Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgments: The author gratefully acknowledges the extensive analysis and expertise of the previous authors of this chapter, including Robert N. Hotchkiss, MD, Peter Amadio, MD, Alex Shin, MD, and Richard J. Smith, MD.
This chapter is intended to provide guidance regarding the treatment of a stiff digit following trauma, primarily with a focus on the metacarpophalangeal (MP) and proximal interphalangeal (PIP) joints. There are numerous resources, including several sections in this book, dedicated to preventing stiffness and maximizing motion after specific injuries such as fractures, tendon lacerations, or burns. This chapter will not replace this specific guidance. Instead, this discussion is dedicated to the treatment of a stiff digit caused by trauma, including the timing, methods, potential pitfalls, and expectations of treatment.
Curtis’s elegant work from 1954 and Smith’s elucidation of intrinsic tightness cannot be improved upon. The detailed, granular record provided by Curtis is an accurate reflection of the complexity and variability of every patient. Reading this work removes any illusions about surgical formulas and reinforces the need for careful analysis and strategies that are designed for each individual. If the reader concentrated on those two masterpieces, little more would be required for a conceptual grasp of the digit’s anatomy, pathologic findings, and reliable strategies for treatment.
The MP joint is a multiaxial condyloid joint that permits motion in the sagittal plane (flexion and extension) and the coronal plane (abduction and adduction), and a slight degree of circumduction. The joint consists of a capsule, two proper collateral ligaments, two accessory ligaments, and a volar plate ( Fig. 10.1 ). The joint capsule is loose and is attached to the crest surrounding the articular surface of the head of the metacarpal and at the base of the proximal phalanx. The redundant capsule allows extensive motion of the proximal phalanx on the metacarpal head and also allows distraction and a minimal amount of rotation.
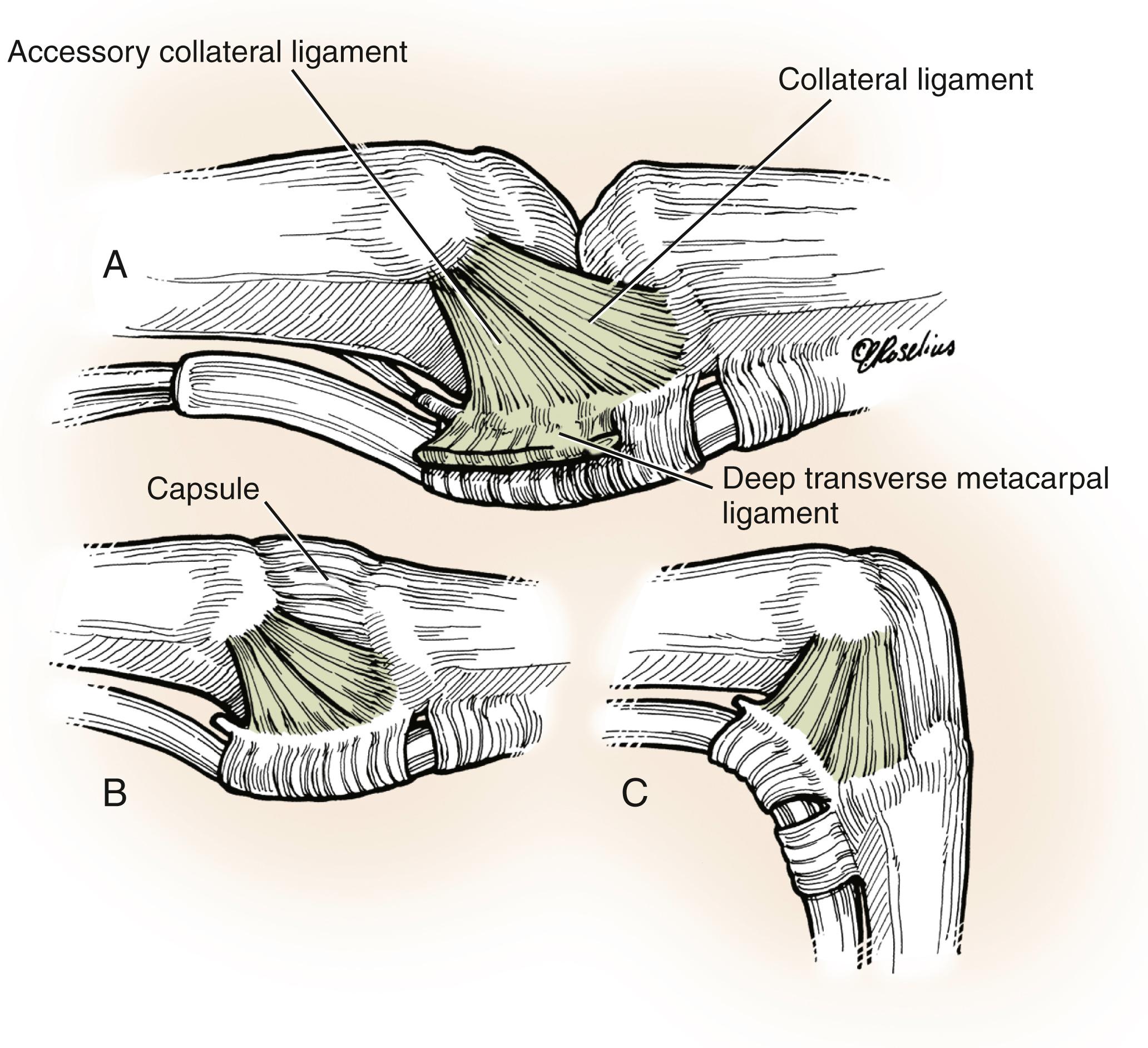
The collateral ligaments are situated on the radial and ulnar aspects of the joint and are quite substantial, 1.5 to 3 mm thick and 4 to 8 mm wide. The collateral ligament arises from the depression in the subcapital area of the dorsal metacarpal head, courses distally toward the volar proximal phalanx, and has a length of 12 to 14 mm. The accessory ligament courses volar to the origin of the proper collateral ligament on the metacarpal head, fans out to blend in with the collateral ligament, and attaches to the proximal phalanx and the volar plate.
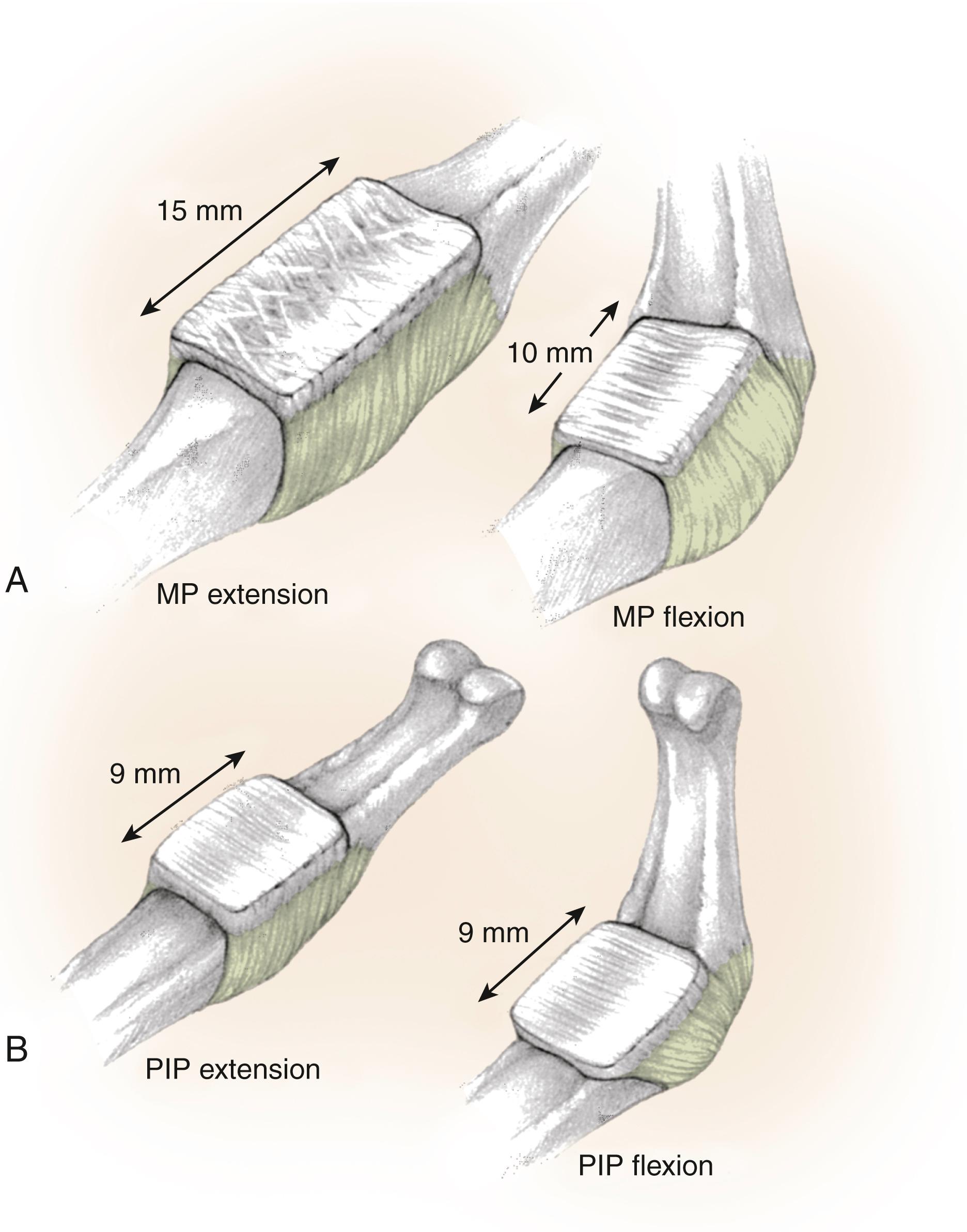
The volar plate is the structure that ultimately restrains hyperextension, which is commonly seen at the MP joint in the ulnar-most digits. The volar plate is composed of crisscrossing fibers that collapse from a fully extended position to a fully flexed position, so its longitudinal length is diminished by a third to half with full flexion, which is notably different than the volar plate structure of the PIP joint. The shape of the metacarpal head is that of a cam with a volar flare. As the proximal phalanx is flexed, the cam and volar flare displace and lengthen the collateral ligaments and thus place them in the position of greatest tension, MP joint flexion, which is also the position of greatest stability. Although the contours of the cam vary slightly from digit to digit, an understanding of this cam effect is essential to understanding MP joint pathologic conditions.
The PIP joint is a hinge or ginglymus joint, the configuration of which facilitates a wide arc of motion in the sagittal plane (flexion and extension) while resisting motion in the coronal plane. The stability of the joint is afforded by the geometry of the articular surfaces as well as the collateral ligaments and volar plate ( Fig. 10.2 ). The PIP joint is supported laterally by two layers of soft tissues. The superficial layer is thin and made of the transverse and oblique fibers of the retinacular ligament of Landsmeer. The deeper and stouter layer is made of the collateral ligaments, which arise from the small recess in the proximal phalanx head and insert into the volar third of the middle phalanx and the volar plate. The accessory ligaments follow a similar path as their MP counterparts but run more obliquely and insert onto the sides of the volar plate. Unlike the MP joint, there is no cam or volar flare of the proximal phalanx head, and the tension of the collateral ligaments is uniform throughout the arc of motion. The volar plate of the PIP joint is also different from that of the MP joint ( Fig. 10.3 ). There are two distinct regions of the volar plate of the PIP joint. , The distal portion is the articular portion, which is fibrocartilaginous and quadrangular in shape, and the proximal portion is thin, compared with that of the MP joint, and membranous. The distal lateral portions of the quadrangularly shaped volar plate form a confluence that anchors the collateral ligament and volar plate to the middle phalanx. On either side of the volar plate, there is an expansion that extends proximally and onto the volar margins of the proximal phalanx. These proximal extensions are volar to the transverse digital artery at the level of the proximal phalanx neck and are variously referred to as checkreins, check ligaments, or swallowtail extensions. , The PIP volar plate, unlike that of the MP joint, does not contract with flexion but slides proximally and distally with flexion and extension of the joint. Thus, any limitation or adhesions of the proximal volar plate or contracture of the checkrein ligaments can result in substantial limitation to PIP extension. Moreover, because the checkrein structure limits hyperextension much more effectively than does the looser arrangement of fibers at the MP joint, the interphalangeal joints typically hyperextend much less than the MP joints. Finally, the dorsal joint capsule is closely connected to the central tendon, which provides a dorsal stabilizing force. The relationship is so intimate that the undersurface of the central tendon undergoes fibrocartilaginous metaplasia and serves as an additional articulating structure for the proximal phalangeal head in flexion. ,
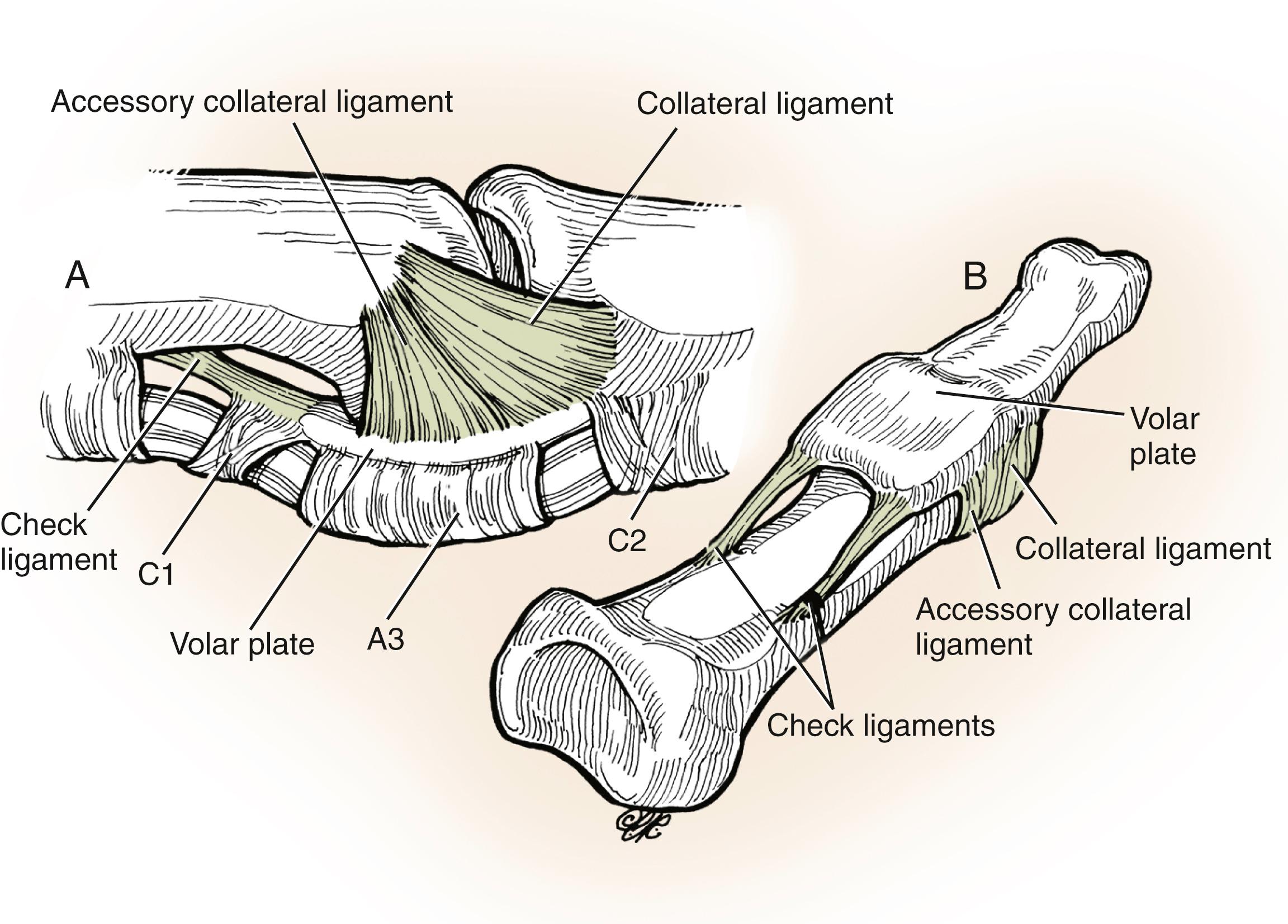
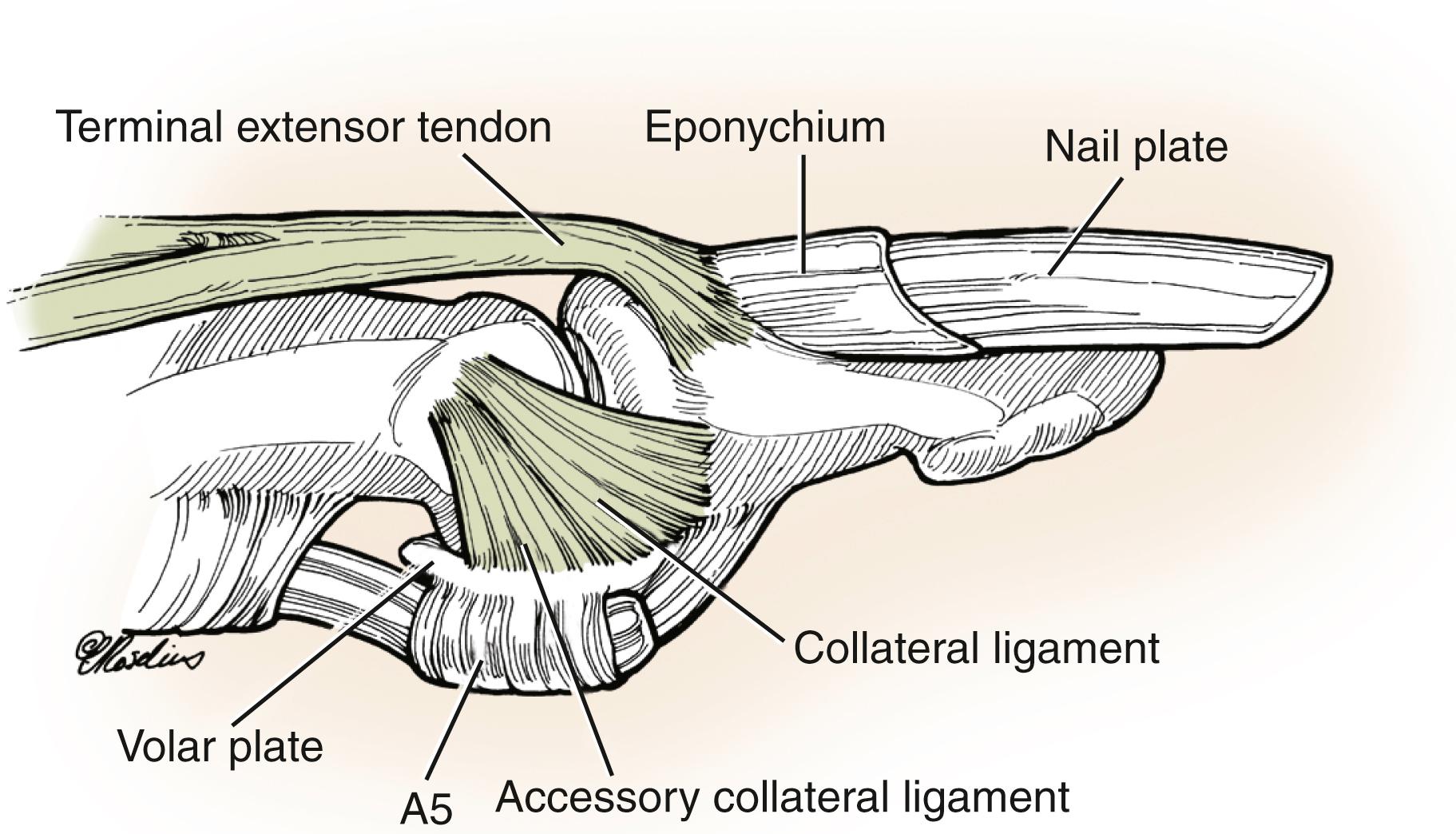
The distal interphalangeal (DIP) joint is also a hinge or ginglymus joint, similar to the PIP joint ( Fig. 10.4 ). The capsule surrounding the DIP joint is reinforced laterally by collateral ligaments that insert into the sides of the head of the middle phalanx and run in a distal and volar direction to insert into the volar lateral tubercle of the distal phalanx. The accessory ligaments are more volar and extend from the sides of the middle phalanx head to the sides of the volar plate. The volar plate serves as an accessory insertion point for the flexor digitorum profundus. Proximally, the plate extends and is attached to the neck of the middle phalanx, but unlike the PIP joint, it does not have lateral volar extensions. Not having checkrein ligaments, the volar plate of the DIP joint can hyperextend. The dorsal aspect of the joint has no reinforcing ligament, but the terminal portion of the extensor mechanism attaches from the dorsal edge of one collateral ligament to the other and blends into the capsular fibers and the periosteum of the distal phalanx.
The anatomy of the hand does not change with time. Although our understanding of the meaning and fine details of that anatomy does, the classic description of the intrinsic system of the hand by the late Richard J. Smith, MD, in previous editions of this textbook, remains, in my opinion, the gold standard. In tribute to Dr. Smith’s enduring contribution to hand surgery, I have preserved his description of the anatomy of the intrinsic system here, in his words.
There are seven interosseous muscles , four dorsal and three volar ( Fig. 10.5 ). The dorsal interossei are abductors. Because the anatomic axis of the hand coincides with the axis of the third metacarpal, the dorsal interossei lie to the radial side of the index and middle fingers and the ulnar side of the middle and ring fingers. The little finger is abducted by the abductor digiti quinti, which functions like an interosseous muscle. The volar interossei are adductors and lie to the ulnar side of the index finger and the radial side of the ring and little fingers. The middle finger therefore has two dorsal interossei (abductors) and no volar interossei (adductors) because the central axis of the hand lies within it. ,
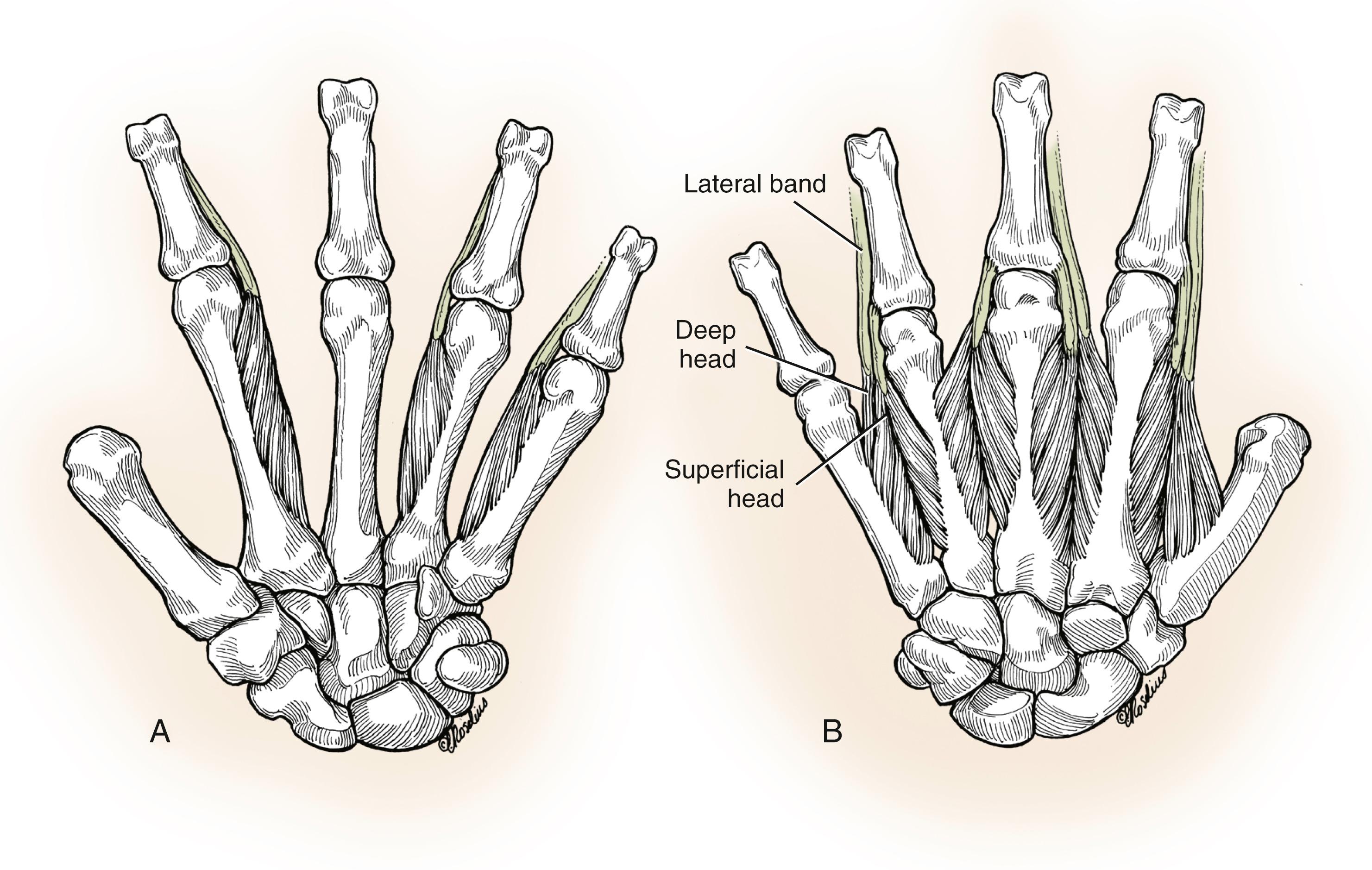
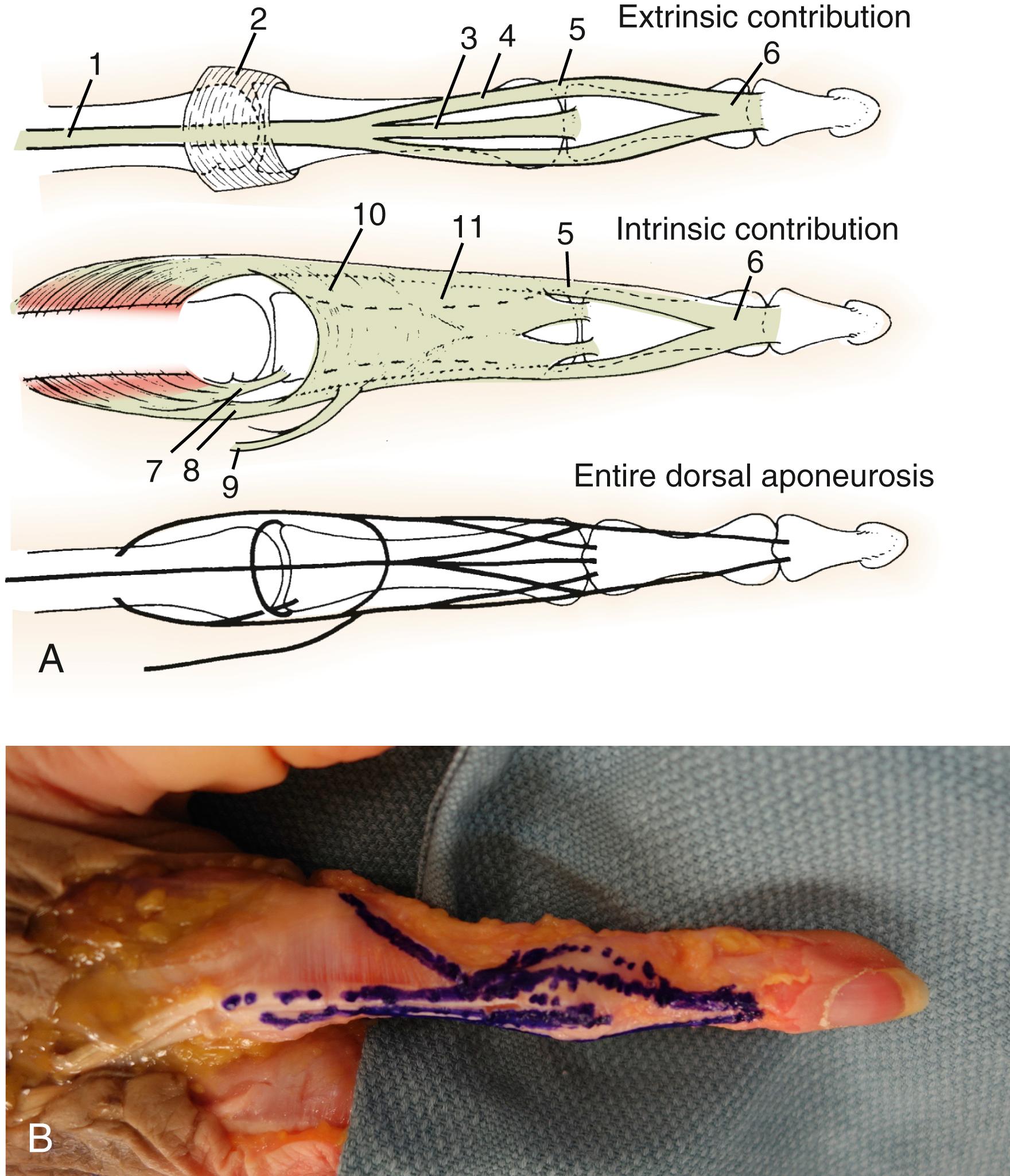
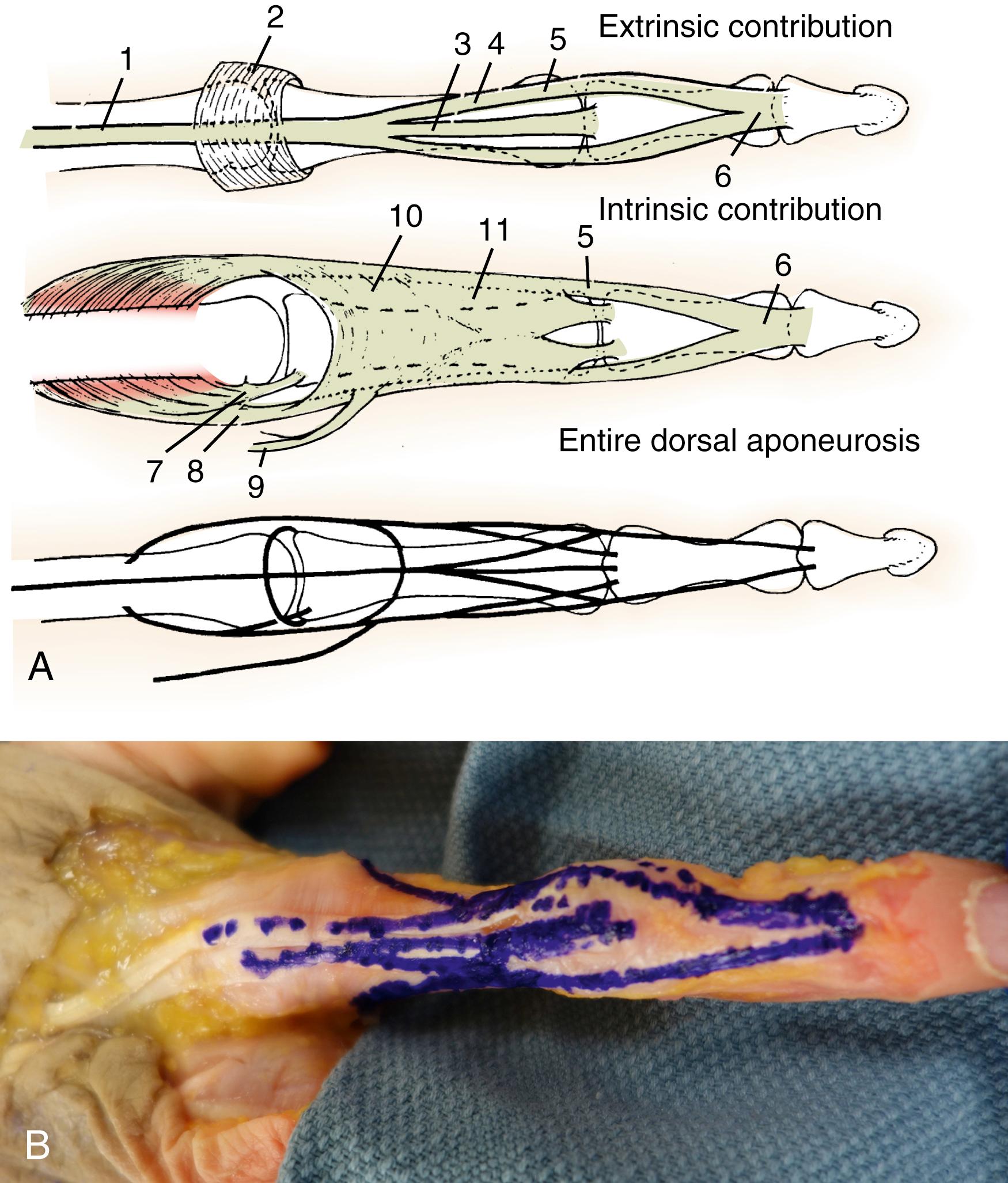
Each dorsal interosseous muscle , with the exception of the third, has two muscle heads. The superficial head arises most dorsally from the shaft of the contiguous metacarpals and is inserted deeply by a medial tendon onto the lateral tubercle of the base of the proximal phalanx. The superficial head abducts and weakly flexes the proximal phalanx. It has no direct effect on the middle or distal phalanges. The deep head of each dorsal interosseous muscle forms a lateral tendon, or lateral band , at the level of the MP joint. The deep head flexes and weakly abducts the proximal phalanx while extending the middle and distal phalanges. At the level of the middle of the proximal phalanx, transverse fibers arch dorsally from each lateral band to join each other over the dorsum of the finger, flexing the proximal phalanx. More distally, oblique fibers (spiral fibers) from the lateral bands sweep over the distal third of the proximal phalanx to insert onto the lateral tubercles at the base of the middle phalanx. The oblique fibers extend the middle phalanx (PIP joint). More distally, the lateral bands are joined by the lateral slips of the extensor tendon to form the conjoined lateral band . The two conjoined lateral bands to each finger unite at the distal third of the middle phalanx to form the terminal tendon . The terminal tendon inserts at the base of the distal phalanx to extend it ( Figs. 10.6 and 10.7 ).
The flexor digiti quinti brevis is structurally and functionally similar to the deep head of the dorsal interossei, forming the ulnar lateral band of the little finger.
The three volar interossei arise from adjacent surfaces of contiguous metacarpal shafts. Unlike the dorsal interossei, each volar interosseous muscle has only one muscle head and none of them insert onto the proximal phalanx. The volar interossei form the ulnar lateral band of the index finger and the radial lateral band of the ring and little fingers. As with the lateral bands of the dorsal interossei, transverse fibers arch over the dorsum of the proximal phalanx and join those of the opposite lateral band to flex the proximal phalanx. They all send oblique or spiral fibers that insert onto the base of the middle phalanx at its lateral tubercle. All lateral bands are joined by the lateral slips of the extensor tendon to form a conjoined lateral band and finally a terminal tendon that extends to the distal phalanx.
Of the hypothenar muscles , the abductor digiti quinti and flexor digiti quinti brevis are similar in both structure and function to the superficial and deep heads of the dorsal interossei, respectively, and arise from the fifth metacarpal. The abductor inserts onto the ulnar lateral tubercle at the base of the proximal phalanx of the little finger. The flexor digiti quinti forms the ulnar lateral band. A third muscle, the opponens digiti quinti , lies deepest. It arises from the pisohamate ligament and the hook of the hamate and inserts onto the ulnar side of the diaphysis of the fifth metacarpal, which it flexes and supinates.
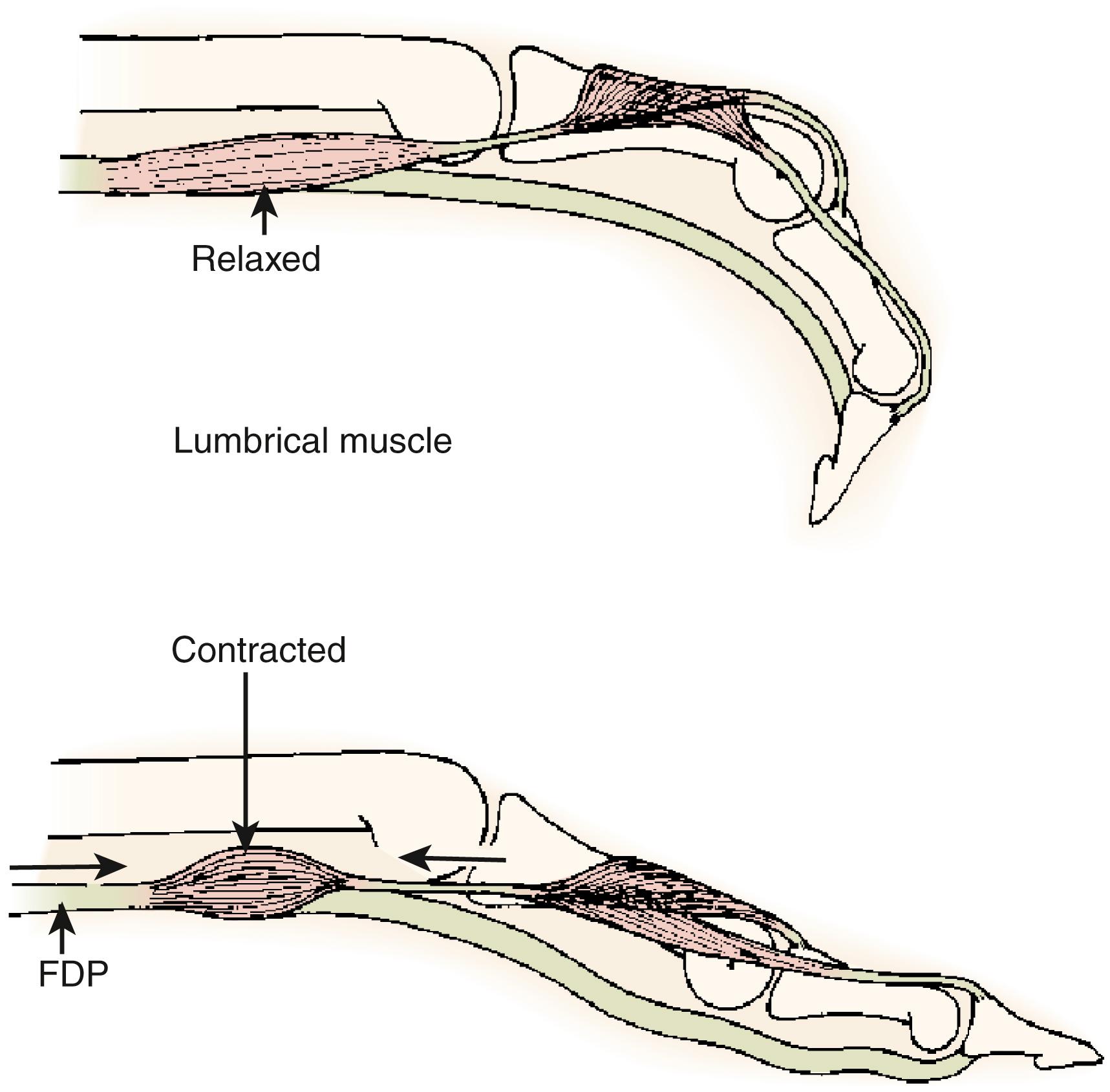
The lumbrical muscles arise from the flexor digitorum profundus tendons in the palm. The lumbricals to the index and middle fingers arise from the radial side of the profundus tendons ( Fig. 10.8 ). The lumbricals of the ring and little fingers arise from the profundus tendons and typically have a head arising from both the radial and ulnar aspect. The tendon of each lumbrical passes volar to the deep transverse metacarpal ligament and joins the radial lateral band at the middle of the proximal phalanx. The lumbricals flex the MP joints and extend the PIP and DIP joints. When a lumbrical muscle contracts, it pulls the profundus tendon distally and the lateral band proximally and thus, lumbrical contraction decreases the force of flexion of the flexor digitorum profundus on the distal phalanx, and it can more effectively extend the interphalangeal joints. , By contrast, when the flexor profundus contracts and the lumbrical contracts as well, interphalangeal joint flexion may be limited (see Fig. 10.8 ).
The extrinsic extensors join the dorsal aponeurosis at the level of the MP joint ( Fig. 10.9 ). The four extensor digitorum communis tendons, the extensor indicis proprius, and the extensor digiti quinti (minimi) proprius tendons are the only extensors of the proximal phalanges. These tendons are loosely tethered to the dorsal joint capsule and the base of the proximal phalanx by a short leash of articular fibers that help hold the extensors at the midline of the MP joint. Normally, the articular fibers have little effect on MP joint extension. In the region of the MP joint, a sling of sagittal (transverse) fibers, the sagittal bands, pass toward the palm from the extensors to insert onto the volar plate and the volar base of the proximal phalanx. The sagittal bands lie deep to the lateral tendons of all the interossei and are superficial to the medial tendon of the dorsal interossei and the joint capsule. When the extensor communis muscle contracts, the extensor tendons lift the proximal phalanx into extension through the sling of sagittal bands. Hyperextension of the proximal phalanx is restricted by the volar plate and the normal tone of the intrinsic muscles of the fingers. Any change in the tendon length can result in a decrease in motion/extension at one or both joints. As tension increases on the extrinsic extensors, pull begins at the MP joint and is then transmitted to the PIP joint. The attachments of the extensor tendon to the MP volar plate preclude further proximal movement of the extensor tendon, and in the event of MP hyperextension, the central tendon cannot fully extend the PIP joint, resulting in an extensor lag. Blocking MP hyperextension will allow adequate proximal movement of the tendon to fully extend the PIP joint. In addition, any skeletal shortening, as may occur with a proximal phalanx fracture, can result in tendon imbalance and resultant PIP joint lag.
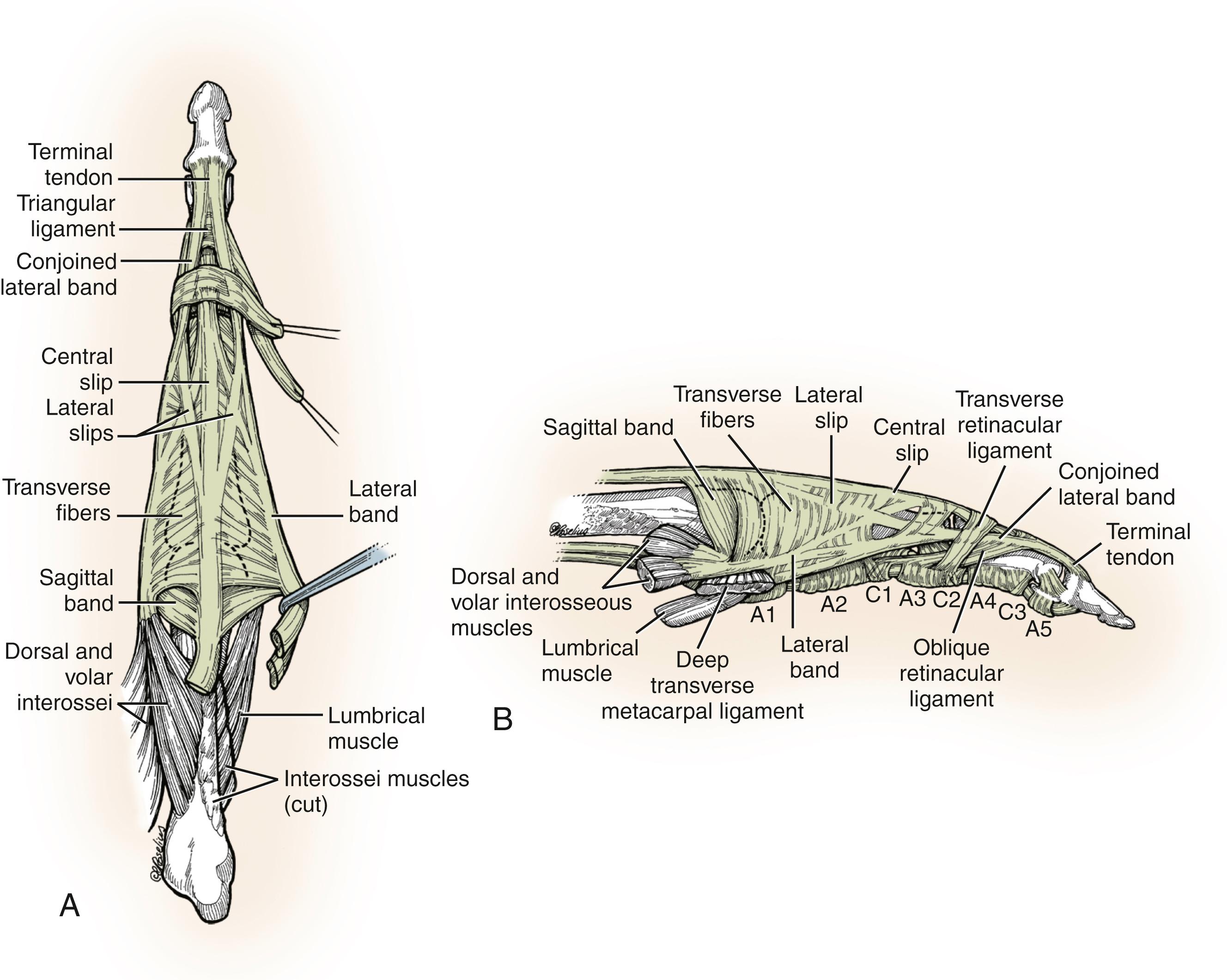
On dissecting the dorsum of the finger, one might confuse the sagittal bands with the transverse fibers. Both structures are directed transversely, and both lie in approximately the same plane at the dorsum of the finger. However, the sagittal bands arise from the extensor tendon at the MP joint and insert into the volar plate and the base of the proximal phalanx to assist in extending the proximal phalanx. The transverse fibers, more distally, arch dorsally from the lateral bands. They are not inserted onto bone, and they flex the proximal phalanx.
Distal to the MP joint, the extensor tendon divides into three slips (see Fig. 10.9 ). The central slip inserts onto the base of the middle phalanx and extends it. The two lateral slips diverge beneath the oblique fibers of the dorsal aponeurosis and join the lateral bands at the distal end of the proximal phalanx. The combined tendon distal to the juncture of the lateral slip and the lateral band is called the conjoined lateral band. The two conjoined lateral bands of each finger join each other proximal to the DIP joint and form the terminal tendon. The conjoined lateral bands are held dorsally by the triangular ligament that passes between them. Thus the borders of the triangular ligament include the medial and lateral tubercles at the base of the middle phalanx and the conjoined lateral bands at its sides. The apex of the triangle is the juncture of the conjoined lateral bands, where they form the terminal tendon. Laterally, the transverse retinacular ligament prevents the bands from bowstringing dorsally. These ligaments extend from the lateral sides of the conjoined bands to the fibroosseous tunnel of the flexor apparatus. , ,
The initial response to nearly any injury to the hand or finger is edema. The injured hand and digit are bathed in a macrophage- and protein-rich fluid that not only encompasses the injured structure but also surrounds and bathes adjacent uninjured structures. Accumulation of edema fluid or hematoma within the layers of tendons, sheaths, and capsular structures of the joint or within the synovial spaces physically limits mobility. , , , The swollen hand assumes a characteristic posture that maximizes the capacity of the joint and comfort of the hand; for the MP joint, this is full extension, and for the PIP joint, this is flexion ( Fig. 10.10 ).
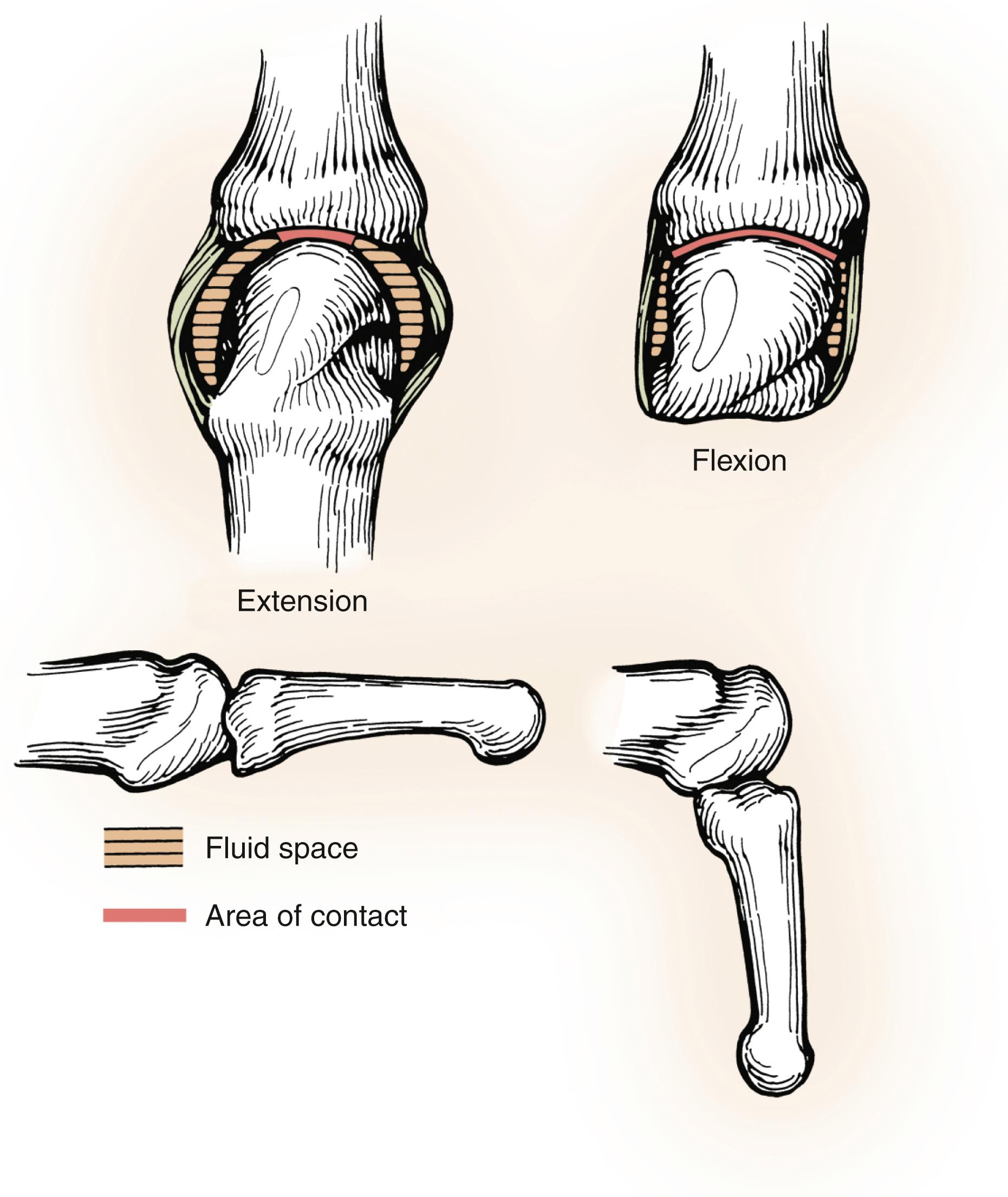
In contrast to the MP joint, the capacity of the interphalangeal joints is affected little by joint position and the hydrostatic effect of edema, although skin tension does have some limiting effect. A PIP joint contracture is the result of an imbalance between the flexor and extensor torque. The posture of resting MP extension following injury has a reciprocal influence on the PIP joint by tipping the finely tuned balance between the extrinsic flexors and extensors in favor of a flexed position. Without intervention, this will predictably progress to a fixed contracture.
The functional demands of the hand obviously vary depending on activity, task, and occupation. However, the basic functions of pinch, grasp, and grip require motion, stability, and strength in the digits. For effective pinch, a stable, well-positioned thumb is crucial. Extremes of movement of the thumb interphalangeal or MP joint are less important for effective pinch than is their stability in a functional position. Some movement of the carpometacarpal (CMC) joint of the thumb may be advantageous but is not crucial. Meeting the thumb at the tip requires MP motion of the index and long fingers, with less motion needed at their PIP joints. In contrast, power grip requires the composite motion of all the MP and PIP joints, especially those of the ulnar three digits. Therefore before embarking on complex and challenging operative attempts to improve mobility of a given digit or joint, a full assessment of need and impact must be undertaken.
The highest priority of function combined with the highest probability of success is seen with attempts to improve flexion at the MP and PIP joints following trauma. Improvement of active and passive flexion of the joints is more likely than improvement of extension (e.g., patients with fixed contractures resulting from intrinsic tightness are excellent candidates for improvement following surgery).
Musicians present a unique and interesting challenge, because different instruments place vastly different demands on the fingers and hands and require an individualistic analysis. Pianists, who play with both hands, can adapt so that little PIP motion is needed, as long as the joint is pain-free. In contrast, musicians who play string instruments need both strength and mobility, especially of the fingering or fretting hand, even including the DIP joint.
If a joint shows signs of posttraumatic arthritis or articular malalignment, there is minimal chance of improvement with capsular release. Therefore, if the joint is in poor condition, contracture release surgery should be avoided. Although implant arthroplasty following posttraumatic stiffness has been successful in the hip, knee, and elbow, this has not been the case for the MP or PIP joints. The reported motion gain is minimal, and implant failure is quite common. Although some limited success has been reported for distraction arthroplasty, at this time a general recommendation regarding this procedure cannot be made.
| Contracture | Lag |
|---|---|
| Passive motion and active motion are both limited | Passive motion is better than active motion |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here