Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acquired disease of the right-sided cardiac valves is much less common than disease of the left-sided valves, possibly because of the relatively lower pressures and hemodynamic stress to which the right-sided valves are subjected. Indeed, right-sided valvular dysfunction most commonly occurs when morphologically normal valves are subjected to abnormal hemodynamic stresses (e.g., pulmonary hypertension) but can also be seen with congenitally malformed valves (tricuspid and pulmonic valvular abnormalities are part of numerous congenital syndromes; discussed in Section VIII) or with infective endocarditis (discussed in Chapter 49 ). Tricuspid and pulmonic valvular abnormalities are also part of numerous congenital syndromes (discussed in Section VIII).
The normal tricuspid valve has a valve area of 4 to 6 cm 2 . Tricuspid stenosis is uncommon, and most cases are due to rheumatic heart disease. When rheumatic tricuspid stenosis is present, it is generally associated with mitral stenosis, which usually accounts for most of the presenting signs and symptoms. Carcinoid heart disease may also cause tricuspid stenosis, and the signs and symptoms may be mimicked by tumors (myxoma or metastasis), or vegetations that obstruct right ventricular (RV) inflow, particularly those associated with pacemaker leads ( Box 48.1 ).
Rheumatic disease
Right atrial myxoma causing right ventricular inflow obstruction
Metastatic disease causing right ventricular inflow obstruction
Vegetations resulting from endocarditis of pacemaker leads or prosthetic valves
Congenital stenosis or atresia
Carcinoid disease
The symptoms of tricuspid stenosis are mainly due to increased systemic venous pressure that results from a hemodynamically significant tricuspid valve lesion ( Fig. 48.1 ). Peripheral edema, ascites, hepatic enlargement, and right upper quadrant discomfort may develop with chronic tricuspid stenosis or regurgitation. Decreased cardiac output may cause pronounced fatigue, and patients will occasionally complain of the appearance or sensation of the prominent a wave in the jugular veins, which results from increased jugular venous pressure due to impaired RV filling during atrial systole. The murmur of tricuspid stenosis is a low-pitched diastolic murmur at the lower left sternal edge. However, this can be difficult to differentiate from the murmur of mitral stenosis if it is also present. The physical examination may demonstrate the presence of tricuspid stenosis in patients with mitral stenosis, including when there is accentuation of the diastolic murmur during inspiration (as is the case for most right-sided murmurs), a prominent a wave in the jugular venous pulse, or both. An opening snap is occasionally appreciated but may be difficult to distinguish from that of coexistent mitral stenosis. When appreciated, it is usually heard following and more medial to the mitral opening snap.
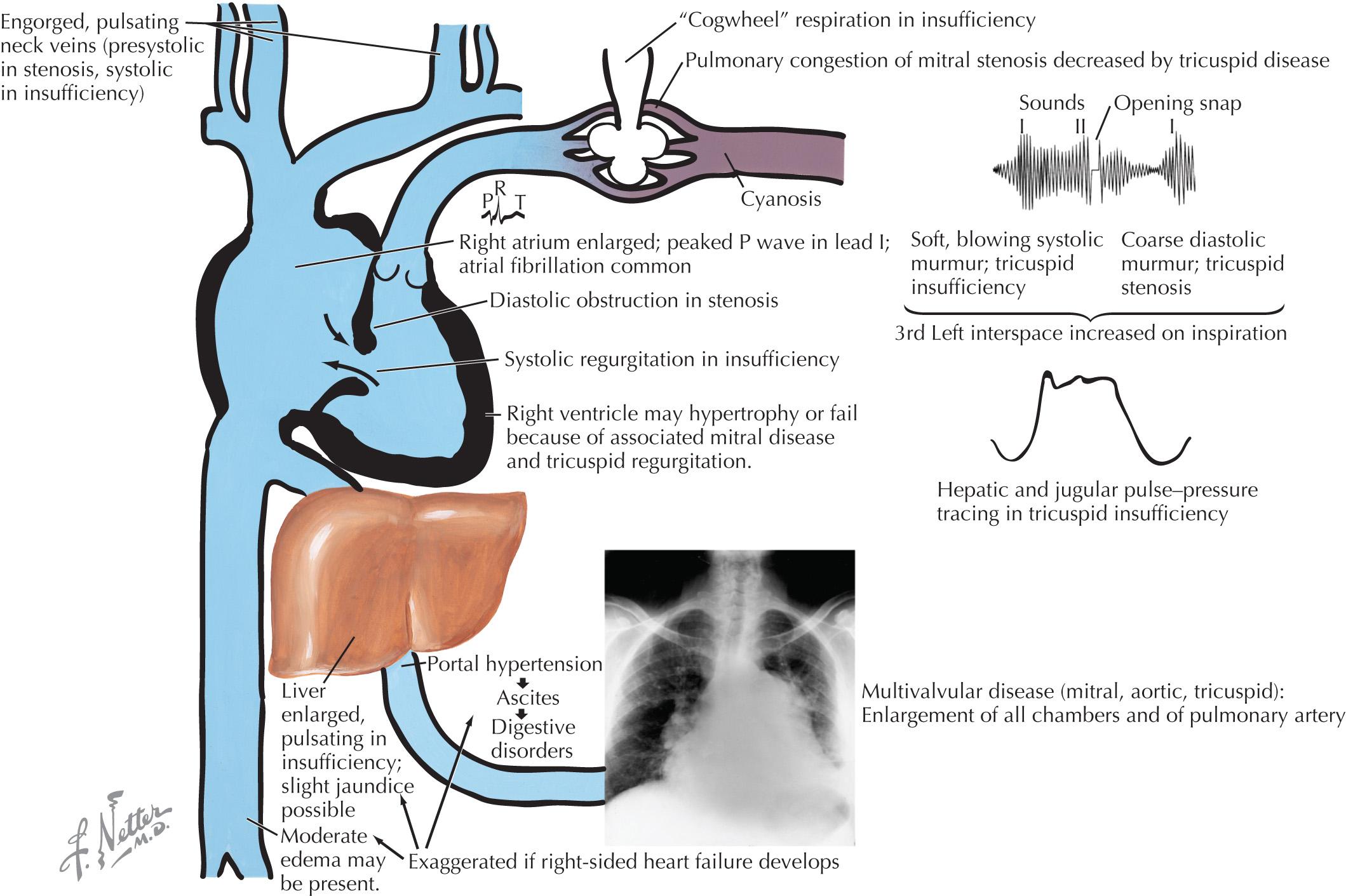
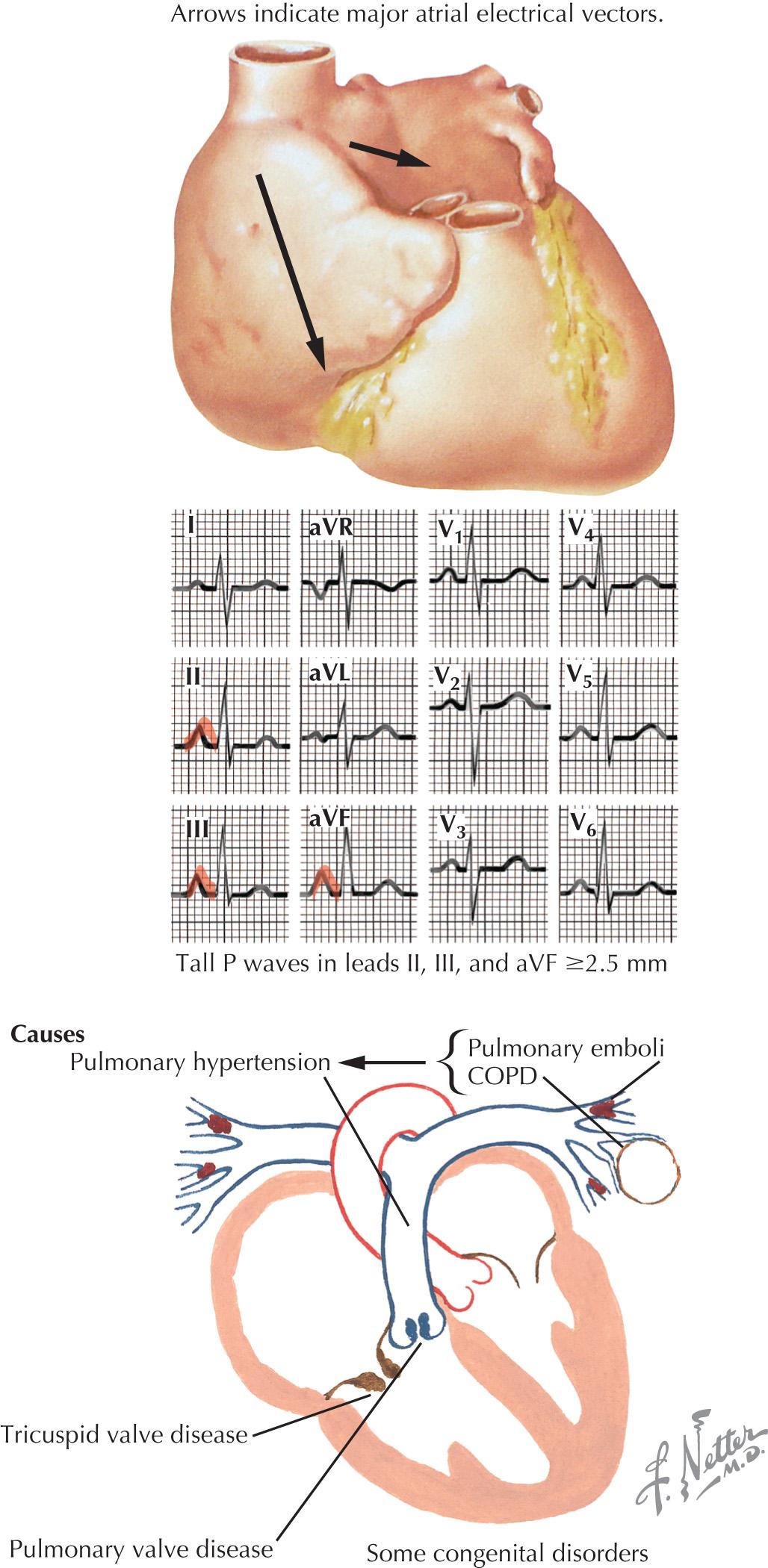
Useful diagnostic studies include chest radiography, ECG, and echocardiography with Doppler evaluation. Right atrial (RA) enlargement is frequently evident on radiographs and manifests on the ECG as a large peaked P wave in lead II ( Fig. 48.2 ). Because of the increased RA pressure, atrial fibrillation is often present.
Echocardiography typically reveals thickened tricuspid leaflets, decreased mobility, scarred chordae, and sometimes doming, if the tricuspid valve leaflets remain pliable. Carcinoid heart disease is associated with a distinctive morphology of a thickened tricuspid valve that is narrowed and fixed in the open position. Doppler evaluation allows estimation of the diastolic pressure gradient by the modified Bernoulli equation. Cardiac catheterization is generally not necessary for the diagnosis of tricuspid stenosis, but when performed, it calls for separate, simultaneous catheters in the RA and the RV. If cardiac output is low, tricuspid gradients may also be low and are not adequately evaluated using a catheter pullback. Clinically significant tricuspid stenosis is usually associated with a valve area of <1.0 to 1.5 cm 2 .
Initial treatment of tricuspid stenosis includes diuretics and nitrates to relieve venous congestion. Refractory cases have traditionally required open tricuspid valve repair or replacement, and the concomitant mitral valve disease has primarily determined the indication and timing for surgery. A surgical approach may also be indicated for debulking of obstructive tumors or myxoma. However, although no randomized trials are available because of the relatively low prevalence of this condition, published studies suggest that percutaneous techniques are effective and safe, either as therapy for isolated tricuspid stenosis or for combined mitral and tricuspid disease; referral to experienced centers should be considered. The most recent American Heart Association/American College of Cardiology guidelines on the management of valvular heart disease state that percutaneous balloon valvotomy may be considered as a treatment option for patients with severe, symptomatic tricuspid stenosis who are inoperable or at an increased surgical risk. However, because percutaneous balloon valvotomy may worsen tricuspid regurgitation, this therapy should not be undertaken if there is more than mild associated tricuspid regurgitation, as is often the case.
Tricuspid regurgitation may be due to primary disease of the valve apparatus or diseases that cause pulmonary hypertension with RV pressure overload and secondary annular dilatation. Annual dilation is the predominant cause of tricuspid regurgitation and can be seen with any condition that causes pulmonary hypertension, including left ventricular failure, mitral regurgitation, mitral stenosis, primary pulmonary disease, and primary pulmonary hypertension. The rare causes of primary tricuspid regurgitation include rheumatic heart disease, myxomatous disease (prolapse), infective or marantic endocarditis, carcinoid heart disease, iatrogenic injury during endomyocardial biopsy or placement of pacemaker or defibrillator leads, and trauma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here