Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tendon transfers in the upper limb are indicated to restore function to paralyzed muscle and tendon following nerve injury, direct muscle, or tendon injury, and to restore balance to hands affected by neurological disease.
In selecting donor tissue, the surgeon has to consider expendability of the muscle–tendon unit, the native strength of donor and paralyzed muscle, and the direction of transfer and integrity of the muscle.
The timing of tendon transfers can be classified as early, conventional, or late.
Upper extremity neurological injury can be subdivided into radial nerve palsy, low and high median nerve palsy, low and high ulnar nerve palsy, and combined nerve injuries.
There are three general indications for tendon transfers in the upper extremity:
To restore function to a paralyzed muscle due to injuries of the peripheral nerves, the brachial plexus, or the spinal cord.
To restore function following closed tendon ruptures or open injuries to the tendons or muscles.
To restore balance to a deformed hand due to various neurological diseases.
Tendon transfers are best conceptualized as a means to restore a lost “function”, rather than a means of substituting for a specific muscle, i.e., restoring strong pinch as opposed to restoring function of the flexor pollicis longus (FPL) ( Table 26.1 ).
| Soft tissue equilibrium |
| Full passive range of motion of involved joints |
| Adequate amplitude of donor muscle |
| Adequate excursion of donor muscle |
| Direct line of pull |
| Single function for each transferred tendon |
| Synergy of transfer |
Timing of tendon transfers may be classified as early, conventional, or late.
A conventional tendon transfer: usually performed after reinnervation of the paralyzed muscle fails to occur 3 months after the expected time of reinnervation based on the rate of nerve regeneration of 1 mm per day.
Early tendon transfer: performed simultaneously with peripheral nerve repair or before the expected time of reinnervation of the muscle; serves as a temporary substitute for the paralyzed muscle until reinnervation occurs, by acting as an internal splint.
Before performing tendon transfers:
All fractures should be healed.
Chronic scarred skin and subcutaneous tissues or skin grafts in the line of pull of a tendon transfer should be excised and the defect resurfaced with a flap that is itself allowed to heal with mature scars.
Full passive range of motion of the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints should be achieved by physical therapy and dynamic splinting.
The donor muscle–tendon unit must be expendable. Its sacrifice must not create an important new deficit.
If multiple tendon transfers are required, a minimum of one wrist flexor, one wrist extensor, and one extrinsic flexor and extensor tendon to each digit should always be retained.
The potential excursion of a donor muscle–tendon unit must be sufficient to restore the specific lost function.
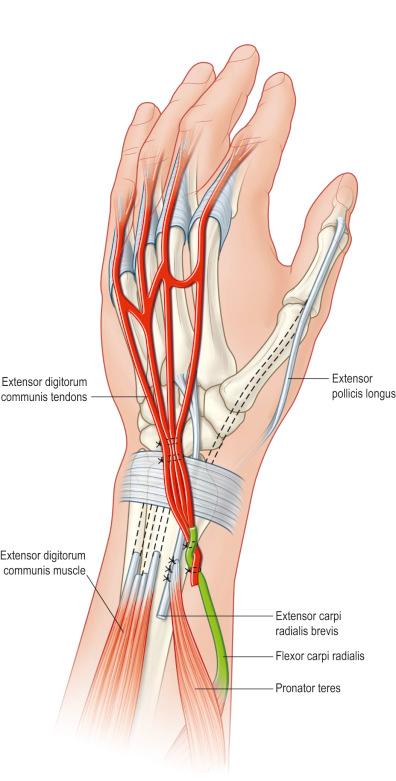
The finger flexors have an amplitude of 70 mm, the finger extensors 50 mm, and the wrist flexors and extensors 33 mm ( Fig. 26.1 ).
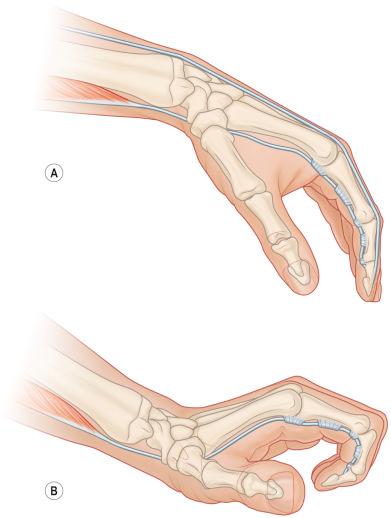
The tenodesis effect of wrist flexion or extension may also increase the effective amplitude of a tendon transfer by 25 mm.
Excursion of a donor muscle may also be increased by extensive release of its surrounding fascia.
A tendon transfer should pass in a direct line from the origin of the donor muscle to its new insertion.
Tendon transfers should only act across one joint and perform one single function.
However, a transfer may be inserted into several recipient tendons as long as they each perform the same function in adjacent digits.
The donor muscle selected should preferably be synergistic with the function of the muscle to be restored or at least be potentially retrainable.
Every muscle in the forearm and hand should be tested by manual muscle testing to document which are functioning and their strength grade.
From this list of functioning muscles, only those that are expendable are available as donor transfers.
The specific functions of the hand that need to be restored are listed in order of priority.
The final step is to match the available donor muscles with the functions that need to be restored, based on the force, amplitude, and direction of the various muscles available.
The success of any tendon transfer depends entirely on preventing scarring or adhesions along the path of the transferred tendon.
Incisions should be carefully planned prior to elevation of the tourniquet so that the final tendon junctures lie transversely beneath skin flaps rather than lying immediately beneath and paralleling the incisions.
The donor muscle should be carefully mobilized to prevent damage to its neurovascular bundle, which usually enters in the proximal third of the muscle.
The transferred tendon should glide in a tunnel through the subcutaneous tissues and not cross bone devoid of uninjured periosteum or through small fascial windows.
Only the distal end of the tendon should be grasped with surgical instruments and care taken to prevent desiccation of the tendon.
Tendon junctures are performed using a Pulvertaft weave technique where possible.
Functional motor deficit: inability to extend the wrist, inability to extend the fingers at the MCP joints, inability to extend and radially abduct the thumb ( Fig. 26.2 ) , and inability to stabilize the wrist with grip resulting in marked weakness in grip strength.

Tendon transfers are required to provide wrist extension, extension of the fingers at the MCP joints, and extension and radial abduction of the thumb.
Unlike the median and ulnar nerves, sensory loss following radial nerve injury is not functionally disabling unless the patient develops a painful neuroma.
Timing of tendon transfers: remains controversial. Either “early” tendon transfer simultaneously with repair of the radial nerve to act as an internal splint to provide immediate restoration of power grip, or delay any tendon transfers until reinnervation of the most proximal muscles, brachioradialis, and extensor carpi radialis longus (ECRL) fails to occur within the calculated time limit.
The more proximal the nerve injury, the less likely that functional muscle reinnervation will occur. If the nerve remains in continuity, most surgeons would suggest that 3 months of observation are indicated to await spontaneous recovery in peripheral nerve palsies.
Several different tendon transfers have been reported for radial nerve palsy, but three patterns of transfer have evolved.
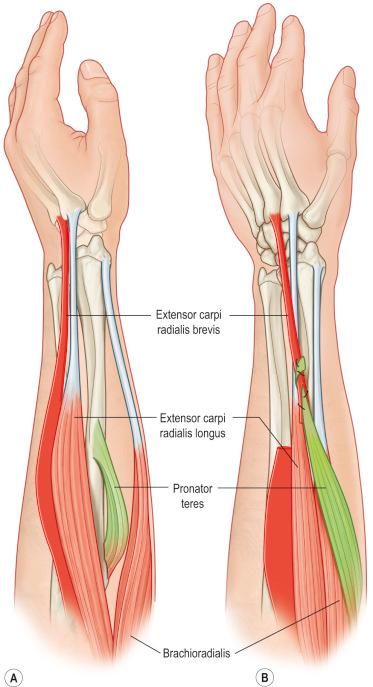
The use of pronator teres (PT) to provide wrist extension has become universally accepted, the only remaining controversy being whether to insert PT into extensor carpi radialis brevis (ECRB) alone or into both ECRL and ECRB.
The three patterns of tendon transfer differ therefore only in the technique of restoring finger extension and thumb extension and radial abduction ( Table 26.2 ).
| Standard FCU transfer | FCR transfer | Boyes superficialis transfer |
|---|---|---|
| PT to ECRB | PT to ECRB | PT to ECRB |
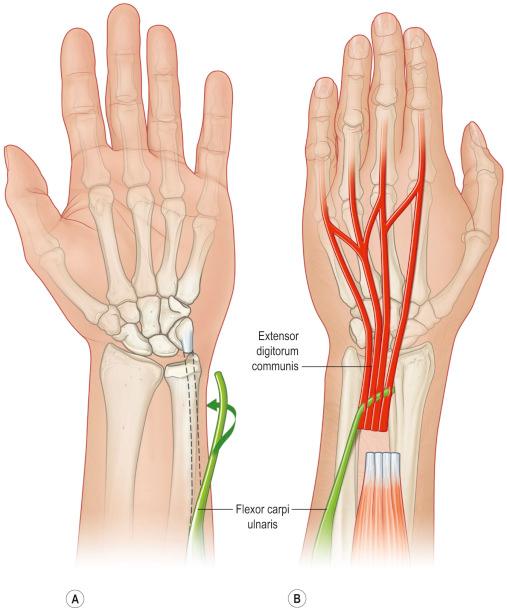
| FCU to EDC | FCR to EDC | FDS of ring finger to EDC middle, ring, and small fingers |
| PL to EPL | PL to EPL | FDS middle finger to EIP and EPL |
| FCR to APL & EPB |
This is the author's preferred technique for radial nerve palsy; in the patient with a posterior interosseous nerve palsy, the flexor carpi radialis (FCR) transfer is preferred ( Figs. 26.3–26.7 ) .


See Fig. 26.8 .
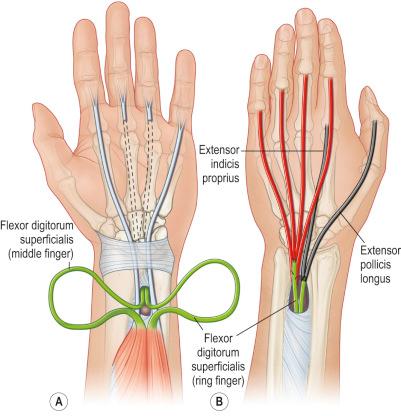
Boyes advocated using the superficialis tendons to the long and ring fingers to act as donor tendons to restore finger extension.
Advantages: potentially allow simultaneous wrist and finger extension, may allow independent thumb and index finger extension, does not weaken wrist flexion.
Disadvantages: the long and ring fingers are deprived of superficialis function, and this may result in weak grip; harvesting of the superficialis tendons may also lead to the subsequent development of either a “swan neck” deformity or a flexion contracture at the PIP joint ( Fig. 26.9 ) .
Functional deficit: loss of opposition of the thumb and absent sensation over the thumb, index, long and radial half of the ring finger.
Opposition is a composite motion, which occurs at all three joints to position the thumb pad opposite the distal phalanx of the partially flexed long finger.
Abduction, pronation, and flexion occur at the carpometacarpal joint, abduction and flexion at the MCP joint, and either flexion or extension at the interphalangeal (IP) joint.
Prior to any opposition transfer, patients with median nerve injuries should be instructed to prevent the development of an adduction or supination contracture of the thumb by a program of passive abduction exercises.
If patients present with an established adduction or supination contracture of the thumb, release of the thumb–index finger webspace skin, fascia over the first dorsal interosseous muscle, or even the first dorsal interosseous and adductor muscles themselves may be required prior to any opposition tendon transfer.
Opposition transfers that are directed along the radial aspect of the palm will produce a greater component of palmar abduction, whereas transfers that pass from the pisiform will produce both abduction and pronation. The more distal the transfer passes across the palm, the greater the power of thumb flexion.
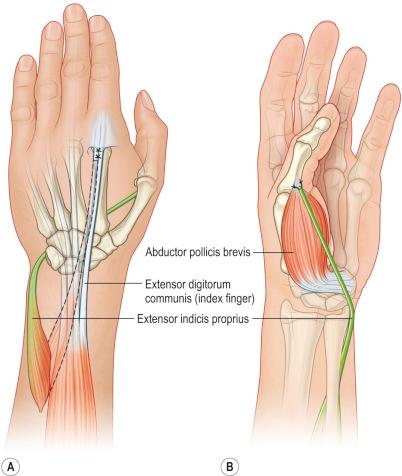
Several methods of insertion of opposition transfers have been advocated; however, a biomechanical study has shown that opposition tendon transfers inserted into the abductor pollicis brevis (APB) tendon alone will produce full abduction and pronation. Therefore, the more complex dual insertions should probably be reserved for combined median and ulnar nerve palsies.
Conventional timing of an opposition tendon transfer may only be required in those patients who fail to demonstrate signs of reinnervation within the usual calculated time interval.
For older patients or those with poor prognostic co-morbid factors, early tendon transfers should be considered.
Careful observation of thumb function following either a low or high median nerve palsy will reveal whether an “early” tendon transfer for thumb opposition is necessary.
Flexor pollicis brevis (FPB) remains innervated by the ulnar nerve in approximately 70% of median nerve injuries so that thumb function may not be significantly compromised. If the patient is able to pick up an object with the forearm in neutral or grasp an object with the forearm in supination, it is likely that FPB remains innervated by the ulnar nerve, and consequently, the decision for performing an “early” opposition tendon transfer can be delayed.
If the surgeon or therapist observes the patient attempting to grasp objects by radial abduction of the thumb with the forearm in pronation, an “early” opposition tendon transfer should be strongly considered. (Burkhalter extensor indicis proprius (EIP) transfer).
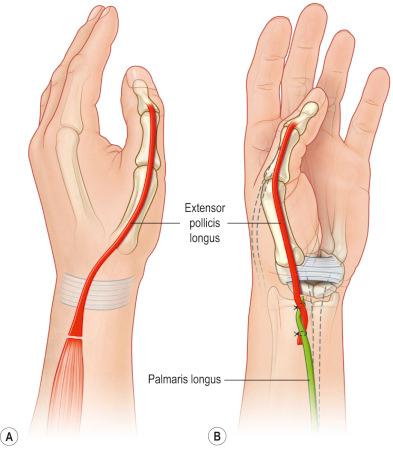
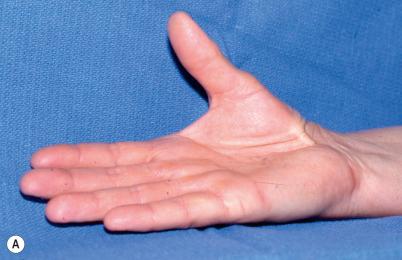
The EIP transfer is the author's preferred technique ( Fig. 26.10A,B ; ), except in elderly patients with thenar atrophy secondary to severe carpal tunnel syndrome ( Fig. 26.11 ) . The only potential disadvantage with this tendon transfer is that the EIP tendon is only just long enough to reach the APB tendon. The postoperative results have been very predictable ( Fig. 26.12 ) .

Bunnell described using the ring finger superficialis tendon as the donor for opponensplasty ( Figs. 26.13 , 26.14 ) .
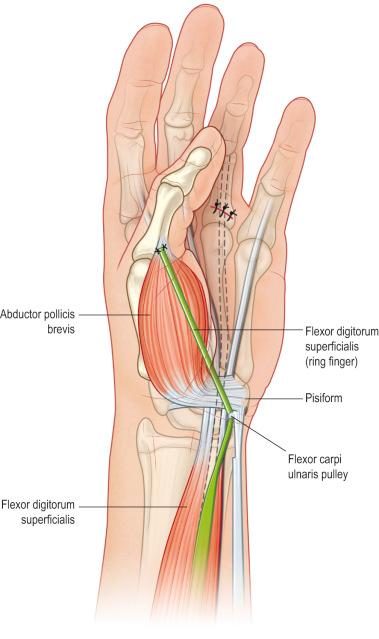
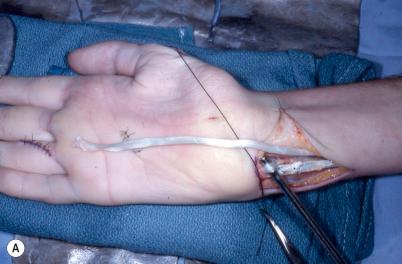
Compared with the EIP transfer, the ring finger superficialis is relatively stronger and has greater length.
Contraindications:
High median nerve palsy or in low median nerve injuries in which there have been associated injuries to the flexor tendons.
Combined low median and high ulnar nerve palsies since the ring finger superficialis is the only remaining flexor tendon in the ring finger.
Low median–low ulnar nerve palsies as the ring finger superficialis may be required for correction of clawing.
Harvesting of the superficialis tendon may result in either a flexion contracture or a “swan-neck” deformity of the PIP joint of the donor finger.
This is perhaps the strongest of the opposition transfers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here