Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Each lung is divided into lobes surrounded by pleura. There are normally two lobes on the left, the upper and lower, separated by the major (oblique) fissure, and three on the right, the upper, middle and lower lobes, separated by the major (oblique) and minor (horizontal) fissures. The fissures are frequently incomplete, particularly medially, containing localised defects which form an alveolar pathway for collateral air drift and the spread of disease.
For a fissure to be visualised on conventional radiographs, the x-ray beam must be tangential to the fissure. In most people, some of the minor fissure is seen in the frontal projection, but neither major fissure can be identified. In the lateral view, both the major and minor fissures are often identified, but usually only part of any fissure is seen; in fact, it is very unusual to see both left and right major fissures in their entirety.
The major fissures have similar anatomy on the two sides. They run obliquely anteriorly and inferiorly from approximately the fifth thoracic vertebra to pass through the hilum and contact the diaphragm 0–3 cm behind the anterior costophrenic angle. Each major fissure follows a gently curving plane somewhat similar to a propeller blade ( Fig. 2.1 ), with the upper portion facing anterolaterally, and the lower portion facing anteromedially. Owing to the undulating course of the major fissure, either fissure may be seen as two lines on the lateral view. Consequently, it may appear to the unwary that a fissure is displaced when it is, in fact, in its normal position, or both fissures may appear to be in their normal positions when in reality one of them is so displaced that it is no longer visible.

The inferior portion of either or both major fissures may be widened due to fat or pleural thickening between the leaves of the pleura. In these circumstances the contact with the diaphragm will often be broadened and lead to a localised loss of silhouette, an appearance referred to as the juxtaphrenic peak.
With modern multidetector computed tomography (CT), the normal major fissures are frequently visible, but if not clearly defined the position can be inferred from the presence of a relatively avascular zone that forms the outer cortex of the lobe. With high-resolution CT (HRCT), a normal major fissure is seen as a thin line traversing the avascular zone, although it may be represented as two parallel lines on at least one level in approximately one-third of the population because of an artefact related to cardiac and respiratory motion.
The minor fissure fans out anteriorly and laterally from the right hilum in a horizontal direction to reach the chest wall. On a standard chest radiograph, the minor fissure contacts the chest wall at the axillary portion of the right sixth rib. The fissure curves gently, with its anterior and lateral portion usually curving downwards. Because of the curvature of the major fissure described above, part of the minor fissure may be projected posterior to the right major fissure on the lateral view.
On CT the minor fissure position is represented by an oval area of reduced vascularity at the level of the bronchus intermedius ( Fig. 2.2 ; see also Fig. 2.1 ). The normal minor fissure is not seen as a line on axial CT imaging but is apparent on multiplanar reformats.

In 1% of the population an accessory fissure, called the ‘azygos lobe fissure’ ( Fig. 2.3 ), is seen. This fissure contains the azygos vein at its lower end and results from failure of normal migration of the azygos vein from the chest wall to its usual position in the tracheobronchial angle and persistence of the invaginated visceral and parietal pleurae. There is no corresponding alteration in the segmental architecture of the lung, so the term ‘lobe’ is a misnomer. The azygos lobe may, however, be smaller and therefore less transradiant than corresponding normal lung. On CT the altered course of the azygos vein can be seen traversing the lung (see Figs 2.3A to D ). Other accessory fissures are occasionally identified (see Fig. 2.2 ). A minor fissure may separate the lingular segments from the remainder of the upper lobe, similar to the right minor fissure. A horizontally orientated fissure, a superior accessory fissure, may separate the apical segment from the basal segments of either lower lobe. An inferior accessory fissure is sometimes seen in one or other lower lobe, usually the right, separating the medial and anterior basal segments. This fissure runs obliquely upward and medially towards the hilum from the diaphragm.

The inferior pulmonary ligaments are pleural reflections from the mediastinum which hang down from the hila and are analogous in shape to many peritoneal reflections. These two layers of pleura may extend down to the diaphragm or may have a free inferior edge. The intersegmental septum of the lower lobe, a septum within the lung immediately beneath the inferior pulmonary ligament, is often visible on CT ( Fig. 2.4 ). When the inferior pulmonary ligament reaches the diaphragm it may contain a small amount of fat. This may efface the diaphragm, resulting in a juxtaphrenic peak. Otherwise, neither the intersegmental septum nor the inferior pulmonary ligament is visible on plain radiographs.

The trachea is a straight tube that, in children and young adults, passes inferiorly and posteriorly in the midline. In subjects with unfolding and ectasia of the aorta the trachea may deviate to the right and may also bow forward. In cross-section the trachea is usually round, oval or oval with a flattened posterior margin. Maximum coronal and sagittal diameters in adults on plain chest radiography are 21 and 23 mm, respectively, for women, and 25 and 27 mm for men. On CT, which allows precise assessment of diameters and cross-sectional areas without magnification, the mean transverse diameter is 15.2 mm ( sd 1.4) for women and 18.2 mm ( sd 1.2) for men, the lower limit of normal being 12.3 mm for women, and 15.9 mm for men. The diameters in growing children and young adults have been documented. Calcification of the cartilage rings of the trachea is a common normal finding after the age of 40 years, increasing in frequency with age. The trachea divides into the two mainstem bronchi at the carina. In children the angles are symmetrical, but in adults the right mainstem bronchus has a steeper course than the left. The range of angles is wide, and alterations in angle can be diagnosed only by right–left comparisons, not by absolute measurement. The left main bronchus extends up to twice as far as the right main bronchus before giving off its upper lobe division.
The lobar and segmental branching pattern is shown in Fig. 2.5 . There are many variations of the segmental and subsegmental branches. Airways to subsegmental level can be routinely identified on volumetric thin-collimation CT.

The usual method of deciding normal lung density in the frontal view is by comparison with equivalent areas on the opposite side. As this is not possible on the lateral chest radiograph, the detection of subtle densities is more difficult, but the density over the spine should decrease gradually as the eye travels down the spine until the diaphragm is reached. Certain other comparisons can be made, but are less reliable: the density of the high retrosternal areas is approximately equal to that of the area immediately posterior to the left ventricle; the density over the heart is usually similar to that over the shoulders; and, apart from the cardiac fat pads and overlying ribs, there should be no abrupt change in density over the heart shadow.
The segmental bronchi divide into smaller and smaller divisions until, after 6–20 divisions, they become bronchioles and no longer contain cartilage in their walls. The bronchioles divide and the last of the purely conducting airways are known as the terminal bronchioles, beyond which lie the alveoli. The walls of the segmental bronchi are invisible on the chest radiograph unless seen end on, when they may cause ring shadows ( Fig. 2.6 ).

The acinus, which is 5 to 6 mm in diameter, comprises respiratory bronchioles, alveolar ducts and alveoli. The acini are grouped together in lobules of three to five acini, which, in the lung periphery, are separated by septa and together compose the secondary pulmonary lobule. These peripheral interlobular septa, when thickened by disease, are the so-called septal or Kerley B lines.
The bronchopulmonary segments are based on the divisions of the bronchi. The boundaries between segments are complex in shape and have been likened to the pieces of a three-dimensional (3D) jigsaw puzzle; there is no septation between them (except in the rare instance of a patient with accessory fissures). Atelectasis or pneumonia may predominate in one or other segment, but rarely conforms precisely to the whole of just one segment, because collateral air drift occurs across the segmental boundary. The position of the segments as seen on standard radiographs is illustrated in Fig. 2.7 .

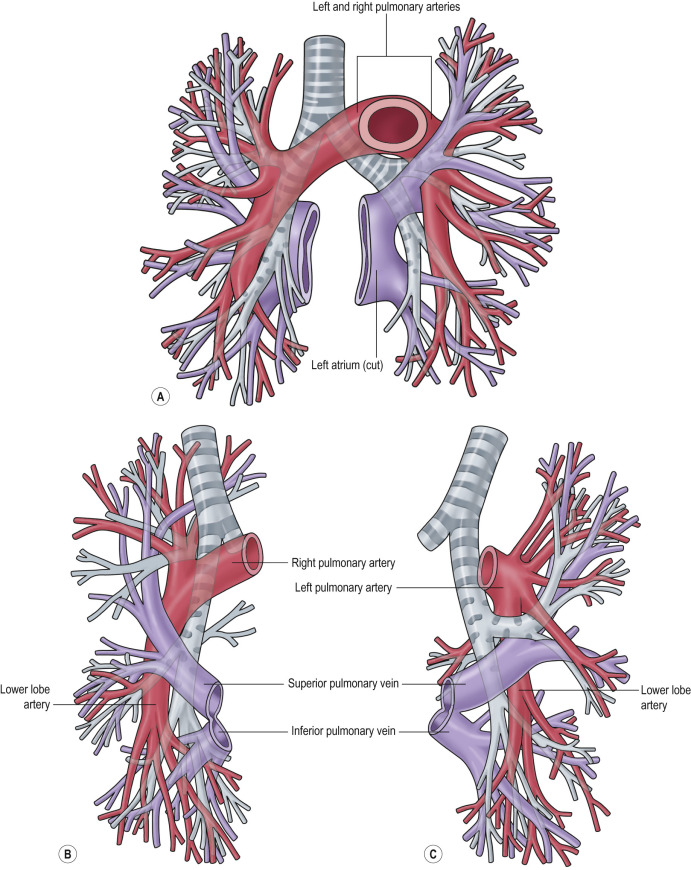
The pulmonary blood vessels ( Fig. 2.8 ) are responsible for branching linear markings within the lungs on both conventional radiographs and CT. It is not possible to distinguish arteries from veins in the outer two-thirds of the lungs on plain radiographs. Centrally, the orientations of the arteries and veins differ: the lower lobe veins run more horizontally and the lower lobe arteries more vertically. In the upper lobes, the arteries and veins show a similar gently curving vertical orientation, but the upper lobe veins lie lateral to the arteries and can sometimes be traced to the main venous trunk, the superior pulmonary vein.

The diameter of the blood vessels beyond the hilum varies with the position of the patient and with various haemodynamic factors. On plain chest radiographs taken in the upright position, there is a gradual increase in the relative diameter of vessels equivalent in distance from the hilum as the eye travels from apex to base. The differences are abolished when the patient lies supine. These observations correlate with physiological studies of perfusion which show that in the erect position there is a gradation of blood flow (the lower zones showing greater blood flow than the upper zones) from apex to base, a difference that is less obvious in the supine patient.
While a general statement regarding these differences in zonal blood vessel size can be made, it is difficult to draw conclusions from the size of any particular peripheral pulmonary vessel. Certain measurements have, however, been suggested for upright chest radiographs:
The artery and bronchus of the anterior segment of either or both upper lobes are frequently seen end on. The diameter of the artery is usually much the same as the diameter of the bronchus (4 to 5 mm). In the authors’ experience, an end-on vessel with a diameter of over 1.5 times the diameter of the adjacent bronchus indicates that the vessel is increased in size.
Vessels in the first anterior interspace should not exceed 3 mm in diameter.
A rich network of lymphatic vessels drains the lung and pleura to the hilar lymph nodes. The subpleural lymphatics are found beneath the pleura at the junction of the interlobular septa with the pleura. These vessels connect with each other and with the lymphatic vessels accompanying the veins in the interlobular septa. Lymph then flows to the hilum via deep lymphatic channels that run peribronchially and in the deep septa of the lungs. In normal circumstances the lymphatic network is invisible radiographically but when thickened the septa are seen as line shadows known as septal or Kerley lines. Thickened interlobular septa correspond to Kerley B lines and thickened deep septa correspond to Kerley A lines.
There are a few intrapulmonary lymph nodes, but they are small and cannot be identified on a chest radiograph but may be seen as small, peripherally located ellipsoid nodules on CT.
This chapter has so far explained the normal anatomy of the lungs and the tracheobronchial tree. The subsequent sections will go into details of the hila structures, mediastinal contents and the relevant anatomy of the diaphragm.
As it will become apparent there are multiple overlapping structures within the thorax that are important to note. This will allow accurate interpretation of the various planar and cross-sectional imaging.
Understanding the normal hilum on plain radiography, CT and magnetic resonance imaging (MRI) requires an appreciation of the anatomy of the major blood vessels ( Figs 2.9 to 2.13 ).




On plain radiograph and CT the densities of the normal hilum are due mainly to blood vessels (see Figs 2.9D to 2.11 and 2.13 ). Normal lymph nodes cannot be recognised as discrete structures, and the bronchial walls contribute little to the bulk of the hila, being thin and easily recognised for what they are. On MRI ( Fig. 2.14 ), the lack of signal from fast-flowing blood within the vessels or from air in the bronchi means that there is relatively little signal generated from normal hilar structures on standard spin-echo sequences. The only signal will be from slow-flowing blood in the vessels (see Fig. 2.14E ), from the bronchial walls and from the fat and hilar nodes. Normal lymph nodes of just a few millimetres in size are often evident as discrete structures on modern multidetector CT. The major points to remember when viewing the hila ( Fig. 2.15 ) are the following:
The transverse diameter of the lower lobe arteries before their segmental divisions can be determined with reasonable accuracy: they measure 9 to 16 mm on the normal posteroanterior (PA) chest radiograph (see Fig. 2.11 ).
The posterior walls of the right main bronchus and its division into the right upper lobe bronchus and bronchus intermedius are outlined by air and appear as a thin stripe on lateral plain radiographs (see Fig. 2.13 ) and on CT (see Fig. 2.12 ). The posterior walls of the equivalent bronchi on the left are rarely visible on the plain radiograph because the left lower lobe artery intervenes between the lung and the bronchial tree. The lung does, in fact, frequently invaginate between the left lower lobe artery and the descending aorta to contact the posterior wall of the left lower lobe bronchus, but this is usually only visible on CT or MRI.
The right pulmonary artery passes anterior to the major bronchi, whereas the left pulmonary artery arches superior to the left main bronchus (see Figs 2.8C, D and 2.9A ). The central portion of the right hilum consists of a combination of the right pulmonary artery and the superior pulmonary vein. As these two vessels are immediately adjacent to one another (on the left, the left main bronchus lies between them), they may be responsible for a density that is sufficiently great to be confused with a mass on lateral plain radiographs and even, on occasion, on CT.
On lateral chest radiographs the angles between the middle and right lower lobe bronchi on the right, and the upper and lower lobe bronchi on the left, do not contain any large end-on vessels; a rounded shadow of greater than 1 cm in these angles is, therefore, unlikely to be a normal vessel.
The pulmonary veins are usually similar on the two sides (see Fig. 2.9 ). However anatomical variation is common; for example nearly 20% of people have an anomalous middle right pulmonary vein. The superior pulmonary vein is the anterior structure in the upper and mid-hilum on both sides. Because, however, the central portions of the pulmonary arteries are so differently organised on the two sides, the relationships of the major veins to the arteries differ. On the right the superior pulmonary vein is separated from the central bronchi by the lower division of the right pulmonary artery, whereas on the left the superior pulmonary vein is separated from the pulmonary artery by the bronchial tree.


Both inferior pulmonary veins travel obliquely anteriorly and superiorly, inferior to the branches of the left lower lobe artery, to enter the left atrium. They are slightly posterior to the plane of the left lower lobe bronchi. They may be seen either end on or in oblique cross-section in PA, lateral and oblique projections and may, therefore, simulate a mass.
The radiographic anatomy of the mediastinum can be described from many points of view, depending on the technique that is under discussion. In this chapter only plain radiographs, CT and MRI will be considered in any detail, CT and MRI being illustrated first because an appreciation of the cross-sectional anatomy of the mediastinum helps in understanding the appearances on plain chest radiographs.
The mediastinum is conventionally divided into superior, anterior, middle and posterior compartments. The exact anatomical boundaries of these divisions are unimportant to the radiologist (indeed, they vary according to different authors), as they do not provide a clear-cut guide to disease and their boundaries do not form any barriers to the spread of the disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here