Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The prediction of sudden cardiac arrest from ventricular arrhythmias remains challenging. Ventricular arrhythmias can occur from all major myocardial diseases and are the most common cause of sudden cardiac death. Malignant arrhythmias are most frequently due to coronary artery disease but can also originate from nonischemic cardiomyopathies. Patients who are at risk of suffering from ventricular arrhythmias can receive medical treatment to lower their risk and most often receive an implantable cardioverter defibrillator (ICD).
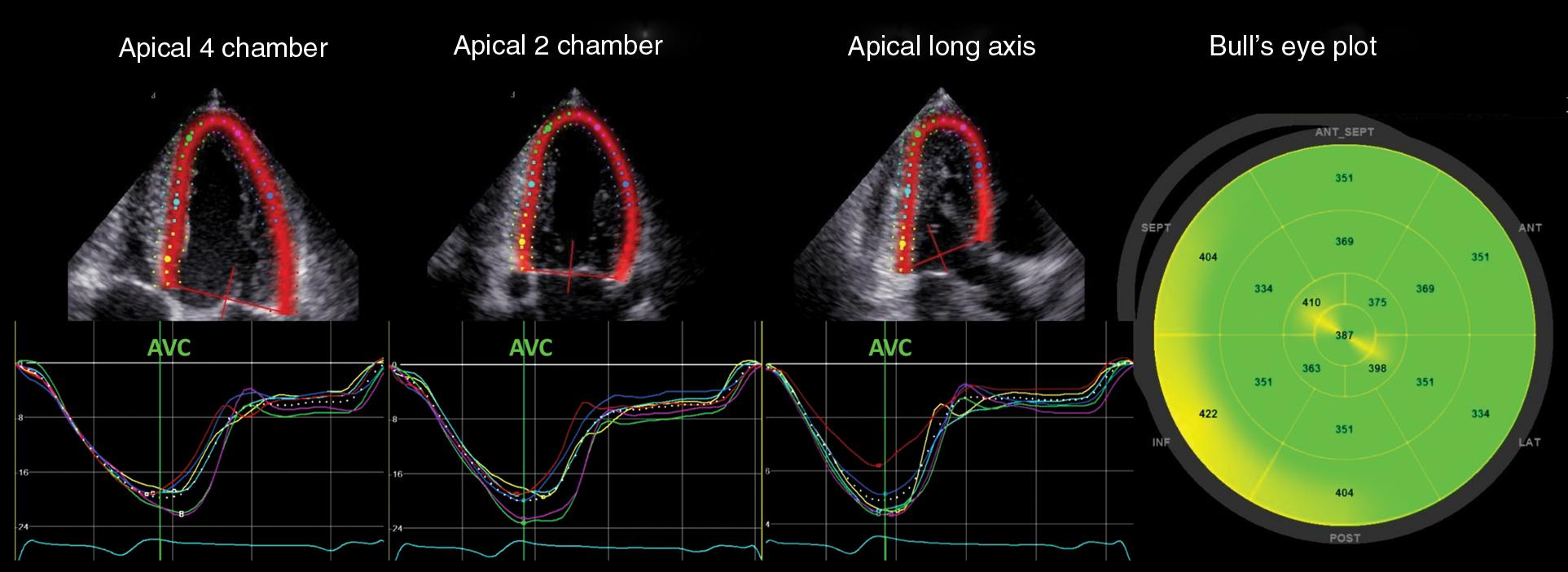
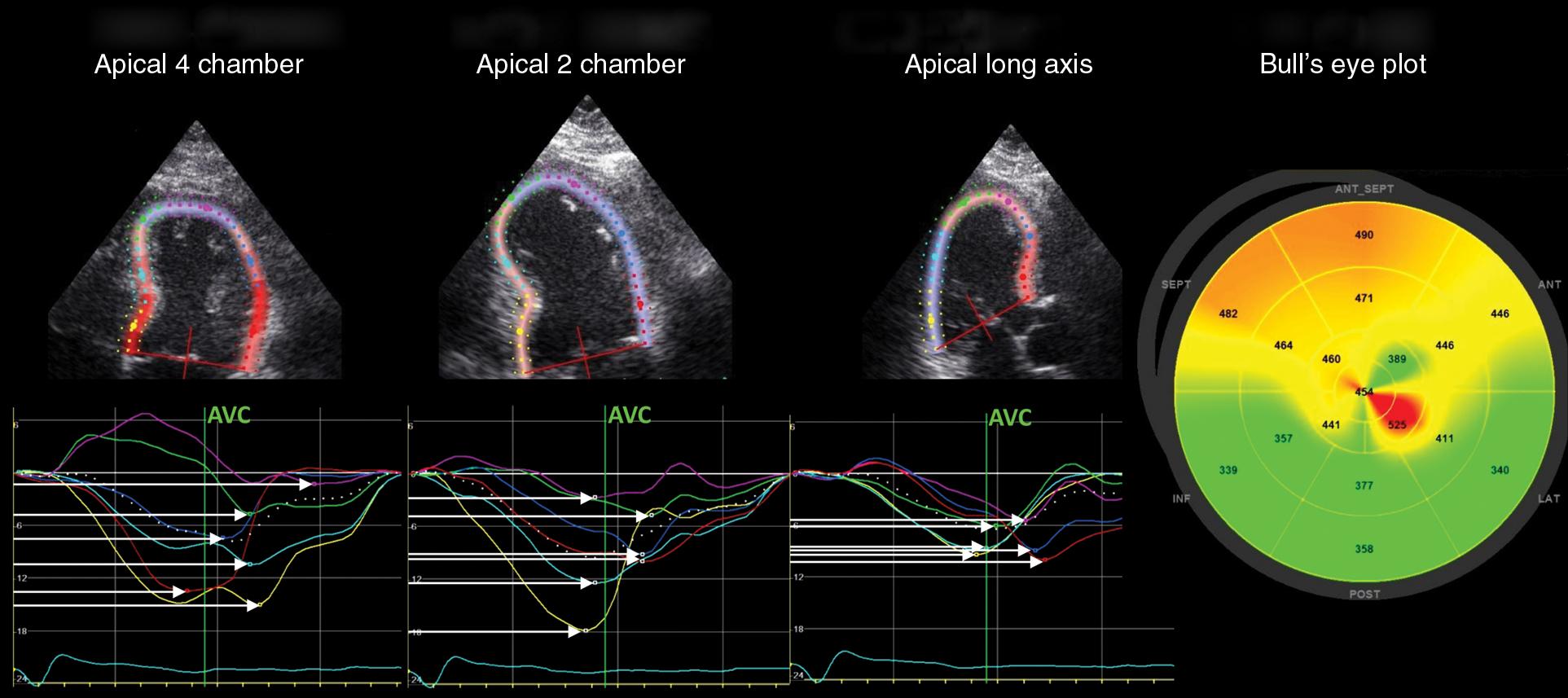
The most common diagnostic echocardiographic tool to predict patient risk has traditionally been left ventricular ejection fraction (LVEF). Although the LVEF has been used as a criterion for ICD placement, it has limited abilities in predicting arrhythmic risk. In contrast to the normal left ventricles, in which all segments contract synchronously ( Fig. 5.1 ), pathologic ventricles show temporal dispersion of contraction ( Fig. 5.2 ). Mechanical dispersion has been proposed to be a more accurate measure for risk prediction and the pathophysiology, and its assessment and potential use in risk prediction will be presented in this chapter.
There is general agreement that conduction abnormalities and dispersion of action potential duration are required for the occurrence of malignant ventricular arrhythmias. The presence of myocardial scar is regarded as important for the electrical mechanisms and substrate leading to lethal reentrant ventricular arrhythmias. , Scar tissue causes areas of slow conduction that generate dispersion of cardiac action potentials. Electrical dispersion of repolarization does exist in normal myocardium—there are differences in action potential duration from the endocardium to the epicardium, and from the LV apex to LV base. This electrical heterogeneity and dispersion increase in ischemic myocardium and have been shown to be arrhythmogenic. , These mechanisms have been linked to myocardial tissue heterogeneity present after myocardial infarction (MI), and presence of infarcted tissue or scar forms the substrate for malignant reentrant arrhythmias. , More extensive tissue heterogeneity correlates with increased ventricular irritability by programmed electrical stimulation. The magnitude of myocardial scar can be assessed by cardiac magnetic resonance (CMR) imaging and has been correlated with the risk of arrhythmias in patients after myocardial infarction.
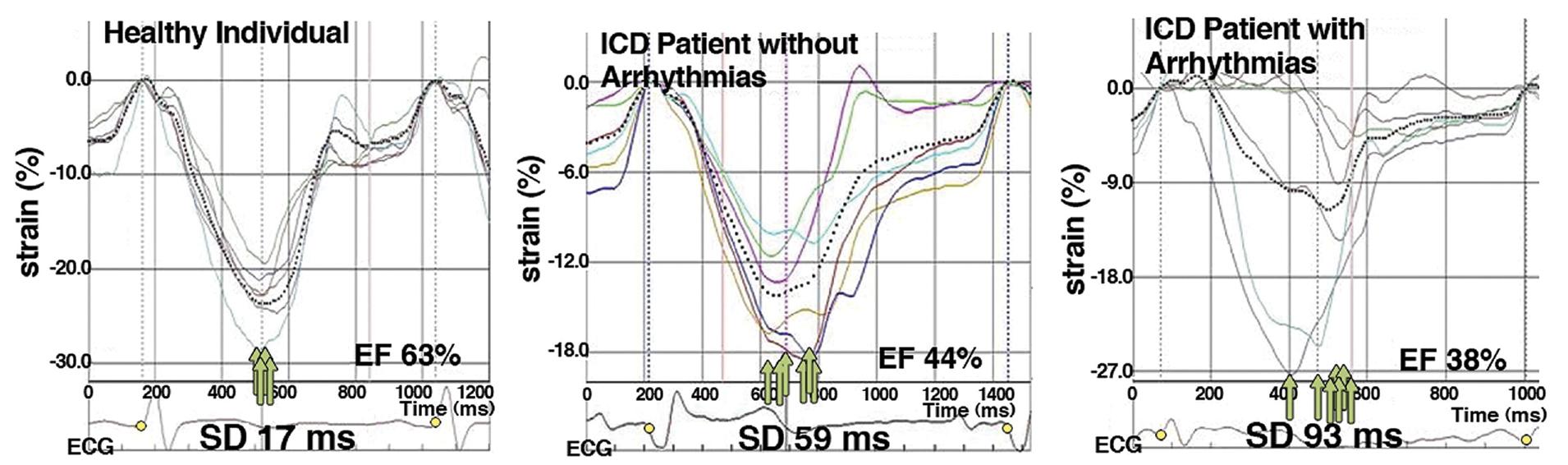
The heterogeneous contraction patterns will cause delays in the LV maximum shortening that can also occur during early diastole and after mitral valve opening. These patterns may be detected by careful assessment of LV function. Speckle-tracking echocardiography has been repeatedly demonstrated to be an accurate and sensitive means of assessing LV function and is well suited to explore a heterogeneous contraction pattern. , Mechanical dispersion is defined as the standard deviation of time from the onset of the Q/R wave on the electrocardiogram (ECG) to peak negative strain in 16 LV segments. Mechanical dispersion has been introduced as a measure of heterogeneous ventricular contraction patterns, and its ability to predict ventricular arrhythmias has been demonstrated in numerous studies ( Fig. 5.3 ).
The electrically dispersed patterns in nonischemic cardiomyopathies originate from mechanisms other than those described in ischemic cardiomyopathy. However, clear similarities in the mechanisms leading to the heterogeneous ventricular contraction patterns of ischemic cardiomyopathy may exist in patients with nonischemic cardiomyopathy. Fibrotic tissue, scar, and tissue heterogeneity provide a substrate for ventricular arrhythmias similar to ischemic cardiomyopathies. Myocardial scar will ultimately lead to a heterogeneous contraction pattern, which can be reflected by mechanical dispersion assessed by speckle-tracking strain echocardiography.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here