operator should be aware that these lesions usually recur.
Aspiration of hematomas is practical but carries a significant risk of infection. Depending on the circumstances, it may be safer to perform open removal and closure of the cavity.
Ultrasound may be used to guide the placement of pigtail catheters for drainage of infected cavities. The needle is positioned, and a catheter is introduced over the needle. Wires introduced may be used to pass the catheter if it is not part of the needle system.
Biopsy of soft tissue structures, which include mass lesions, potential infected areas, and inflamed synovium, are occasionally carried out by clinicians without image guidance, but increasingly the majority of prudent practitioners will use an image-guided technique. There are obvious dangers from taking a specimen that includes parts of a vessel, nerve, or viscus. Image guidance minimizes these risks and also increases the chance that an appropriate and diagnostic specimen is obtained. The general principle is that the image-guided technique should be one that demonstrates the abnormality and allows visualization of the structures that the operator does not wish to penetrate or damage ( eFig. 125-4 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here