Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hands are involved in more than 80% of all severe burns. Each hand represents less than 3% of the total body surface area; nonetheless, the American Burn Association categorizes burns of the hand as major injuries. Even small burns of the hand may result in severely limited function. When burns of the hand occur as part of a major thermal injury, treatment of the hands receives high priority because the patient’s ability to perform useful work after recovery is to a great degree determined by residual hand function. The functional importance of the hand cannot be overemphasized inasmuch as severe hand burns may leave individuals unable to work or even care for themselves. The hand plays a crucial role in the evaluation of our environment (“get a grip on a problem”), in communication with others, in sending and receiving emotional signals, and in sexuality, and the hand is frequently a mirror image of our mental state. ,
Burns on the hand frequently have devastating consequences in terms of functional outcome and also esthetic appearance. Although burned areas of the trunk or lower extremity can easily be hidden under clothing, burned hands are readily visible. Social and professional reintegration of the patient may be delayed because of the psychological stigma that is caused by the visible mutilation. For these reasons, burned hands deserve to be treated with excellent conservative and surgical techniques to achieve not only the best function but also the best possible esthetic result. The statement by Guy Foucher that “hand surgery is also aesthetic surgery” has never been truer than in the treatment of burned hands. The functional importance of the hand gives it top priority in modern treatment concepts. The most important treatment principles include early initiation of physical therapy; the use of splinting, passive motion, and topical treatment, including enzymatic debridement; and, when indicated, the use of excision and grafting. A multidisciplinary team, including plastic surgeons, physical and occupational therapists, and psychologists, should be involved from the day of admission to ensure the best quality of care. ,
It is estimated that about 1% of the population in Western countries will have a burn injury each year, approximately a quarter of which will require medical care. , This makes thermal injury the most frequently reported accident. The workplace, however, accounts for less than a third of burn unit admissions and fire-related deaths. The upper extremity is the most common anatomic area burned, being involved in up to 89% of burns. , The two main reasons for this frequent involvement are the protective reflex with which patients try to guard their faces and the fact that the hand in most instances is exposed without any form of protection. Scalds and contact burns are the major cause in pediatric hand burns, when at around 4 months children start to explore their environment. The dorsum of the hand is predominantly involved in flame or explosion injuries, whereas injuries to the palm are more frequently found with chemical exposure, friction burns, or high-voltage injuries. Thermal energy may be transmitted directly by contact with a hot object or liquid. More commonly, however, energy is transmitted indirectly, as when gas escaping from an oven ignites.
The skin and soft tissues of the hand demonstrate some unique properties. The dorsal skin is thin and very flexible and lies on a rather thin subcutaneous layer of fatty tissue. This structure provides little mechanical protection but allows maximum tendon excursion and joint mobility without the necessity for excess skin. The wrinkles over the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints deepen with finger extension and stretch with flexion. Similar movements are facilitated by longitudinal creases in the web space. The dorsal skin contains large superficial veins, hair follicles, and sebaceous glands but contains no sweat glands. The skin is especially thin over the PIP joints, where the extensor tendons are at risk. Attenuation or rupture of the central slip with PIP joint exposure is one of the most frequently encountered complications after deep dorsal burns. The underlying cause of many functional disturbances following burns is disruption of the coordinated interplay of extrinsic and intrinsic muscles, tendons, and joints.
The palmar skin shows similarities to the plantar skin of the weight-bearing portion of the foot. The thick, subcutaneous fatty layer has a honeycomb-like structure that has shock-absorbing properties and provides grip stability by means of numerous fibrous septa that connect the skin with the deep fascia. Thick epidermal layers are found in the areas of greatest mechanical stress. In the finger, the Cleland ligament (dorsal to the neurovascular bundle) and Grayson ligament (palmar to the neurovascular bundle) provide stability.
The anatomic properties described above can lead to severe direct thermal effects in the hand that are not seen elsewhere in the body. Blood vessels, tendons, and joints are situated just beneath the skin surface over the dorsum of the fingers, making these structures extremely susceptible to the effects of thermal energy. The cylindrical form of the fingers, with their ligaments limiting swelling and changes in volume of the fingers after thermal injury, can lead to dermal compartment syndromes in the event of deep dermal circumferential burn injury.
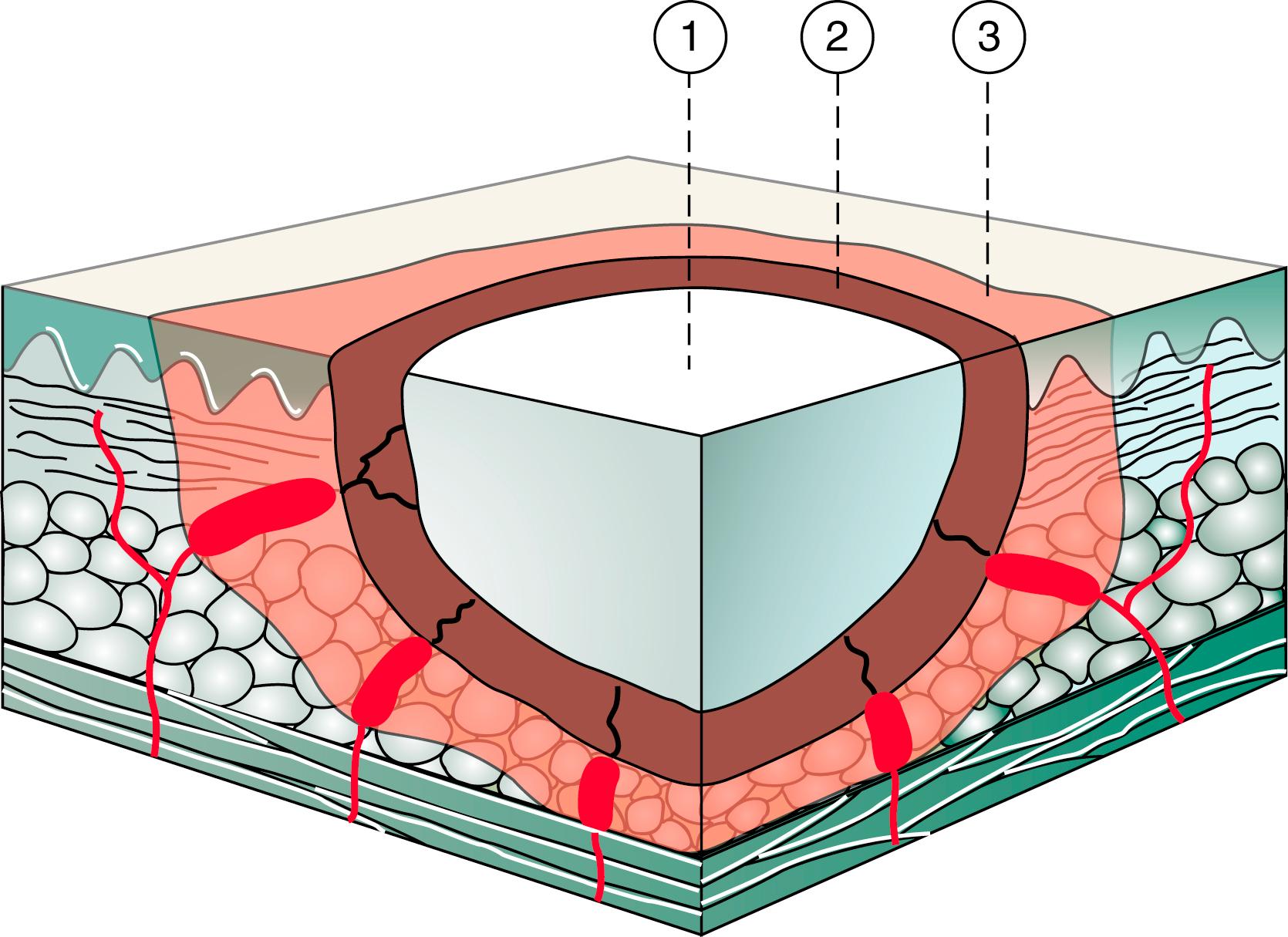
The severity of a thermal injury depends on the amount of transferred energy, which is correlated with the duration of exposure and the temperature of the heat source. Longer exposure to lower temperatures has the same pathophysiologic consequences as short exposure to high temperatures. The character of the skin at the site of injury also determines the depth of the injury. The palmar skin, for example, can withstand greater thermal energy than the dorsal skin can. The heat leads to coagulation of blood vessels, denaturation of proteins, and an increase in capillary permeability (capillary leak). This phenomenon divides the burn wound into a zone of necrosis, a zone of stasis, and a zone of impaired circulation. Insufficient primary treatment (i.e., no escharotomy if indicated or insufficient fluid replacement) may convert the zone of stasis into a zone of necrosis (afterburn) ( Fig. 57.1 ).
Intravascular fluid shifts into the interstitial space and causes a protein-rich edema. Burns of more than 20% of the body surface area lead to a generalized edema in which swelling of the skin and subcutaneous tissue is also encountered in nonburned areas. Edema causes several pathologic effects by increasing intercellular pressure and decreasing circulation. In the intrinsic musculature of the hand, this may lead to a compartment syndrome requiring fasciotomy. Intracellular edema results from disruption of the sodium pump and subsequent entry of sodium and water into the cell. In the hand, persistent interstitial edema that has not resolved after 72 hours may lead to subcutaneous fibrosis with subsequent stiffness of the joints.
Blisters are the cutaneous equivalent of the accumulation of intercellular edema. The blister fluid is rich in proteins and inflammatory cytokines, leukotrienes, and prostaglandins, in addition to multiple growth factors such as angiogenic factors13 and platelet-derived growth factor, interleukin-6 (IL-6) and IL-8, and transforming growth factor-α. Fluid losses through blistering may be considerable in major burns because the ability of the epidermis to limit loss of water vapor is unbalanced, but this does not play a role in isolated hand burns. Blisters are found in partial-thickness (second-degree) burns and superficial dermal (second-degree) burns and less frequently in deep dermal (third-degree) burns.
Any burn injury, even if considered minimal in extent, can still be catastrophic if the hand burns are severe enough to result in deformities that render the individual unable to perform personal daily functions. One of the major basic principles of management of injuries to the skin and subcutaneous tissue of the hand is to achieve wound healing as rapidly as possible. It is equally important to avoid complications that may extend the magnitude of the injury. The basic considerations in treating a burned hand can be divided into treatment goals and treatment principles. The most important treatment goals can be defined as follows:
Avoid any additional injury or increase in the depth of the burn (do no harm).
Achieve early wound closure.
Maintain active and passive range of motion.
Prevent infection or loss of soft tissue coverage.
Initiate early functional rehabilitation.
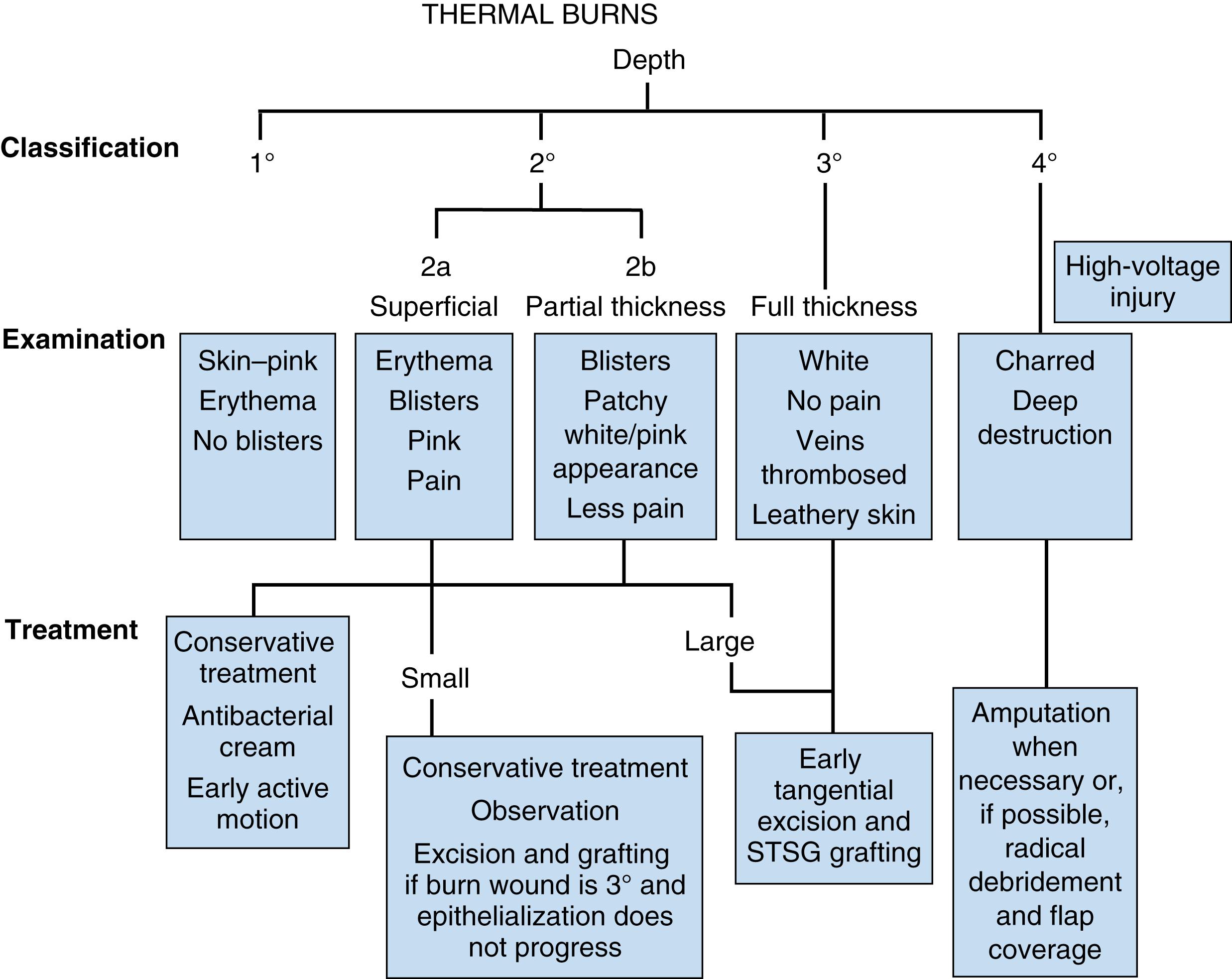
Treatment should always focus on these goals while taking into consideration the individual circumstances of the patient, which may lead to a shift in priorities. , To achieve these goals, the following basic treatment principles should be followed ( Fig. 57.2 ):
Evaluate the size and depth of the burn.
Perform escharotomy if indicated.
Apply proper wound care and dressings.
Make a decision about conservative or operative treatment.
Initiate early hand therapy and splinting.
Manage the burn surgically (removal of eschar, transplantation of skin grafts, flap coverage if necessary).
Begin early postoperative physical therapy.
Provide functional rehabilitation.
Perform secondary and tertiary corrections if necessary.
A careful and comprehensive history of the injury is of great diagnostic value and prognostic importance and may provide important information for necessary decisions about treatment. After the history, a thorough physical examination should define the extent and probable depth of the burn, the presence and severity of associated injuries, and the general health of the patient. Physical diagnosis of the depth of burn is initially difficult even with years of experience, but knowledge of the mechanism and circumstances can help in indicating the amount of thermal energy conveyed to the tissue.
All injuries should be documented carefully to create a solid foundation for further decisions and a baseline for follow-up and evaluation of outcome during the treatment course. Photographic documentation is highly recommended, especially in view of potential medicolegal issues. The status of perfusion, capillary refill, skin color, and other characteristics have to be documented to facilitate decisions about escharotomy, compartment release, or acute eschar excision.
The cause of the burns can be considered the most useful predictive factor with regard to the prognosis for healing. Scalds usually result in a mixed-depth pattern of injury and frequently involve the palms. Especially in younger patients, scald burns demonstrate a high capacity for spontaneous healing. A more aggressive approach is indicated in elderly individuals with thinner skin. Flame burns are the most serious type of burns, with the notable exception of high-voltage injuries. Flame burns are usually deep partial-thickness or full-thickness burns and often require surgical treatment. ,
Treatment of burns is dictated by the severity of the injury, and severity is determined by the level of thermal energy transmitted to the tissue. Burn wounds have been classified in many ways, although the most common is an anatomic classification based on the depth of the damage ( Box 57.1 ).
First web adduction contractures
Web space contractures
Dorsal skin contractures
Digital flexion contractures
Boutonnière deformity
Dorsal skin deficiency
Digital loss secondary to ischemia
Median and ulnar nerve compression syndrome
Superficial, first-degree burns are characterized by an erythematous epidermis without blistering and are moderately painful. The clinical appearance is similar to sunburn. First-degree burns are those in which cell damage occurs without cell death. These injuries require only symptomatic care, principally directed at relieving pain, which is usually achieved by the application of cooling lotions and pain relievers. They will heal without scarring, usually in 2 to 3 days, and with good return of function.
Superficial partial-thickness second-degree burns destroy the epidermis and some elements of the basal epidermal regenerating layers of the dermis. They are considered to be the most painful type in the immediate posttrauma period because sensitive nerve endings are not damaged. They have the potential to heal by virtue of regeneration from the living epidermal elements remaining in the dermis (sweat or sebaceous glands and hair follicles). , Regeneration, however, may be quite prolonged, depending on the depth of the injury. In second-degree injuries, the resulting scar formation is directly dependent on the depth of injury, and the quality of the regenerated skin is inversely proportional: The deeper the burn, the poorer the quality of the regenerated skin ( Fig. 57.3 ).

Deep partial-thickness second-degree burns appear as a moist mottled surface that may be pale or erythematous, depending on the depth of the burn. These wounds typically blanch with pressure and refill on release. Nerve endings are still present in the vital layers, and thus these burns can be quite painful. The skin still bleeds after a needle prick ( Fig. 57.4 ).

Full-thickness third-degree burns are characterized by the death of all germinal epidermal elements. The wound extends below the level of the dermis. The skin has a leathery unyielding appearance and is pale to brown in color. The nerve endings are destroyed, so the pain may not be significant. Because all the dermal appendages, as well as the overlying epidermis, are destroyed, these wounds cannot heal by epithelial regeneration and thus are not self-healing ( Fig. 57.5 ).

A fourth-degree injury involves necrosis of deeper structures such as tendons and bone and is usually found only after contact burns or high-voltage injuries. , ,
Clinical assessment has not been usurped by modern technology in the evaluation of burn depth. Evaluation is based on the clinical appearance, testing of residual sensibility, pinprick testing for bleeding, and evaluation of capillary refill. These findings are correlated with classification of the burn. Modern devices such as laser Doppler imaging, high-resolution ultrasound studies, thermography, and spectrometric analysis are interesting adjunctive techniques but have not replaced or significantly improved clinical assessment in hand burns.
Initial delivery of first aid to an individual with a hand burn includes immediate cooling of the wound by rinsing with cold tap water within the first 30 minutes of injury. , Cold packs or crushed ice may cause additional harm by decreasing the tissue temperature too much. There is good evidence that the immediate application of cooling to a burn wound will reduce subsequent edema formation and may decrease the actual depth of injury by reducing the zone of stasis. A positive side effect is reduction of pain by cooling the burn wound. Another major defense against edema in the early management of acute hand burns is proper positioning of the hand. Strict elevation of the burned hand above the level of the heart of the patient is recommended. This elevation must be maintained continuously during the early postburn period.
The most important principle in the initial management of a burned upper extremity is maintenance of perfusion, which is ensured by adequate fluid resuscitation to maintain circulating volume and removal of any mechanical obstruction to the flow of fluid in the extremity. The tourniquet effect of an unyielding circumferential burn eschar may worsen the situation of edema following a burn, and the potential for circulation insufficiency is great, especially with deep partial-thickness or full-thickness circumferential burns. The initial therapy for these burn injuries of the upper extremity should therefore be directed toward releasing subdermal tissue pressure and maintenance of the circulation. ,
Escharotomy for tight constricting burns was first described by Fabry of Hilden in 1607. The need for escharotomy is relatively common in the treatment of circumferential full-thickness burn injuries and has been recommended frequently for some years, especially over the last 3 decades.
Indications for escharotomy include pain, resistance to passive extension of the fingers, and disappearance of capillary refill in the nail beds. The forearm and hand feel tense to palpation. Doppler measurement of digital or superficial palmar arch pulses may also help, but by the time that the radial or ulnar pulses disappear, tissue ischemia is well advanced. Measurement of subcutaneous pressure with Wick catheters has been recommended by several authors. Escharotomy is indicated when intracompartmental tissue pressure is greater than 30 mm Hg on two separate readings. However, the clinical experience of the surgeon is the most important factor in making the decision to perform an escharotomy. ,
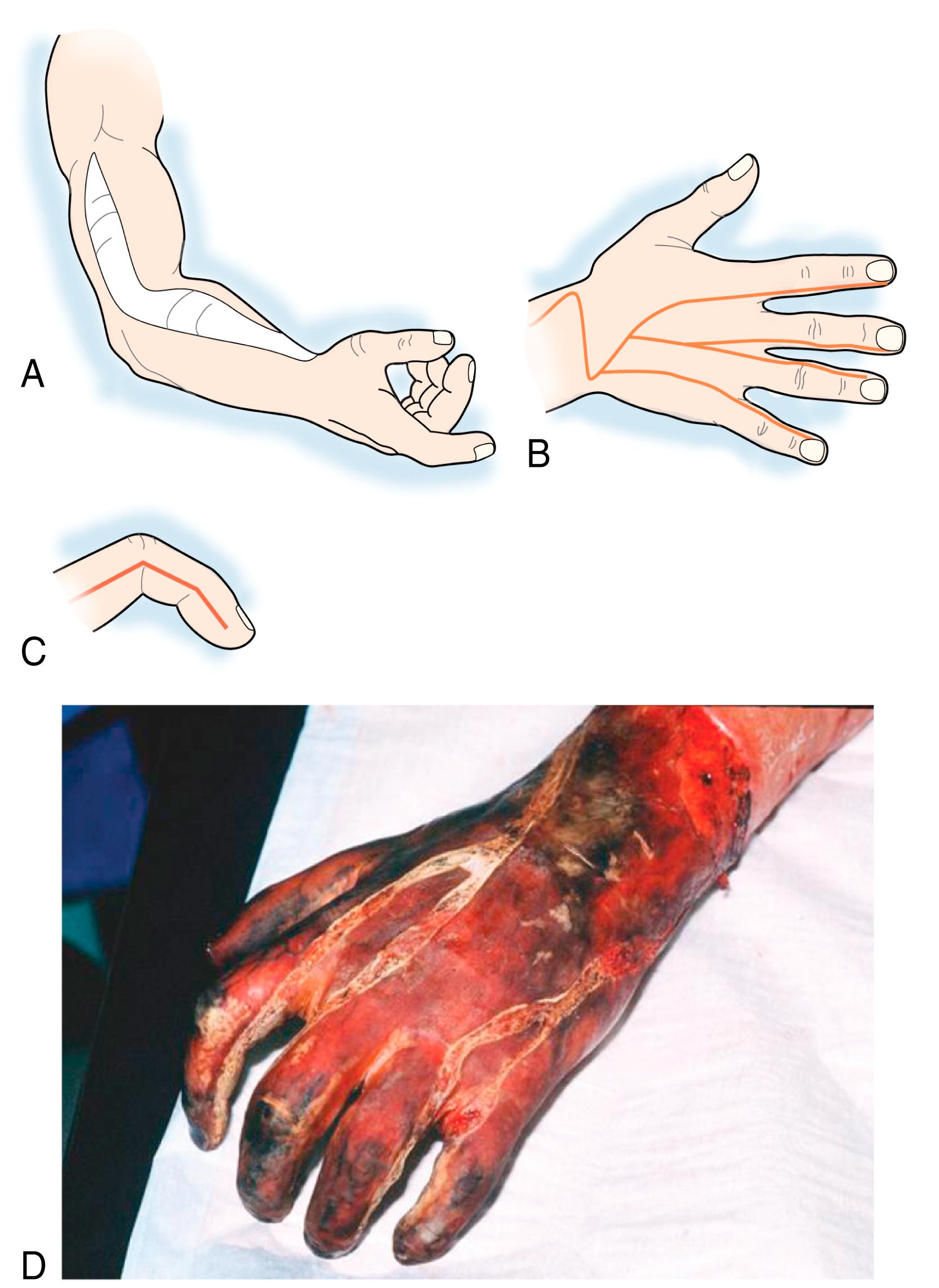
The surgeon should carefully plan surgical escharotomy incisions with the aim of releasing areas of circulatory restriction and restoring adequate flow while avoiding injuries to underlying structures such as nerves or vessels. Escharotomies can be carried out either with the use of electrocautery or by scalpel. A radial full-thickness incision to decompress the hand and arm should be performed as the first step because there is no risk of any injury to one of the peripheral sensory nerves except the superficial branch of the radial nerve. The length of the incision depends on the size of the constricting eschar. The maximum length of the incision should extend on an axis from the tip of the acromion to the lateral edge of the antecubital flexion crease and up to the radial aspect of the distal flexion crease of the wrist. If necessary, medial ulnar escharotomy can be added. The incision line should be drawn from the axilla to the medial aspect of the antecubital flexion crease to the ulnar aspect of the distal flexion crease of the wrist.
In patients with tight circumferential burn eschar of the fingers, digital escharotomies should be performed. The ulnar incision can be continued along the hypothenar eminence to the midlateral line of the ulnar border of the little finger. The radial escharotomy incision line can be extended along the radial aspect of the thenar eminence and the midlateral aspect of the thumb. The index, long, and ring fingers can be decompressed with similar midlateral incisions on the ulnar aspect of each finger. If the blood supply is not restored adequately with these incisions, the opposite side of each digit can be released in similar fashion, thereby performing bilateral digital escharotomies. Decompression (fasciotomy) of the dorsal interossei should be performed in hands with significant edema and diminished flexion. Small vertical escharotomy incisions are made on the dorsum of the hand between the metacarpals. In a randomized trial, Salisbury and coworkers were able to show that there was an almost threefold increase in the number of fingers that could be salvaged by extended digital escharotomy ( Fig. 57.6 ). ,
Pegg and Wang and associates have pointed out the importance of intrinsic muscle decompression to overcome ischemic contracture of the hands. It is therefore vitally important with deep burns in the upper extremity to detect possible muscle ischemia to prevent the loss of fingers or the thumb because of secondary vascular compromise. If there is significant subfascial edema, escharotomy can be combined with fasciotomy. , The early signs of ischemic necrosis of the intrinsic muscles are hyperextension of the fingers at the MCP joint with flexion of the interphalangeal joints.
The role of enzymatic debridement in avoiding surgical escharotomy has not yet been clearly defined. Approximately 5% to 15% of all burn injuries are suitable for enzymatic debridement. Higher treatment costs are generated when enzymatic and surgical methods have to be combined. There are an increasing number of reports describing the use of bromelain-based techniques to reduce the need for escharotomies, but well-designed studies with sufficient numbers of patients have yet to be performed ( Fig. 57.7 ).

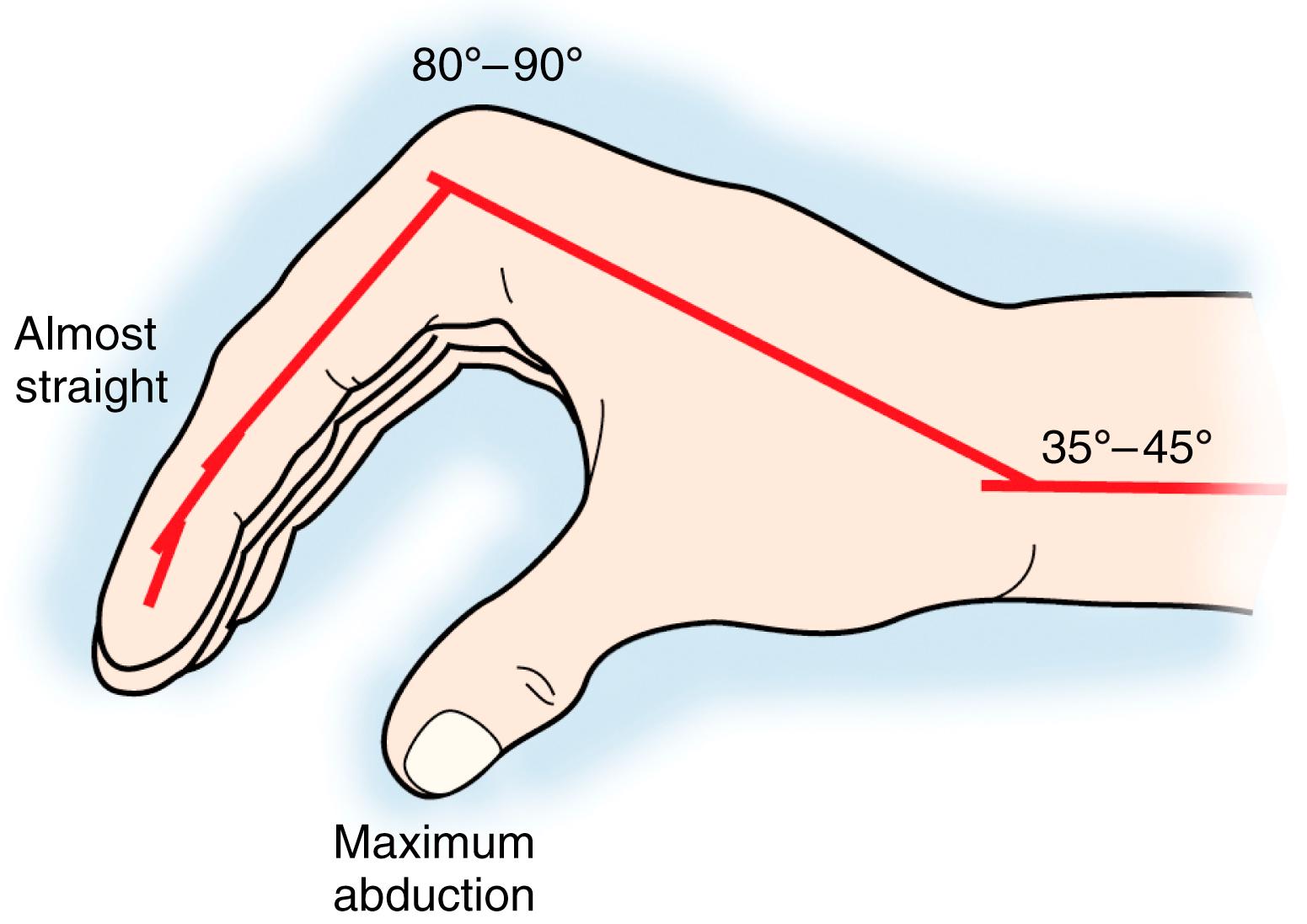
Without appropriate early splinting and positioning, a typical intrinsic-minus posture develops in a severely burned hand that is initially in large part due to swelling of the hand. The injured hand takes the characteristic position of wrist flexion, hyperextension of the MCP joints, and flexion of the interphalangeal joints. The thumb usually adducts toward the palm with the interphalangeal joint hyperextended. , , In a short period, edema, inflammation, and immobility are replaced by scarring and fibrosis, which result in deformities not correctable without surgical intervention. Scar contractures across the dorsum of the hand further accentuate extension of the MCP joints and lead to the so-called claw deformity that is typical of neglected burns of the hand.
The anticlaw position is essential to prevent permanent contracture deformities. To maintain this position, the hand should be splinted immediately in the so-called position of safety (intrinsic-plus position; Fig. 57.8 ). In this position, the MCP joints are fully flexed and the interphalangeal joints are essentially fully extended. The first web space is maximally abducted. This position keeps the ligaments of the digital joints in the best tension to prevent shrinking of these ligaments. With the burned hand in this position, the dorsal skin is stretched somewhat tightly across the metacarpals and there is little room for excessive edema formation. The so-called position of function with all digital joints slightly flexed should be avoided at all times because this position will inevitably lead to contractures. The elbow should be kept in an extended position because flexion contractures are the most frequent deformities. Care must be taken, however, to keep the elbow moving, for a permanent contracture in the fully extended position is much more of a functional problem than is a contracture in a flexed position. The shoulder is best positioned in abduction to prevent axillary contractures.
Hand splints should be applied on the day of injury. Customized splints made of thermoplastic material are most effective and can be adjusted to every clinical situation. Whether one chooses to initiate early motion or maintain the hand relatively immobilized for a longer period depends principally on the condition of the skin over the PIP joints. Here the skin is very thin, and deep burns over this area frequently lead to disruption of the central extensor mechanism over the PIP joint and development of the so-called boutonnière deformity. If the burn over the PIP joint is fairly superficial, early active flexion and extension exercises of these joints can be initiated. However, if the skin over the PIP joint appears to be more deeply burned, it is best to maintain the joints splinted in nearly full extension. The use of Kirschner wires has been advocated to maintain the PIP joints in extension with deep dorsal burns, but we have seen more problems (such as pin track infections and joint stiffness) than detectable benefits, so this technique is used only on rare occasions. One approach has been external fixation of the hand and fingers in the intrinsic plus position to eliminate the risk of loss of position during dressing changes ( Fig. 57.9 ).

Local care of the burn wound depends on the depth of the injury, the injury pattern, and the general condition of the patient. The decision-making process is illustrated in Fig. 57.2 . Basic wound care includes debridement, daily cleaning, prevention of infection with topical agents, and wound dressings. ,
In a partial-thickness second-degree burn, spontaneous healing can be expected within 7 to 14 days, depending on the size of deeper areas. The burn wound should be debrided of all contamination. Areas of peeled skin also need to be removed. Treatment of blisters remains controversial. Small intact blisters less than 1 cm in diameter can be left intact and the wound allowed to heal spontaneously. It has previously been proposed that larger blisters should be left intact as a biologic dressing because they may protect against infection. However, the fluid of burn blisters was found to be rich in prostaglandins and other proinflammatory cytokines, such as IL-6 and IL-8, that may propagate the burn wound injury and increase the zone of necrosis. The current recommendation for larger blisters is aspiration of the fluid, removal by incision, or debridement of the blisters. Dressings can then be applied directly to the burn wound.
The principle of moist wound healing is applied for spontaneously healing burns. The burn wound should be cleaned daily either in a hydrotherapy tank or under filtered tap water. This is followed by the application of an antibacterial cream. The cutaneous immune response of the individual against bacteria is compromised during the edema phase of the burn wound. Administration of antibacterial creams during this period can prevent sequelae such as streptococcal cellulitis or erysipelas of the burned hand.
With superficial thermal injury, agents such as water-soluble bacitracin can alternatively be used. A deeper partial-thickness burn wound should be dressed with a topical antibacterial agent that has more penetrating capability, such as silver sulfadiazine. Unless the thermal injuries to the hand are associated with large surface areas, systemic antibiotics are not indicated. Vaseline gauze strips and elastic netting are generally used to hold the dressing in place and to provide a custom fit, with the opportunity for maximum movement of the extremity. The fingertips should remain visible in the dressings to allow observation of their color and vascularity. Siliconized gauze can alternatively be applied.
As the superficially burned areas begin to epithelialize, care must be taken to avoid shearing of the new epithelium with dressing changes or exercise. Bland ointments or creams such as vitamin A and D ointment are helpful to prevent dehydration of the new epithelium. These new epithelial surfaces will require some maturation before sebaceous and sweat gland function recovers.
In recent years, some simpler techniques of burn care have been introduced that involve less work and are less time consuming. The simplest treatment of these types of burns is a large surgical glove filled with silver sulfadiazine cream. The patient slips his or her hand into the glove, which is then fixed with a bandage at the wrist level. Some patients feel uncomfortable in the rather tight-fitting glove, but for many patients this technique provides a simple inexpensive solution that is also applicable in developing countries. Flammacerium® (cerium nitrate and silver sulfadiazine) is routinely used in large surface area burns in Europe but remains controversial in the management of hand burns due to a tanning effect on the skin. (This medication is not available in the United States as it lacks approval from the U.S. Food and Drug Administration.) Harrison and Parkhouse described the use of silicone oil in a glove for the same purpose. In patients who cannot tolerate the tight-fitting glove, the extremely large Gore-Tex glove provides a useful alternative ( Fig. 57.10 ). The glove can be left on for several days; however, daily dressing changes are easy and almost painless with both techniques.

The Biobrane® glove provides an excellent alternative to the techniques just described. The biohybrid membrane of knitted nylon, silicone mesh and peptides from porcine proteins is perfectly fitted to the hand and then sealed. It is semipermeable, and small amounts of wound fluid can evaporate through the membrane. Larger fluid collections have to be evacuated through little puncture holes in the material. The glove remains on the wound until the surface is epithelialized and then automatically peels off. Because the glove is transparent, changes in the wound can be observed through the membrane. Dressing changes are not necessary, so the primary high cost of the glove is equalized over time, especially since only limited nursing care is required. The major disadvantage of this method is that the initial wound assessment has to be correct because only wounds of superficial thickness will heal spontaneously under the glove. However, our experience has shown that in cases in which patches of deeper burns are detected, the glove can be removed and treatment in these areas can be directed toward surgical intervention ( Fig. 57.11 ). Similar techniques can be applied with polyurethane films such as OpSite® or Omniderm® or with polyacrylic mesh (SurfaSoft®). Many authors claim that film dressings lead to superior results in superficial burns; however, gauze dressings can provide the same effect, provided that the moist environment of the wound is maintained. Most recently, the new epithelial substitute Suprathel®, a cellulose material, has been used for second-degree burns with excellent results.

Deep dermal and full-thickness burns of the hand have traditionally been treated by early excision and grafting. With the advent of enzymatic debridement, some patients may benefit from waiting to allow chemical debridement rather than proceeding with early excision of the burn. It is usually accepted that the burn wound is uninfected and suitable for primary surgical treatment within the first 5 days. If this initial ideal period is missed, a delay of 3 weeks before surgery is thought to be best because of the increased risk for graft loss secondary to infection and excessive bleeding from the inflamed bed of the eschar. , , , , , ,
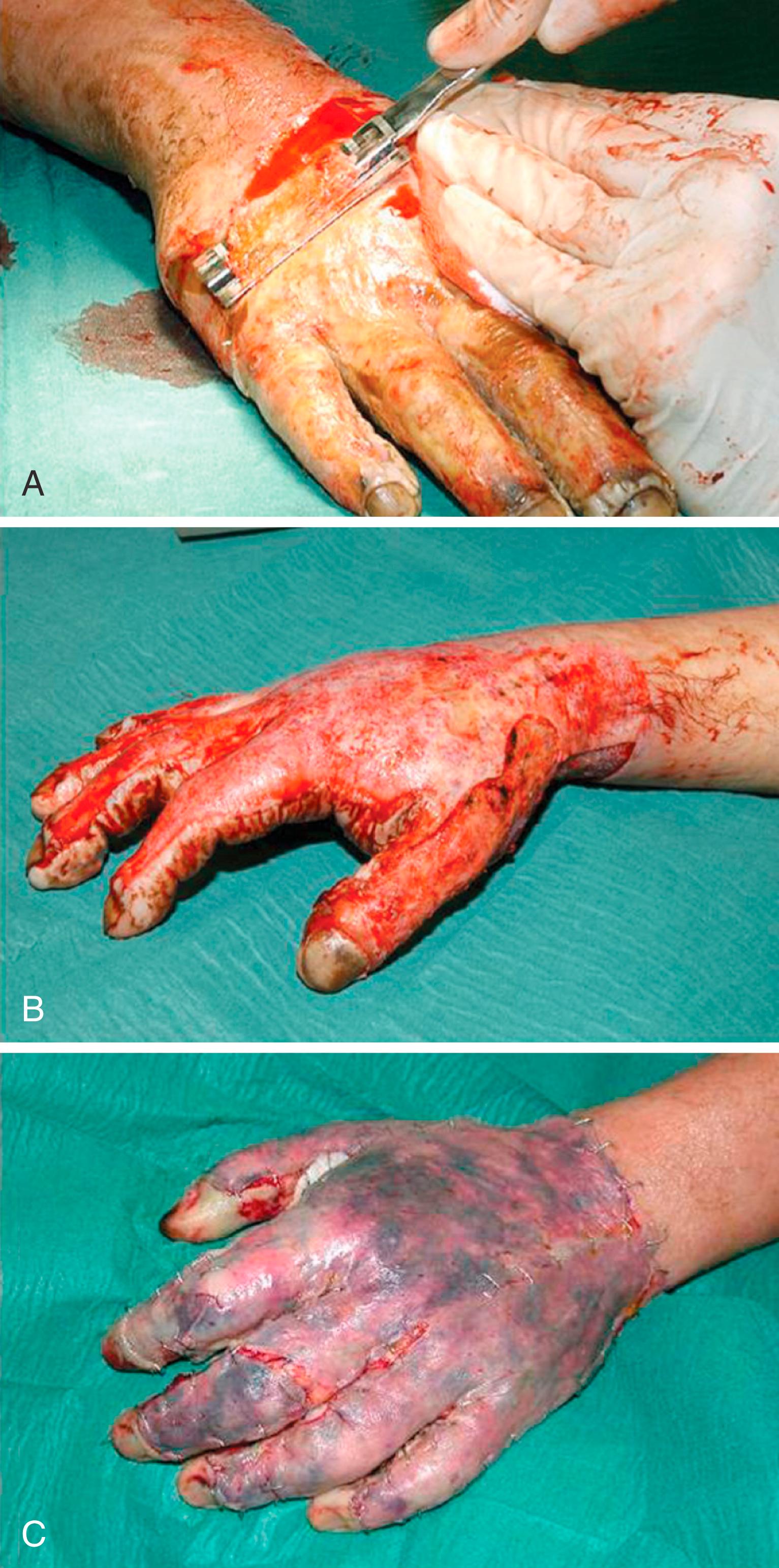
Tangential excision is the preferred surgical procedure for hand burns. It involves shaving of the burned skin in thin layers until brisk capillary bleeding is encountered. A typical instrument used for the hand is the Weck-Goulian knife, which consists of a single-edged razor blade with a guard. Layers of devitalized tissue can be removed until healthy tissue is encountered. It is very important to not leave residual devitalized tissue because this might prevent adequate take of skin grafts, promote wound infection, and delay the process of recovery. Reddish areas of fat are considered to represent the zone of stasis and should be excised. No matter how deep the burn is, salvage of the paratenon of the extensor tendons and the fine layer of areolar tissue above the joint capsules is essential to facilitate skin graft take. After excision of the eschar, sponges soaked with epinephrine are applied to reduce bleeding. The most crucial area is the dorsal skin over the PIP and MCP joints. Failure of skin graft take in these areas almost inevitably leads to exposure of the joint, with the consequence of joint infection and cartilage erosion and resulting joint stiffness.
A technique with rising popularity is hydrosurgery or water dissection. Studies confirmed that avital tissue can be removed with less blood loss and a higher rate of preservation of healthy tissue. Thereby, the surface area requiring skin grafting can be reduced. ,
Debridement can also be performed under tourniquet control, especially if the hands are involved in a major burn. This makes assessment of the wound a little more difficult and requires more surgical experience, but it may reduce blood loss. Our procedure includes wrapping the hand with epinephrine-soaked sponges and tight elastic bandaging before releasing the tourniquet and leaving them in place for approximately 20 minutes. Most capillary bleeding has usually stopped by this time; however, meticulous further hemostasis is still necessary.
After bleeding is controlled, skin grafts are transplanted. Resurfacing the wound with split-thickness grafts is considered the “gold standard” in most cases. , There is still ongoing debate about whether the grafts should be meshed or unmeshed. Many authors claim that sheet grafts provide a superior esthetic appearance compared with mesh grafts. It is said that they produce less scar tissue than mesh grafts do and usually provide a more functional result ( Fig. 57.12 ). Meshed grafts have the advantage of facilitating drainage of wound fluid, blood, and bacteria through the holes in the mesh. They generally have a higher overall “take” rate in critical wound beds when there is some remaining bleeding or patches of questionable viability. The main disadvantage is the high rate of scar contracture that frequently leads to major functional disturbances. The mesh-graft expansion ratio used in burned hands should not exceed 1.5:1 ( Fig. 57.13 ). There are studies showing no significant difference in esthetic appearance and function between sheet or meshed split-thickness skin grafts after 12 months, however. In patients with major burns involving the rest of the body, skin grafts may be in short supply and meshed grafts have to be selected for coverage. Our recommendation for the choice of graft depends on the availability of skin graft donor sites and the general condition of the patient. If sufficient donor sites are present, split-thickness sheet grafts are the first choice. In patients with limited graft availability, meshed grafts have to be used. In rare cases with isolated hand burns, split-thickness skin grafts may be harvested a little thicker. This will result in more supple skin with fewer contractures and better functional results.

Full-thickness skin grafts have no indication in acute burns. Their take rate depends too much on a perfect wound bed, perfect hemostasis, and the ability to provide a perfect tie-over dressing. With the significant risk for graft loss, full-thickness grafts are generally reserved for secondary corrections.
The graft is held in place with either single interrupted stitches or a running stitch (4-0 or 5-0), and skin staples are a good choice on larger grafts. Care should be taken to create smooth transitions between the grafts and the edges of the remaining skin. The wound is dressed with Vaseline gauze or siliconized gauze. Cotton balls are placed over the gauze for a bolster tie-over dressing on concave surfaces. Experimental data suggest that skin graft take is best when pressure of 30 mm Hg is exerted evenly over the wound. Clinical experience has shown that a conventional bolster tie-over dressing reaches this goal. A rather new technique to enhance skin graft take is the application of vacuum pressure to the wound. This has been shown to yield very good results in skin grafting of chronic wounds, but it is technically very difficult to apply this technique to a burned hand. Early results with vacuum gloves have been reported, but larger series are still lacking. ,
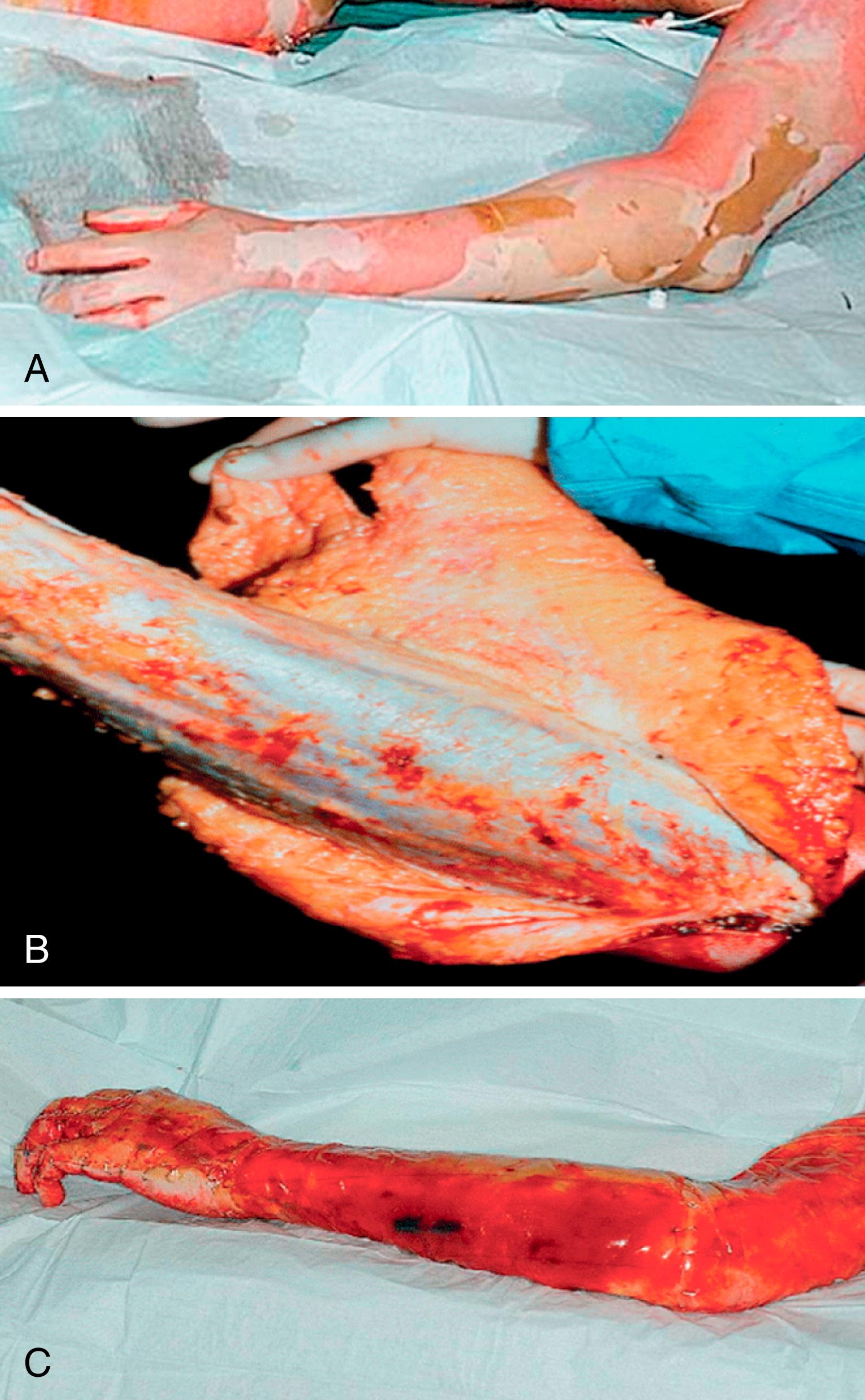
In full-thickness burns of the upper extremity and involvement of a large surface area of the entire body, epifascial excision may be indicated. The skin envelope may be reconstructed with meshed skin grafts in these cases, but this will most likely result in severe postburn contractures. Artificial dermal equivalents such as Integra®, AlloDerm®, or Matriderm® can be used in these circumstances. Use of one of these materials may result in a more pliable skin envelope, with less need for corrective surgeries later ( Fig. 57.14 ).
Dressings are left in place for 5 days. Skin graft take can be assessed by then and decisions for further wound care can be made. If the wound becomes odiferous, the dressing can be changed earlier to avoid graft loss through infection. If the wound is found to be clean with satisfying graft take, no particular treatment is indicated. Only Vaseline or any similar basic cream is administered to keep the graft moist and supple. If traces of infection such as suppuration or colored crusts are found, all debris must be removed carefully and the wound rinsed with an antiseptic solution such as chlorhexidine (Hibiclens™) or polyhexanide (Lavasept™). All skin graft areas that seem to be nonviable have to be removed. The wound is redressed with gauze and an antiseptic cream such as mafenide acetate (Sulfamylon™) or silver sulfadiazine (Silvadene™). Dressing changes are performed daily until the wound does not show any signs of infection. With this technique, many “endangered” grafts may be salvaged.
Special emphasis has to be given to postoperative splinting and physical therapy. Splints are an integral part of the postoperative treatment plan. After grafting, the hands are immobilized for 5 days until graft take is secured. Passive physical therapy is then initiated to prevent and reduce stiffening of the joints. Minor graft loss has to be accepted if joint mobility can be maintained. Even in situations in which graft take over the PIP joints is not guaranteed, mobility of the remaining joints has priority. Active range of motion is initiated as soon as the patient is awake and conscious.
In rare cases, tangential excision does not suffice. With full-thickness injuries the skin damage may reach down to the paratenon and tendons, and the metacarpal bones or joints may be exposed. In these cases, primary flap coverage is indicated. The choice of flaps depends on donor site availability and the ideal tissue for the particular situation. In younger females and children, a conventional groin flap still may be the prime choice. This donor site can easily be hidden, the skin is supple, and immobilization of the shoulder is usually well tolerated. A drawback of this flap is that four to five procedures are required to achieve a definitive result. However, in patients with thick subcutaneous fatty layers, the flap may be too thick and yield esthetically unsatisfying results.
In most situations, when the general condition of the patient allows more sophisticated procedures, the flap can be tailored to the individual need of the patient (i.e., free flaps, pedicled forearm flaps, or intrinsic hand flaps). Fascial flaps have proven to be very helpful for coverage of dorsal hand defects when cutaneous flaps would yield flaps that are too thick. , They provide stable but supple tissue, secondary reconstructive procedures can be performed under these flaps, and the esthetic results after grafting the fascia with split-thickness skin grafts are pleasing. Temporoparietal fascia, serratus fascia, or anterolateral thigh fascia flaps are the most frequently used. They seldom require secondary debulking ( Fig. 57.15 ). ,

In situations in which large flaps are required, the latissimus dorsi flap, the anterolateral thigh flap, or a cutaneous flap from the subscapular system would be the primary choice. These flaps are rarely indicated for flame burns but are more frequently used for chemical burns, contact burns, or high-voltage injuries (see later). Secondary revisions of these flaps are frequently required.
The principles of physical therapy are the same for a flap-covered hand as for a grafted hand. After 5 days, flap healing is usually secured, and passive exercises can be initiated.
Skin grafting is rarely necessary with palmar burns because of the enormous capacity for spontaneous healing from the many glabrous skin appendages. This is the reason why thick split-thickness skin grafts are seldom required. Flap coverage may be needed more frequently with deep palmar burns. In our practice, fascial flaps offer the best solution for this problem. The stability of the tissue is sufficient, and there is almost no shearing within the flap to diminish the quality of grip. Deep sensation is reported to return within 12 to 15 months.
In children, Pensler and colleagues found no significant difference in the number of operative procedures with either full-thickness or split-thickness grafts. They claim that split-thickness skin grafts have less tendency toward hyperpigmentation, thereby leading to superior cosmetic results; are more expeditious to harvest; and preserve donor sites for future reconstruction. In contrast, Pham and coauthors consider full-thickness skin grafts as a first choice for deep palm burn injuries in children. ,
Although split-thickness skin grafts are considered the gold standard in the acute care of deep hand burns, new innovative skin replacement concepts may broaden the therapeutic spectrum in the near future. The first study with cultured autologous dermoepidermal skin substitutes for full thickness defects in burns showed promising results. Artificial dermal equivalents are replaced by dermal templates generated from autologous fibroblasts, which are transplanted together with cultured autologous keratinocytes. Multicenter studies are currently underway to strengthen the database.
Skin bioprinting may be another way to reconstruct full-thickness burn wounds in the future. The concept of this new technology is the layer-by-layer deposition of cells together with scaffold material. There are no clinical data available at this time. ,
Complications after isolated hand burns are rare and can usually be avoided by proper treatment. They are more frequent with major burns in which the immune response of the patient is severely suppressed and the patient remains in a catabolic state for a considerable period. Three types of complications can jeopardize the treatment result: secondary infection, graft loss, and early hypergranulation.
Secondary infection can be a major problem in hand burn injuries. Two areas of the hand are extremely susceptible to secondary infection. The thin skin overlying the dorsum of the PIP joints makes the tendons likely to be injured or can result in an open joint. A decreased blood supply may also increase susceptibility to infection with secondary joint involvement ( Fig. 57.16 ). The nail bed is the other area that is particularly susceptible to injuries. Despite its high vascularity, the nail bed is readily exposed to thermal injury and to secondary trauma and infection. ,

Infected areas are treated with the local application of antibacterial creams or ointments (see above). Systemic antibiotic therapy is rarely indicated and should be used only when clinical signs of cellulitis or ascending lymphangitis are seen. The hand is cleaned and rinsed daily, and then antibacterial agents are applied.
The loss of skin grafts can have several underlying causes:
Insufficient debridement with residual layers of nonvital tissue
Bleeding of the wound bed with hematoma under the graft
Imperfectly fitting tie-over dressing
Secondary infection of the wound bed
In the event of graft loss or nonviable grafts, the wound has to be debrided surgically. All nonviable skin must be removed, and the wound bed has to be debrided until healthy bleeding is encountered; meticulous hemostasis is mandatory to prevent further graft loss. Hydrodissection may be a valuable technique under these circumstances.
Regrafting can be performed in the same session if there is minimal drainage and hemostasis is adequate. If the wound is seriously infected, the viability of the deeper layers is questionable, or if the wound is bleeding too much because of inflammation, it is best to treat the wound for several days with local care and delay secondary regrafting to avoid additional graft loss.
RGTAs® (ReGeneraTing Agents) are chemically engineered polymers that are specifically designed to replace degraded heparan sulfate (HS) in the injured extracellular matrix. CACIPLIQ20® contains RGTA® OTR4120, a biodegradable polymer of 1‐6 alpha polyglucose substituted carboxymethyl and sulfated. They protect naturally existing structural and signaling proteins by sequestering proteins through low‐affinity binding, allowing for faster and high‐ quality tissue repair. This agent has been shown in small series to accelerate healing and decrease scarring in hand burns. This concept may be an interesting treatment option for burns in the near future.
Early hypergranulation occurs between nonepithelialized areas of mesh grafts or the borders of sheet grafts. It is rarely encountered in large surface area burns because the immune response of patients with these injuries is usually severely impaired. Surgical removal of these hypergranulated areas is not recommended because it will cause profuse bleeding. Dressing the wound with steroid-containing gauze (Corticotulle™) has proven to be extremely useful. Several days of treatment generally suffice until the wound has reepithelialized. Early treatment with pressure gloves and silicone sheets is mandatory in these patients.
Even if in the initial phase of acute hand burn injury all treatment measures have been executed properly, postburn deformities still occur and are the most common causes of skin contracture in the hand. Postburn scarring and contractures affect the function as well as the esthetic appearance of the hand and remain the most frustrating late complication of a hand burn. If contractures or scarring affect the dominant hand, as they do on most occasions, the vocation and thereby the economic status of the patient suffers. Proper management of these deformities is thus highly desirable. A classification of postburn deformities has been proposed by Achauer.
Claw deformity
Complete
Incomplete
Palmar contracture
Web space deformity
Web space contracture
Adduction contracture
Syndactylism
Hypertrophic scar and contracture bands
Amputation deformity
Nail bed deformity
Elbow
Flexion contracture
Deep burn with extensive tissue loss
Heterotopic ossification
Axilla
Scars can also be assessed with scoring systems such as the Vancouver Scar Score, which allows classification of the scar based on the variable clinical picture.
It is well accepted that the best therapy for burn wound contractures is prevention. Prasad and colleagues suggest that comprehensive treatment efforts have led to a significant reduction in the development of burn scar contractures. It appears that factors such as improved burn wound management, liberal use of positioning, improved splinting, early maintenance of range of motion, and exercise programs have contributed to this success. , The introduction of three-dimensional printed splints could be the next steps forward to improve the results of splinting in the correction of postburn deformities. A decrease in the need for late reconstructive surgical procedures is reflected in the literature over the last 35 years. In 1972 Dobbs and Curreri reported a serious contracture rate of 27% in 681 adult burn patients. Pegg and coauthors reported on 411 patients in 1979 with a 7.8% incidence of burn scar contractures, and Kraemer and associates noted only a 3.7% rate of reconstructive procedures 9 years after burn scar release in a population of 839 adults and children with burn injury in 1986. These data suggest that improved treatment protocols and splinting for prolonged periods are reducing the need for readmission for reconstructive procedures.
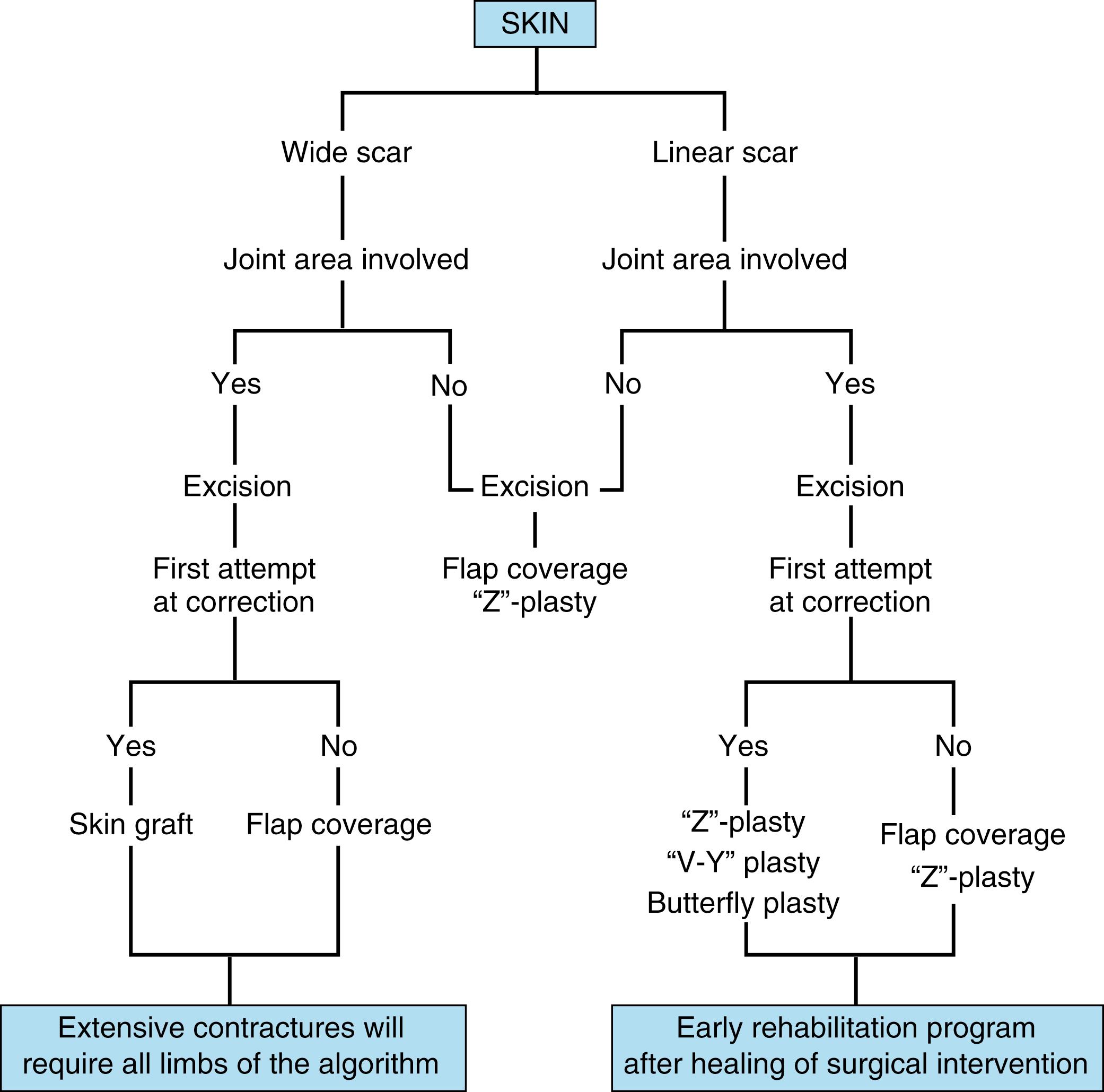
Postburn deformities are usually related to the initial soft tissue deficit. Contractures can be caused by spontaneous healing of deeper burns (i.e., the burn wound itself) or more frequently by the inevitable contracture of transplanted split-thickness skin grafts. This phenomenon occurs more extensively in the acute burn situation and is less pronounced in elective situations. The clinical impression that secondary split-thickness grafts contract more in burn wound releases than in other post trauma situations is shared by many authors; however, scientific evidence of this tendency is rare. Release of contractures may be accomplished by various patterns of Z-plasties, , but skin grafting or flap coverage is frequently required. Full-thickness skin grafts play an important role in these secondary corrections because they are more similar to normal skin than split-thickness grafts in texture, color, and resilience. However, full-thickness grafts take less readily than do split-thickness grafts and may suffer the setback of limited availability in patients with larger burns. , The latter problem, in some situations, may be solved by preexpansion of the donor sites. Full-thickness grafts have less tendency for contraction because there is an inverse relationship between thickness of the dermis and graft contraction.
Before surgically addressing the problem, a thorough analysis is mandatory. Several questions have to be answered:
What is the nature of the contracture or the limiting scarring?
Are there any underlying joint problems (e.g., shrinking of the ligaments or capsules, cartilage destruction)?
Are soft tissue procedures sufficient?
Which type of coverage is adequate after contracture release?
Where should the skin grafts or flaps be harvested?
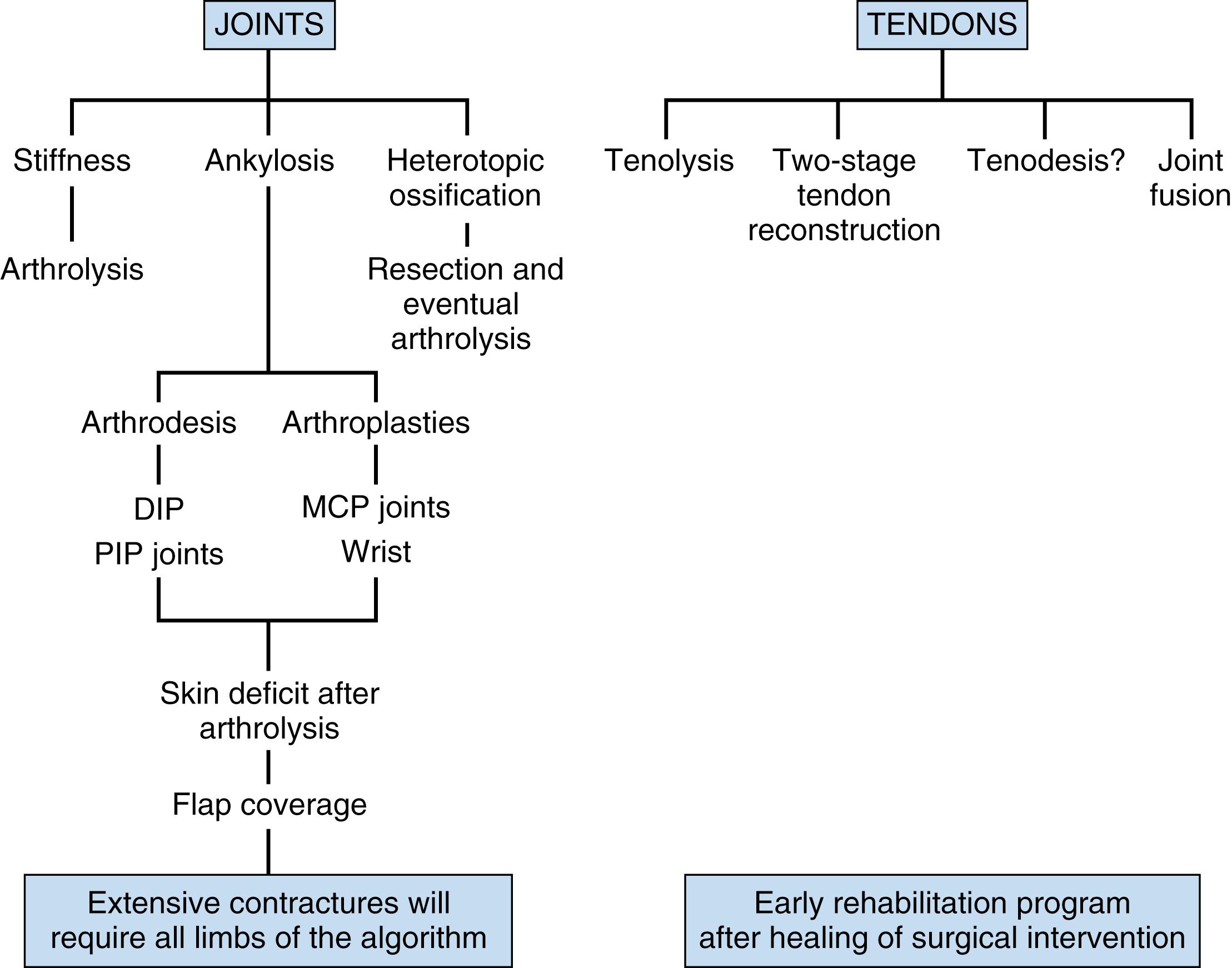
Only after these questions have been answered can a surgical plan be designed. The most disturbing functional problems are usually addressed first; however, the patient may perceive esthetic deformities as the more urgent problem. Decision-making algorithms are presented in Figs. 57.17 and 57.18 .
Dorsal scarring over the DIP joint leads to distortion of the eponychial fold, retraction of the eponychium, and proximal nail exposure. In cases involving only skin tightness without severe retraction of the nail fold, skin release and skin grafting may be sufficient.
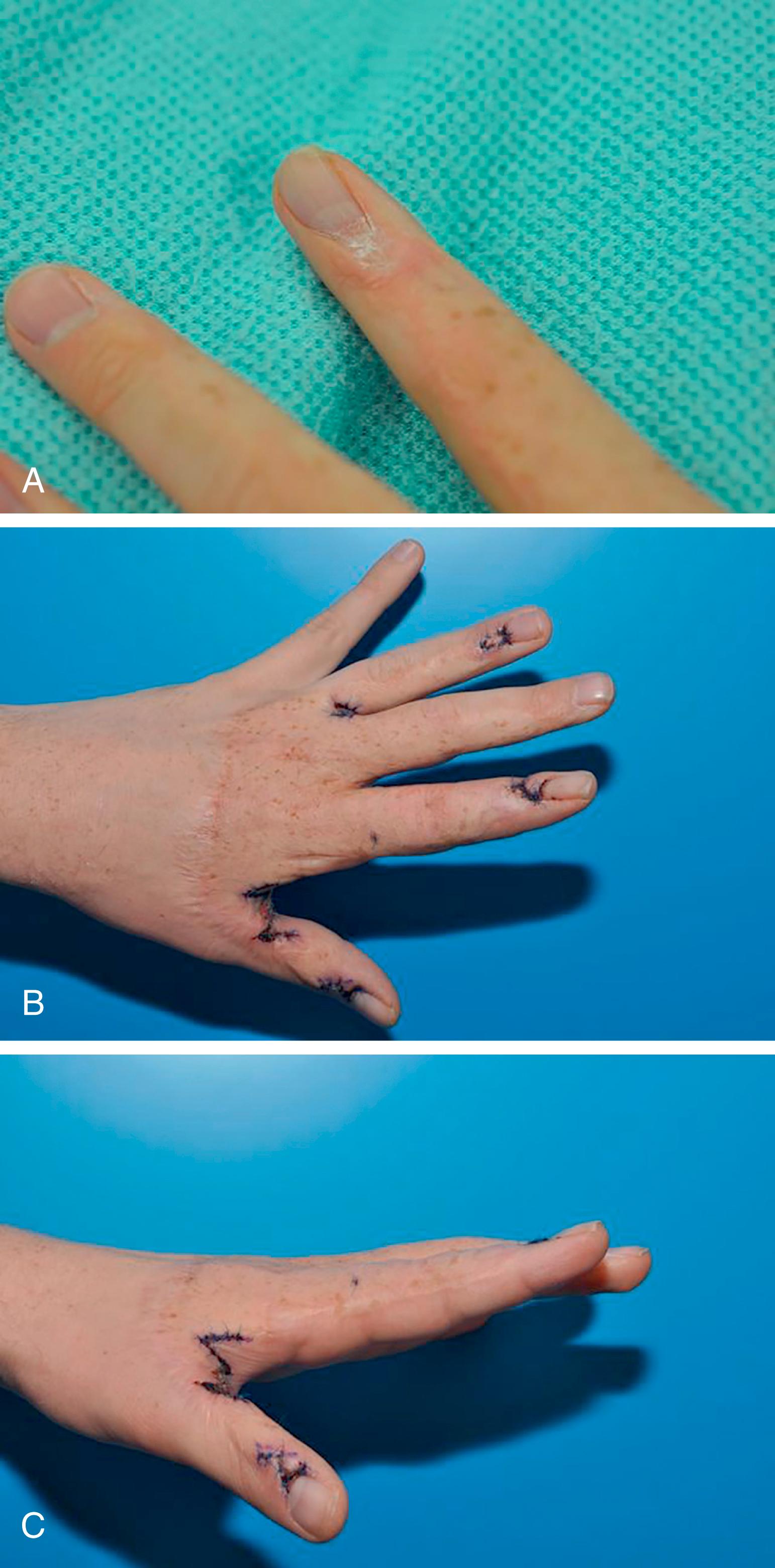
When reconstruction of the nail fold is required or skin grafts are not appropriate, proximally based lateral skin flaps are recommended. The donor site of these narrow flaps can generally be closed primarily, and the resulting tip deformity evens out over time ( Fig. 57.19 ).
Claw deformities may be difficult to correct ( Fig. 57.20 ). They usually consist of hyperextended MCP joints with flexion contracture of the PIP joints. In contrast to Achauer’s classification, we prefer to divide claw deformities into (1) long-standing fixed deformities with ligament shrinkage and (2) cutaneous deformities in which simple release of the skin contracture solves the joint position problem.

The first group requires arthrolysis, either from the dorsum or in rare cases from the palmar aspect of the joint. Both approaches to the joint can usually be performed from the dorsal skin incision. These situations generally require some sort of flap coverage because the extensive dissection has eliminated all tissue layers where skin graft take is likely. The new adipofascial flap described by Lee may widen the options in arthrolysis of the PIP joint. This distally based flap is based on branches of the dorsal digital vessels and is elevated in the plane between the skin and deep structures, then rotated to cover the joint as necessary. The same holds true for situations in which the extensor tendon apparatus is exposed and stable soft tissue coverage is required. As mentioned previously, the choice of flaps depends on the individual profile of the patient and ranges from regional flaps such as the radial forearm flap to distant flaps (groin flap) and microvascular flaps.
Full-thickness skin grafts are preferred when skin grafts will suffice for skin reconstruction. Only in cases of limited availability, as when other important areas require full-thickness skin grafts (e.g., eyelids, lips), are split-thickness grafts used.
Temporary fixation with Kirschner wires is indicated only in joints in which “elastic” resistance remains after release of the skin and ligaments and the patient will probably not be able to mobilize sufficient strength to overcome this resistance. ,
The same holds true for the PIP joint in claw deformities. In most cases there is a relative palmar tissue deficit that requires either full-thickness skin grafting or flap coverage after release. Local intrinsic hand flaps are generally limited in these hands, so distant flaps or free tissue transfers are frequently indicated because the problem is usually encountered in more than one digit.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here