Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac tumors are rare and when they occur, they are most frequently benign. The autopsy incidence of primary cardiac tumors varies greatly by study with estimates ranging from 0.001% to 0.3% and a clinical prevalence of 0.001%–0.03% , of which 75% are benign and 25% malignant. Myxoma is the most common benign tumor (50%–70%) and angiosarcoma is the most common malignant tumor (30%), followed by rhabdomyosarcoma (20%) . Secondary (metastatic) tumors, on the other hand, are the most common tumors of the heart with the reported ratio of cardiac metastases to primary cardiac tumors ranging from 100:1 to 1000:1 . More than three-fourths of primary cardiac tumors are benign with cardiac myxoma (CM) representing the majority of these neoplasms . Malignant cardiac tumors are sarcomas (angiosarcoma is found almost in 30% cases, rhabdomyosarcoma in 20%), pericardial mesothelioma, and lymphoma . The four most common tumors in children younger than 16 years of age are rhabdomyomas (55%), teratomas (16%), fibromas (10%), and myxomas (10%) and account for approximately 90% of benign cardiac tumors in this age group .
The relative frequency of cardiac tumors that are surgically removed and their mean ages at presentation are presented in Table 19.1 .
| Tumor type | % | Mean age at presentation |
|---|---|---|
| Rhabdomyoma c | 2 | 33 weeks |
| Fibroma c | 2 | 13 years |
| Rhabdomyosarcoma | <1 | 15 years |
| Hemangioma | 1 | 31 years |
| Paraganglioma | <1 | 39 years |
| Sarcoma (cardiomegaly) | 4 | 40 years |
| Sarcoma (myofibroblastic) | 9 | 41 years |
| Myxoma | 76 | 50 years |
| Papillary fibroelastoma | 5 | 59 years |
| Lipomatous hypertrophy/lipoma | <1 | 64 years |
| Primary lymphoma | 1 | 67 years |
a Based on 250 tumor resections from five institutional surgical series.
b Based on authors’ experience of consultation material.
c Incidence of pediatric tumors varies by institutional setting—that is, proportion of pediatric patients.
The fourth edition of the World Health Organization (WHO) classification of tumors published in 2015 divides primary cardiac tumors into benign, malignant, and intermediate tumors of uncertain behavior, with separate sections on germ cell tumors and tumors of the pericardium ( Table 19.2 ). The overall characteristics of heart tumors are presented in Table 19.3 .
| Benign tumors and tumor-like conditions | ICD-O codes |
|---|---|
| Rhabdomyoma | 8900/0 |
| Histiocytoid cardiomyopathy | |
| Hamartoma of mature cardiac myocytes | |
| Adult cellular rhabdomyoma | 8904/0 |
| Cardiac myxoma | 8840/0 |
| Papillary fibroelastoma | |
| Hemangioma, NOS | 9120/0 |
| Capillary hemangioma | 9131/0 |
| Cavernous hemangioma | 9121/0 |
| Arteriovenous malformation | 9123/0 |
| Intramuscular hemangioma | 9132/0 |
| Cardiac fibroma | 8810/0 |
| Lipoma | 8850/0 |
| Cystic tumor of the atrioventricular node | 8454/0 |
| Granular cell tumor | 9580/0 |
| Schwannoma | 9560/0 |
| Tumors of uncertain biologic behavior | |
| Inflammatory myofibroblastic tumor | 8825/1 |
| Paraganglioma | 8680/1 |
| Germ cell tumors | |
| Teratoma, mature | 9080/0 |
| Teratoma, immature | 9080/3 |
| Yolk sac tumor | 9071/3 |
| Malignant tumors | |
| Angiosarcoma | 9120/3 |
| Undifferentiated pleomorphic sarcoma | 8830/3 |
| Osteosarcoma | 9180/3 |
| Myxofibrosarcoma | 8811/3 |
| Leiomyosarcoma | 8890/3 |
| Rhabdomyosarcoma | 8900/3 |
| Synovial sarcoma | 9040/3 |
| Miscellaneous sarcomas | |
| Cardiac lymphomas | |
| Metastatic tumors | |
| Tumors of the pericardium | |
| Solitary fibrous tumor | 8815/1 |
| Malignant | 8815/3 |
| Angiosarcoma | 9120/3 |
| Synovial sarcoma | 9040/3 |
| Malignant mesothelioma | 9050/3 |
| Germ cell tumors | |
| Teratoma, mature | 9080/0 |
| Teratoma, immature | 9080/3 |
| Yolk sac tumor | 9071/3 |
| Histologic type | Age | Site in heart | Multiplicity | Syndromic association | |||
|---|---|---|---|---|---|---|---|
| Fetuses, infants | Children | Adults | Layer | Location | |||
| Benign congenital tumors | |||||||
| Rhabdomyoma | ++ | + | Myocardium a | Ventricles | Usual | Tuberous sclerosis | |
| Fibroma | + | ++ | + | Myocardium | Ventricle, ventricular septum | Rare | Gorlin syndrome |
| Histiocytoid cardiomyopathy | ++ | +/1 | Endocardium, myocardium | Ventricles, atrial, AV SA nodes | Always | ||
| Benign acquired tumors | |||||||
| Myxoma | +/− | ++ | Endocardium | LA, atrial septum | Rare | Carney complex | |
| RA, atrial septum | |||||||
| Papillary fibroelastoma | ++ | Endocardium | Valves > atria > ventricles | Occasional | |||
| Hemangioma b | + | + | + | Myocardium Endocardium c | Atria > ventricles | Unusual | |
| Lipomatous hypertrophy | ++ | Myocardium of atrial septum | |||||
| Lipoma | ++ | Myocardium, epicardium, endocardium | All sites | Rare | |||
| Inflammatory myofibroblastic tumor d | ++ | + | +/− | Endocardium | Valves > atria | Occasional | |
| Germ cell tumors | |||||||
| Teratoma | ++ | + | +/− | Pericardial cavity | No | ||
| Ventricular septum (rare) | |||||||
| Yolk sac tumor | ++ | + | Pericardial cavity | No | |||
| Ventricular septum (rare) | |||||||
| Malignant tumors | |||||||
| Angiosarcoma | +/− | ++ | All layers | Right atrium, pericardium | Occasional | ||
| UPS/myxofibrosarcoma | +/− | +/− | ++ | Endocardium | Left atrium | Rare | |
| Other sites | |||||||
| Rhabdomyosarcoma | +/− | ++ | + | Myocardium | Ventricles | No | |
| Leiomyosarcoma | +/- | ++ | Endocardium | Left atrium | No | ||
| Lymphoma | +/− | ++ | Myocardium | Right atrium, others | Occasional | ||
a Boldface indicates an exclusive site.
b Hemangioma is considered alternatively as a congenital tumor, especially in children.
c Especially the capillary type.
d Inflammatory myofibroblastic tumors are sometimes considered low-grade malignancies, although none in the heart has metastasized.
In this chapter, for ease of discussion, we have broadly divided cardiac neoplasms into five types: pseudotumors, ectopias and tumors arising from ectopic tissue, tumors of mesenchymal tissue (primary benign and malignant tumors), lymphoid neoplasms, and metastatic lesions. Pseudotumors are discussed first, followed by benign and malignant lesions, in turn. Finally, we provide a brief discussion of vascular tumors.
Cardiac tumors are diagnosed noninvasively by echocardiograms, magnetic resonance imaging (MRI), computed tomography (CT) scan, and angiography. The goal of cardiac imaging is to provide information about mass size, anatomic location and extent, functional implications in relation to flow obstruction, valvular involvement, regional contractility, presence or absence of pericardial metastasis, and effusion . Most simple primary and some complex primary cardiac tumors should be surgically resected . The surgical pathologist, who makes a histologic diagnosis on a cardiac mass, must be familiar with the spectrum of primary tumors of the heart. The prognosis following surgery is usually excellent in the case of benign tumors, but despite advances in cardiac imaging, which allows early detection and surgical removal, malignant cardiac tumors continue to carry a poor prognosis.
Finally, several tumors are found exclusively in the heart and deserve special mention. The CM is unique to the heart and possesses several histologic/immunohistochemical features that clearly separate it from soft tissue myxomas. Other tumors that are found only in the heart include cardiac rhabdomyoma, Purkinje cell hamartoma, cystic tumor of the atrioventricular (AV) node, papillary fibroelastoma (PFE), and lipomatous hypertrophy of the atrial septum.
The clinical presentation of cardiac tumors ranges from asymptomatic detection on imaging performed for other reasons, and cardiac tumors are considered great mimickers. When symptomatic, they can present with constitutional symptoms (fever and weight loss), distal embolization, or direct effects from the tumor .
They usually present with congestive heart failure, arrhythmia, or thromboembolism with over 50% of cases due to a large intracavitary mass; depending upon the chamber of involvement, they may result in either backward or forward low-output heart failure . The signs and symptoms are related to the precise location within the heart, tumor size, and chamber of involvement ( Table 19.4 ). However, the identification of an intracardiac mass should first be placed in the context of the patient’s clinical history. Intracavitary tumors have a point of attachment to the wall of the heart and therefore may cause arrhythmias ( Table 19.5 ). Myxomas, as well as other primary cardiac tumors, may present with one or more of the classic symptom triad, including sequelae of valvular obstruction, embolic phenomena, and constitutional symptoms. The symptoms related to embolic phenomenon include strokes, transient ischemic attacks, claudication of the extremities, renal insufficiency, myocardial infarction, and when located on the right side, pulmonary embolism. Tumors of the right ventricle produce symptoms of pulmonary stenosis and usually present with syncope.
| Benign tumors |
|---|
| Cardiac myxomas |
|
| Papillary fibroelastoma |
|
| Rhabdomyoma (most common tumor in children) |
|
| Fibroma (most common resected tumor in children) |
|
| Atrioventricular nodal tumors |
|
| Cardiac lipomas |
|
| Malignant tumorsAngiosarcoma |
|
| Undifferentiated pleomorphic sarcoma (UPS) |
|
| Osteosarcoma |
|
| Leiomyosarcoma |
|
| Rhabdomyosarcoma |
|
| Cardiac lymphoma |
|
| Pericardial mesothelioma |
|
| Metastatic cardiac tumor (depends on the primary tumor as well as myocardial or pericardial involvement) |
|
| Type of tumor | Left atrium | Right atrium | Left ventricle | Right ventricle | Valve | Pericardium |
|---|---|---|---|---|---|---|
| Myxoma | 90% | 10% | Rare | Rare | Rare | 0 |
| Sarcoma | 46% a | 26% | 21% (right or left) b | b | 0 | 7% |
| Fibroma | Rare | Rare | 80% (majority in IVS) | 20% | 0 | 0 |
| Papillary fibroelastoma | 2% | c | 10% | 3% (right heart) c | 85% (AV, MV) | 0 |
| Rhabdomyoma d | 0 | 30% (atrium or ventricle) e | 70% (and ventricular septum) | e | 0 | 0 |
| Lipoma (LI)/lipomatous hypertrophy (LH) | 0 | Majority LH | Epicardial surface (LI) | Epicardial surface (LI) | 0 | 0 |
| Angioma | Any location | Any location | Any location | Any location | Varix | 0 |
a Angiosarcomas predominately arise in right atrium.
d 90% are multiple, and occur in newborn or children, rare in adults.
Thrombus is the most commonly identified intracardiac mass and can be found within the atrial or ventricular cavities. Endocardial thrombi in the atria are generally left-sided and the majority of mural thrombi occur in association with underlying heart disease with higher frequency in the setting of atrial enlargement, atrial fibrillation, and mitral valve disease . Thrombi, in general, are also more common among those with hypercoagulable states such as malignancy and the antiphospholipid antibody syndrome or with endomyocardial fibrosis in hypereosinophilic syndrome, or intracardiac prosthetic material such as prosthetic valves or indwelling catheters .
Although not strictly cardiac tumors, mural thrombi are occasionally removed surgically, and are often clinically and pathologically misdiagnosed as myxomas. For these reasons, it is important for a pathologist to be familiar with the histologic and clinical features of cardiac thrombi. Left atrial thrombi are frequently associated with mitral valvular disease, especially mitral stenosis, and thrombi occur in either atria in patients with atrial fibrillation. Ventricular thrombi likewise may form with decreased or abnormal ventricular contractility, particularly in patients with ischemic heart disease, especially at sites of transmural infarction or cardiomyopathy. In patients with known cardiac disease, mural thrombi are readily diagnosed by imaging studies and biopsy or resection is only rarely performed. Cardiac MRI is highly accurate in differentiating cardiac thrombi from tumors and should therefore be included in the routine evaluation of suspected cardiac masses .
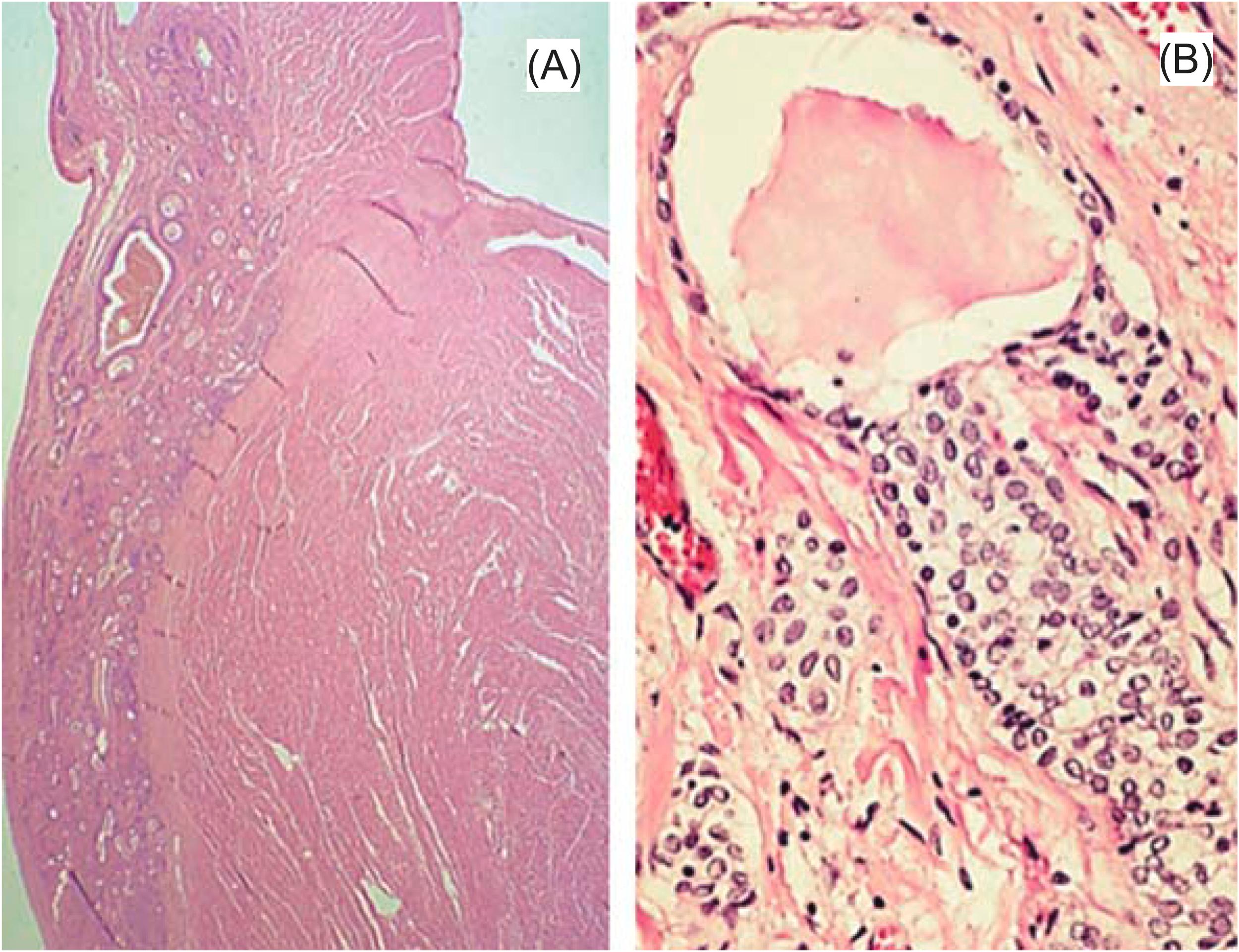
Mural thrombi in the absence of heart disease occur in any chamber but are most common in the right atrium. In the majority of patients, a coagulation defect is either suspected or documented. One of the more common coagulopathies diagnosed in patients with mural thrombi is antiphospholipid syndrome , but a wide variety of conditions may be the underlying predisposing factor, including essential thrombocytosis ( Fig. 19.1 ), protein C or S deficiency, and Behçet’s disease . In some patients, the nature of coagulopathy is not appreciated, and the preoperative diagnosis is most often thought to be CM . If venous emboli become dislodged in the right ventricle, a mistaken preoperative diagnosis of the right ventricular tumor may be made .
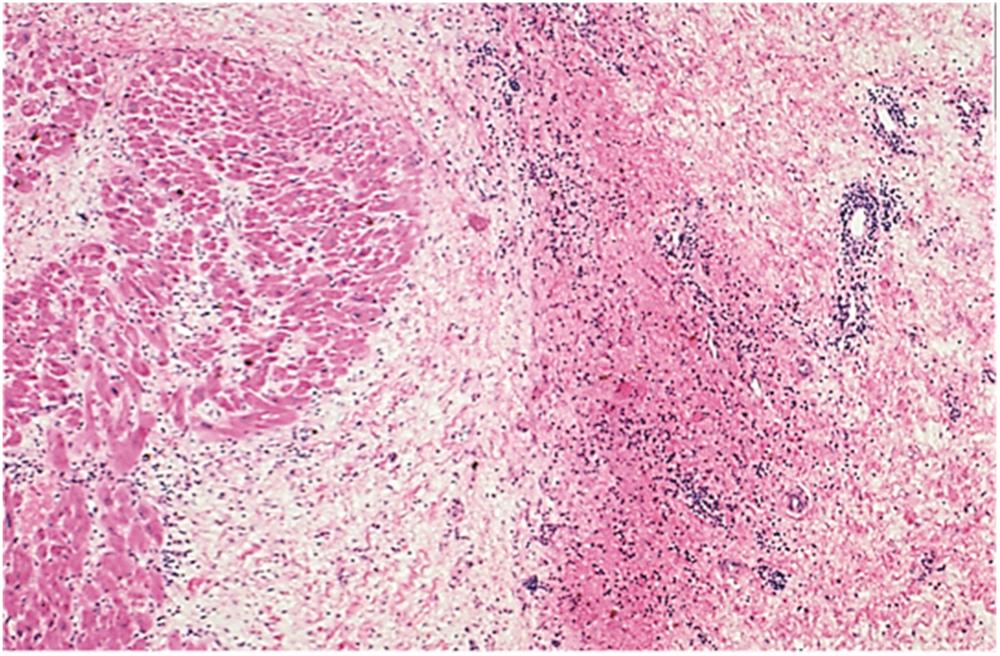
Histologically, organizing thrombi are characterized by layers of degenerating blood cells, fibrin, and a margin of granulation tissue with varying degrees of fibrosis depending on the age of the thrombus ( Fig. 19.2 ). The endocardium demonstrates thickening and elastosis. It is worthwhile to evaluate the underlying myocardium to make a specific diagnosis. Numerous eosinophils and extracellular eosinophil breakdown products may suggest hypereosinophilic syndrome (eosinophilic endocardial disease), and intramural arterioles are often thrombosed. Obliteration of intramural arterioles with fibrointimal proliferation raises the diagnostic possibility of essential thrombocytosis or embolic disease resulting in myocardial infarction and mural thrombus. In most cases, however, the diagnosis is simply mural thrombus, and the clinician must attempt to explain the mass on the basis of underlying heart disease or a coagulation defect.
The pathologic differential diagnosis of mural thrombus includes primarily CM. Before even considering the histologic appearance, the site of attachment helps make this distinction. Mural thrombi typically occur in the atrial appendages or posterior walls of the atrium, whereas myxomas almost exclusively occur at the fossa ovalis. Histologically, myxoma is a heterogeneous proliferation of myxoma cells, capillaries, and inflammatory cells, which in most cases allows a straightforward diagnosis.
Cardiac calcified thrombus is a rare nonneoplastic cardiac mass that can present like an intracardiac tumor. Calcification within a mural thrombus often leads to the erroneous clinical diagnosis of CM .
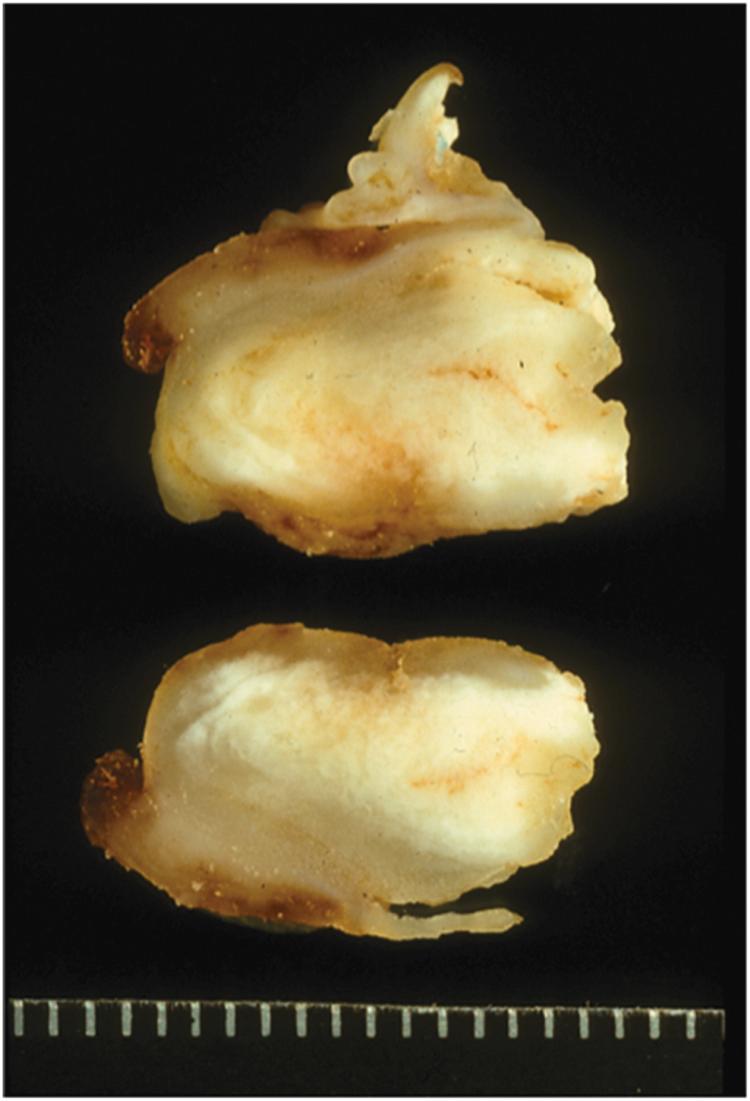
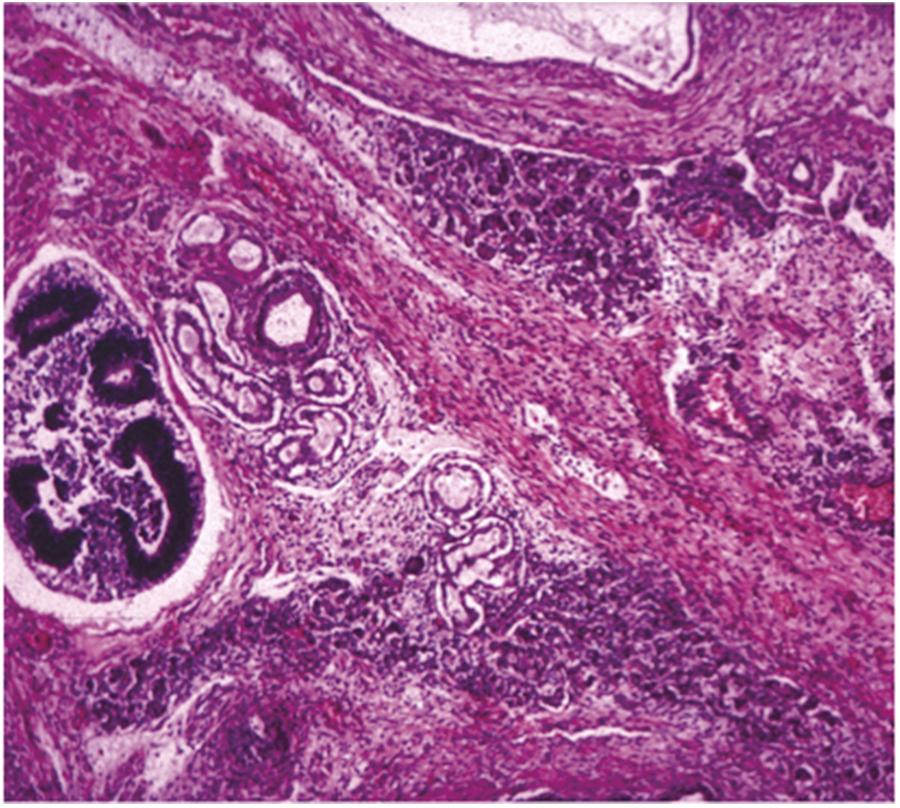
In some mural thrombi, the calcification may be diffuse, resulting in a rock-hard mass that must be subjected to days of decalcification before histologic sectioning is possible ( Fig. 19.3 ). Calcified mural thrombi may occur in any cardiac chamber; most commonly, the right atrium is often associated with antiphospholipid syndrome or renal failure, and has been fancifully designated cardiac CAT or calcifying amorphous tumor . Histologically, there are abundant microcalcifications in a hyalinized stroma ( Fig. 19.4 ). The presence of foamy histiocytes (CD68+) has also been reported .

Reactive inflammatory masses in the myocardium are rare. Inflammatory myofibroblastic tumors (IMFTs), also called pseudotumors, are rare benign primary tumors of the heart in infants, with worldwide reports of approximately 15 cases. Most of these tumors in the heart show a predilection for atria and appear to behave in a benign fashion, although local recurrence and multiple lesions have been described . In parts of the world where parasitic diseases are endemic, echinococcal cysts in the myocardium may produce a tumor-like lesion. Within the heart, the left ventricle is the most common site, although most reports describe cysts in the epicardial borders of the ventricle. CT and MRI of the heart are diagnostic .
Mesothelial/monocytic incidental cardiac excrescences (MICEs) are uncommon pseudotumors and may histologically mimic metastatic adenocarcinoma. They consist of nonneoplastic proliferations of mesothelial cells intermingled with foamy macrophages enmeshed in fibrin. They are not true tumors and are incidental findings in surgical tissue removed from the heart and pericardium ( Fig. 19.5 ). These structures are histologically identified by their total lack of stroma or vascularity and by their characteristic cellular constituents. Immunohistochemistry shows histiocytoid elements staining strongly and diffusely for CD68 along with mesothelial marker calretinin and WT1, which highlight mesothelial elements. Histiocytic cells also may be stained for CD31. Most are thought to be artifacts of open-heart surgery . Originally they were considered a form of hemangioma .
Cystic tumor of the AV node, also known as mesothelioma of the AV node, is a benign congenital tumor that is located in the triangle of Koch in the AV nodal region of the atrial septum of the heart. It accounts for 2.7% of cardiac tumors and is the most common primary cardiac tumor causing sudden death . Although once considered of mesothelial or even of endothelial origin, these inclusions are believed to be derived from primitive endoderm . Others have hypothesized that the lesion may represent an ultimobranchial heterotopia congruent with an alteration in cardiac neural crest cell development . Similar lesions have not been described elsewhere in the body. The majority of patients have congenital heart block, and almost three of four are female. Most tumors occur sporadically, but there is an association with cysts of endocrine organs and other midline defects, such as ventricular septal defect, nasal septal defect, encephalocele, thyroglossal duct cysts, and absent septum pellucidum.
Most tumors are diagnosed first at autopsy, although these lesions should be considered in the differential diagnosis of congenital heart block, especially in girls. Death is usually sudden and unexpected. Ventricular arrhythmias are somewhat more frequent in patients with heart block, from any cause, than in patients without heart disease. The mean age at death is in the fourth decade, although there is a wide range, from birth to the eighth decade. There have been rare reports of biopsy diagnosis of AV nodal tumors .
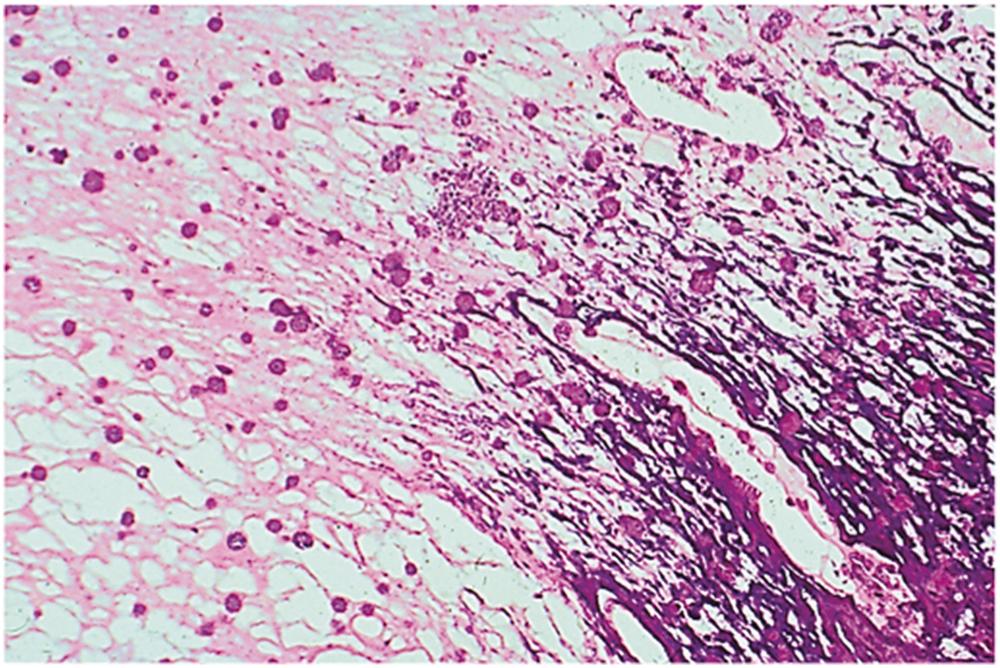
In almost half of the hearts with AV nodal tumors, cysts are grossly evident to the naked eye in the atrial approaches to the AV node; in the remainder of cases, the tumor is first noted on histologic examination of the conduction system. The cystic tumor of the AV node often exhibits a small, multicystic appearance with cysts varying in sizes from 2 mm to 2 cm . Histologically, there are multiple cysts, which occur in the area of the AV node and the nearby atrial tissues, without the involvement of the central fibrous body or penetrating bundle ( Fig. 19.6A ). The cysts are lined by cuboidal, transitional, or squamous epithelium, and there is often a combination of epithelial elements ( Fig. 19.6B ) mixed with occasional clear cells (neuroendocrine or C cells) . Cells can interdigitate with myocytes within the inferior septum, resulting in degenerative changes within the myocytes. Intervening stroma is generally composed of dense fibrous connective tissue. Many cysts are collapsed, forming nests of cells with an infiltrative appearance. Remnants of AV nodes are rarely identifiable. There are no mitotic figures or atypical features of the nuclei. The cells of the cystic tumor of the AV node stain with alcian blue and periodic acid-Schiff (PAS), exhibiting resistance to both hyaluronidase and diastase digestion, respectively . Immunohistochemically, the main cells of the lesion stain positive for cytokeratin CAM5.2, cytokeratin AE1/AE3, cytokeratin 34βE12, cytokeratin 5/6 (CK5/6), cytokeratin 7 (CK7), epithelial membrane antigen (EMA), carcinoembryonic antigen (CEA), carbohydrate antigen (CA)19.9, p63, bcl2, and galectin 3 . The neuroendocrine cells of the lesion stain positive for CAM5.2, pan-keratin (AE1/AE3), CEA, calcitonin, chromogranin, synaptophysin, and thyroid transcription factor 1 (TTF1). The lesion stains negative for keratin 20 (CK20), p53, Bcl-2, cyclin D1, cytokeratin 20 (CK20), vimentin, CD31, factor VIII-related antigen, estrogen receptor, progesterone receptor, thrombomodulin, Wilm’s tumor 1, and calretinin . This is in contrast with the true mesothelium, which stains positive for thrombomodulin, Wilm’s tumor 1, and calretinin and negative for PAS . Ki-67 staining shows minimal proliferation (2%) . There are a few entities one should consider in the differential diagnosis; these include bronchogenic cyst, mesothelial cyst and teratomas, and rarely histiocytoid cardiomyopathy when they occur in children . The diagnosis of teratoma rests on the identification of endodermal, ectodermal, and mesodermal elements.
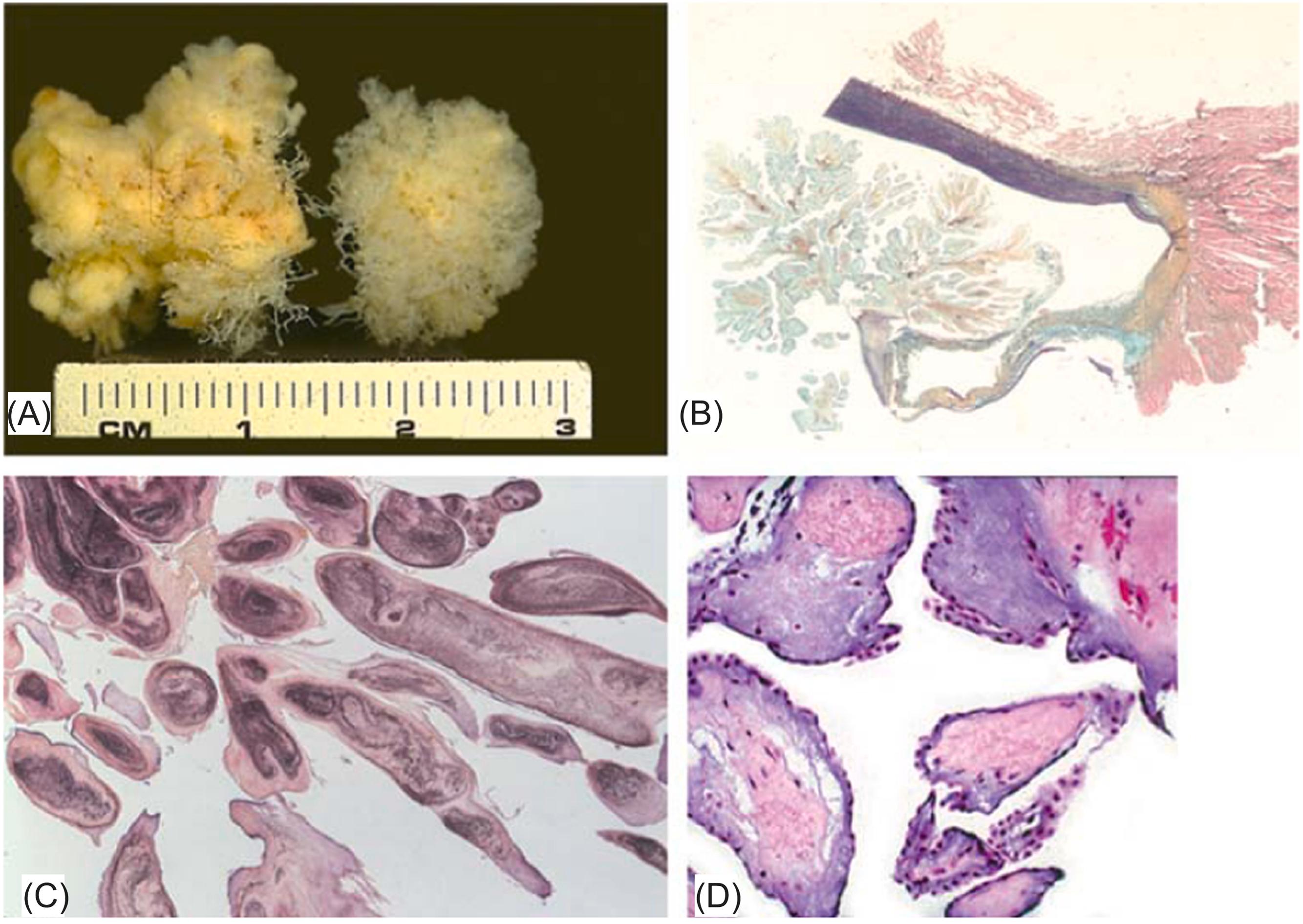
Almost all germ cell tumors of the heart are teratomas; rare yolk sac tumors have also been described within the pericardium . The majority of cardiac teratomas are located in the pericardial sac in fetuses, newborns, infants, or children. Rarely, they may occur within the myocardium in the ventricular septum or in the area of the AV node. Histologically, they resemble testicular teratomas and are usually benign ( Fig. 19.7 ). The clinical diagnosis may be made in utero , and symptoms include tamponade, hydrops fetalis, and sudden death .
Ectopic thyroid tissue when it occurs in the myocardium is called “struma cordis.” Ectopic thyroid tissue occurs because of embryological malformation, and its prevalence is approximately 1 in 300,000–400,000 individuals .
The right ventricular outflow is generally involved. The condition is believed to occur early in embryogenesis when part or all of the functioning thyroid tissue becomes lodged in the ventricular outflow region . Although pulmonary stenosis with right ventricular hypertrophy may occur, most patients are asymptomatic . Histologically, there are follicular structures containing colloid; if there is any difficulty in diagnosis, immunohistochemical stains for thyroglobulin may be performed. The differential diagnosis includes metastatic carcinoma of various origins and metastatic thyroid carcinoma. The latter distinction may be difficult purely on histologic grounds, and is made clinically by the exclusion of a dominant mass in the thyroid. In these cases, thyroid hormone levels are often normal.
PFE is an unusual lesion occurring exclusively on the endocardial surface, most commonly on valve leaflets. PFE is a pedunculated mass with multiple fronds attached to the endocardium by a stalk, generally with a diameter smaller than 1 cm and occurs in all age groups. The most commonly involved valve is the aortic valve. Tumor mobility and aortic valve location can lead to serious complications, namely thromboemboli.
It is rare with an estimated frequency of 0.0017%–0.33% in the autopsy series . The majority of PFEs are solitary, but multiple PFEs are found in 7%–13% of all PFE cases . However, because many surgically excised valves are not carefully examined and sectioned, it is believed by some to be the most common benign cardiac growth as these small lesions are often missed on gross examination alone . A PFE is probably an exaggerated form of Lambl’s excrescence , which is a reactive filiform growth that occurs at the sites of greatest hemodynamic stress, usually at the nodules of Aranti of the semilunar valves. Like Lambl’s excrescences, they occasionally occur in areas of previous endocardial damage or in patients with preexisting heart disease. We have seen them in patients with prosthetic heart valves and previous radiation therapy. Unlike Lambl’s excrescences, PFEs can become quite large and occur on any valve surface or area of the endocardium.
The pathogenesis of PFE is unknown, and it is unclear if it is a reactive or hamartomatous process. The most serious complication is thromboembolism. Its frequency has been reported as high as 53% and is higher than other benign cardiac tumors . Thrombi may occur on the surface of the proliferation, and dislodged clots are responsible for embolic symptoms. The high frequency of thromboembolism in PFE is ascribed to two potential mechanisms from tumor fragment or micro-thrombus attached to the irregular surface on the tumor . However, we have not noted thrombi on incipient lesions and doubt that thrombosis is the inciting event, a theory corroborated by established immunohistochemical differences between PFE and organizing thrombus .
The majority of cardiac PFE are incidental findings at autopsy. However, left-sided lesions may cause symptoms by embolization of attached fibrin clots or prolapse into the coronary orifices . The most common symptoms are transient neurological defects and myocardial ischemia, although sudden death has also been reported .
Grossly, the PFE has been compared to a “sea anemone,” an appearance heightened by placing the specimen in a bowl of water ( Fig. 19.8A ) . Their most common location is the aortic valve, followed by the mitral and tricuspid valves, pulmonary valve, and endocardial surfaces. They are usually attached to the endocardial surface by a short slender stalk, but more than one attachment to the endocardium has been observed. Histologically, they are avascular papillary structures lined by endothelial cells ( Fig. 19.8B and C ). The papillary cores contain a proteoglycan-rich stroma, and layers of elastic fibers and collagen are prominent near the base of the lesion. The cells covering the surface express vimentin, factor VIII-related antigen, and CD34, and the stroma is rich in collagen type IV .
The major differential diagnosis is CM. Most reported “myxomas” of cardiac valves are, in fact, PFEs. Myxomas are highly vascular lesions that rarely occur on the valve surfaces and contain characteristic “myxoma” cells not seen in PFE. Surgical excision is necessary for symptomatic lesions. Valve repair may also be performed. Aortic valve PFE is generally treated with valve-sparing techniques. Only 10% of PFE cases need valve replacement .
Rhabdomyoma is the most common primary cardiac neoplasm in children. The diagnosis is established before birth to the age of 6 years, with a mean age at diagnosis of 2 weeks and without sex predilection . It is a hamartoma of cardiac myocytes and is intimately associated with the tuberous sclerosis syndrome. The clinical presentation is determined by the size and position of the tumor. The tumor has been diagnosed antenatally (as early as 20 weeks) or postnatally by transthoracic or transoesophageal echocardiography and cardiac MRI. Most, if not all, patients with tuberous sclerosis complex (TSC) will, at echocardiography, demonstrate multiple cardiac masses, presumed to be rhabdomyomas, in infancy . Conversely, 50% of patients with rhabdomyomas will have other manifestations of the syndrome, such as intracranial hamartomas, facial angiofibromas, subungual fibromas, linear epidermal nevi, renal angiomyolipomas, and other hamartomas . Rhabdomyoma in patients with TSC is related to the loss of hamartin or tuberin proteins following mutations in tumor suppressor genes TSC1(9q34) or TSC2(16p13.3), respectively .
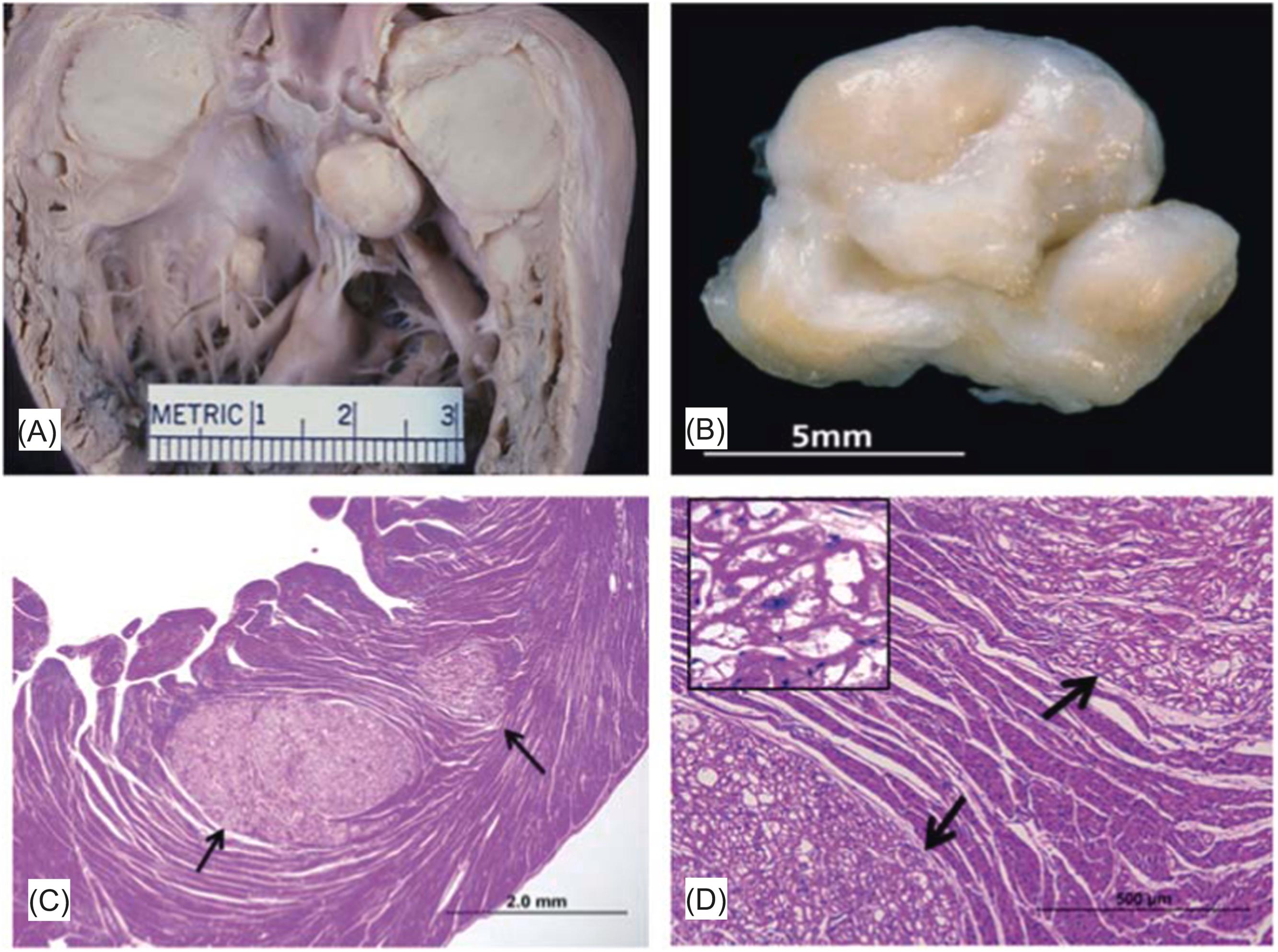
Rhabdomyomas in patients with TSC are usually multiple masses that, with extensive cardiac involvement, may result in intrauterine hydrops ( Fig. 19.9A ) . These masses tend to regress spontaneously in the first 4 years of life without any medical or surgical intervention and there are often no cardiac symptoms if the patient survives the first month of life. Sporadic rhabdomyomas are more likely solitary endocardial-based lesions that may cause ventricular outflow tract obstruction requiring surgical excision or induce cardiac arrhythmias. However, there is an overlap between the morphologic findings in patients with and without tuberous sclerosis .
Most patients are diagnosed in the first few months of life. However, cardiac rhabdomyomas may be detected in children and teenagers, and should, especially when multiple, prompt the cardiologist to search for other manifestations of tuberous sclerosis .
Grossly, rhabdomyomas are well-demarcated, nonencapsulated, yellow-tan nodules that occur within the myocardium or on the endocardial surface, with sizes ranging from 0.3 to 9.0 cm, with a mean size of 3.4 cm .
Incidental rhabdomyomas are often endocardial lesions near the AV valves ( Fig. 19.9B ). Rhabdomyomas are composed of enlarged vacuolated cells with sparse cytoplasm. The characteristic cell is the vacuolated “spider cell,” which possesses strands of cytoplasm emanating from the nucleus ( Fig. 19.9C and D ). The apparent spaces within the cell contain large amounts of glycogen. Ultrastructurally, there are glycogen granules, myofibers, dispersed Z-band material, and intercalated disks along the cell periphery . Its immunoreactivity toward desmin and myoglobin confirms the striated muscle characteristics of the tumor cells . Spider cells are also positive for ubiquitin, which is associated with myofilament degradation with enlargement of glycogen vacuoles leading to cytoplasmic vacuolation and myxoid degeneration .
There are few entities in the differential diagnosis. Vacuolated cells may occur in storage diseases in a diffuse, nondiscrete distribution. Purkinje cell hamartomas are usually smaller lesions with abundant mitochondria .
Diffuse cardiac rhabdomyomatosis is a rare cause of pediatric cardiomyopathy presenting as sudden cardiac death. Histologically, there is diffuse involvement of the myocardium by rhabdomyoma-like cells with infiltrating borders associated with significant fibrosis. The large clear cells contain glycogen and are PAS positive, as reported in the classic rhabdomyoma .
Adult cellular rhabdomyoma is a rare tumor that is histologically and clinically distinct from congenital rhabdomyoma. These tumors are considered to be true neoplasms with striated muscle differentiation, expansile growth, and evidence of cell proliferation (Ki67 or PCNA) (70). Adult rhabdomyoma represents <2% of all muscular tumors, mostly occurs in adults (median age 60 years), and males are more commonly affected than females (M:F=3:1). These tumors usually present as solitary lesions and most are found in the atria . Electrical disturbances such as supraventricular tachycardia or nonsustained ventricular tachycardia are common.
Grossly, these tumors range in size from 2 to 5 cm. Adult cellular rhabdomyomas demonstrate small, tightly packed round to polygonal cells with finely granular eosinophilic cytoplasm; spindling of tumor cells is also a common feature. Unlike congenital rhabdomyoma, vacuolated spider cells are rarely present. Immunohistochemically, the cells show strong positivity for myoglobin, actin, desmin, and myogenin. . The differential diagnosis includes rhabdomyosarcoma, but the absence of tumor necrosis, mitotic figures, and the presence of a well-defined pseudocapsule helps to distinguish it from the malignant rhabdomyosarcoma. The long-term biologic behavior of these neoplasms is not known .
Purkinje cell hamartoma, also known as histiocytoid/oncocytic cardiomyopathy, comprises a small percentage of surgical resections of heart tumors and occurs predominantly in the first 2 years of life. The histogenesis of the lesion is debated, and it is unclear whether the cell of origin is the Purkinje cell or the cardiac myocyte . The abundance of mitochondria on the ultrastructural study and the histologic appearance have led to the use of the term “oncocytic cardiomyopathy.”
At the time of diagnosis, most patients are younger than 3 years, and there is female 4:1 predominance. The most common presenting features are arrhythmias, followed by seizures, heart failure, cyanosis, dyspnea, and sudden death . Associated cardiac and extracardiac anomalies, such as ventricular septal defect and midline defects of the central nervous system, affect approximately 25% of patients.
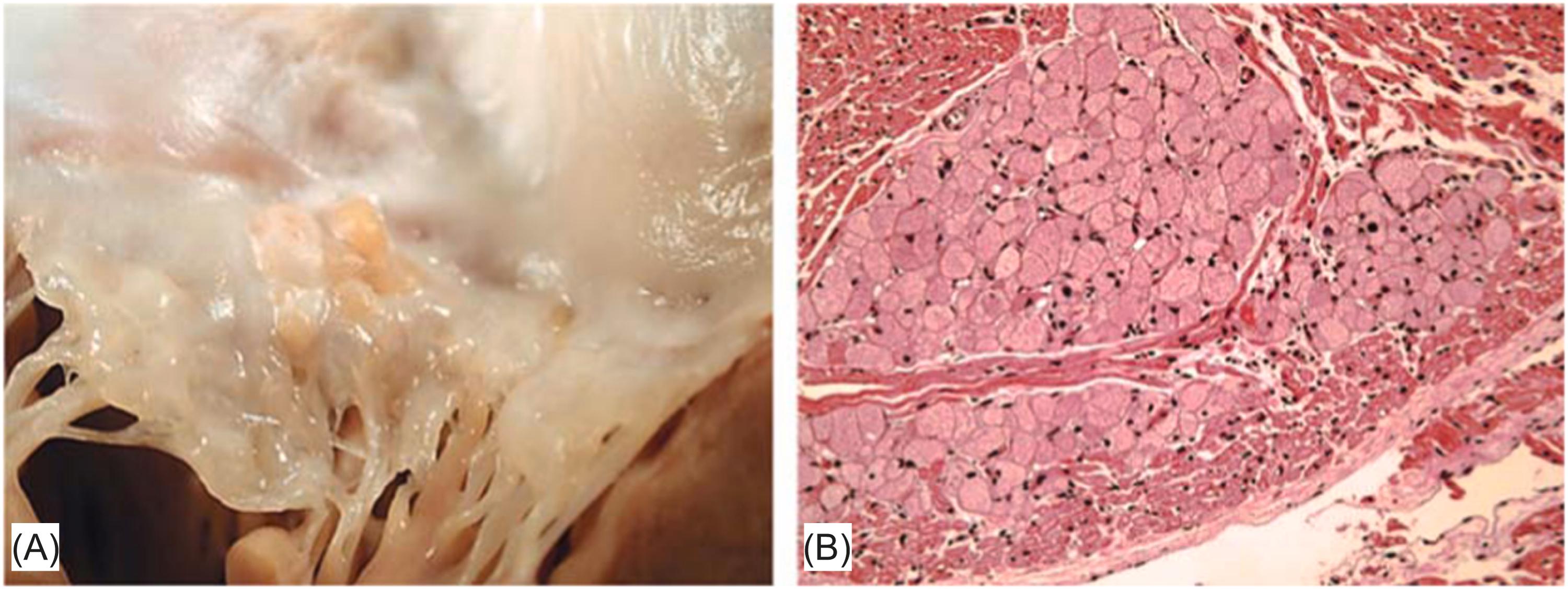
The nodules of histiocytoid cardiomyopathy are raised and yellowish, range from 1 mm to 1.5 cm in diameter, and are usually less than 2 mm ( Fig. 19.10A ) . The nodules occur mainly in the subendocardium following the distribution of the bundle branches of the conduction system but may also occur anywhere in the heart. Histologically, there are clusters of foamy cells that are well demarcated from the adjacent normal myocardium ( Fig. 19.10B ). The abnormal cells are large, pale, rounded to oval, often surrounded by thin collagen fibers, and stain faintly with PAS. In contrast to those of a rhabdomyoma, large vacuoles and cytoplasmic streaming are absent. By immunohistochemical techniques, the cells are negative for lysozyme and alpha-1 antitrypsin, and weakly positive for myoglobin, desmin, myosin, and muscle-specific actin. Ultrastructurally, there are abundant swollen mitochondria with disorganized cristae, occasional leptomeric fibers, and few desmosomes. T tubules are absent and intercalated disks are rarely seen.
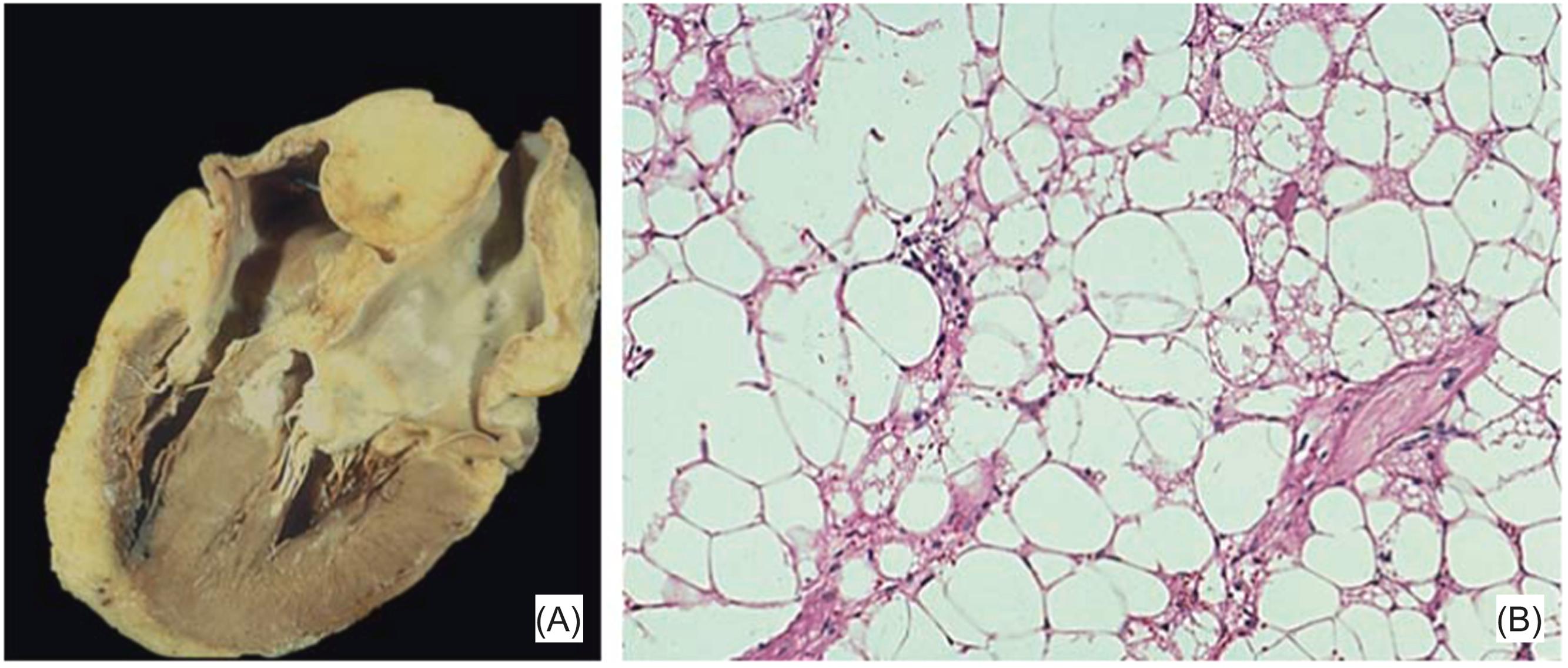
Considered a benign neoplasm, it enters in the differential diagnosis of lipoma. It is a deposition of fat occurring solely in the interatrial septum resulting in a thickness greater than 2 cm . There are no precise criteria for the autopsy diagnosis because the condition is an exaggeration of the normal components and septal thickness may vary depending on the area measured. In general, the fat deposit is measured above the oval fossa, where it forms a triangular mass roofed by the epicardial surface of the atria. Lipomatous hypertrophy occurs almost exclusively in adults, and there is an association with obesity, although not all patients are overweight . Lipomatous hypertrophy of the atrial septum is usually an incidental finding at autopsy. However, an association between interatrial fat deposits and arrhythmias, particularly atrial and supraventricular tachycardias, has been well established . In the absence of other findings, lipomatous hypertrophy has even been blamed for sudden cardiac death .
Recently, imaging techniques have allowed antemortem diagnosis . The surgical pathologist now encounters it in the rapid diagnosis suite, either because the surgeon removes the mass incidentally during open-heart surgery for other causes or for relief of cardiac symptoms, such as congestive heart failure or vena caval obstruction . The preoperative diagnosis is usually right atrial myxoma because the mass bulges into the right atrial cavity , or if tissue density has been ascertained, the correct diagnosis is made before surgery .
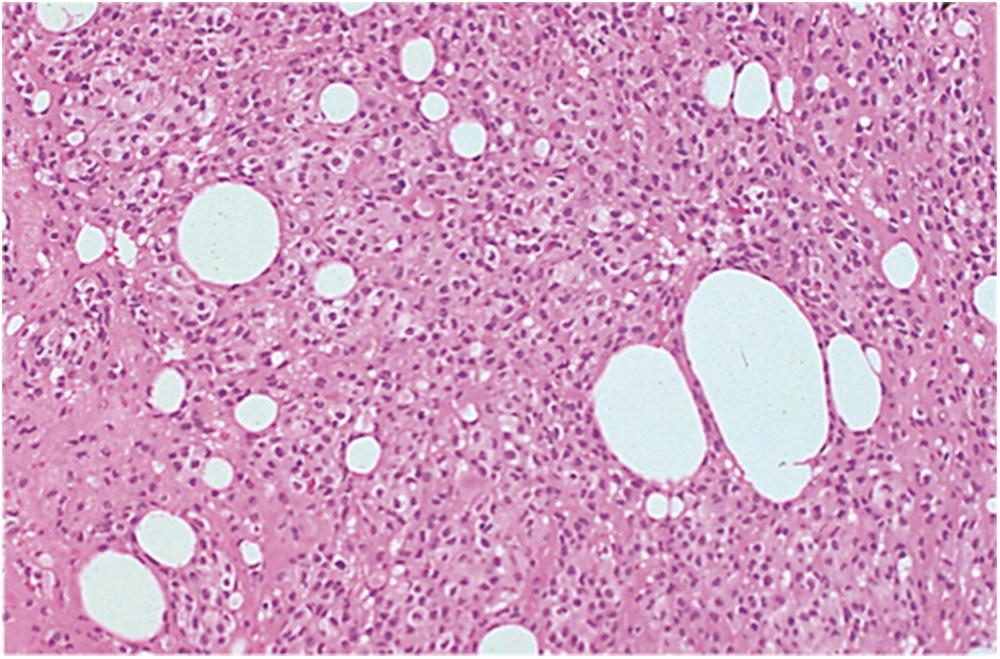
Grossly, the tumor-like lesion is not encapsulated and bulges from the atrial septum ( Fig. 19.11A ). Histologically, there is a mixture of mature and brown fat, which ultrastructurally contains abundant mitochondria and it is distinct from a lipoma because of the presence of brown fat in lipomatous hypertrophy and is therefore a form of hamartoma or hyperplasia , . Entrapped, enlarged myocytes are common and may lead to the false diagnosis of sarcoma, or the brown fat clusters may be mistaken for lipoblasts ( Fig. 19.11B ). The pathologist must remember that fatty masses of the atria, even if large and causing symptoms, are far more likely benign than malignant, as liposarcomas of the heart are vanishingly rare.
True lipomas of the heart are rare, comprising less than 0.5% of the excised tumor. These tumors may occur anywhere in the heart, with a predilection for the epicardium or the endocardium. Most are epicardial tumors. Occasionally, they are multiple . If small, they are usually an incidental finding at autopsy; larger lesions may result in pericardial constriction, heart failure, and sudden death. Histologically, they resemble lipomas of soft tissue, although entrapped cardiomyocytes may be seen . Prognosis is excellent but rare cases of arrhythmias and sudden death have been reported .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here