Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Q49.1 Which cells in the skin have vitamin D receptors? In the most general sense, what is the biologic impact of vitamin D on these cells? (Pg. 557)
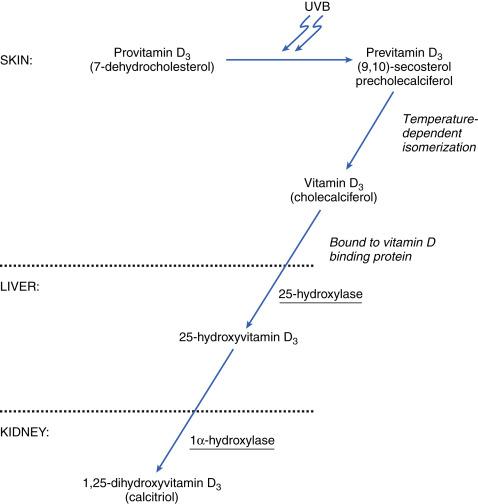
Q49.2 What are the major steps (and sites in the body) for conversion of provitamin D 3 through 1,2-hydroxy vitamin D 3 ? (Pg. 558, Fig. 49.1 )
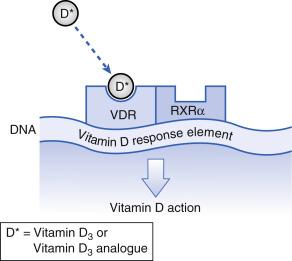
Q49.3 At the molecular level how does vitamin D induce various biologic effects? (Pg. 559)
Q49.4 Which adverse effects limit oral calcitriol use in dermatology and why does topical calcipotriene differ in the risk of these adverse effects? (Pg. 559x2)
Q49.5 How does calcipotriene compare with other vitamin D analogs and topical corticosteroids regarding efficacy in psoriasis therapy? (Pg. 560)
Q49.6 How does the proprietary compounded formulation of calcipotriene and betamethasone dipropionate compare in psoriasis efficacy versus either ingredient alone? (Pg. 561)
Q49.7 What is the impact of ultraviolet radiation on topical calcipotriene and calcitriol? (Pg. 562)
Q49.8 Concerning calcipotriene stability when compounded, (1) which products are compatible, and (2) which products are not compatible with calcipotriene? (Pg. 562)
Q49.9 Which traditional systemic psoriasis therapies can have a significant dose reduction when combined with calcipotriene? (Pg. 562)
Q49.10 In general, for which dermatoses have vitamin D 3 analogs been successfully used in an ‘off-label’ fashion? (Pg. 562)
Q49.11 What is a reasonable maximum weekly dose of calcipotriene to limit the likelihood of hypercalcemia and hypercalciuria? (Pg. 563)
Q49.12 How do topical calcitriol and calcipotriene differ regarding the incidence of (1) photosensitivity, and (2) allergic contact dermatitis? (Pg. 563x2)
1,25 Dihydroxyvitamin D 3
Granulocyte–macrophage colony-stimulating factor
Psoriasis Area and Severity Index
Psoralen plus ultraviolet A
Topical corticosteroid
Ultraviolet A
Vitamin D receptor
Vitamin D is a hormone integral to the maintenance of normal serum calcium and phosphorus levels. Its critical importance in calcium homeostasis is exemplified by rickets, a devastating bone disease. By the turn of the twentieth century, the incidence of rickets had reached epidemic levels in industrialized cities of northern Europe and the northeastern United States. Cities at the time were characterized by heavy pollution and sunless streets. As early as 1882, it was observed that rickets was much less common among children living in rural areas, and it was hypothesized that the disease was caused by lack of sun exposure. About 40 years later, radiographic evidence demonstrated that sunlight alone could cure rickets. Rickets was also noted to improve with ingestion of cod liver oil. Eventually, vitamin D was determined to be the active ingredient in cod liver oil and the entity responsible for the clinical improvement. Subsequently, ultraviolet (UV) radiation was found to be the initiating signal for vitamin D biosynthesis in the skin, completing the loop linking sun exposure, vitamin D, and rickets.
Dermatologic interest in vitamin D centers on the fact that the skin is both (1) a site of initial vitamin D biosynthesis (where 7-dehydrocholesterol is converted to vitamin D 3 in the presence of UV irradiation) and (2) a target organ for vitamin D activity. Q49.1 In the skin, vitamin D receptors (VDR) have been identified in keratinocytes (in the basal and spinous layers of the epidermis), Langerhans cells, melanocytes, fibroblasts, and endothelial cells. The VDR is a nuclear zinc-finger protein that regulates the transcription of target genes. Via the VDR, 1,25 dihydroxy vitamin D 3 (1,25[OH] 2 D 3 ) regulates cutaneous immunity, cell proliferation, differentiation, and apoptosis.
Increased understanding of the immunomodulatory effects of vitamin D 3 and its analogs has paralleled increased knowledge of its mode of action in psoriasis and other inflammatory dermatologic disorders. This knowledge has led to the development of topical formulations of vitamin D 3 and its analogs, which are approved for the treatment of psoriasis and have demonstrated efficacy in other skin diseases.
Although provitamin D 3 (7-dehydrocholesterol; Fig. 49.1 ) is found in plants and animals, dietary sources comprise less than 10% of the vitamin D requirement for most people. Only a few foods, such as oily fish and egg yolks, naturally contain Vitamin D 3 . Additionally, milk, some juice products, and some breads and cereals are fortified with synthetically produced vitamin D 2 (ergocalciferol). The skin has a large capacity to produce vitamin D, and exposure to ultraviolet B (UVB) light is still the most efficient mechanism for producing adequate amounts.
Q49.2 In the epidermis, provitamin D 3 is cleaved by UVB light to form previtamin D 3 (9,10-secosterol precholecalciferol), which is inert. Temperature-dependent isomerization of previtamin D 3 then occurs, generating vitamin D 3 (cholecalciferol) in the skin. Vitamin D 3 is a very labile molecule, and may become inactivated if it does not promptly enter into the circulation. Once in circulation, vitamin D 3 is transported to the liver, where it undergoes hydroxylation by the cytochrome P-450-dependent enzyme 25-hydroxylase to become 25-hydroxyvitamin D 3 . In the kidney (as well as in other tissues such as placenta, pulmonary alveolar macrophages, and bone cells), 25-hydroxyvitamin D 3 is hydroxylated by 1 α -hydroxylase to form calcitriol (1,25[OH] 2 D 3 ), the active hormone. 1α-Hydroxylation is the rate-limiting step in the biosynthesis of 1,25(OH) 2 D 3 , and the activity of this enzyme is tightly regulated by serum levels of calcium, phosphorus, parathyroid hormone, and 1,25(OH) 2 D 3 itself.
Recent studies in human keratinocytes have demonstrated that the keratinocyte is unique in that it contains all the necessary enzymes to convert 7-dehydrocholesterol to active calcitriol. Both 1 α -hydroxylase and 25-hydroxylase have been demonstrated in human keratinocytes, although their physiologic role is still unknown.
The active form of vitamin D, 1,25(OH) 2 D 3 , is metabolized by 24-hydroxylase to 1,24,25-trihydroxyvitamin D 3 , which has very little biologic activity compared with the active form, 24-hydroxylase, which is expressed both in the kidney and in human skin. It is an inducible enzyme; topical application of calcitriol to human skin markedly enhances its activity.
Q49.3 Vitamin D in the form of 1,25(OH) 2 D 3 acts mainly via the VDR to regulate cell proliferation, differentiation, and immune function, as well as calcium and phosphorus metabolism. The VDR protein belongs to the thyroid hormone, corticosteroid, and retinoic acid nuclear receptor gene family. When the VDR is activated by its ligand 1,25(OH) 2 D 3 or the synthetic analogs discussed in this chapter, the drug–receptor complex, in association with the retinoid X receptor-α (RXR-α) binds to specific deoxyribonucleic acid (DNA)-binding sites called vitamin D response elements, with subsequent induction or repression of the gene that contains these elements ( Fig. 49.2 ). Vitamin D inhibits proliferation of keratinocytes in culture and modulates epidermal differentiation. It promotes the formation of the cornified envelope by increasing gene expression and protein levels of involucrin, loricrin, filaggrin, and transglutaminase. Vitamin D has a number of effects on inflammatory markers and immunomodulators, although the physiologic significance of these effects is not fully understood. Vitamin D inhibits production of interleukin (IL)-2, IL-6, and interferon (IFN)-γ by T-helper (Th)1 cells, and IL-17 by Th17 cells. It also blocks transcription of granulocyte–macrophage colony-stimulating factor (GM-CSF) messenger ribonucleic acid (mRNA), and inhibits cytotoxic T-cell and natural killer cell activity. Conversely, vitamin D increases the activity of T regulatory cells and the production of IL-4 by Th2 cells. Additionally, vitamin D contributes to innate immune responses by inducing gene expression of cathelicidin and β-defensin.
Q49.4 Pharmacologic doses of oral 1,25(OH) 2 D 3 can potentially produce substantial hypercalcemia and hypercalciuria, thereby limiting its use for dermatologic indications. Consequently, vitamin D analogs have been synthesized that have a reduced risk of hypercalcemia, but preserve other vitamin D 3 -mediated cellular effects. There are three analogs in widespread use: calcipotriene (originally named calcipotriol), calcitriol, and tacalcitol ( Table 49.1 , Fig. 49.3 ). Double-blind studies have demonstrated greater efficacy of calcipotriene than of calcitriol and tacalcitol. In addition, calcipotriene may be less likely to induce hypercalcemia (with resultant hypercalciuria) than tacalcitol.
| Generic Name | Trade Name | Manufacturer | Generic | Cream | Ointment | Solution | Foam |
|---|---|---|---|---|---|---|---|
| Calcipotriene | Dovonex (US) Sorilux (US) |
Warner Chilcott Mayne |
Yes | 0.005% | No | 0.005% | No |
| Tacalcitol a | (Various in Europe, Asia) | (Various in Europe, Asia) | Yes | 0.0002% b | 0.0002% b 0.0004% c 0.002% b |
0.0002% b | No |
| Calcitriol | Silkis (Europe) Vectical (US) |
Galderma Galderma |
?? Yes |
No No |
0.0003% c 0.0003% |
No No |
No |
| Calcipotriene plus betamethasone dipropionate | Taclonex (US) Enstilar (US) |
LEO Pharma LEO Pharma |
Yes Yes |
No No |
0.005%/0.064% No |
0.005%/0.064% No |
No
0.005%/0.064% |
a Not yet released in the United States.
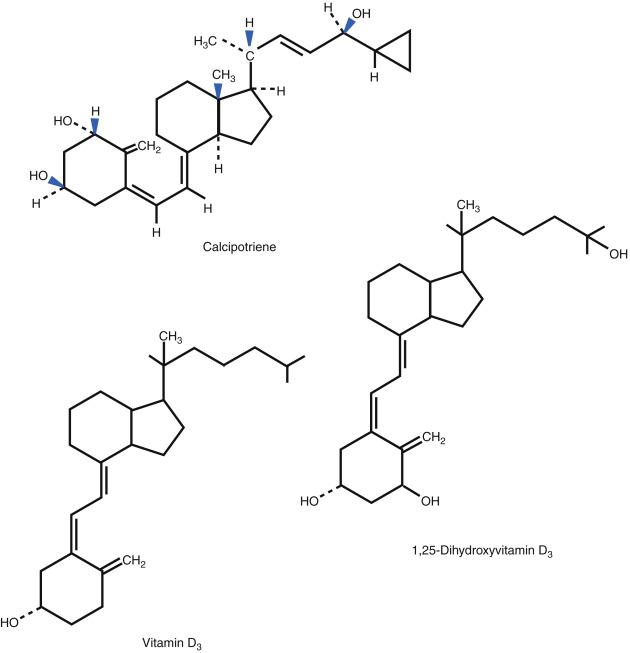
Q49.4 Calcipotriene (calcipotriol) is a synthetic analog of calcitriol. It binds to the VDR with the same affinity as calcitriol, but is less likely to cause hypercalcemia, owing to its rapid local metabolism when applied topically. It is available under the trade names Dovonex cream (USA), Sorilux foam (USA), Calcitrene ointment (USA), Daivonex (Europe, Asia), Psorcutan (Europe), and Dermocal (South America). Only one small, short-duration study has directly compared ointment and cream formulations of calcipotriene; it found that the ointment formation resulted in significantly greater improvement in Psoriasis Area Severity Index (PASI) scores compared with the cream formulation.
Calcitriol is the natural bioactive form of 1,25(OH) 2 D 3 . The drug is available for systemic administration (oral and intravenous routes). It is now available in the United States under the trade name Vectical as a 3 μg/g ointment topically applied twice daily for the treatment of psoriasis.
Tacalcitol (1α,24-dihydroxyvitamin D 3 ) differs structurally from calcitriol in that there is a hydroxyl group at the 24-position, rather than at the 25-position. Like calcipotriene, it has less hypercalcemic activity than calcitriol. It was developed in Japan, where it is available as a 2 μg/g (0.0002%) ointment, cream, lotion, and solution, as well as a 20 μg/g (0.002%) ointment. In Europe, tacalcitol is available as a 4 μg/g (0.0004%) ointment for once-daily application in the treatment of psoriasis. It is not currently available in the United States.
Studies are under way with other topical vitamin D analogs. Two that have undergone placebo-controlled, double-blind studies are topical maxacalcitol (1α,25-dihydroxy-22-oxacalcitriol) and hexafluoro-1,25-dihydroxyvitamin D 3 . Both showed benefit in the treatment of psoriasis, and neither was associated with hypercalcemia. Neither is currently available in the United States.
Box 49.1 lists indications and contraindications for calcipotriene.
US Food and Drug Administration-Approved Indication
Psoriasis
Off-Label Uses
Disorders of keratinization
X-linked ichthyosis
Lamellar ichthyosis
Epidermolytic hyperkeratosis
Sjögren–Larsson syndrome
Autoimmunine dermatoses
Morphea
Vitiligo
Neoplastic diseases
Cutaneous T-cell lymphoma
Miscellaneous dermatoses
Acanthosis nigricans
Confluent and reticulated papillomatosis
Disseminated superficial actinic porokeratosis
Erythema annulare centrifugum
Grover disease
Inflammatory linear verrucous epidermal nevus (ILVEN)
Lichen amyloidosis
Pityriasis rubra pilaris
Prurigo nodularis
Verruca vulgaris
Contraindications
Absolute
None
Relative
Conditions causing hypercalcemia
Pregnancy Prescribing —category C
Calcipotriene is approved for the treatment of plaque-type psoriasis in adults. Early studies were all short term (4–8 weeks). Q49.5 Calcipotriene was superior to vehicle in double-blind controlled studies. It was also superior to calcitriol; tacalcitol; coal tar; combined coal tar 5%, allantoin 2%, and hydrocortisone 0.5%; and short-contact dithranol (anthralin). The effects of calcipotriene are comparable to those of potent topical corticosteroids (TCS), including betamethasone valerate 0.1%, betamethasone dipropionate 0.1%, desoximethasone 0.25%, fluocinonide 0.05%, and halobetasol 0.05%, at 8 weeks of treatment. Calcipotriene applied twice daily is more effective than once-daily application. Twice-daily use is not associated with increased irritation.
In an open and uncontrolled study, patients with psoriasis in the axillary, inguinal, and anal regions were treated with calcipotriene. Calcipotriene proved to be a well-tolerated and effective form of treatment of this psoriasis subset. Half of the patients complained of minimal burning or demonstrated slight lesional or perilesional irritation.
In a multicenter prospective observational cohort study, patients with scalp psoriasis were treated with calcipotriene twice daily over an 8-week period either alone or in combination with TCS or salicylic acid. In this study, 80% of patients showed ‘very good’ or ‘good’ clinical improvement. Combination with other modalities led to an increased treatment response. Calcipotriene proved to be an effective, safe, and well-tolerated treatment modality.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here