Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
© 2018 Elsevier Inc. All rights reserved. Please note that the copyright for the original figures submitted by the contributors is owned by Contributors.
Skull base neoplasms are known to be difficult to access and often impossible to cure; their removal often requires extensive and/or complex approaches through a myriad of neurovascular structures. Chordomas and chondrosarcomas epitomize this challenge, as they arise in the heart of the posterior and middle skull base, the clivus, and middle fossa, the petroclival junction.
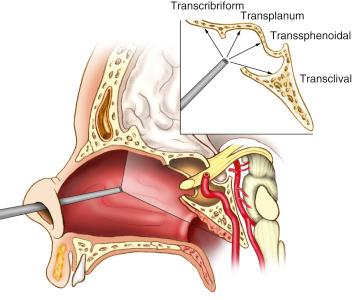
Endonasal approaches provide a direct approach to the entire ventral surface of the skull base, from the anterior to the posterior fossa ( Fig. 12.1 ), by taking advantage of the natural interface between the paranasal sinuses and the skull base. The broad expansion of these approaches from their precursor, the transsphenoidal approach to the sella, is achieved through use of the endoscope as the visualization tool. Unique in its ability to be introduced into the surgical field of the sinuses via the nares and applied through by two surgeons, an otolaryngologist and neurosurgeon working together, the endoscope allows full visualization and access to the clivus and paraclival regions via this sinus/skull base interface.
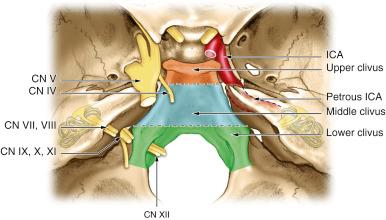
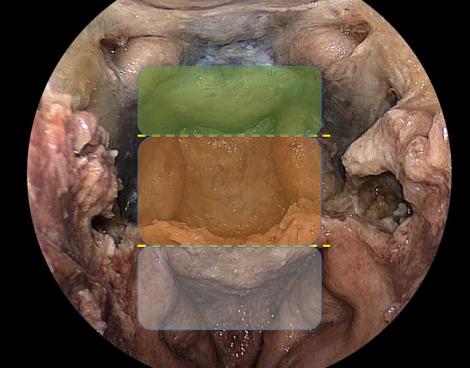
Traditionally, for lateral transcranial approaches, the clivus is divided into thirds based on neural foramina ( Fig. 12.2 ). The same division can be used for endonasal purposes, though a slight reclassification using endonasal landmarks that emphasize the importance of the abducens nerve is more relevant ( Fig. 12.3 ). The upper clivus consists of the sella, sellar floor, dorsum sellae, and posterior clinoid processes and is bounded laterally by the cavernous sinus and its neurovascular contents. The middle third of the clivus extends from the sellar floor to the sphenoid floor. The abducens nerve crosses posterior to the paraclival (vertical petrous) internal carotid artery (ICA) approximately halfway between foramen lacerum and the sellar floor, and is the critical nonvascular landmark. The lower clivus then extends from the floor of the sphenoid to the foramen magnum and includes the jugular foramen/medial jugular tubercle and transitions to the petrous bone laterally at the petroclival fissure/synchondrosis. The lower clivus has the primary landmark and lateral limitation of the hypoglossal canal/nerve, above which lies the medial jugular tubercle and below which lies the occipital condyle. Superficially, the anterior capitis muscles attach to the clivus at the supracondylar groove, a thin ridge of bone that demarcates the level of the hypoglossal canal.
Chordomas (and rarely chondrosarcomas) can originate from or extend to the upper cervical spine. The EEA can typically access the upper portion of the anterior ring of C1 and the dens deep to it. The anterior ring of C1 has a midline anterior tubercle that is an excellent landmark. The lateral limitation of the entire craniocervical junction is the parapharyngeal ICA, which is typically most medial at the level of C1.
Newly diagnosed clival lesions can be difficult to define as chordoma or chondrosarcoma. Lesions such as fibrous dysplasia and cholesterol granuloma usually require no treatment unless symptomatic from cranial nerve involvement. Conversely, other clival tumors such as plasmacytoma, nasopharyngeal carcinoma, lymphoma, and metastasis may require biopsy to make a definitive diagnosis, but radical resection may not be the primary treatment, as is generally the case with chordoma/chondrosarcoma. Finally, benign notochordal remnants, ecchordosis physaliphora, and even some longstanding chondrosarcomas may have little or no progression over time and can merely be observed.
Symptomatic tumors that are radiographically consistent on MRI and CT with chordoma or chondrosarcoma should be approached with the goal of maximal safe resection. Common symptoms include occipital headache, cervicalgia, diplopia from abducens palsy, and dysphagia and dysarthria from hypoglossal palsy. Relief of these symptoms is often a secondary goal, with the primary goal being complete resection when possible. The aggressiveness of surgery should be tempered by potential morbidity, but this is a very vague and subjective guideline, dependent upon surgeon comfort and experience. In addition, recurrent tumors may be incompletely resectable because of scar, multifocality, or metastasis and some indolent chondrosarcomas can be controlled with debulking of symptomatic portions. This latter situation is especially true if tumors are calcified and occur in older patients. Both chordomas and chondrosarcomas have a wide range of natural histories, from indolent to extremely aggressive. Over time, improved understanding of the molecular profiles of these tumors will help differentiate them and guide aggressiveness of resection. At this time, however, available data shows that complete resection provides the best long-term survival for both tumor types.
Preoperative evaluation for patients with both chordoma and chondrosarcoma is similar. Patients with diplopia or other vision changes should be evaluated by a neuroophthalmologist whenever possible. They can often determine the recoverability of nerves based on chronicity and severity of nerve dysfunction. A full hormone panel to test pituitary function is also key, especially in patients who have had prior irradiation, as hypopituitarism is quite common. In addition, invasive prolactinomas can rarely imitate chordomas and would be diagnosed with a significantly elevated prolactin level.
A preoperative swallow evaluation is critical for patients with any dysphagia or dysphonia. Vocal cord paralysis can significantly affect postoperative care and preoperative counseling. In addition, a full head and neck exam to rule out pathologic lymph nodes is standard. In preparation for endonasal surgery, consultation with the otolaryngology cosurgeon is helpful, for any case and critical in the setting of prior surgery, in evaluation for changes in nasal anatomy or signs of infection, both of which can be fully evaluated with nasal endoscopy and imaging.
Preoperative imaging should include MRI with fine cut T2 axial images and fine cut and SPGR pre- and postcontrast axial imaging. CT angiography is also key to evaluating bony erosion and arterial involvement, compression and displacement. In addition, any patient with significant craniocervical involvement should be evaluated for limitation of range of motion and, in cases with concern for stability, with flexion-extension lateral radiographs.
The aim of chordoma surgery should be complete removal of tumor and any bone or dura in contact with the tumor. This ensures the lowest recurrence rate. Rarely, only the outer/periosteal layer of dura is involved and the inner/meningeal layer can be preserved to avoid an intraoperative CSF leak. More commonly, though, the inner dura has some tumor invasion that can only be realized with resection. As such, each phase of the endonasal approach should provide the widest access to all areas of the tumor and the tissues it contacts.
The EEA to the clivus can be tailored to the region of the clivus that is involved. To access the upper and middle clivus, a wide sphenoidotomy with removal of the rostrum is sufficient. If reconstruction of a dural defect is anticipated, a nasoseptal (NS) flap is elevated on one side prior to the sphenoidotomy. For the lower clivus/foramen magnum, the nasopharyngeal mucosa between the Eustachian tubes is excised with electrocautery or microdebrider or reflected inferiorly as a mini mucosal (retropharyngeal) flap. The inferior turbinates may need to be laterally displaced for wider access to the lower clivus. More lateral access requires a transpterygoid approach (via a maxillary antrostomy) for the upper and mid-clivus and lateralization or resection of the Eustachian tubes for the lower clivus.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here