Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter deals with one of the most complex—and difficult to treat surgically—of all congenital cardiac malformations: tetralogy of Fallot with pulmonary atresia. We focus particularly on tetralogy of Fallot with pulmonary atresia (TOF/PA) and major aortopulmonary collateral arteries (MAPCAs). MAPCAs are defined as systemic arterial vessels that terminate in the lung parenchyma. These vessels form during embryologic development and persist until birth and after. A wide spectrum of abnormalities of the intraparenchymal, or native, pulmonary artery system, including hypoplasia and arborization deficiencies, is essentially always present with MAPCAs. MAPCAs are most often associated with the cluster of defects that include TOF, PA, and absent ductus arteriosus. There are very good reasons why this association is most common, as will be outlined. Although this chapter deals solely with TOF/PA, it is important to appreciate that MAPCAs can be associated, albeit less often, with a wide spectrum of intracardiac anomalies, including transposition, double-outlet right ventricle, common arterial trunk, congenitally corrected transposition, PA with intact ventricular septum, other forms of single ventricle, atrioventricular septal defect, atrial isomerism, and others. The common theme that links MAPCAs with all of these varied intracardiac anomalies is that there is either absence or severe restriction of all central sources of pulmonary blood flow during embryologic development; in essence, absence of a ductus arteriosus and PA. There are unusual “transition” cases in which there is a nearly atretic but nevertheless patent pulmonary valve. A ductus arteriosus to confluent central branch pulmonary arteries is essentially never present in association with MAPCAs, although a unilateral ductus to one native branch pulmonary artery can occur with MAPCAs supplying the contralateral lung if it has no embryologic central source of blood flow.
Several arguments can be marshalled to explain why TOF is the most common intracardiac anomaly associated with MAPCAs. First, tetralogy is simply the most commonly occurring intracardiac anomaly relative to the other intracardiac anomalies associated with MAPCAs. Second, restriction of pulmonary blood flow is an intrinsic feature of tetralogy in all its forms, whereas this is not the case with some of the other anomalies. Third and most interesting, embryologic absence of the ductus arteriosus is a common occurrence in all forms of tetralogy. An absent ductus occurs in about one-third of patients with tetralogy; this association appears to span the entire spectrum of severity of tetralogy, from mild pulmonary stenosis all the way to PA. In simple tetralogy, absence of the ductus is usually of no clinical consequence, either during embryologic development or after birth, since forward flow across the stenotic pulmonary valve is an adequate source of central pulmonary artery blood flow. In TOF/PA, however, absence of a ductus arteriosus sets up the embryologic substrate for persistence of foregut blood supply to the lungs and lack of development of native pulmonary arteries (i.e., no central source of pulmonary blood flow). It is not surprising that in newborns with TOF/PA, approximately two-thirds have a ductus arteriosus, well-developed native confluent branch pulmonary arteries, and no MAPCAs, whereas about one-third have absent ductus arteriosus, abnormal native pulmonary arteries, and MAPCAs.
Because there is no uniformity in the methods of classifying the patients to be described, it is difficult to provide precise incidence for those having TOF/PA. When TOF is considered as an overall entity, the lesion makes up almost 4% of patients with congenitally malformed hearts. It is likely that up to one-tenth of these will have had PA rather than pulmonary stenosis. In many cases, the intracardiac anatomy suggests that the pulmonary outflow tract was initially patent but became atretic during fetal life. In others, particularly those with systemic-to-pulmonary collateral arteries, the atresia was probably part of the initial developmental abnormality. PA, rather than stenosis, is particularly frequent when tetralogy is found in association with deletions of chromosome 22q11. Such deletions have also been established as the cause of the velocardiofacial syndrome, which is typically found with TOF as the cardiac component of the association.
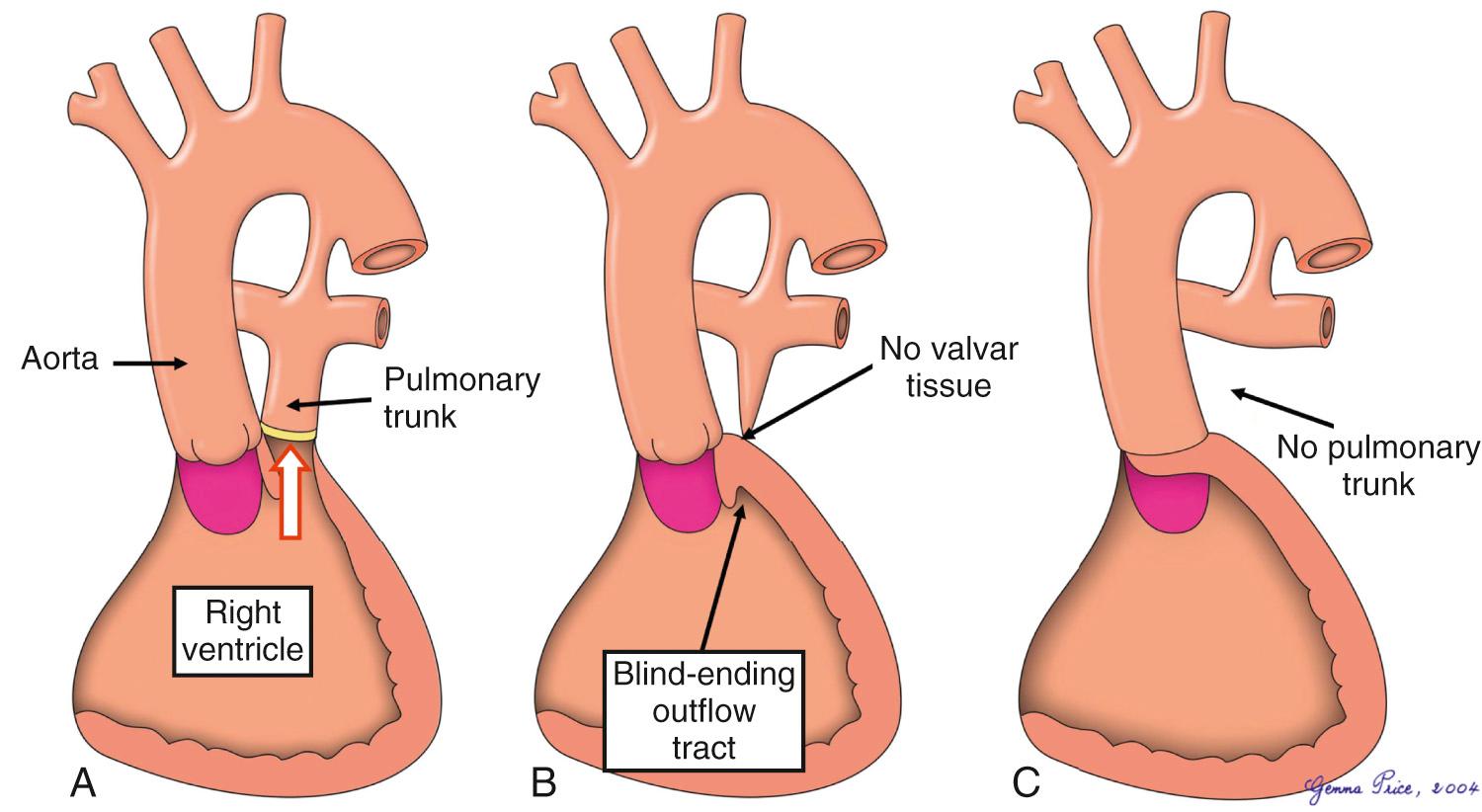
PA exists when there is either complete obstruction or absence of the communication normally present between the cavities of the ventricular mass and the pulmonary arteries. In the setting of TOF, the obstruction can sometimes be produced by an imperforate pulmonary valve ( Fig. 36.1A ). More often, the blockage of the pathway is muscular, either at the entrance to or at the distal end of the subpulmonary infundibulum ( Fig. 36.1B ). The connection is lacking when there is absence of the pulmonary trunk, with the extreme form represented by absence of all the intrapericardial pulmonary arteries ( Fig. 36.1C ).
Just as TOF with pulmonary stenosis can be found with marked variability in intracardiac morphology, so can TOF/PA. Before discussing the crucial variations in pulmonary arterial anatomy, therefore, the variations in morphology within the heart are discussed in the following paragraphs.
Significant variations are to be found in the morphology of the ventricular outflow tracts, the morphology of the interventricular communication, and the precise connection of the aorta to the ventricular mass as well as in the associated malformations. Apart from the associated malformations, these features are interrelated. To fulfil the basic diagnosis as TOF, the aorta must be connected to the ventricles in posterior position relative to the atretic pulmonary outflow tract. The aortic valvar orifice overrides the crest of the muscular ventricular septum, albeit to varying degrees. The phenotypic feature of tetralogy is seen in the structure of the subpulmonary outflow tract, with the muscular outlet septum, or its fibrous remnant, when present, being displaced anteriorly and cephalad relative to the limbs of the septomarginal trabeculation ( Fig. 36.2 ).
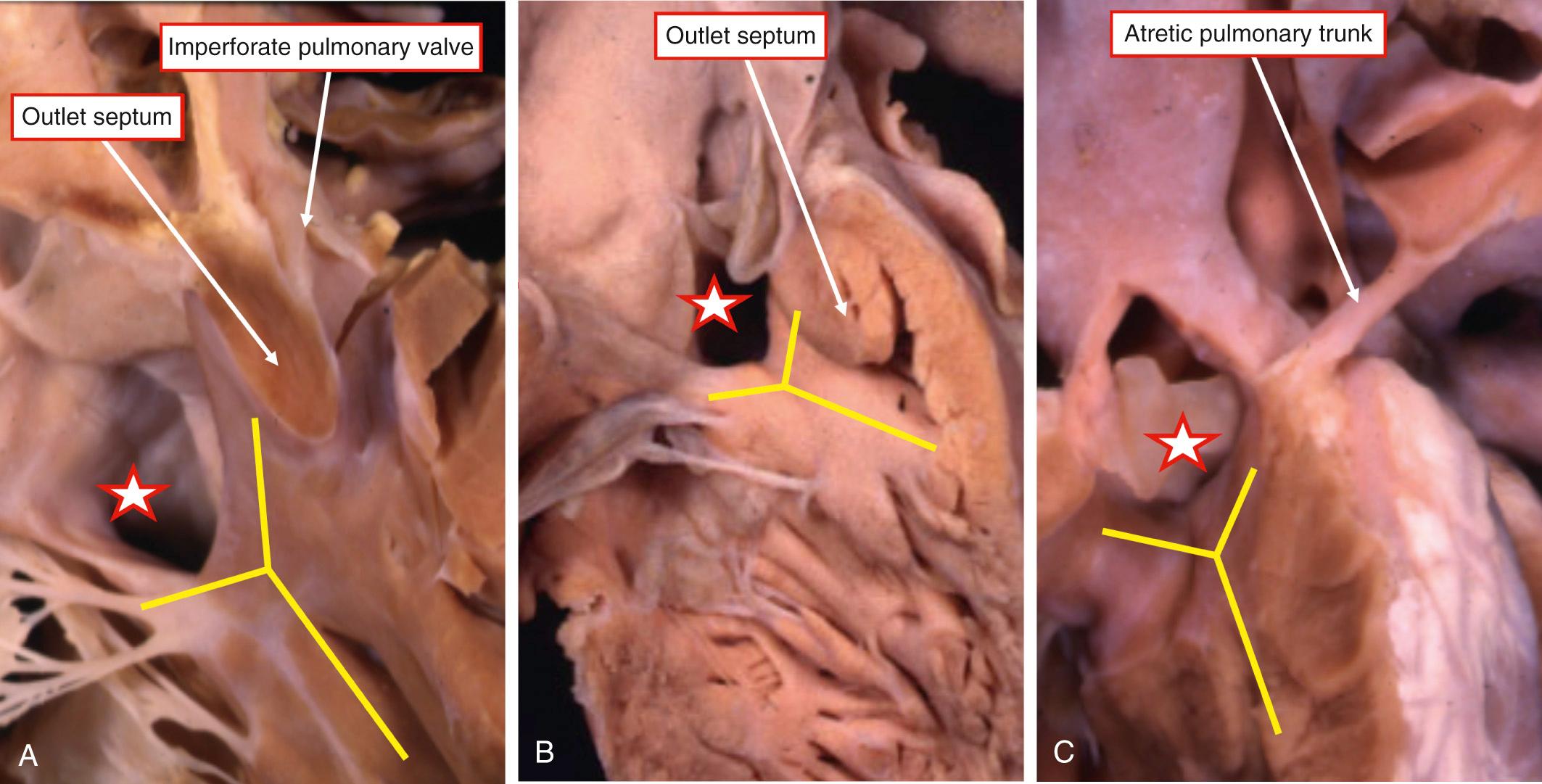
In a small number of cases, the atresia is found at the mouth of the muscular infundibulum, and the pulmonary valve itself may be patent. Alternatively, there can be an imperforate pulmonary valve (see Fig. 36.2A ). In the most common pattern, the muscular outlet septum fuses directly with the parietal musculature of the right ventricle, thus obliterating the ventriculopulmonary junction (see Fig. 36.2B ). There is a muscular wall between the cavities of the right ventricle and the pulmonary trunk. Occasionally the subpulmonary outflow tract is completely absent, so that the leaflets of the aortic valve are attached directly to the parietal ventricular wall (see Fig. 36.2C ). This arrangement is reminiscent of common arterial trunk. In the example shown in Fig. 36.2 , however, the atretic pulmonary trunk takes its origin from the right ventricular musculature, confirming that the patent arterial trunk is an aorta. Should the intrapericardial pulmonary arteries also be absent, it would be impossible to be sure whether the patent trunk had, initially, been an aorta and not a common structure. Thus the arrangement with absence of the pulmonary trunk is best described as a solitary arterial trunk, although that clinical presentation is the same as for TOF/PA. In other cases, a fibrous remnant of the outlet septum interposes between the leaflets of the aortic valve and an imperforate pulmonary valve. This arrangement represents TOF/PA in the setting of a doubly committed and juxta-arterial ventricular septal defect, as does the arrangement with complete absence of the subpulmonary infundibulum (see Fig. 36.2C ).
The ventricular septal defect, roofed by the overriding aorta, usually has a fibrous posteroinferior border made up of continuity between the leaflets of the aortic and tricuspid valves and often reinforced by a membranous flap. This arrangement makes the defect perimembranous (see Fig. 36.2A ). Cases can also be found, as in tetralogy with pulmonary stenosis, when the posteroinferior limb of the septomarginal trabeculation fuses with the ventriculoinfundibular fold. In this setting, the defect has exclusively muscular borders when viewed from its right side (see Fig. 36.2B ). This muscular rim, when present, serves to protect the ventricular conduction tissues, separating them from the crest of the septum. As discussed earlier, the defect can also extend to become doubly committed and juxta-arterial. Such doubly committed defects can themselves extend to become perimembranous, but more usually they have a muscular posteroinferior rim (see Fig. 36.2C ). Rarely the ventricular septal defect may be restrictive due to tissue tags derived from the leaflets of the tricuspid valve. In this setting, the overall anatomy of the heart is more like PA with intact ventricular septum, usually with a thick-walled right ventricle and a reduced cavity. The precise connection of the leaflets of the aortic valve, as in tetralogy with pulmonary stenosis, can vary markedly. In most instances, the leaflets of the aortic valve are connected largely within the left ventricle. Hearts can also be found with predominant or even total commitment of the aorta to the right ventricle. This last combination produces TOF/PA, but with the ventriculoarterial connection of double-outlet ventricle.
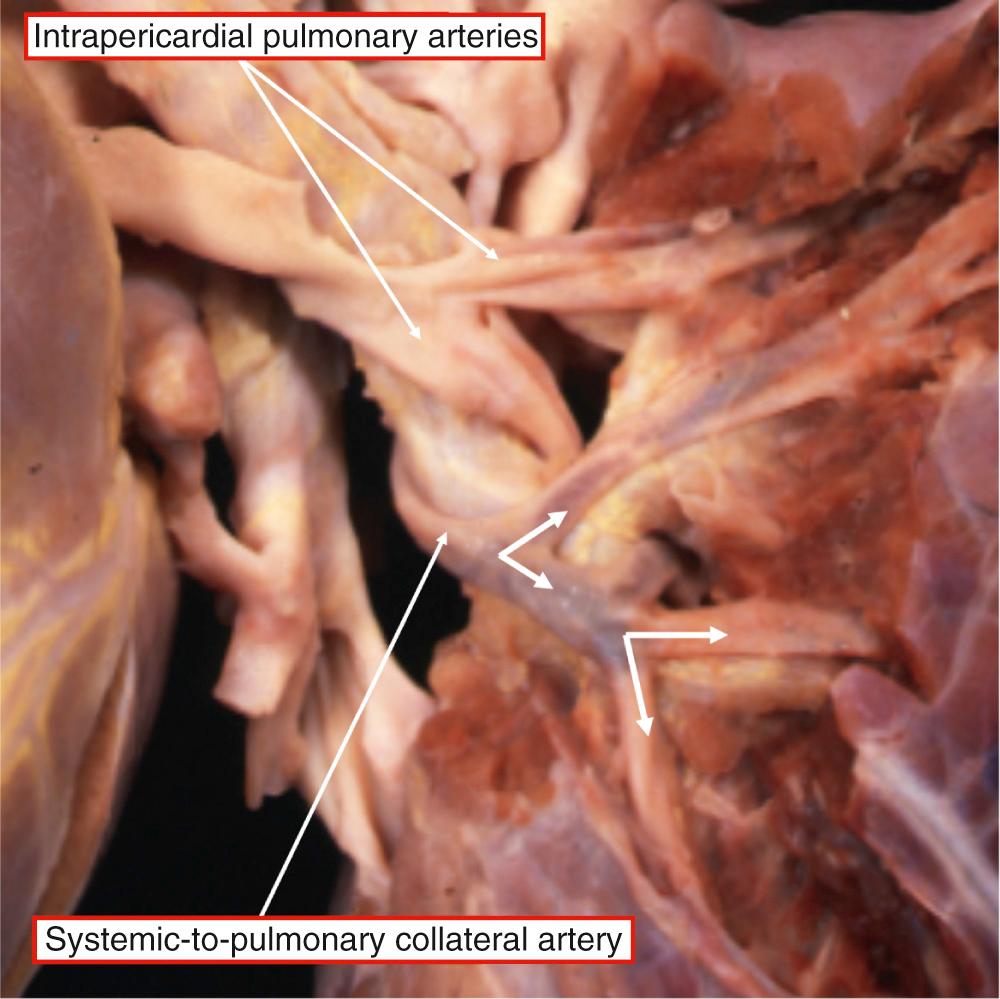
When the pulmonary valve is imperforate, the pulmonary trunk is patent to the level of the ventriculopulmonary junction (see Fig. 36.2A ). Even in this setting, the trunk itself may supply only one pulmonary artery, the other either having no connection with the pulmonary trunk or being completely absent. In many other cases, the pulmonary trunk itself is atretic. In extreme cases, it is recognizable only as a fibrous strand between the ventricular outflow tract and the pulmonary arterial confluence (see Fig. 36.2C ) or one of the pulmonary arteries. When the right and left pulmonary arteries are present, they are usually confluent. The confluence itself, usually tethered by either a patent or atretic pulmonary trunk to the ventricular mass, has the characteristic angiographic appearance of a flying seagull. It can vary markedly in size, usually depending on its source of arterial supply. The right and left pulmonary arteries can be nonconfluent, but one of them usually retains its connection to the remnant of the pulmonary trunk. Nonconfluent pulmonary arteries can rarely be found in the absence the pulmonary trunk. Each can either be supplied by one of the bilateral arterial ducts or one lung can be supplied by systemic-to-pulmonary collateral arteries with the other fed by a duct through the persisting extrapericardial pulmonary artery. In the most severe examples, the entire intrapericardial arterial tree can be lacking, with supply to the lungs exclusively through systemic-to-pulmonary collateral arteries.
The final common pathway of pulmonary blood supply is the capillaries associated with the air sacs of the lungs. These capillaries are connected to an intrapulmonary plexus of arteries, which ramifies within the bronchopulmonary segments. Different parts of the plexus can be supplied with blood from different systemic sources. If all intrapulmonary arteries are connected to unobstructed and confluent intrapericardial pulmonary arteries, the confluence typically supplies all of both lungs, and the pulmonary arterial supply is said to be unifocal. When different parts of one lung are supplied from more than one source, the supply is said to be multifocal.
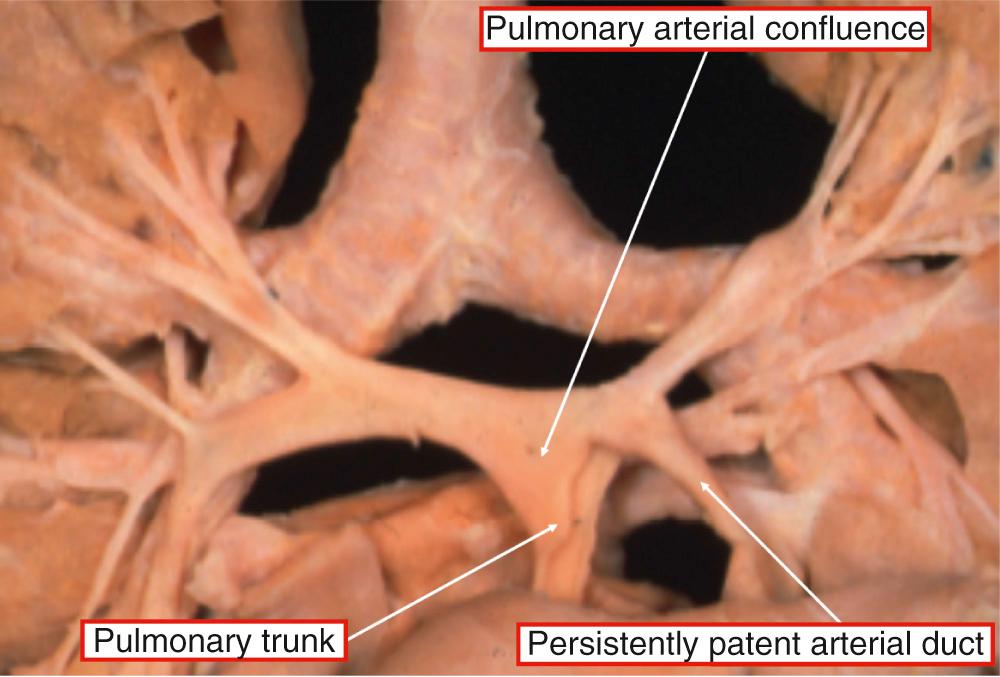
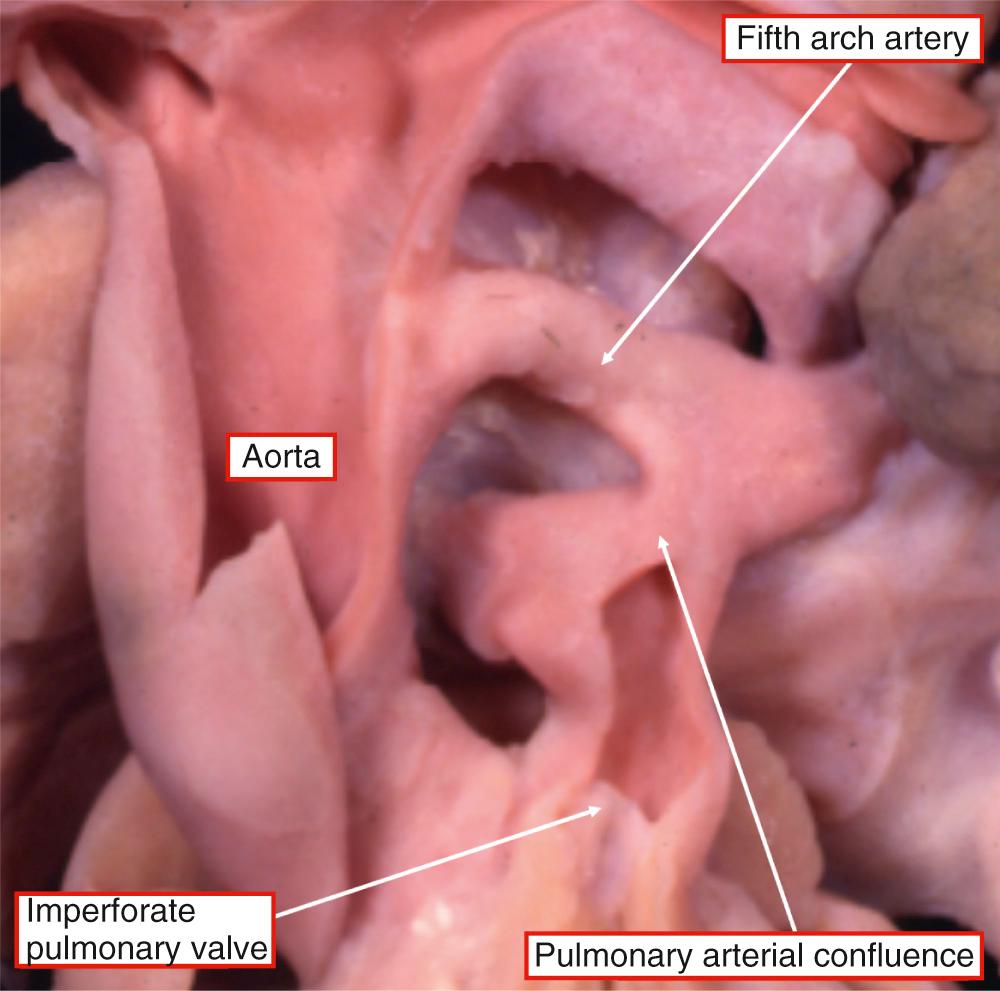
It is usually the persistently patent arterial duct that provides unifocal pulmonary arterial supply ( Fig. 36.3 ). It is exceedingly rare for confluent pulmonary arteries feeding all of both lungs to be supplied by a solitary systemic-to-pulmonary collateral artery. In rare cases, however, the confluent pulmonary arteries can be fed in unifocal fashion through an aortopulmonary window or via a fistula from the coronary arteries. The pulmonary arteries can also, rarely, be fed unifocally through a persistent artery of the fifth pharyngeal arch, such as an anomalous pulmonary artery from the ascending aorta ( Fig. 36.4 ).
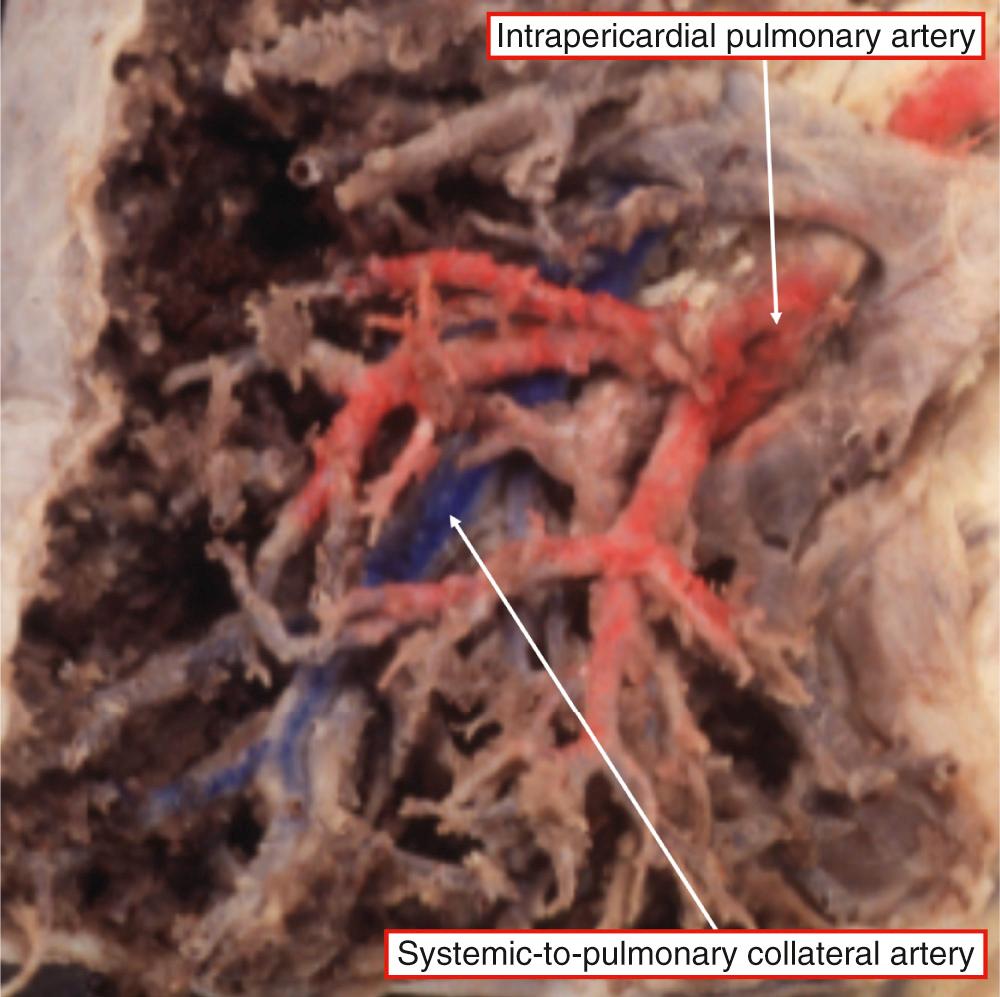
The presence of a multifocal pulmonary arterial supply creates the clinical complexity in TOF/PA. The multiple vessels feeding the pulmonary parenchyma are systemic-to-pulmonary collateral arteries ( Fig. 36.5 ).
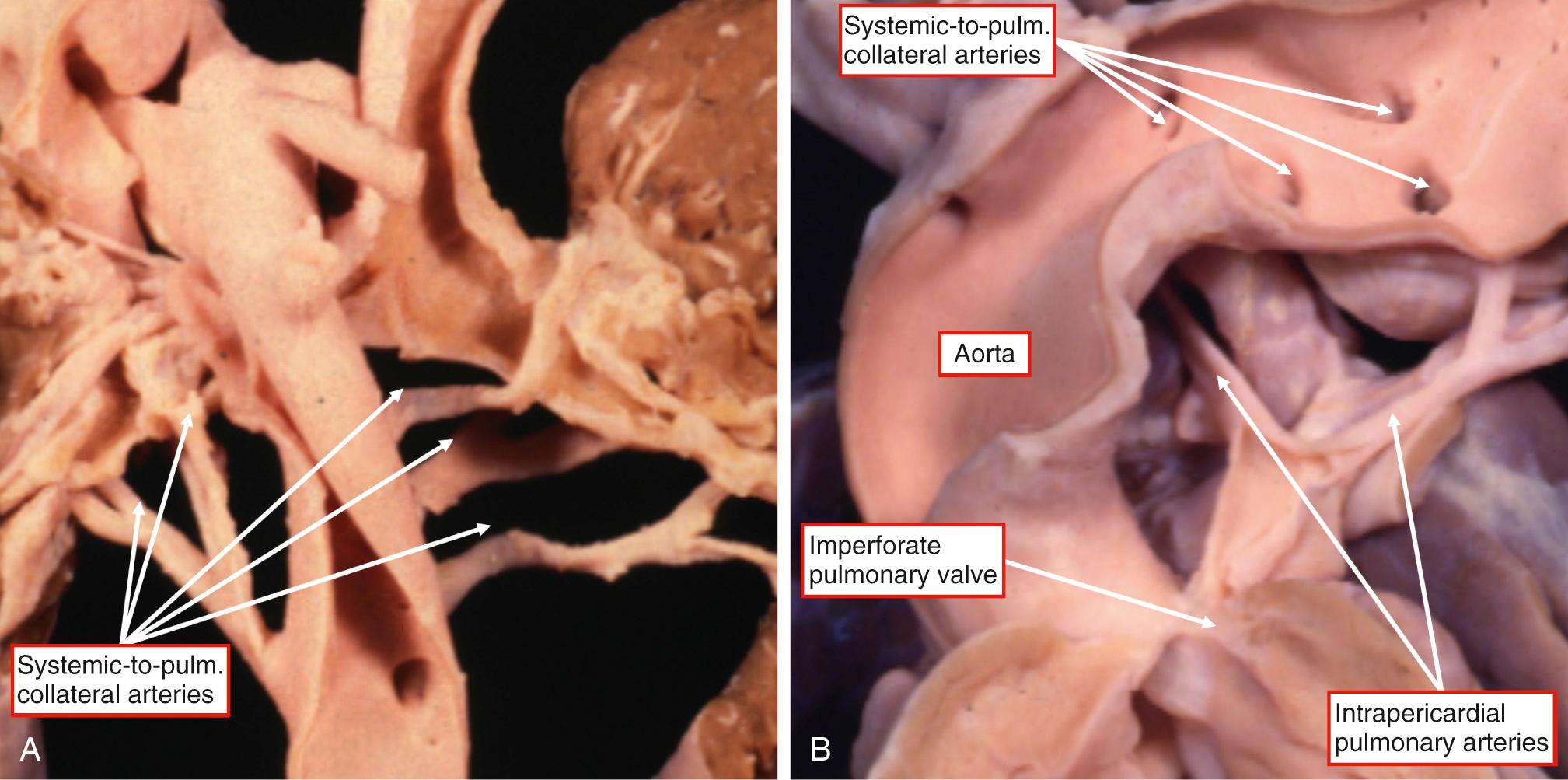
The collateral arteries hardly ever feed a lung that also receives supply via the arterial duct. It is a useful working rule, therefore, to assume that an arterial duct will not be present when a lung is supplied by systemic-to-pulmonary collateral arteries. Although the systemic-to-pulmonary collateral arteries hardly ever coexist in the same lung with an arterial duct, they do usually coexist with confluent intrapericardial (central) pulmonary arteries (see Fig. 36.5B ). In such circumstances, the confluent pulmonary arteries are usually connected to some but not all of the bronchopulmonary segments of both lungs. Instead, it is typically the case that different arteries supply different segments of the two lungs with no interconnections between them. The confluence of intrapericardial pulmonary arteries, itself fed by one or more major systemic-to-pulmonary collateral arteries, is usually connected to the greater parts of the lungs, but some components of the pulmonary parenchyma are supplied directly and exclusively by systemic-to-pulmonary collateral arteries. These individual collateral arteries, therefore, can feed individual intrapulmonary segments, or groups of segments, and are referred to as isolated supply collaterals ( Fig. 36.6 ). In a minority of cases, all of the collaterals are dual supply, meaning that they feed a pulmonary artery tree that arborizes fully to all bronchopulmonary segments.
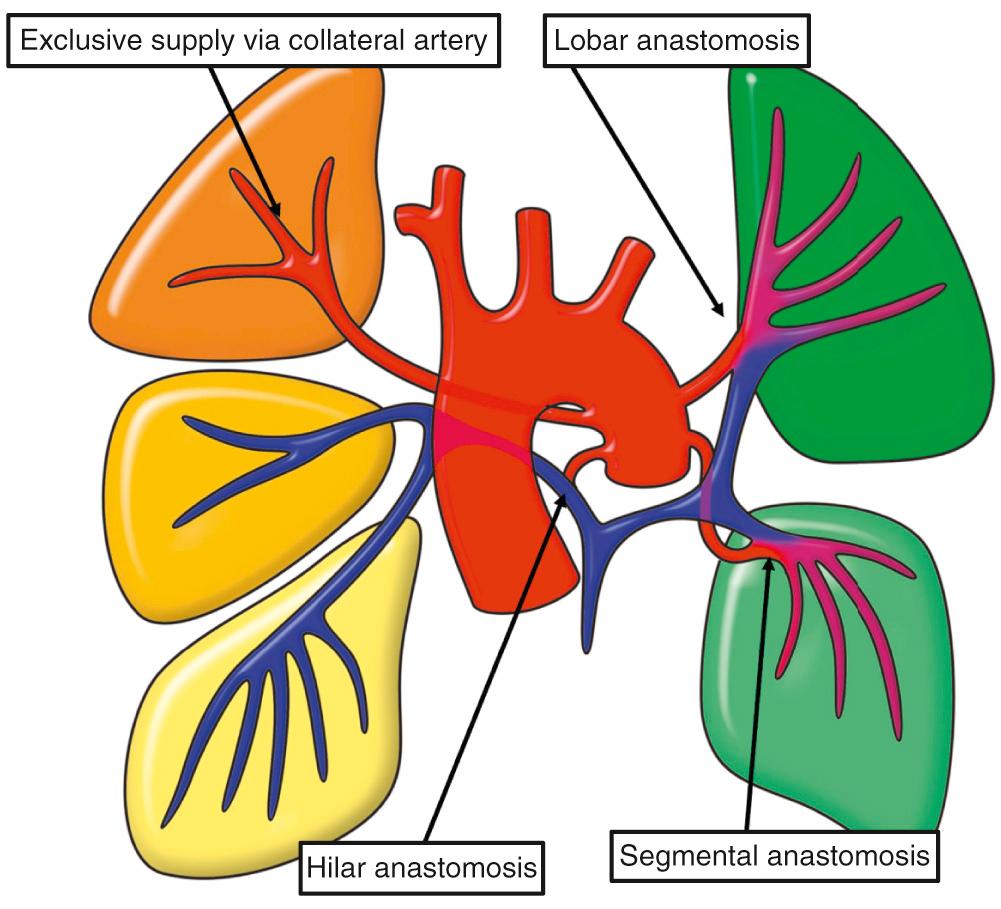
When both intrapericardial and systemic-to-pulmonary collateral arteries feed different parts of the pulmonary parenchyma, it is essential to determine the proportions supplied by each of the pathways, remembering that in the extreme form of the anomaly both lungs are fed exclusively by systemic-to-pulmonary arteries. Another variety of multifocal supply is found when the pulmonary arteries are present but nonconfluent. The different parts of the lungs may be supplied by systemic-to-pulmonary collateral arteries, by a duct or anomalous pulmonary artery from the ascending aorta, by a coronary arterial fistula or aortopulmonary window, or by a combination of these. Alternatively, the intrapulmonary arteries may not be supplied by any of these sources, with blood reaching them only at the precapillary level through acquired collateral arteries that enter the lungs either centrifugally through the bronchial arteries or centripetally via the intercostal or coronary arteries. Acquired collateral arteries can also coexist with the other varieties of arterial supply.
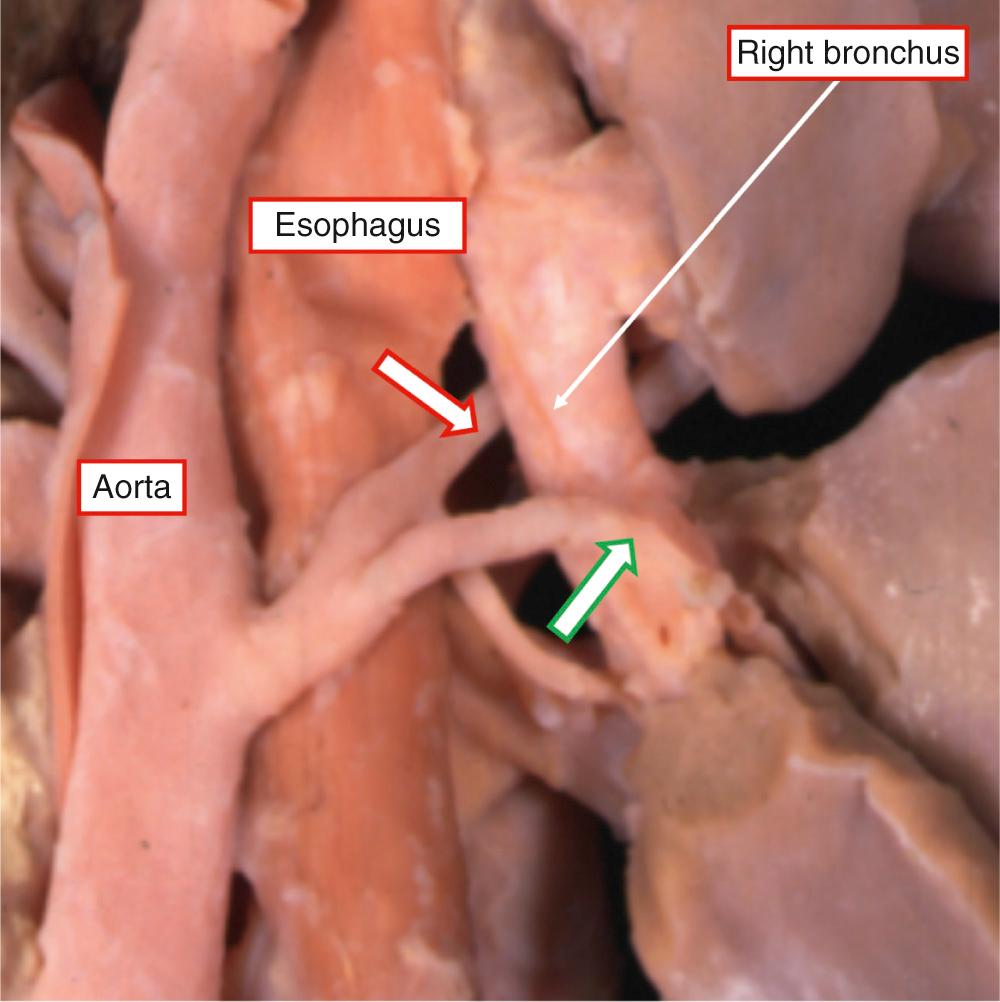
These arteries are characteristic for the so-called complex variant of TOF/PA. Their relationship to the bronchial arteries has yet to be fully established. Some of the major collateral arteries have no independent course within the lung parenchyma, extending only from a systemic artery, usually the aorta, to the origin of the intrapulmonary arteries at or near the hilum. Arteries with this morphology are simple conduits. They can pass in front of, behind, or even through the esophagus. They also frequently branch and encircle the branches of the bronchial tree ( Fig. 36.7 ).
In other circumstances, the collateral arteries extend into the lung along the bronchial tree, branching in the pattern of a bronchial artery, and also supplying the bronchial wall. A common embryologic origin of these vessels with the bronchial arteries cannot be excluded ( Fig. 36.8 ). The Melbourne group have summarized evidence to support this theory, although the Stanford group has argued against it.
Our preference is to describe these vessels as systemic-to-pulmonary collateral arteries, or major aortopulmonary collateral arteries. The arteries, typically between two and six in number, usually arise from the anterior wall of the aorta opposite the origin of the intercostal arteries (see Fig. 36.5 ). Individual collateral arteries can also take origin from the brachiocephalic arteries or even from the coronary arteries. When they arise from the aorta, the arteries frequently run a retroesophageal course (see Fig. 36.7 ). They can be distinguished from a duct by their histologic structure as well as anatomically in most cases, since the arterial duct originates only from a given point within the aortic arch, permitting its distinction from the arteries of the fifth pharyngeal arch (see Fig. 36.4 ). Even when it branches from a nondominant aortic arch, the duct originates more or less opposite the takeoff of a brachiocephalic or subclavian artery. A collateral arising in the region typical for the ductus can also be distinguished from a ductus intraoperatively by noting that the recurrent laryngeal nerve does not wrap around it.
The potentially complex situation can be simplified by recognizing three major patterns of pulmonary arterial supply: (1) confluent right and left right pulmonary arteries supplied by an arterial duct, (2) confluent intrapericardial pulmonary arteries coexisting with systemic-to-pulmonary collateral arteries, and (3) absence of intrapericardial pulmonary arteries. The most favorable arrangement is that in which the right and left pulmonary arteries are confluent and are supplied by an arterial duct (see Fig. 36.3 ). With this pattern, the pulmonary arteries themselves are usually distributed in normal fashion to all the bronchopulmonary segments. Such a pulmonary arterial supply is unifocal. In the second major pattern, the intrapericardial pulmonary arteries are confluent but coexist with systemic-to-pulmonary collateral arteries (see Fig. 36.6 ). The distribution of the confluent pulmonary arteries themselves is variable, although it is unusual to find them supplying all the bronchopulmonary segments. In most instances the blood passing through the confluence supplies two-thirds or less of the pulmonary parenchyma. Even in this setting, the ultimate supply to the pulmonary arteries is via the collateral arteries, although the anastomoses with the intrapericardial network can be found at hilar, lobar, or segmental levels (see Fig. 36.6 ). The confluence of the pulmonary arteries itself also varies markedly in size, reflecting the number of the bronchopulmonary segments supplied. In this setting the parts of the lung not supplied by the intrapericardial pulmonary arteries are fed directly by systemic-to-pulmonary collateral arteries (isolated supply), with further variation in the number of arteries present and the amount of lung supplied by each artery. In most cases the pulmonary arteries and the collateral arteries do not separately supply different portions of a given lung segment, but in some cases the two sets of arterial ramifications can intermingle within the same segment ( Fig. 36.9 ). The third typical pattern of arterial supply is encountered when there is absence of the intrapericardial pulmonary arteries. In such circumstances, all of the bronchopulmonary segments are supplied by systemic-to-pulmonary collateral arteries, which are designated as isolated supply. In the presence of systemic-to-pulmonary collateral arteries, therefore, the keys to complete clinical diagnosis are to establish the course of each artery, to document whether it runs directly into the lung or makes connections with intrapericardial and central pulmonary arteries, and to identify with precision the sites of these anastomoses.
Much has been written about the morphogenesis of both the ventricular and pulmonary arterial features of TOF/PA, although derived from speculative embryologic concepts and arguably not improving our understanding. From the stance of ventricular morphology, the anomaly is readily explained in terms of end-stage TOF, with variation depending on the specific morphology of the subarterial outlets. Some cases, in contrast, can be interpreted as representing a common arterial trunk with absence of the intrapericardial pulmonary arteries, such as those in which a solitary trunk is connected to the ventricular mass in the absence of central pulmonary arteries. In the setting of absence of the intrapericardial pulmonary arteries and with no evidence of a subpulmonary infundibulum within the right ventricle, the distinction between a common trunk as opposed to an aorta depends on whether, had the intrapericardial pulmonary arteries been present, they would have taken origin from an arterial trunk or directly from the right ventricle. This argument cannot be considered hypothetical, since hearts do exist with an atretic pulmonary trunk arising from an arterial trunk, thus showing that the trunk itself was initially a common structure. Studies of rats dosed with bisdiamine, furthermore, have revealed that some fetuses developed TOF, whereas others exhibited a common arterial trunk with PA. From the standpoint of description, the conundrum is resolved simply by describing the ascending great artery found in the absence of the pulmonary trunk as a solitary arterial trunk rather than an aorta.
Embryology has also long been used to explain the typical patterns of pulmonary arterial supply. Thus the lungs in TOF/PA are supplied either through the confluence of the pulmonary arteries fed by the arterial duct, itself derived from the embryologic sixth aortic arch, or else through systemic-to-pulmonary collateral arteries. Initially the developing intrapulmonary arterial plexus is connected to the primitive intersegmental arteries that in turn, are connected to the arteries coursing through the pharyngeal arches, eventually retaining connection to the arteries of the fourth arch. It is suggested that when the intrapulmonary plexus eventually achieves its connection to the sixth arch, it loses its connections with the systemic arterial system. The systemic-to-pulmonary collateral arteries are explained on the basis of persistence of the primitive intersegmental arteries, some of which also become bronchial arteries. It is argued that these collateral arteries persist only in the absence of the duct, which is the critical connection between the structures derived from the sixth arch and the aortic sac. This concept accounts adequately for the majority of cases and offers an excellent working hypothesis. In the majority of cases, nonetheless, these developmental considerations aid in providing an explanation of the complexity of the pulmonary arterial supply. In essence, the intraparenchymal pulmonary arteries develop along with the lungs. They are the final common pathway supplying arterial blood to the pulmonary air sacs. This common pathway can be supplied at the hilum, either by the intrapericardial pulmonary arteries fed through the arterial duct, the derivative of the artery to the sixth pharyngeal arch, by the rarer sources of unifocal supply, or else by systemic-to-pulmonary collateral arteries, which are primitive intersegmental arteries. These sources of supply can anastomose with different parts of the lungs in the same patient, although usually all the arteries in one lung are supplied either by the duct or else by the systemic-to-pulmonary collateral arteries. The common pathway can subsequently be further enhanced by acquired collateral arteries, which reinforce the acinar supply at precapillary level.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here