Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Normal fetal lungs appear homogeneously echogenic on ultrasound surrounding the heart with a cardiothoracic ratio that remains constant through the second and third trimesters.
Pulmonary hypoplasia can be primary or secondary and unilateral or bilateral.
Congenital pulmonary airway malformations (CPAMs) are a spectrum of disorders that include bronchopulmonary malformation, hybrid lesions (CPAM and sequestration), and congenital lobar overinflation/bronchial atresia.
A large fetal lung mass can compress and shift the heart and vena cava, resulting in fetal hydrops.
Congenital pulmonary airway malformation volume ratio (CVR) is the CPAM volume divided by the head circumference. A CVR of 1.6 or less without a dominant cyst is considered low risk for the development of hydrops.
Congenital lobar overinflation (CLO) appears echogenic on ultrasound and can involve a segment or subsegment of lung. CLO accounts for up to 20% of prenatally diagnosed fetal lung malformations.
Congenital diaphragmatic hernias have a variable outcome dependent on severity of lung hypoplasia, liver herniation, and the presence of additional anomalies.
Familiarity with the normal development of the fetal chest is critical both for recognizing chest anomalies and for understanding the consequences of these anomalies. Accurate prenatal diagnosis of thoracic lesions is important in providing appropriate recommendations for counseling, planning potential in utero interventions, and determining the optimal mode of delivery and postnatal care. Prenatal imaging can identify thoracic lesions and assess their impact on mediastinal structures and potential development of hydrops. Although chest abnormalities may be associated with lethal pulmonary hypoplasia, fatal chromosomal abnormalities, and lethal structural anomalies, many chest lesions resolve in utero with minimal sequelae. Fetal magnetic resonance imaging (MRI) can be a useful adjunct in cases with unclear sonographic diagnosis or potential need for in utero interventions.
In the human lung, there are five distinct stages of development, during which the lung matures and the number of alveoli increases. At birth, the lungs are functional but structurally immature; the greatest increase in number of alveoli occurs postnatally. During the first 3 years of life, the alveoli are formed through a septation process that increases the gas exchange surface area. It is important to understand that this lung development process is ongoing, and that space-occupying lesions, or extrinsic abnormalities that do not allow for normal lung growth, can lead to improper lung development.
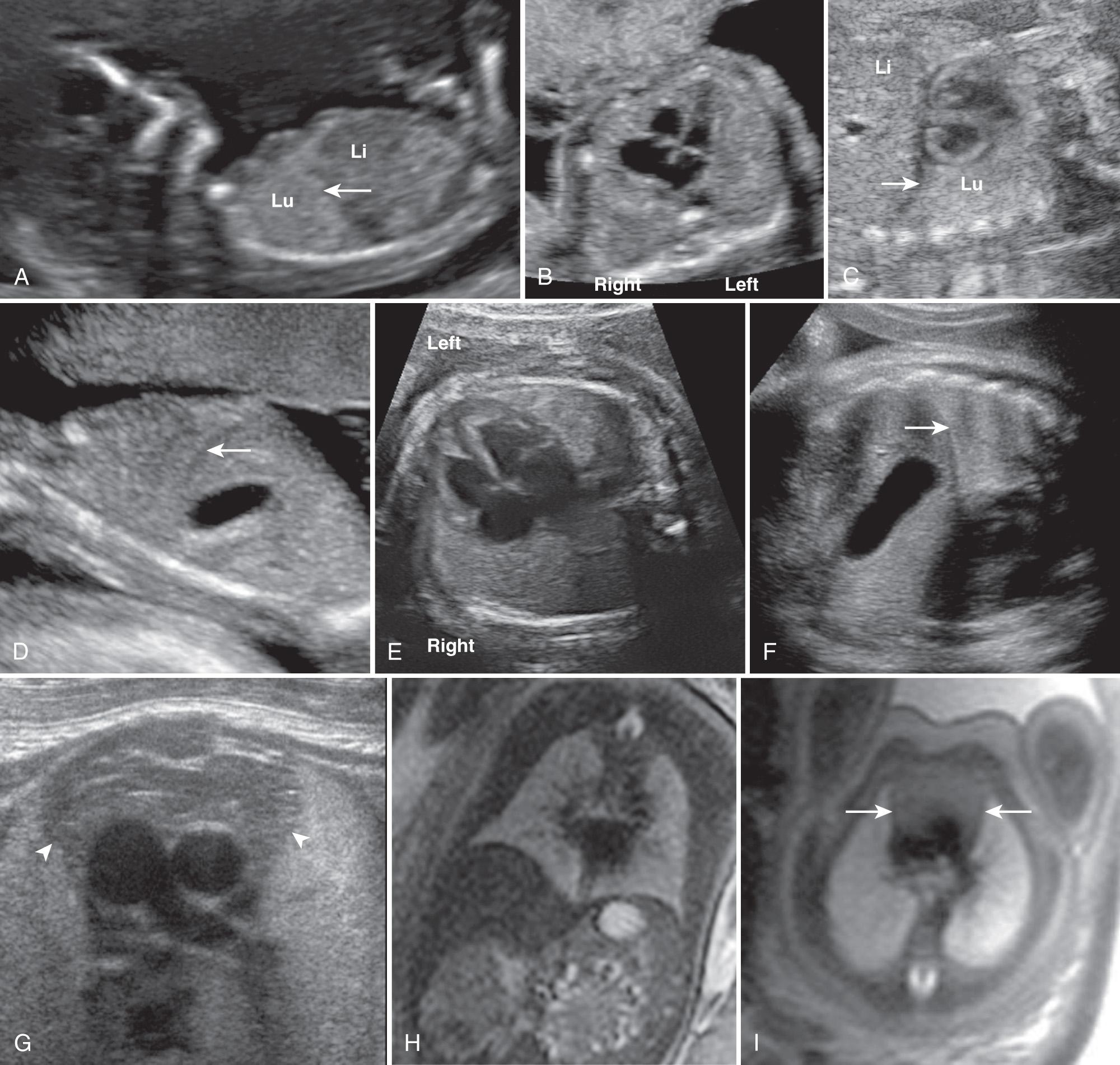
The fetal lungs are identified by ultrasound as homogeneously echogenic tissue surrounding the heart, separated by the hypoechoic, dome-shaped diaphragm from the abdominal organs ( Fig. 36.1A and B ). The fetal ribs are highly echogenic, curved bony structures arising near the spine and extending anteriorly to encompass more than half the thoracic circumference. Lung echogenicity varies during gestation, in general increasing in echogenicity as lung development progresses.
Assessment of lung volume is important for evaluation of fetuses at risk for pulmonary hypoplasia, particularly in cases of congenital diaphragmatic hernia (CDH), pleural effusions, prolonged oligohydramnios, and skeletal deformities. Methods to assess pulmonary size include measurement of the thoracic circumference, lung area (defined as internal thoracic area minus cardiac area in diastole on a transverse four-chamber view ), and three-dimensional lung volumetry with ultrasound or MRI.
The fetal lungs, thorax, and heart grow at similar rates, such that the normal cardiothoracic ratio remains constant in the second and third trimesters. On a normal four-chamber transverse view of the heart, the heart should occupy one-third to one-half the sonographic diameter of the thorax.
Embryonic stage. Extends to about 7 weeks
Pseudoglandular stage. Extends from 6 to 16 weeks; the lungs resemble tubuloacinar glands, with epithelial tubes sprouting and branching into the surrounding mesenchyme
Canalicular stage. Extends from 16 to 28 weeks; the cuboid epithelium differentiates into type I and type II cells, with production of surfactant and formation of the first, thin, air-blood barriers
Saccular stage. Extends from 28 to 36 weeks; the pulmonary parenchyma forms, the surrounding connective tissues thins, and the surfactant system matures
Alveolar stage. Extends from the 36th week of gestation to the first 3 years of life
The cardiac position and axis are constant in normal fetuses. The apex of the heart points left and touches the anterior chest wall. The posterior aspect of the right atrium lies to the right of midline ( Fig. 36.1E ).
Familiarity with the normal anatomy and position of the fetal heart is crucial, along with in utero establishment of the right and left sides of the fetus. The reference to cardiac position and situs is identified by noting that the left atrium lies posteriorly, closest to the spine, and the right ventricle lies anteriorly, closest to the chest wall. Any deviation in the position of the heart should prompt a search for cardiac or pulmonary abnormalities. Anatomy of the fetal heart, including size and position, can be easily influenced by extracardiac thoracic anomalies.
Early in embryogenesis, the narrow pleuroperitoneal duct connects the pleural and peritoneal cavities. The development of the diaphragm, at 9 weeks' gestation, divides the two cavities. The normal diaphragm can be visualized as early as 10 weeks of gestation. The diaphragm appears as a thin, hypoechoic, arched line separating the chest from intraabdominal contents ( Fig. 36.1C-F ). It is best recognized as a dome on each side on sagittal and coronal views, with no difference in the height of the diaphragm on either side. The intact left hemidiaphragm is more easily verified by the presence of the fluid-filled stomach in the abdomen. On the right side, however, meticulous effort is required to identify the hypoechoic linear muscular diaphragm between the liver and lung.
The fetal thymus can be identified as early as 14 weeks' gestation in the anterior mediastinum. By the third trimester, the thymus is visualized as an ovoid, relatively hypoechoic structure ( Fig. 36.1G and I ). The thymus contains spindle-shaped echogenicities that differentiate it from the surrounding echogenic lungs. Thymus size varies greatly during gestation. Thymic imaging and measurements are not performed routinely on prenatal scans. However, prenatal identification and measurement of the fetal thymus is important when DiGeorge syndrome (with thymic aplasia or hypoplasia) is suspected. At times a large thymus will be confused with a mediastinal mass. Homogeneity and lack of mediastinal deviation can help differentiate normal thymus from a mediastinal teratoma or thymic cyst. The normal thymic average transverse measurement is 12 mm at 19 weeks' gestation and 33 mm at 33 weeks. The normal thymic average perimeter is 128 mm at 38 weeks. Acute fetal thymic involution has been reported in association with chorioamnionitis.
Mediastinal teratomas are rare anterior mediastinal complex masses. By ultrasound, the mass is heterogeneous and calcifications may be noted. MRI is a useful adjunct in the assessment of the mass for potential in utero and postnatal surgical treatment. The mass can cause polyhydramnios secondary to esophageal compression, and hydrops due to impaired venous return with resultant fetal demise. Fetal intervention with aspiration of the tumor cyst has been described with a resultant decrease in intrathoracic pressure, which may stop the progression to hydrops and prevent lung hypoplasia. The ex utero intrapartum treatment (EXIT) procedure may be recommended to establish a proper airway at delivery.
Pulmonary hypoplasia is defined as a reduction in the number of cells, airways, and alveoli that results in an absolute decrease in the size and weight of the fetal lungs relative to gestational age. Aplasia is the presence of rudimentary bronchi with no associated lung parenchyma. Agenesis is the complete absence of bronchi, vessels, and lung parenchyma. The earlier the insult to the fetal lungs occurs, the more severe is the degree of pulmonary hypoplasia, aplasia, or agenesis. Pulmonary hypoplasia can result in postnatal respiratory distress and associated high neonatal mortality. Pulmonary hypoplasia can be primary or secondary and can be unilateral or bilateral depending on the cause and time of insult to the lungs. Primary pulmonary hypoplasia is rare and is caused by a primary process in which the lung does not form normally. Unilateral pulmonary agenesis has an incidence of 1 in 15,000 births and is associated with other congenital anomalies. Bilateral pulmonary agenesis is incompatible with postnatal life.
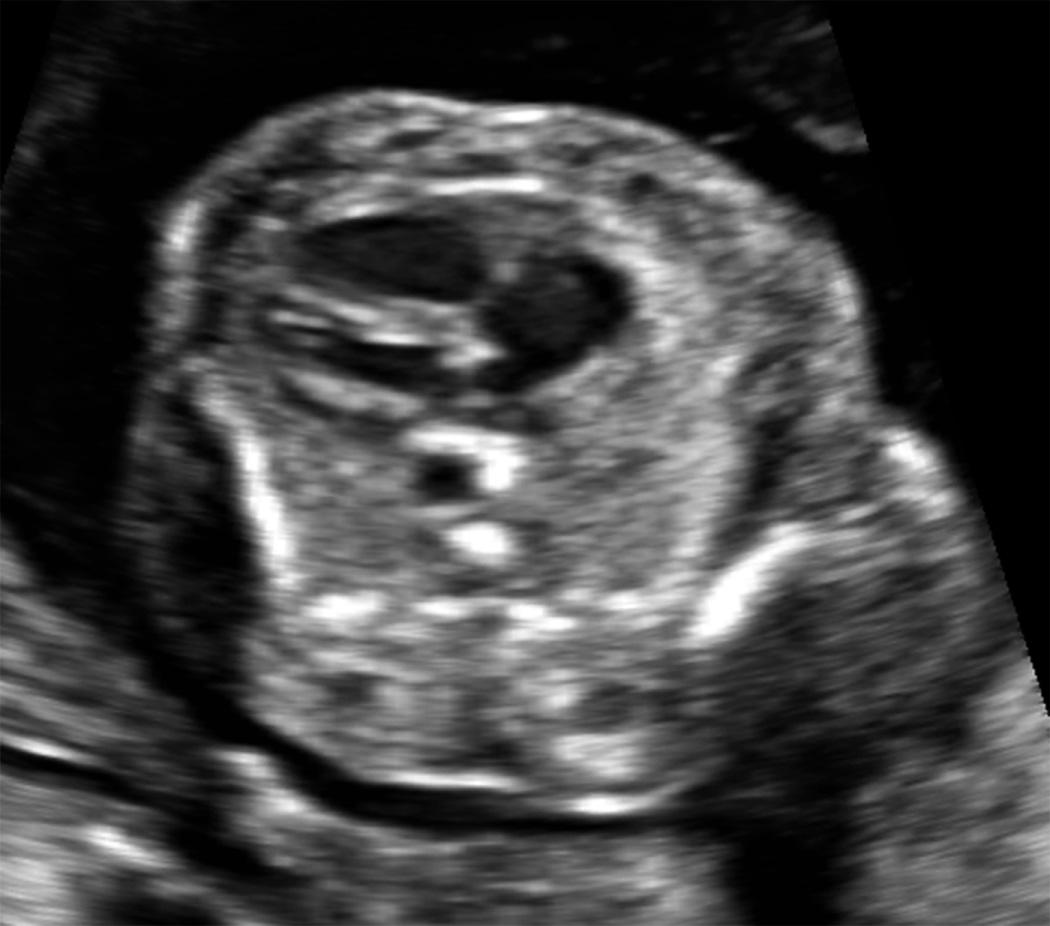
Secondary causes of pulmonary hypoplasia include masses that compress the lungs (e.g., CDH), skeletal malformations that do not allow the lungs to grow (e.g., thanatophoric dysplasia) ( Fig. 36.2 ), and severe prolonged oligohydramnios (e.g., bilateral renal agenesis). Other factors that contribute to pulmonary hypoplasia include hormonal influences, pulmonary fluid dynamics, and abnormal fetal breathing movements. The majority of cases of pulmonary hypoplasia are associated with major structural or chromosomal abnormalities ( Table 36.1 ).
| Main Category | Examples |
|---|---|
| Primary pulmonary hypoplasia or aplasia | Developmental abnormality |
| Thoracic space-occupying process | Congenital diaphragmatic hernia |
| Lung masses | |
| Mediastinal mass | |
| Large pleural effusions | |
| Oligohydramnios | Bilateral renal agenesis |
| Prolonged preterm rupture of membranes | |
| Skeletal anomalies | Skeletal dysplasias |
| Chest wall tumors | |
| Abnormal breathing | Phrenic nerve abnormalities, neuromuscular and central nervous system abnormalities |
| Chromosomal anomalies and syndromes | Trisomy 13, 18, and 21 |
Prenatal prediction of pulmonary hypoplasia and the degree of severity are important for parental counseling as well as for postnatal management planning, particularly if intensive respiratory care is required immediately after birth. Proposed methods for prediction of prenatal pulmonary hypoplasia include estimation of lung volumes by three-dimensional ultrasound or by MRI, thoracic circumference ( Table 36.2 ), lung-to-head ratio, lung-to-body weight ratio, and Doppler studies of pulmonary arteries.
| PREDICTIVE PERCENTILES | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age (Wk) | 2.5 | 5 | 10 | 25 | 50 | 75 | 90 | 95 | 97.5 |
| 16 | 5.9 | 6.4 | 7.0 | 8.0 | 9.1 | 10.3 | 11.3 | 11.9 | 12.4 |
| 17 | 6.8 | 7.3 | 7.9 | 8.9 | 10.1 | 11.2 | 12.2 | 12.8 | 13.3 |
| 18 | 7.7 | 8.2 | 8.8 | 9.8 | 11.0 | 12.1 | 13.1 | 13.7 | 14.2 |
| 19 | 8.6 | 9.1 | 9.7 | 10.7 | 11.9 | 13.0 | 14.0 | 14.6 | 15.1 |
| 20 | 9.5 | 10.0 | 10.6 | 11.7 | 12.9 | 13.9 | 15.0 | 15.5 | 16.0 |
| 21 | 10.4 | 11.0 | 11.6 | 12.6 | 13.7 | 14.8 | 15.8 | 16.4 | 16.9 |
| 22 | 11.3 | 11.9 | 12.5 | 13.5 | 14.6 | 15.7 | 16.7 | 17.3 | 17.8 |
| 23 | 12.2 | 12.8 | 13.4 | 14.4 | 15.5 | 16.6 | 17.6 | 18.2 | 18.8 |
| 24 | 13.2 | 13.7 | 14.3 | 15.3 | 16.4 | 17.5 | 18.5 | 19.1 | 19.7 |
| 25 | 14.1 | 14.6 | 15.2 | 16.2 | 17.3 | 18.4 | 19.4 | 20.0 | 20.6 |
| 26 | 15.0 | 15.5 | 16.1 | 17.1 | 18.2 | 19.3 | 20.3 | 21.0 | 21.5 |
| 27 | 15.9 | 16.4 | 17.0 | 18.0 | 19.1 | 20.2 | 21.3 | 21.9 | 22.4 |
| 28 | 16.8 | 17.3 | 17.9 | 18.9 | 20.0 | 21.2 | 22.2 | 22.8 | 23.3 |
| 29 | 17.7 | 18.2 | 18.8 | 19.8 | 21.0 | 22.1 | 23.1 | 23.7 | 24.2 |
| 30 | 18.6 | 19.1 | 19.7 | 20.7 | 21.9 | 23.0 | 24.0 | 24.6 | 25.1 |
| 31 | 19.5 | 20.0 | 20.6 | 21.6 | 22.8 | 23.9 | 24.9 | 25.5 | 26.0 |
| 32 | 20.4 | 20.9 | 21.5 | 22.6 | 23.7 | 24.8 | 25.8 | 26.4 | 26.9 |
| 33 | 21.3 | 21.8 | 22.5 | 23.5 | 24.6 | 25.7 | 26.7 | 27.3 | 27.8 |
| 34 | 22.2 | 22.8 | 23.4 | 24.4 | 25.5 | 26.6 | 27.6 | 28.2 | 28.7 |
| 35 | 23.1 | 23.7 | 24.3 | 25.3 | 26.4 | 27.5 | 28.5 | 29.1 | 29.6 |
| 36 | 24.0 | 24.6 | 25.2 | 26.2 | 27.3 | 28.4 | 29.4 | 30.0 | 30.6 |
| 37 | 24.9 | 25.5 | 26.1 | 27.1 | 28.2 | 29.3 | 30.3 | 30.9 | 31.5 |
| 38 | 25.9 | 26.4 | 27.0 | 28.0 | 29.1 | 30.2 | 31.2 | 31.9 | 32.4 |
| 39 | 26.8 | 27.3 | 27.9 | 28.9 | 30.0 | 31.1 | 32.2 | 32.8 | 33.3 |
| 40 | 27.7 | 28.2 | 28.8 | 29.8 | 30.9 | 32.1 | 33.1 | 33.7 | 34.2 |
Prognosis and management are variable and depend on the severity of the hypoplasia, age at delivery, and nature of the associated conditions. Absence of fetal breathing movements in the setting of oligohydramnios in pregnancies resulting from premature rupture of membranes is a predictor for pulmonary hypoplasia. The spectrum of clinical outcomes ranges from mild respiratory insufficiency to neonatal death.
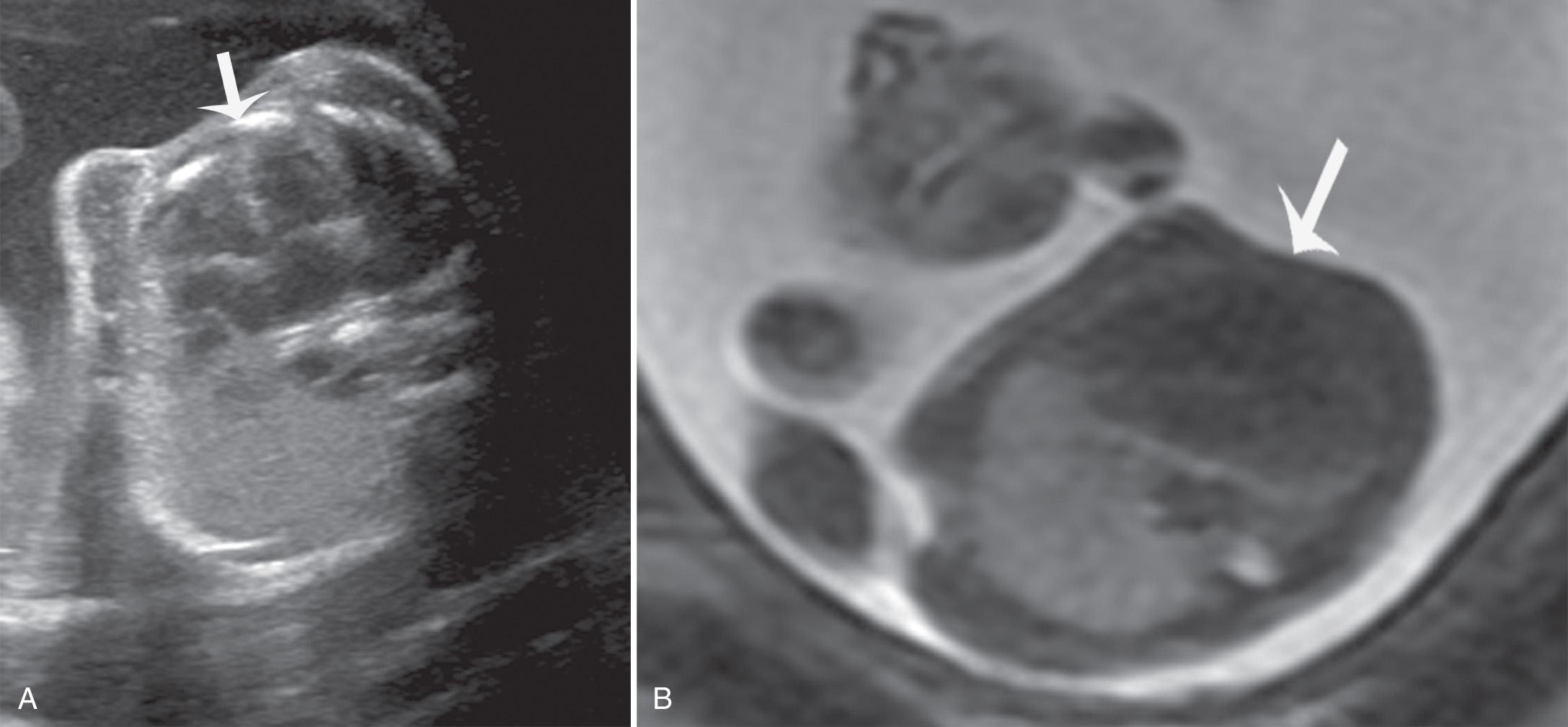
In cases of unilateral pulmonary hypoplasia or aplasia, there is mediastinal shift to the side of the hypoplastic lung, with no associated mass in the contralateral lung to explain the degree of mediastinal shift ( Fig. 36.3 ). The contralateral lung may be enlarged and echogenic. Pulmonary hypoplasia can also be secondary to space-occupying lesions, such as congenital pulmonary airway malformations (CPAMs), diaphragmatic hernia (CDH), or pleural effusion.
An echogenic lesion in the fetal thorax ( Table 36.3 ) or a cystic lesion in the fetal thorax can be part of the CPAM spectrum. This spectrum includes lesions that have been historically called congenital cystic adenomatoid malformation (CCAM), bronchopulmonary sequestration (BPS), and congenital lobar emphysema. CPAM is a congenital hamartomatous lung lesion that communicates with the bronchial tree through an abnormal communication and has normal pulmonary blood supply and venous drainage into the pulmonary veins. BPS is normally developed lung tissue with systemic circulation. However, CPAM and BPS lesions often occur together and are then call hybrid lesions or part of the CPAM spectrum. For clarity, we will describe these lesions separately, but the reader should be aware that careful histologic inspection will often find regions of CPAM in what appears to be a sequestration, as well as lesions that resemble a CPAM that have both pulmonic and systemic feeding vessels. Both of these types of lesions can have air trapping postnatally and therefore may have elements of congenital lobar overinflation (CLO; previously known as congenital lobar emphysema ).
| Abnormality | Location | Distinguishing Features |
|---|---|---|
| Congenital pulmonary airway malformation (CPAM) | Unilateral (2%-3% bilateral) |
Multiple cysts may be seen in association with echogenic lesion |
| Sequestration | Unilateral; left lower lobe most often | Systemic blood supply |
| Congenital lobar overinflation | Unilateral; upper lobe most often | Similar to microcystic CPAM; enlarged echogenic lung with mediastinal shift |
| Congenital diaphragmatic hernia (CDH) | Typically unilateral; left sided most often | Peristalsis of bowel in chest Stomach above diaphragm Absence of part of the diaphragm |
| Congenital high airway obstruction (CHAOS) | Bilateral | Distended trachea and main central airways Symmetrical bilateral enlarged lungs with eversion of hemidiaphragms |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here