Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The spinal cord is the segment of the central nervous system that lies within the spinal canal caudal to the foramen magnum ( Figs. 5-1 to 5-3 ). The top of the spinal cord is taken to be the plane immediately rostral to the emergence of the C1 nerve roots. The bottom of the spinal cord merges into the filum terminale at approximately the L1-L2 vertebral level. The spinal cord is subdivided into 31 segments: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal.
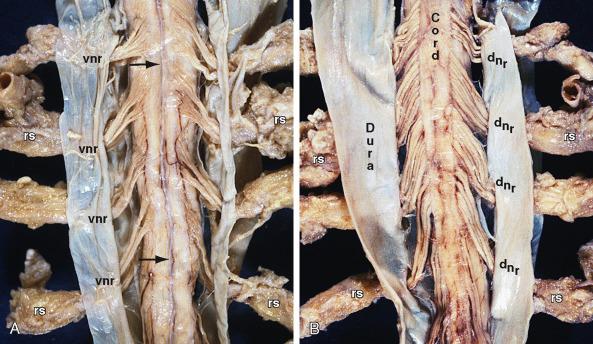

Grossly, the spinal cord is a tubular neural structure situated with the cranial two-thirds of the spinal canal. It is approximately 45 cm long and weighs about 30 g. In cross section, the spinal cord is narrow anteroposteriorly and wide transversely, especially where the cervical and lumbar segments enlarge to innervate the shoulder and pelvic girdles. The cervical enlargement lies at C5-T1, with a maximum circumference at the C6 level (38 cm). The lumbar enlargement occurs at the L2-S3 neural levels, with a maximum circumference at the T12 vertebral level (35 cm). The portion of the spinal cord caudal to the lumbar enlargement tapers to a point, so that the caudal portion is designated the conus medullaris. In the average adult, the caudal tip of the conus medullaris lies at approximately the L1-L2 vertebral level. However, the specific level of termination varies widely (see Imaging, MRI, later in this chapter).
A connective tissue filament, the filum terminale, extends caudad from the conus. The filum terminale is approximately 20 cm long and has two portions. The proximal intradural portion of the filum (15 cm) arises at the precise tip of the conus medullaris and descends through the subarachnoid space to penetrate the precise tip of the arachnoid sac at approximately S2. The distal extradural portion of the filum (5 cm) fuses with the dura and continues through the sacral canal to insert into the dorsum of the first coccygeal segment. As with the conus, the precise level of termination of the dural sac varies widely (see Imaging, MRI, later in this chapter).
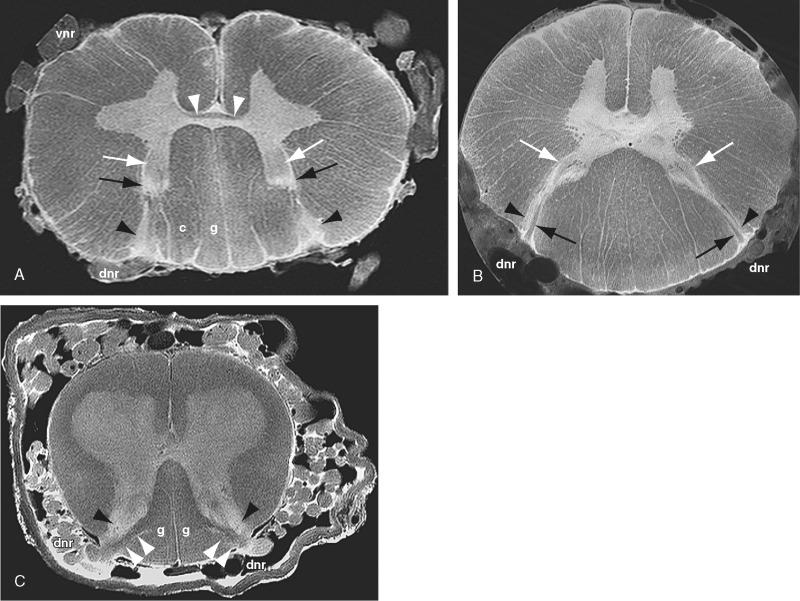
Grossly, the spinal cord is organized as a series of hollow cylinders arrayed concentrically along the length of the cord. From deep to superficial these are the central canal of the cord, the deep gray matter of the cord, and the surrounding white matter. The ratio of gray matter to white matter within each spinal segment varies systematically along the length of the cord ( Fig. 5-4 ). Upper spinal segments show larger proportions of white matter, because they carry the white matter tracts to and from the entire distal cord. Lower spinal segments carry only the white matter for the few segments distal to them. The spinal gray matter is usually sharply delimited from the white matter, except in the cervical cord where strands of gray matter extend into the lateral white matter as the reticular formation.
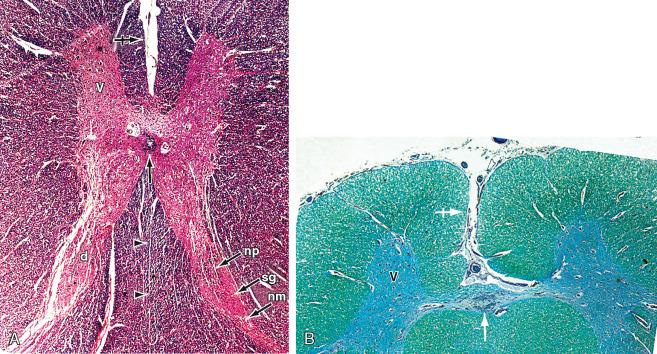
The central canal extends downward from the caudal end of the fourth ventricle into the proximal filum terminale (see Fig. 5-4 ). It is lined by ciliated ependyma and surrounded by neuroglia and a network of fine nerve fibers constituting the substantia gelatinosa centralis. The central canal typically measures less than 1 mm in diameter in youth, partially closes in adulthood, and is mostly obliterated by age 40 years. Within the distal cord and/or proximal filum terminale, the caudal end of the central canal widens into a fusiform “terminal ventricle,” 8 to 10 mm long, that contains less than 1 mL of cerebrospinal fluid. There may be ependymal rests and lumina of abortive accessory canals within the conus medullaris and proximal filum.
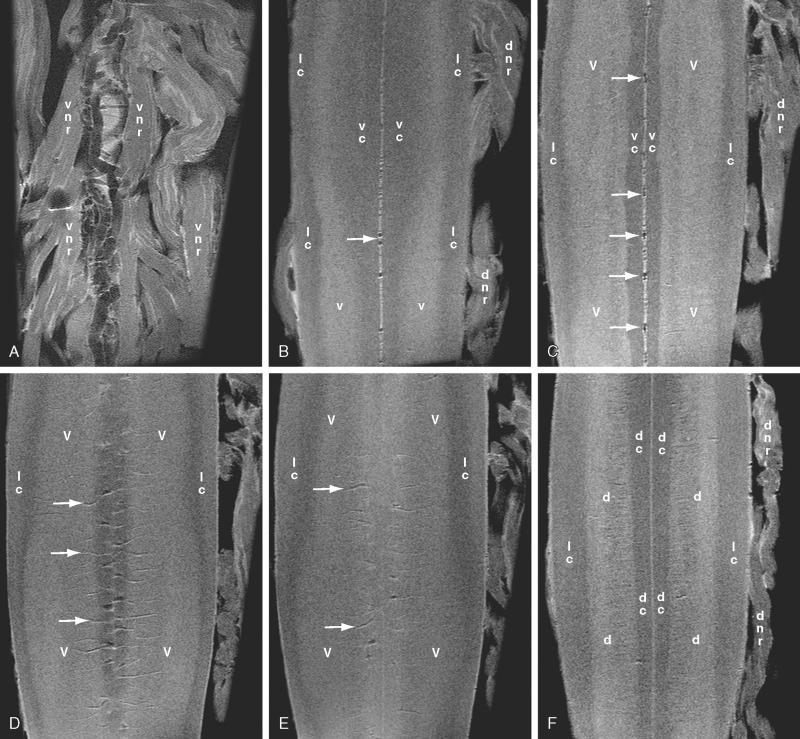
Just external to the central canal, and surrounding it, the longitudinal column of spinal gray matter forms a “fluted gray column” that appears H-shaped in cross section ( Figs. 5-4 and 5-5 ). The ventral arms of the H are the symmetric ventral horns containing motor neurons. The dorsal arms of the H are the symmetric dorsal horns receiving the central fibers of sensory neurons that reside in the dorsal root ganglia. The crossbar of the H is the central gray matter. In the thoracic region, paired additional lateral horns project into the lateral white matter and contain the preganglionic sympathetic neurons. Considered vertically over the length of the spinal cord, the ventral, dorsal, and lateral horns form ventral, dorsal, and lateral columns of gray matter.
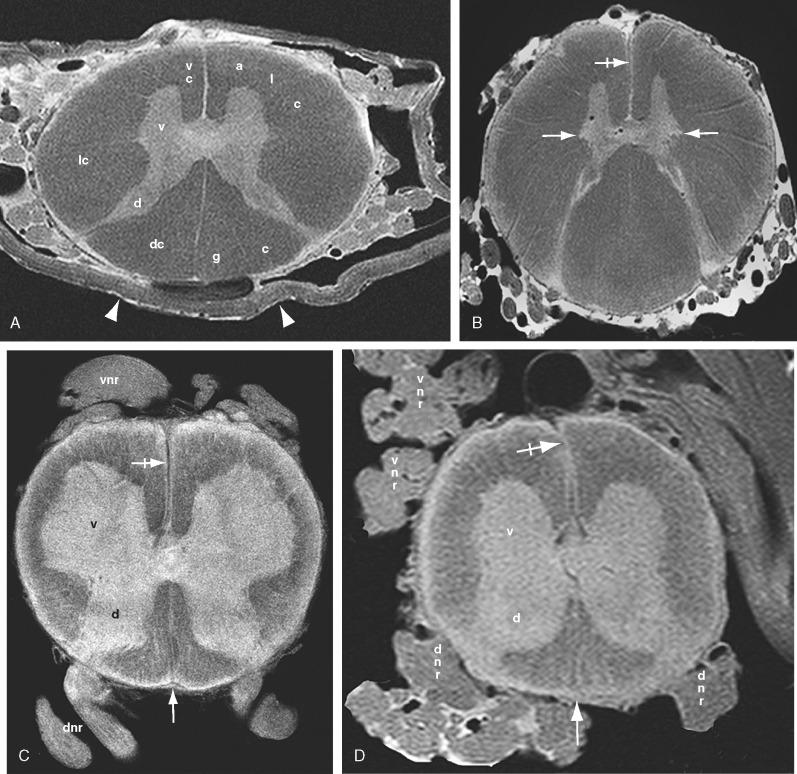
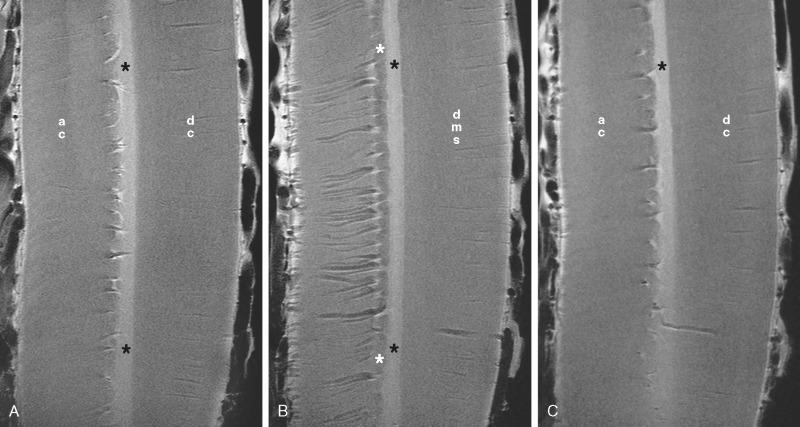
External to the gray matter, the white matter of the spinal cord is subdivided into paired dorsal, lateral, and ventral columns (funiculi) by fissures, septa, sulci, and nerve roots (see Figs. 5-4 and 5-5 ). In the ventral midline, the deep ventral median fissure extends nearly to the central canal, dividing the white matter of the ventral cord into paired ventral columns (anterior columns, anterior funiculi). Anterolaterally, the paired ventrolateral sulci mark the line of exit of the ventral motor nerve roots. The ventral columns are the paired white matter tracts situated to each side of the ventral median sulcus as far laterally as the ventrolateral sulci (including the emerging ventral roots). In the dorsal midline, the shallow dorsal median sulcus and subjacent posterior median glial septum extend nearly to the central canal, dividing the dorsal white matter into paired dorsal columns (posterior columns, dorsal funiculi). Posterolaterally, the paired dorsolateral sulci mark the line of entry of the dorsal nerve roots. The dorsal columns are the paired white matter tracts situated to each side of the dorsal median sulcus and septum as far laterally as the dorsolateral sulci (but not including the entering dorsal roots). At cervical and thoracic levels above T6, a posterointermediate sulcus and septum further divide each dorsal column into a medial fasciculus gracilis and a lateral fasciculus cuneatus. The lateral columns are the white matter tracts situated between the ventrolateral and dorsolateral sulci.
The fibers coursing within the longitudinal columns may cross the midline close to the central canal of the cord via the gray and white commissures. The dorsal and ventral gray commissures are tracts of crossing unmyelinated (hence “gray”) fibers situated just dorsal and ventral to the central canal. The ventral white commissure is a tract of crossing myelinated (hence “white”) fibers situated ventral to the ventral gray commissure and dorsal to the depth of the ventral median fissure ( Fig. 5-6A ).
The ventral motor roots arise from cell bodies situated within the ventral horns of the spinal gray matter. The cell bodies are organized longitudinally into medial, central, and lateral longitudinal cell columns, which supply different groups of muscles. The motor roots emerge into the subarachnoid space through the ventrolateral sulci and course ventrolaterally toward the exiting segmental root sleeves.
At each level the dorsal (sensory) roots arise from cell bodies situated within the dorsal root ganglia in the neural foramina. Each dorsal root ganglion cell gives rise to one short fiber that quickly divides into a central and a peripheral process. The central process (central axon) of the dorsal root ganglion cell passes centrally through the subarachnoid space toward the spinal cord. Multiple central processes arise from each segmental ganglion. These fan out to form six to eight dorsal rootlets that enter the corresponding segment of the spinal cord at the dorsolateral sulcus. As the central processes approach the cord, they become sorted by size and degree of myelination. Larger, more heavily myelinated fibers pass medially to enter the dorsal root entry zone as a medial bundle of central fibers (see Fig. 5-6B,C ). Lightly myelinated and unmyelinated fibers pass laterally to enter the dorsal root entry zone as a lateral bundle of central fibers. Each entering central process bifurcates into ascending and descending branches. Long ascending branches of the medial fibers enter the dorsal columns directly or pass through the medial portion of the dorsal horn to deeper layers of gray matter. Thin lightly myelinated or unmyelinated branches of the lateral fibers enter the dorsolateral tract (fasciculus) of Lissauer (see later).
The peripheral process of the dorsal root ganglion cell courses laterally through the root sleeve toward the sensory receptor. Within each segmental neural foramen, the ventral motor rootlets that arise from the spinal cord unite with the peripheral sensory processes that arise from the dorsal root ganglion distal to (on the far side of) the dorsal root ganglion to form the spinal nerve. Thus, the term nerve signifies the united motor and sensory roots of a segment starting distal to the dorsal root ganglion. In humans, there are 8 cervical nerve roots, 12 thoracic roots, 5 lumbar roots, 5 sacral roots, and 1 coccygeal root. The C1 nerve exits the spinal canal between the foramen magnum and C1, superior to the bony C1 ring. The C8 nerve exits the spinal canal between C7 and T1, superior to the T1 vertebra. All of the subsequent thoracic, lumbar, and sacral roots exit the spinal canal immediately inferior to the pedicles of the same-named vertebrae. That is, the T7 nerve exits the canal immediately under the T7 pedicle via the T7-T8 neural foramen and the L4 nerve exits the spinal canal immediately under the L4 pedicle via the L4-L5 neural foramen. In the upper cervical spine, some nerve roots also emerge directly through the lateral surface of the lateral columns of white matter to form the spinal accessory nerves (cranial nerve XI) that course superiorly through the subarachnoid space and foramen magnum to join the medullary portion of the spinal accessory nerve within the posterior fossa.
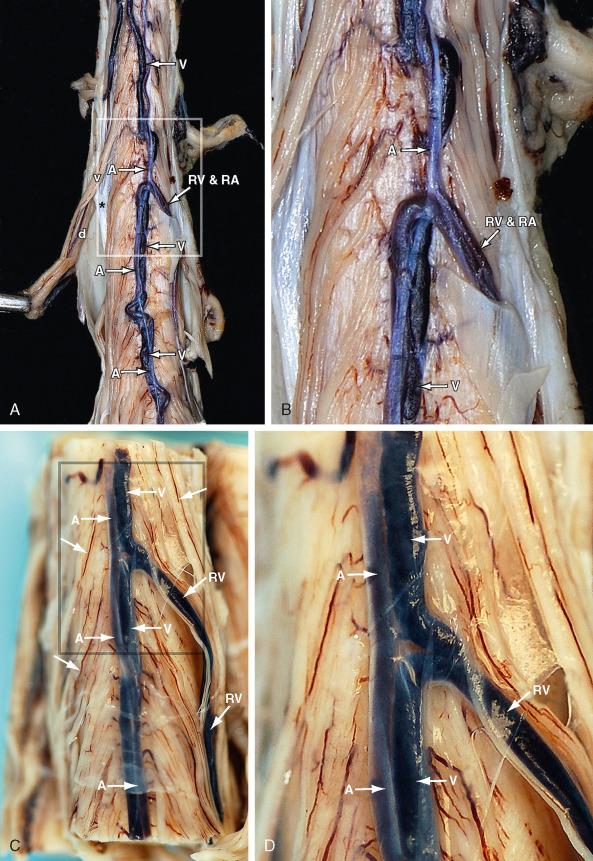
The spinal cord receives its arterial supply from a single anterior spinal axis and paired dorsal and/or dorsolateral arteries ( Figs. 5-1 to 5-3 and 5-7 to 5-9 ). Ventrally, the anterior spinal axis is a long, usually continuous midline trunk that is 0.2 to 0.8 mm in diameter. It arises near the foramen magnum by union of the paired anterior spinal branches of the vertebral arteries and courses caudad within the anterior median fissure. It varies in caliber along its length, being relatively narrow in the thoracic region and widest inferior to the anastomosis with the artery of Adamkiewicz (0.5-1.0 mm). The anterior spinal axis receives supplemental feeders at multiple, irregularly spaced intervals. These typically join the main arterial axis with a hairpin turn. One large feeder entering between C4 and C8 may be designated the artery of the cervical enlargement. The largest supplementary feeder (arteria radicularis magna) typically arises between T9 and T12 and passes to the thoracolumbar enlargement. It may be designated the artery of the lumbar enlargement (i.e., the artery of Adamkiewicz). Within the anterior median fissure, the anterior spinal axis gives rise to numerous sulcomarginal branches that supply the anterior two thirds of the spinal cord, including most of the gray matter and much of the white matter.
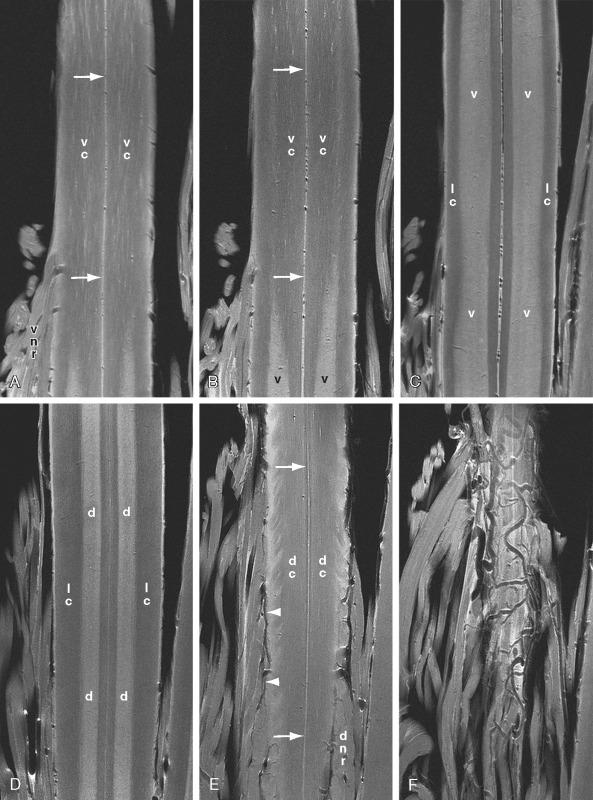
At each feeder, the blood entering the anterior spinal axis is directed both craniad and caudad. This creates multiple less well-vascularized “watersheds” at the junctions of the feeder territories. At these watersheds, therefore, flow within the anterior axis may be markedly reduced or nearly absent.
Dorsally, the paired arterial trunks form a variably complete plexus of longitudinal vessels (<0.5 mm in diameter) that course along the dorsal surface of the cord, either medial to (dorsal spinal arteries) and/or lateral to (dorsolateral spinal arteries) the entry of the dorsal nerve roots at the dorsolateral sulci. The paired dorsal/dorsolateral trunks do not supply the spinal cord directly. Instead they feed into a circumferential pial vascular plexus called the vasocorona. The vasocorona then gives rise to multiple small arterial branches that enter each segment of the cord radially, perpendicular to the circumference of the cord, to supply the posterior one third of the spinal cord.
The venous drainage of the spinal cord is more variable than the arterial supply and shows no real parallelism to the arterial tree ( Figs. 5-2 , 5-3 , and 5-7 to 5-11 ). On the ventral surface, a continuous anterior median spinal vein (0.4-1.0 mm) is located within the ventral median fissure, deep to the anterior spinal axis. This vein is largest in the lumbosacral region and, in 60% to 70% of cases, continues along the filum terminale as a very large terminal vein. The anterior median spinal vein is typically larger than the corresponding anterior spinal axis. The largest vein draining the anterior thoracolumbar cord is designated the great anterior radiculomedullary vein (see Fig. 5-2 ). This is easily mistaken for the artery of Adamkieciwz.
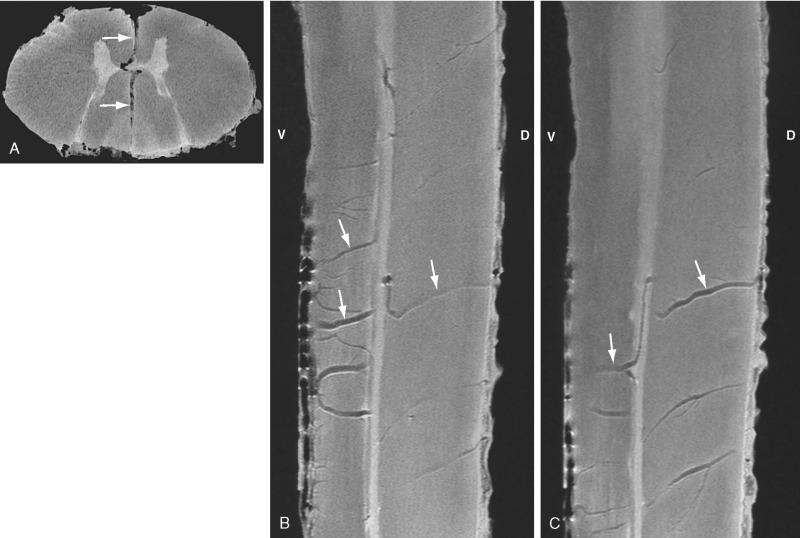

On the dorsal surface, the most nearly constant vein is a large posterior median spinal vein. This is largest rostral to the thoracolumbar enlargement and continues into the cervical region. It is easily recognized because it has a tortuous course at the dorsal aspect of the lumbar enlargement and because there is no posterior midline artery.
A secondary system of short, smaller-caliber veins also courses along the surface of the spinal cord. The most nearly continuous of these are the anterolateral veins, which may replace the median veins wherever the median veins are interrupted. An additional plexus of superficial transverse veins interconnects the longitudinal channels. The intrinsic veins of each segment drain outward, radially, to the superficial venous plexus. Within the spinal cord, true transmedullary anteroposterior venous anastomoses may arise from the ventral median vein, course through the ventral median fissure into the spinal cord, zigzag craniocaudad as they circle around the central canal, and then pass directly outward along the dorsal median septum to enter the dorsal median vein (see Fig. 5-10 ). Such transmedullary venous anastomoses typically ascend rostrally as they pass from ventral to dorsal. They receive few, if any, veins draining from the spinal cord.
The gray matter of the spinal cord is composed of neurons, their terminal axons and dendrites (collectively designated neurites), and the neuroglial support cells. The neurons may be designated intrasegmental if their processes remain within the same spinal segment, intersegmental if their processes extend over adjacent segments, and suprasegmental if their processes extend beyond the spinal cord into the brain. The neurons and neurites of the spinal cord interconnect widely across the midline commissures, so the paired halves of the spinal gray matter form one functional system (see Figs. 5-4 and 5-6A ).
In cross section, the spinal gray matter resembles an H or a “butterfly” with dorsal horns, ventral horns, and lateral horns (at T2-L1 levels only) (see Figs. 5-4 to 5-6 ). The volume of gray matter varies with the spinal level (see Fig. 5-5 ). The gray matter is most extensive at lumbosacral levels, where it supplies the lower extremities, perineum, and pelvis. It is thinnest in the thoracic region, where it supplies only the axial musculature, and second most prominent in the cervical region, where it supplies the shoulder girdle. The broad ventral horns are considered to have a base oriented toward the central canal and a large head that projects ventrolaterally. The narrow dorsal horns have a similar base near to the central canal, a constricted neck, an oval to fusiform head, and an apex that projects dorsolaterally (see Figs. 5-4 to 5-6 ). The junction of the dorsal and ventral horns centrally is designated the intermediate gray matter.
The spinal gray matter contains multiple specific nuclei. The most important of these are discussed below.
Three major cell groups may be identified within the dorsal horns.
The nucleus marginalis (posteromarginal nucleus, marginal zone) is a thin superficial layer of neurons at the apex of the dorsal horn, projecting into the dorsolateral tract of Lissauer (see later). It is present at all levels and has prominent input from cutaneous nociceptors ( Figs. 5-4 , 5-12 , and 5-13 ; see later discussion of Rexed lamina I).
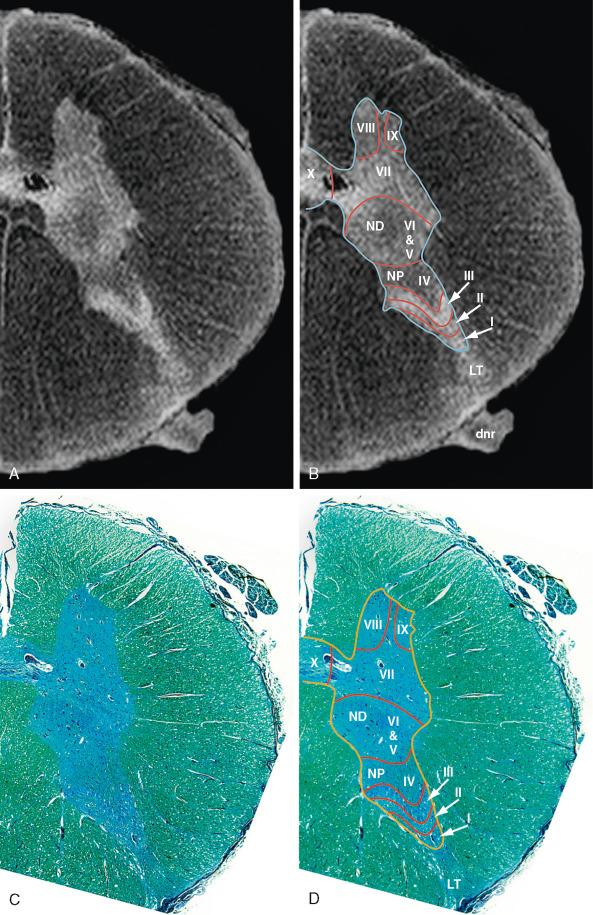
The substantia gelatinosa (of Rolando) lies just deep to the marginal nucleus. It is present at all levels. It receives afferents for pain and temperature from the entering dorsal nerve roots and connects with the spinothalamic tract to convey pain and temperature data onward to the brain (see Figs. 5-4 , 5-6C , 5-12 , and 5-13 ; see later discussion of Rexed laminae II and III).
The nucleus proprius (proper sensory nucleus) is a prominent nucleus situated just deep to the substantia gelatinosa within the dorsal horn. It is present at all levels. It receives sensory impulses for light touch, among other modalities and corticospinal fibers for motor control (see Figs. 5-4 , 5-6 , 5-12 , and 5-13 ; see later discussion of Rexed lamina IV).
Four major cell groups may be identified within the intermediate gray matter.
The nucleus dorsalis of Clarke (nucleus thoracicus, Clarke's column) is found in the gray matter at the base of the dorsal horn, medially, along the length from C8 to L2 or even L3-L4. It is largest in the lower thoracic and upper lumbar levels, where it may bulge medially into the dorsal funiculus (see Figs. 5-12 and 5-13 ). The nucleus dorsalis gives rise to the dorsal spinocerebellar tract (see later discussion of Rexed lamina VII).
The intermediolateral spinal nuclei occupy the lateral horn (column of Terni) that extends from approximately T1 to L2-L3. Neurons in this column send axons into the ventral spinal roots and, via white rami communicantes, to the sympathetic trunk.
An intermediate column of neurons in similar location at S2-S4 gives rise to the sacral preganglionic parasympathetic outflow. However, at this level, the cell column does not project laterally to form a lateral horn.
The intermediomedial column of neurons from T1-L2 receives pain afferents from the viscera.
Three major groups of motor nuclei, designated the medial, central, and lateral longitudinal cell columns, may be identified within the ventral gray matter. These columns extend over multiple segments, either as long columns that are continuous throughout the cord or as island-like aggregations of cells in specific spinal locations.
The medial cell column extends along the length of the spinal cord, except at L5 and S1. The medial motor group innervates the axial musculature of the trunk, including the erector spinae dorsally and the flexors of the trunk ventrally.
The central cell column is found in limited cervical and lumbosacral segments. From C1 to C5-C6, neurons in the central column form the spinal accessory nucleus. At C3-C7, central neurons constitute the phrenic nucleus that innervates the diaphragm.
The lateral cell column is most prominent at the cervical and lumbar enlargements. It innervates the musculature of the upper and lower extremities.
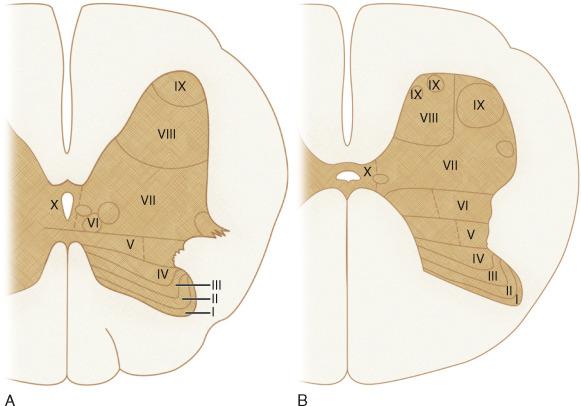
The Swedish neuroscientist Bror Rexed classified the spinal gray matter into 10 cytoarchitectonic zones. These Rexed laminae (RLs) I to X are organized from dorsal to ventral as successive strata of gray matter that extend along most of the length of the cord (see Figs. 5-12 and 5-13 ). RL I forms the most dorsal portion of the dorsal horn. RL IX forms the most ventral portion of the ventral horn, and RL X forms the central gray matter that surrounds the central canal. Integrated over the length of the spinal cord, these laminae may be regarded as 10 long columns of gray matter, layered sequentially, each one cradling the next.
RLs I to VI lie within the dorsal horns. The neurons in these layers receive sensory information entering via the dorsal (sensory) nerve roots and transmit it onward. RL I is a thin layer of marginal cells sometimes designated the marginal nucleus. RLs II and III correspond to the substantia gelatinosa. RL IV contains the nucleus proprius. RLs V and VI give rise to many propriospinal neurons and cannot be distinguished from each other in humans.
RL VII is in the intermediate gray matter and adjoining ventral horn. It contains the nucleus dorsalis of Clarke and the intermediomedial and intermediolateral cell columns.
RL VIII lies within the ventromedial portion of the ventral horn. Many of its neurons send commissural axons to the opposite side of the spinal cord.
RL IX lies within the ventral horn. It contains motor cell columns from which alpha, beta, and gamma motor neurons send their axons into the ventral motor roots to innervate skeletal muscle.
RL X surrounds the central canal.
RLs I to IV are the major reception zones for cutaneous primary afferent nerves and their collateral branches. In turn, these give rise to long afferent tracts that ascend to higher levels and to complex polysynaptic intrasegmental and intersegmental pathways that course ipsilaterally or contralaterally.
RLs V to VI are major reception zones for both primary proprioceptive afferent fibers and corticospinal projections to the spinal cord from the motor and sensory cortices. This anatomic conjunction indicates that these laminae play a substantial role in controlling motor function.
RL VII (lateral portion) has extensive ascending and descending connections with the midbrain and cerebellum for regulating posture and movement. RL VII (medial portion) has numerous propriospinal connections with gray matter segments concerned with movement and autonomic function.
RL VIII is largely composed of propriospinal interneurons that receive ipsilateral fibers from adjacent laminae, commissural fibers from the contralateral RL VIII, and descending fibers from the reticulospinal tract, vestibulospinal tract, and the medial longitudinal fasciculus. It appears to influence and coordinate motor neurons of both the left and right sides.
RL IX contains alpha and gamma motor neurons and many interneurons involved with activity and control of the motor units of striated muscles.
RL X is the gray matter surrounding the central canal plus the dorsal and ventral gray commissures and the substantia gelatinosa centralis.
The spinal white matter contains nerve fibers, neuroglia, and blood vessels. Those nerve fibers that are well myelinated appear white. Nonmyelinated and lightly myelinated nerve fibers appear gray, hence the terms white commissure and gray commissure to indicate different groups of fibers crossing the midline near to the central canal.
The white matter tracts are typically considered in three groups: propriospinal tracts, long ascending tracts, and long descending tracts ( Fig. 5-14 ). The major propriospinal tracts lie immediately external to the gray matter of the spinal cord within each of the ventral, lateral, and dorsal columns. The major ascending tracts include the fasciculi gracilis and cuneatus in the dorsal columns, the spinocerebellar tracts in the lateral columns, and the spinothalamic tracts in adjoining portions of the ventral and lateral columns (“anterolateral” columns). The major descending tracts include the corticospinal and vestibulospinal tracts in the ventral and lateral funiculi, and possibly a minor contribution from the rubrospinal tract in the dorsal portion of the lateral funiculus.
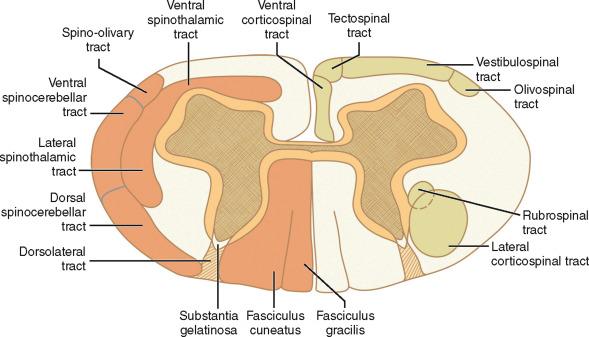
Propriospinal tracts (fasciculi proprii) are intersegmental tracts that arise from neurons in the dorsal and ventral horns, travel in the white matter immediately external to the gray matter, and link nearby and distal segments of the spinal cord to integrate local reflexes into coordinated body movement and visceral function. Most spinal neurons are actually propriospinal neurons and are found predominantly within RLs V through VIII. By definition, the axons of propriospinal neurons remain confined to the spinal cord. Among other roles, the propriospinal system is responsible for the automatic functions that continue after the spinal cord is transected (e.g., sudomotor and vasomotor activities, bowel and bladder function). Many axonal projections of neurons in the substantia gelatinosa (RL II) and in RL VIII stay within the gray matter of their own laminae, so they do not contribute to the propriospinal pathways.
The propriospinal fibers of humans are considered in three groups: ground bundles, the dorsolateral tract (of Lissauer), and the ventral white commissure of the spinal cord.
Ground bundles are fasciculi proprii that descend or ascend within their own fasciculus. The ventral, lateral, and dorsal ground bundles, therefore, lie solely within the ventral, lateral, and dorsal columns, respectively.
The ventral ground bundle extends the length of the cord and is the first spinal tract to myelinate. Within it, individual fibers vary in length from one segment to the full extent of the cord. The shortest fibers lie immediately adjacent to the gray matter. Longer fibers lie more peripherally. All the fibers of the ventral ground bundle terminate in the ventral gray matter throughout the cord.
The lateral ground bundle also extends the length of the cord, but it is particularly well developed in the cervical and lumbar enlargements. The individual fibers arise mainly from the intermediate gray and dorsal gray matter of the cord. The fibers have variable length, course craniad or caudad, pass ipsilateral or contralateral to their cells of origin, and have many collaterals throughout the gray matter.
The dorsal ground bundle comprises only the fine unmyelinated fibers of the fasciculi proprii, which ascend and descend through the posterior white columns. They probably arise from cells of the posterior gray columns and are distributed to the gray matter of the medial part of the posterior gray column.
The dorsolateral tract (of Lissauer) consists of fine myelinated (white) and unmyelinated (hence gray) fibers that surround the entering fibers of the dorsal nerve roots. The tract runs the length of the cord in the dorsolateral zone between the dorsolateral sulcus on the cord surface and the apex of the posterior gray horn. It is best developed in the upper cervical region. The small, less well-myelinated and unmyelinated dorsal root fibers that enter through the lateral portion of the dorsal root entry zone bifurcate into ascending and descending branches that enter the dorsolateral tract. These send collaterals to multiple dorsal horn cells. In addition, the dorsolateral tract contains many propriospinal fibers, including short axons of small neurons of the substantia gelatinosa, which then re-enter the posterior gray column.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here