Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Dizziness is a common but very nonspecific chief complaint about which some elaboration by the patient is generally required for the physician to understand exactly what the patient is experiencing. The description of the sensation is critical in distinguishing whether it is caused by vertigo, disequilibrium, lightheadedness, presyncope, or ataxia ( Table 7.1 ). Although the differential diagnoses of these entities may overlap, there are conditions that are most specific to the individual symptom. All the entities are conditions that may affect children at any age, but older children are more capable of articulating the abnormal sensation they feel. Children younger than 6 years of age may present with nausea, vomiting, ataxia, or syncope.
| Vertigo | Presyncope | Disequilibrium | Lightheadedness | |
|---|---|---|---|---|
| Patient complaint | “My head is spinning” “The room is whirling” |
“I feel I might pass out” “I feel faint” “I feel like blacking out” |
“I feel unsteady” “My balance is off” |
“I feel dizzy” “I feel disconnected, drugged” |
| Associated features | Motion, swaying, spinning, nystagmus | Syncope: loss of postural tone, brief loss of consciousness Situational |
Poor balance No vertigo or ataxia |
Anxiety, hyperventilation, paresthesias, respiratory alkalosis, panic attacks |
| Usual cause | Vestibular disorders | Impaired cerebral perfusion | Sensory and/or central neurologic dysfunction | Anxiety and/or depressive disorders |
| Key differential diagnoses | Peripheral (labyrinthine- cochlear)vs Central neurologic disorder |
Neurocardiogenic (vagal)vs Cardiac syncopevs Neuropsychiatric syncope |
Sensory deficitvs Central neurologic disease |
Anxiety/depressionvs Hyperventilationvs Medication effects |
Syncope is the abrupt transient loss of consciousness and postural tone that results from inadequate cerebral perfusion. There is a rapid and spontaneous recovery. Syncope is a common phenomenon in children and adolescents that is usually benign. Between 30% and 40% of all adolescents and young adults have had one episode of syncope.
Presyncope is the feeling that the person is “about to pass out.” The patient feels as if they are going to lose consciousness but does not. The patient may experience lightheadedness, tunnel vision, graying out, and a spectrum of altered consciousness without loss of consciousness. Presyncope may or may not reflect the same pathophysiologic process as true syncope. Presyncope may abort or progress to syncope. The diagnostic approach to presyncope is the same as for syncope.
Dizziness must be considered a change in mental status. It may potentially herald serious underlying central nervous system dysfunction. Dizziness must be better defined to distinguish vertigo from lightheadedness. The principal distinction with vertigo is the description of perceived environmental motion: swaying, whirling, or spinning. Lightheadedness is frequently associated with psychological stress, including anxiety, hyperventilation, depression, and panic attacks. The history surrounding episodes of lightheadedness is vital for formulating the differential diagnosis.
Disequilibrium refers to “balance problems” without vertigo. The characteristic historical feature is difficulty ambulating. A rare complaint among children, disequilibrium in the young is most often caused by vestibular or cerebellar dysfunction and manifests as ataxia. Ataxia is an impairment of coordination, movement, and balance; this impairment is generally associated with dysfunction of the cerebellum or of the sensory and/or motor pathways connecting to the cerebellum. There are transient forms and progressive degenerative conditions that produce ataxia.
Syncope is a common phenomenon among children and adolescents. As many as 40% of children experience a syncopal event between the ages of 8 and 18 years. Before age 6 years, syncope is very unusual except in the setting of seizure disorders, breath-holding spells, systemic illnesses, and primary cardiac dysrhythmias. Syncopal episodes cause a large number of health care visits and a number of admissions to hospitals. Neurocardiogenic syncope (vasovagal) is reported as the most common cause followed by cardiogenic syncope. The differential diagnosis of syncope is noted in Tables 7.2 and 7.3 ; distinguishing features are noted in Tables 7.4 and 7.5 .
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Diagnostic Consideration |
| Neurocardiogenic |
|
| Organic Heart Disease (e.g., Coronary Artery Disease, Aortic Stenosis, Primary Arrhythmia, Obstructive Hypertrophic Cardiomyopathy, Pulmonary Hypertension) |
|
| Neurologic |
|
| Other Vascular |
|
| Drug Induced |
|
| Psychiatric Illness |
|
| Features | Syncope | Seizures |
|---|---|---|
| Relation to posture | Common | No |
| Time of day | Diurnal | Diurnal or nocturnal |
| Precipitating factors | Emotion, injury, pain, crowds, heat, exercise, fear, dehydration, coughing, micturition | Sleep loss, drug/alcohol withdrawal |
| Skin color | Pallor | Cyanosis or normal |
| Diaphoresis | Common | Rare |
| Aura or premonitory symptoms | Long | Brief |
| Convulsion | Rare, brief | Common |
| Other abnormal movements | Minor twitching | Rhythmic jerks |
| Injury | Rare | Common (with convulsive seizures) |
| Urinary incontinence | Rare | Common |
| Tongue biting | No | Can occur with convulsive seizures |
| Postictal confusion | Rare | Common |
| Postictal headache | No | Common |
| Postevent recovery | Seconds to minutes | Often delayed |
| Focal neurologic signs | No | Occasional |
| Cardiovascular signs | Common (cardiac syncope) | No |
| Abnormal findings on EEG | Rare (generalized slowing may occur during the event) | Common |
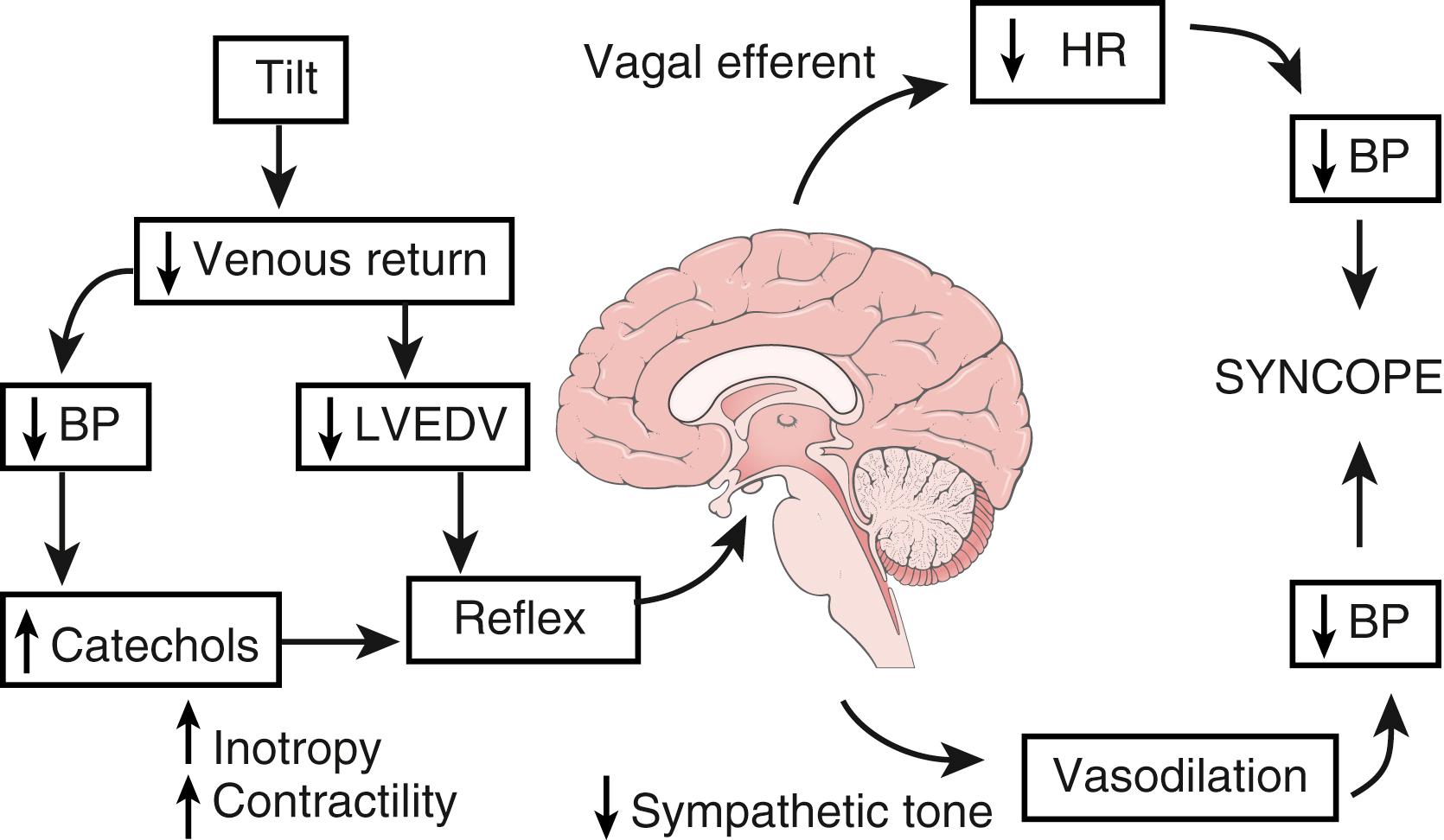
The pathophysiologic mechanism of syncope follows a common pathway with many inciting stimuli. Cerebral perfusion is compromised by a transient decrease in cardiac output as a result of vasomotor changes, decreasing venous return, primary dysrhythmia, or impairment of cerebral vascular tone. Adolescents with syncope subjected to a head-up tilt-table test reported blurred vision and constriction of visual fields before losing consciousness, as well as nausea, pallor, sweating, and dizziness, which may be accompanied by hypotension (systolic blood pressure <60 mm Hg) or bradycardia (heart rate <40 beats/min) with an occasional junctional rhythm and occasionally asystole. Symptoms are relieved rapidly by returning to the supine position. Several situational factors can exacerbate this response, including warm temperature, a confined space such as being in a crowded room, anxiety or fear, sudden surprise, the sight of blood, and pain such as from needle sticks or shots. Other situational factors include urination, swallowing, coughing, defecation, and hair combing.
This response is caused by an imbalance of parasympathetic and sympathetic tone, which results in peripheral vasodilation, including venodilation, but in no augmentation of venous return, because there is no accompanying increase in large skeletal muscle activity to augment systemic venous return and maintain cardiac filling. Subsequent vagal output results in inappropriate bradycardia and further compromises cardiac output. The child faints and becomes supine, which restores systemic venous return. Awakening is accompanied by increased sympathetic output, which restores the heart rate. The episode tends to be brief but may recur if the patient stands too quickly after the event.
In obtaining the history of a syncopal episode, attention should be paid to the time of day, time of last meal, activities leading up to the event, and associated symptoms such as palpitations, racing heartbeat, chest pain, headache, shortness of breath, nausea, diaphoresis, visual changes, and hearing changes. Cataplexy may be confused with syncope and is characterized by partial or complete paralysis of skeletal muscles resulting in a rapid progression of weakness of the face and neck followed by the muscles of the trunk and extremities. The patient loses tone and may fall to the floor but remains awake and immobile for 1–2 minutes. The patient usually senses an episode and may sit or lie down. Cataplexy is seen in patients with narcolepsy characterized by daytime sleepiness, hypnagogic hallucinations, or sleep paralysis. Triggers of cataplexy include intense positive or negative emotions, such as laughing, frustration, fright, surprise, or anger. Details of the syncopal event, such as the patient’s position (syncope while supine suggests a cardiac arrhythmia) when symptoms appeared, duration of the episode, and characterization of the patient’s appearance during and immediately after the episode, are also important. Almost without exception, by the time the patient presents to the office or emergency room, the physical examination findings are normal. Therefore, the history becomes the most important piece of information for developing the differential diagnosis, diagnostic evaluation, and management plan.
There are several causes of neurocardiogenic syncope (vasovagal); this is the dominant etiology of syncope in children and adolescents. Excessive vagal tone may be primary or secondary to breath holding, cough, deglutition syncope, micturition, defecation, carotid sinus pressure sensitivity, and orthostasis. Neurocardiogenic syncope has been described in association with hair brushing, swallowing, stretching, orthodontic maneuvers, anomalies of the cervical spine, and dental trauma. Many of these episodes may be forms of carotid sinus sensitivity. Cough syncope may be related to prolongation of high intrathoracic pressure that results in decreased venous return and subsequent decreased cardiac output.
The prodromal history is very important in evaluating neurocardiogenic syncope. Syncope without warning, while the patient is supine, or during exercise implies a primary cardiac cause and a more serious etiology; it is associated with greater morbidity and potential mortality (see Table 7.3 ).
Neurocardiogenic syncope is a type of autonomic dysfunction that is also referred to as vasodepressor syncope , vasovagal syncope , and reflex syncope . Presentations include:
Primary bradycardia, sometimes to the extreme of sinus arrest or even brief asystole, with subsequent hypotension. This is known as the cardioinhibitory response.
Primary vasodepressor response that is characterized by hypotension with the heart rate relatively preserved.
Mixed response, the most common response that features simultaneous hypotension and bradycardia.
The common pathway producing the heart rate and blood pressure responses and cerebral hypoperfusion is the Bezold-Jarisch reflex ( Fig. 7.1 ). For most children and adolescents, prodromal warning signs herald the impending syncopal episode and can, after the first episode, allow the child enough time to prevent fainting by sitting with the head between the knees or by lying supine.
The physiologic mechanisms of neurocardiogenic syncope have been demonstrated with head-up tilt-table testing. Tilt-table testing can be performed with or without invasive blood pressure monitoring. The goal is to reproduce the patient’s symptoms under close monitoring. Various tilt angles and durations have been described, as has the use of isoproterenol as a provocative stimulus.
If the history suggests the diagnosis of neurocardiogenic syncope with normal physical examination findings and a normal ECG, treatment may be empirically started.
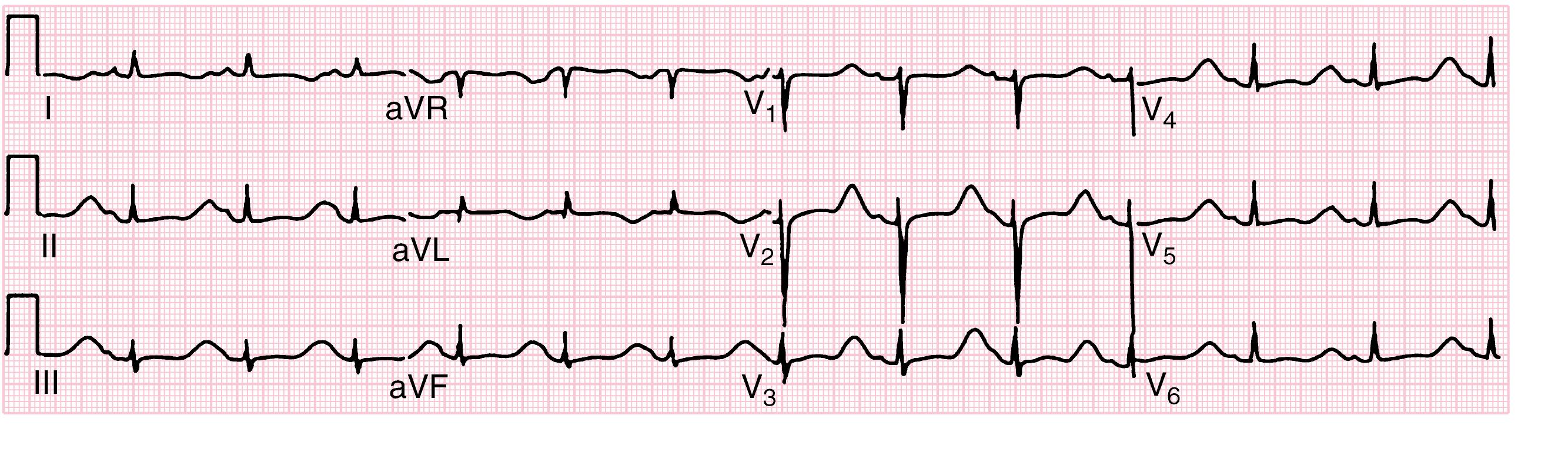
An ECG is recommended for all patients with syncope . Even when no longer symptomatic, the ECG may demonstrate characteristic features of Wolff-Parkinson-White syndrome, Brugada syndrome, long and short QT syndromes, hypertrophic cardiomyopathy, arrhythmogenic right ventricular dysplasia, and heart block.
Guidelines for the treatment of neurocardiogenic syncope are found in Table 7.6 . The first line of treatment is education and counseling. Most patients will eventually outgrow neurocardiogenic syncope. Patients should maintain hydration and increase dietary salt if there are not any contraindications. Patients should be counseled to avoid situations that precipitate an event and taught to abort an event by lying down. Physical counterpressure maneuvers are helpful when there is a prodrome (see Table 7.6 ).
RECOMMENDATIONS
|
|
|
|
|
|
|
|
|
If the patient fails conservative therapies, pharmacologic treatments may be tried. Physicians have used fludrocortisone with increased salt intake, β-adrenergic blockers, and midodrine, which has had promising results.
Conditions that produce hypotension (orthostatic or supine) frequently produce syncope or presyncope. Cardiac function and structure are usually normal before the episode; during the predisposing illness, cardiac filling pressures are often reduced because of reduced venous return from hypovolemia or decreased peripheral vascular resistance (peripheral pooling of blood). Dehydration from diarrhea and vomiting, hyperthermia, hyperpyrexia, heat exhaustion, polyuria (diabetes mellitus), or poor intake from anorexia, together with the systemic effects of the primary illness, may produce orthostatic or true hypotension and syncope. In these conditions, dizziness, hypotension, or syncope occurs rapidly when the patient assumes an upright position. Prolonged bed rest, combined with poor fluid intake during an illness, may also result in syncope or presyncope when the child arises to leave the bed. In most of these situations, fluid administration is sufficient to restore intravascular volume and venous return to alleviate postural or supine hypotension.
Postural orthostatic tachycardia syndrome (POTS) is characterized by recurrent (often daily) and long-standing symptoms of orthostatic intolerance, exercise intolerance, lightheadedness, fatigue, sweating, headache, chest tightness, brain fog, palpitations, anxiety, tremor, and presyncope when upright. The syndrome may be secondary to autonomic dysfunction. Symptoms are improved with lying down. Criteria to diagnose POTS include symptoms that have lasted >6 months; heart rate that increases by at least 40 beats/min or a maximum rate of 130 if younger than 18 years or 30 beats/min or a maximum rate of >125 if older than 18 years after assuming a standing from supine position for at least 10 minutes; symptoms worsen with standing and improve with recumbence; and the absence of other overt causes of orthostatic intolerance.
Several different pathophysiologic mechanisms have been described in patients with POTS, including:
Peripheral autonomic denervation (neuropathic) leading to reduced venoconstriction and venous pooling with secondary tachycardia
Hypovolemia
Hyperadrenergic POTS associated with elevated systolic blood pressure and increased norepinephrine levels after standing for 10 minutes
Poor exercise tolerance
POTS associated with other diseases including autoimmunity
A detailed history of orthostatic intolerance may identify symptoms of headache, fatigue, sleep disorder, weakness, hyperventilation, shaking, sweating, anxiety, dizziness, and presyncope. An evaluation for POTS may include a CBC, glucose, electrolytes, and thyroid function. Cardiac evaluation should include an ECG. A tilt-table test is helpful to demonstrate the effects of orthostatic stress (increased heart rate).
There is no specific treatment for POTS. Medications that may aggravate symptoms of POTS should be avoided, including antihypertensive agents, sedatives, and many other psychiatric medications. Patients should avoid aggravating factors, such as dehydration, extreme heat, and alcohol. Nonpharmacologic treatment includes aerobic exercise, compressive stockings, and increased fluid and salt intake. Pharmacologic treatment should be tailored to the variant the patient exhibits ( Table 7.7 ).
|
|
|
|
|
|
|
|
|
|
Inappropriate sinus tachycardia (IST) presents with palpitations, fatigue, dizziness, and near syncope. It may be initially confused with POTS. In IST, the heart rate is elevated at rest (>100 beats/min) when supine and increases further with exercise. The mean 24-hour heart rate is >90 beats/min. The differential diagnosis includes hyperthyroidism and pheochromocytoma. Treatment is difficult, but ivabradine with or without metoprolol may be effective.
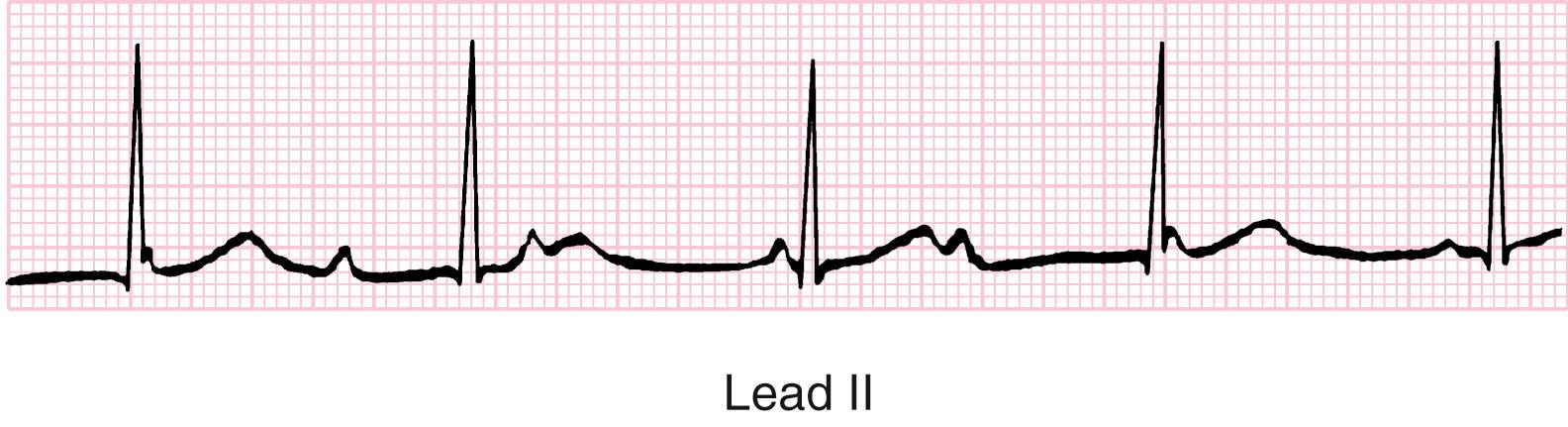
A variety of cardiac conditions can result in hypotension and syncope ( Tables 7.8, 7.9 , and 7.10 ; see Table 7.3 ). Dysrhythmias are common and are usually silent between episodes (see Table 7.8 ). Supraventricular tachycardia, ventricular tachycardia, and heart block are the most common types of dysrhythmia and may be primary or result from medications or illicit drugs. Any form of acquired heart block carries a high mortality rate ( Fig. 7.2 ). A common cause of acquired heart block is Lyme disease. Heart block may necessitate temporary or permanent electronic pacing to maintain cardiac output.
| Primary Electrical Abnormalities | Features | ECG | Treatment |
|---|---|---|---|
| LQTS: Romano-Ward, Jervell–Lange-Nielsen, acquired | Familial genetic disorder Ion channel variant Presents in torsades de pointes Romano-Ward is MC inherited LQTS Jervell–Lange-Nielsen has congenital deafness |
Prolonged QT measured from the onset of the Q wave to the end of the T wave in lead II Varies with HR but >0.44 in men, >0.46 in children and women for HR 50–90 beats/min is prolonged Torsades de pointes can occur Can deteriorate from polymorphic ventricular tachycardia to ventricular fibrillation |
β Blocker therapy Recommendations on exercise intensity by a cardiologist ICD if β blockers fail |
| Brugada syndrome | Inherited autosomal dominant arrhythmogenic syndrome characterized by life-threatening ventricular arrhythmias Genetic variant in SCN5A and 13 other genes |
ECG abnormalities are from repolarization and depolarization abnormalities Coved-type ST segment elevations in the right precordial leads J wave amplitude ≥2 mm followed by a negative T wave |
Placement of ICD |
| Wolff-Parkinson-White | Owing to one or more re-entrant pathways inducing SVT or atrial fibrillation Up to 14% associated with malignant tachycardias Malignant arrhythmias from short re-entrant pathway repolarization or multiple pathways |
Short PR interval Delta waves present |
Undergo EPT and ablation |
| Dilated cardiomyopathy: ventricular tachycardia/fibrillation | Cardiac dilation and systolic dysfunction Inherited or acquired Lamin AC gene variant a common cause of DCM and SCD |
Marked LVH Poor R wave progression Left atrial enlargement Right axis deviation |
Permanent pacemaker and ICD placement |
| Catecholamine-exercise: ventricular tachycardia | Ventricular ectopy induced by exercise or emotional stress Variant in gene that encodes Ca-mediated sarcoplasmic fibers Lethal in 30–50% if left untreated |
Pre-exercise ECG is usually normal, stress testing recommended ECG with exercise Nonsustained wide ventricular tachycardia |
β Blocker therapy Recommendations on exercise intensity by a cardiologist ICD if β blockers fail |
| SIDS and SIDS “Mimics” |
|
| Corrected or Unoperated Congenital Heart Disease |
|
| Coronary Arterial Disease |
|
| Myocardial Disease |
|
| Conduction System Abnormality/Arrhythmia |
|
| Miscellaneous |
|
| Gene | Locus | Protein |
|---|---|---|
| Long QT Syndrome (LQTS) | ||
| Major LQTS Genes | ||
| KCNQ1 (LQT1) | 11p15.5 | I Ks potassium channel α subunit (KVLQT1, K v 7.1) |
| KCNH2 (LQT2) | 7q35-36 | I Kr potassium channel α subunit (HERG, K v 11.1) |
| SCN5A (LQT3) | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
| Minor LQTS Genes (listed alphabetically) | ||
| AKAP9 | 7q21-q22 | Yotiao |
| CACNA1C | 12p13.3 | Voltage-gated L-type calcium channel (Ca v 1.2) |
| CALM1 | 14q32.11 | Calmodulin 1 |
| CALM2 | 2p21 | Calmodulin 2 |
| CALM3 | 19q13.2-q13.3 | Calmodulin 3 |
| CAV3 | 3p25 | Caveolin-3 |
| KCNE1 | 21q22.1 | Potassium channel β subunit (MinK) |
| KCNE2 | 21q22.1 | Potassium channel β subunit (MiRP1) |
| KCNJ5 | 11q24.3 | Kir3.4 subunit of I KACH channel |
| SCN4B | 11q23.3 | Sodium channel β 4 subunit |
| SNTA1 | 20q11.2 | Syntrophin-α 1 |
| Triadin Knockout (TKO) Syndrome | ||
| TRDN | 6q22.31 | Cardiac triadin |
| Andersen-Tawil Syndrome (ATS) | ||
| KCNJ2 (ATS1) | 17q23 | I K1 potassium channel (Kir2.1) |
| Timothy Syndrome (TS) | ||
| CACNA1C | 12p13.3 | Voltage-gated L-type calcium channel (Ca v 1.2) |
| Cardiac-Only Timothy Syndrome (COTS) | ||
| CACNA1C | 12p13.3 | Voltage-gated L-type calcium channel (Ca v 1.2) |
| Short QT Syndrome (SQTS) | ||
| KCNH2 (SQT1) | 7q35-36 | I Kr potassium channel α subunit (HERG, K v 11.1) |
| KCNQ1 (SQT2) | 11p15.5 | I Ks potassium channel α subunit (KVLQT1, K v 7.1) |
| KCNJ2 (SQT3) | 17q23 | I K1 potassium channel (Kir2.1) |
| CACNA1C (SQT4) | 12p13.3 | Voltage-gated L-type calcium channel (Ca v 1.2) |
| CACNB2 (SQT5) | 10p12 | Voltage-gated L-type calcium channel β 2 subunit |
| CACN2D1 (SQT6) | 7q21-q22 | Voltage-gated L-type calcium channel 2 δ 1 subunit |
| Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) | ||
| RYR2 (CPVT1) | 1q42.1-q43 | Ryanodine receptor 2 |
| CASQ2 (CPVT2) | 1p13.3 | Calsequestrin 2 |
| KCNJ2 (CPVT3) | 17q23 | I K1 potassium channel (Kir2.1) |
| CALM1 | 14q32.11 | Calmodulin 1 |
| CALM3 | 19q13.2-q13.3 | Calmodulin 3 |
| TRDN | 6q22.31 | Cardiac triadin |
| Brugada Syndrome (BrS) | ||
| SCN5A (BrS1) | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
| Minor BrS Genes (listed alphabetically) | ||
| ABCC9 | 12p12.1 | ATP-binding cassette, subfamily C member 9 |
| CACNA1C | 2p13.3 | Voltage-gated L-type calcium channel (Ca v 1.2) |
| CACNA2D1 | 7q21-q22 | Voltage-gated L-type calcium channel 2 δ 1 subunit |
| CACNB2 | 10p12 | Voltage-gated L-type calcium channel β 2 subunit |
| FGF12 | 3q28 | Fibroblast growth factor 12 |
| GPD1L | 3p22.3 | Glycerol-3-phosphate dehydrogenase 1–like |
| KCND3 | 1p13.2 | Voltage-gated potassium channel (I to ) subunit K v 4.3 |
| KCNE3 | 11q13.4 | Potassium channel β 3 subunit (MiRP2) |
| KCNJ8 | 12p12.1 | Inward rectifier K + channel Kir6.1 |
| HEY2 | 6q | Hes-related family BHLH transcription factor with YRPW motif 2 |
| PKP2 | 12p11 | Plakophilin-2 |
| RANGRF | 17p13.1 | RAN guanine nucleotide release factor 1 |
| SCN1B | 19q13 | Sodium channel β 1 |
| SCN2B | 11q23 | Sodium channel β 2 |
| SCN3B | 11q24.1 | Sodium channel β 3 |
| SCN10A | 3p22.2 | Sodium voltage-gated channel α 10 subunit (Na v 1.8) |
| SLMAP | 3p14.3 | Sarcolemma-associated protein |
| Early Repolarization Syndrome (ERS) | ||
| ABCC9 | 12p12.1 | ATP-binding cassette, subfamily C member 9 |
| CACNA1C | 2p13.3 | Voltage-gated L-type calcium channel (Ca v 1.2) |
| CACNA2D1 | 7q21-q22 | Voltage-gated L-type calcium channel 2 δ 1 subunit |
| CACNB2 | 10p12 | Voltage-gated L-type calcium channel β 2 subunit |
| KCNJ8 | 12p12.1 | Inward rectifier K + channel Kir6.1 |
| SCN5A | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
| SCN10A | 3p22.2 | Sodium voltage-gated channel α 10 subunit (Na v 1.8) |
| Idiopathic Ventricular Fibrillation (IVF) | ||
| ANK2 | 4q25-q27 | Ankyrin B |
| CALM1 | 14q32.11 | Calmodulin 1 |
| DPP6 | 7q36 | Dipeptidyl-peptidase-6 |
| KCNJ8 | 12p12.1 | Inward rectifier K + channel Kir6.1 |
| RYR2 | 1q42.1-q43 | Ryanodine receptor 2 |
| SCN3B | 11q23 | Sodium channel β 3 subunit |
| SCN5A | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
| Progressive Cardiac Conduction Disease/Defect (PCCD) | ||
| SCN5A | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
| TRPM4 | 19q13.33 | Transient receptor potential cation channel, subfamily M, member 4 |
| Sick Sinus Syndrome (SSS) | ||
| ANK2 | 4q25-q27 | Ankyrin B |
| HCN4 | 15q24-q25 | Hyperpolarization-activated cyclic nucleotide–gated channel 4 |
| MYH6 | 14q11.2 | Myosin, heavy chain 6, cardiac muscle, α |
| SCN5A | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
| “Ankyrin-B Syndrome” | ||
| ANK2 | 4q25-q27 | Ankyrin B |
| Familial Atrial Fibrillation (FAF) | ||
| ANK2 | 4q25-q27 | Ankyrin B |
| GATA4 | 8p23.1-p22 | GATA-binding protein 4 |
| GATA5 | 20q13.33 | GATA-binding protein 5 |
| GJA5 | 1q21 | Connexin 40 |
| KCNA5 | 12p13 | I Kur potassium channel (K v 1.5) |
| KCNE2 | 21q22.1 | Potassium channel β subunit (MiRP1) |
| KCNH2 | 7q35-36 | I Kr potassium channel α subunit (HERG, K v 11.1) |
| KCNJ2 | 17q23 | I K1 potassium channel (Kir2.1) |
| KCNQ1 | 11p15.5 | I Ks potassium channel α subunit (KVLQT1, K v 7.1) |
| NPPA | 1p36 | Atrial natriuretic peptide precursor A |
| NUP155 | 5p13 | Nucleoporin 155 KD |
| SCN5A | 3p21-p24 | Cardiac sodium channel α subunit (Na v 1.5) |
Primary cardiac conduction abnormalities that may result in syncope include Wolff-Parkinson-White syndrome, long QT syndromes, and catecholamine-sensitive ventricular tachycardia. Wolff-Parkinson-White syndrome is characterized by a short PR interva l, pre-excitation seen as a widened QRS duration, and a delta wave on the proximal portion of the QRS. The delta wave represents the presence of accessory electrical tissue from atria to ventricle, with rapid antegrade conduction causing excitation of ventricular tissue before atrioventricular node–His bundle stimulation. If that pathway can conduct in the retrograde manner, a re-entrant circuit is created, causing a narrow QRS complex tachycardia. This greatly shortens the diastolic ventricular filling time and results in diminished left ventricular end-diastolic volume, with subsequently decreased stroke volume and decreased cardiac output. Although the tachycardia is rarely sufficiently fast to result in syncope, some children have profound hypotension and a rapid loss of consciousness. In adults, a similar mechanism results from atrial flutter or fibrillation if the ventricular response rate is fast.
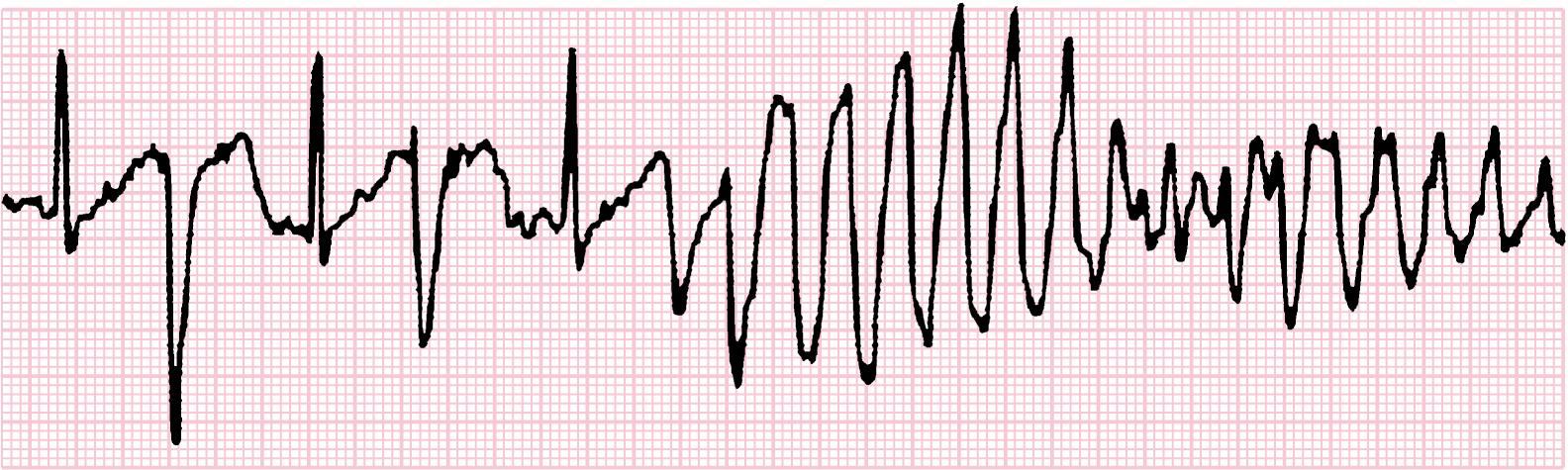
Long QT syndromes are inherited (usually autosomal dominant) or acquired abnormalities in the electrical recovery (repolarization) of the heart ( Fig. 7.3 ). Prolongation of the repolarization phase results in the risk of simultaneous depolarization, the “R-on-T” phenomenon, which causes disorganized ventricular electrical stimulation characterized by torsades de pointes (coarse ventricular tachycardia), a potentially lethal dysrhythmia ( Fig. 7.4 ). There may be a family history of sudden cardiac death. Family studies with the same gene variant have demonstrated that affected patients may not always have a long QT interval on ECG as defined for the syndrome, but an increased QT interval may become evident with exercise or during catecholamine infusion. Long QT syndromes may be responsible for some cases of sudden infant death syndrome and drowning. Although additional genetic forms have been described, most gene variants for prolonged QT involve either a potassium or sodium ion channel (see Table 7.10 ). There is some genotype-phenotype correlation in LQT genes: LQT1 events are frequently associated with stress, exercise, emotion, or swimming; LQT2 events are associated with auditory triggers (alarm clocks); while LQT3 events may be associated with sleep. Long QT syndromes may present as a syncopal episode, seizures, palpitations, or presyncope. Diagnosing long QT syndromes is based on clinical history and ECG findings of a prolonged rate-corrected QT interval. Genetic testing may identify approximately 75% of patients. Acquired prolongation of the QT interval is seen in electrolyte abnormalities (hyperkalemia) and with a variety of medications ( Table 7.11 ). A drug history and toxicology screen may be warranted if there is any question of QT prolongation.
| Drugs Commonly Involved | Other Drugs |
|---|---|
| Disopyramide | Amiodarone |
| Dofetilide | Arsenic trioxide |
| Ibutilide | Cisapride |
| Procainamide Quinidine Sotalol Bepridil |
Calcium channel blockers: lidoflazine (not marketed in the United States) |
| Anti-infective agents: clarithromycin, erythromycin, halofantrine, pentamidine, quinoline-class antibiotics, hydroxychloroquine | |
| Antiemetic agents: domperidone, droperidol | |
| Antipsychotic agents: chlorpromazine, haloperidol, mesoridazine, thioridazine, pimozide | |
| Methadone |
Patients who have undergone corrective or palliative surgery for congenital cardiac disease are at risk for both early- and late-onset dysrhythmias that might result in syncope. Sinus node disease (in patients undergoing atrial surgery) may result in tachycardia-bradycardia episodes that can be associated with hypotension. Ventricular dysrhythmias are particularly common after repair of tetralogy of Fallot, double-outlet right ventricle, truncus arteriosus, and pulmonary atresia involving right ventriculotomy with subsequent ventricular scar formation.
Uncorrected structural heart disease is a relatively rare cause of a sudden decrease in cardiac output. However, hypertrophic cardiomyopathies can result in obstruction of left ventricular outflow with resultant high transmural pressure and secondary cardiac ischemia, which can be fatal. This type of obstruction is exacerbated by high sympathetic tone, causing increased contractility, and is a frequent mechanism of syncope associated with exercise in competitive athletes. The presence of an outflow tract murmur in the setting of syncope, especially if there is a positive family history, warrants evaluation with both electrocardiography and echocardiography. Any condition that impedes left ventricular outflow (valvular aortic stenosis or subaortic stenosis), left ventricular inflow or filling (mitral stenosis or pericardial tamponade), or blood flow through the pulmonary vasculature (primary or secondary pulmonary hypertension) may result in syncope. In almost all cases, characteristic physical findings lead the clinician to the diagnosis. Pulmonary hypertension may be associated with cyanosis, in which case there is cerebral hypoxia resulting from right-to-left shunting, as well as decreased left ventricular output resulting from poor transpulmonary flow and decreased left ventricular filling.
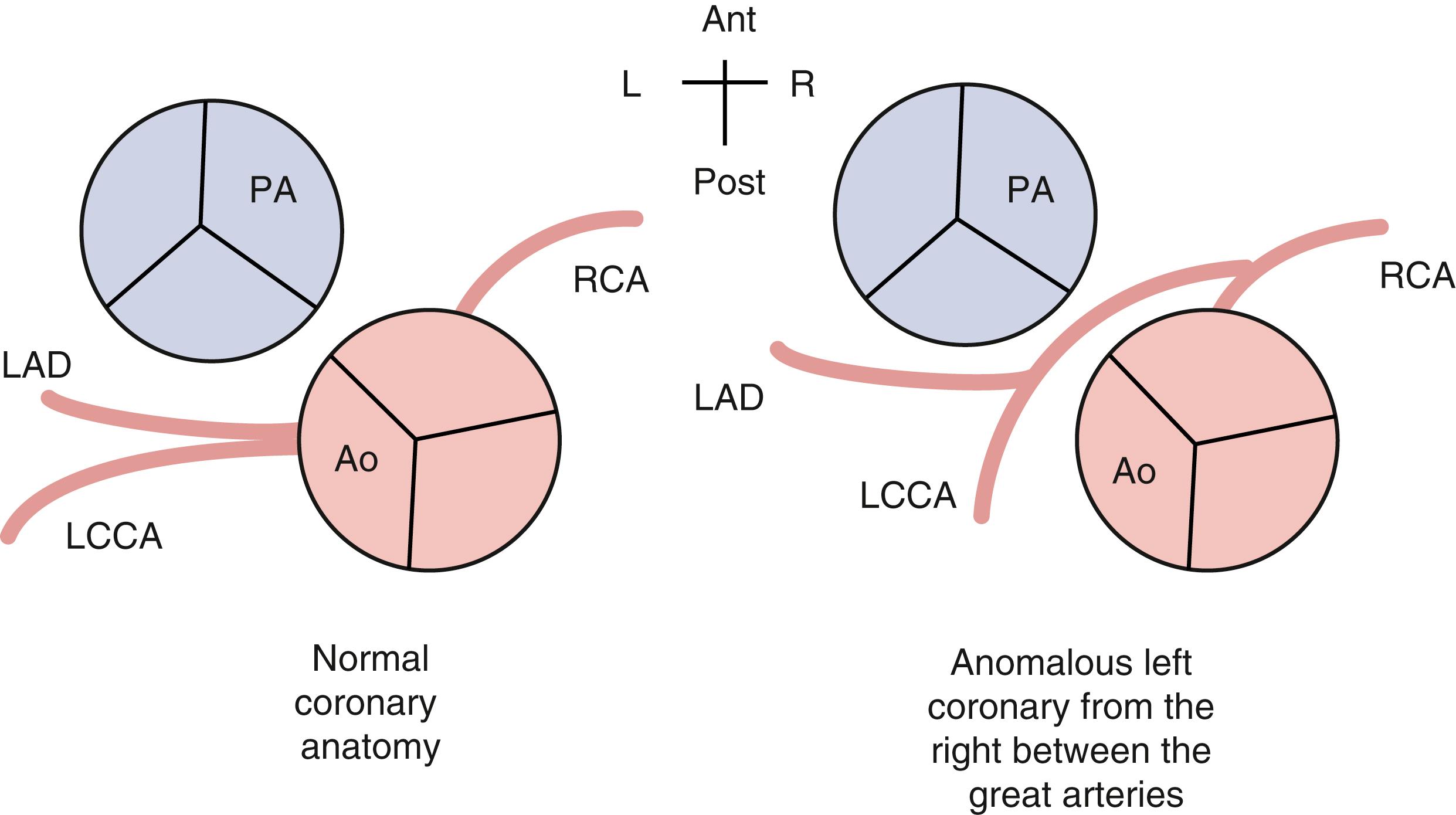
Other rare causes of cardiac syncope are thoracic masses and intracardiac tumors or masses, coronary artery abnormalities, and inflammatory cardiac diseases (myocarditis). Masses or tumors, such as myxomas, fibromas, and rhabdomyomas, tend to produce paroxysmal symptoms, which are often associated with position changes, especially from the recumbent position. Coronary artery anomalies are usually not accompanied by signs of ischemia. Rather, the most common manifestation is syncope or sudden cardiac death from compression of the anomalous left main coronary artery as it courses between the pulmonary outflow and the aortic root ( Fig. 7.5 ). This usually occurs in a competitive athlete whose hypertrophied heart responds to catecholamine stimulation during activity and inadvertently compresses the anomalous coronary artery. Inflammatory conditions, such as heart block associated with Lyme disease and ventricular tachycardia associated with myocarditis or pericarditis, predispose to dysrhythmias.
Cardiac syncopal episodes can be accompanied by brief tonic-clonic seizure activity known as Stokes-Adams syndrome . The seizure activity appears 10–20 seconds after the onset of asystole and is usually of short duration with no subsequent postictal phase. Many children with cardiac syncope are initially referred to a neurologist.
Sudden cardiac death is discussed with cardiac causes of syncope because cardiac causes of syncope may also produce sudden death (see Table 7.3 ). Sudden cardiac arrest or death is defined as the abrupt and unexpected loss of heart function. Structural causes include valvular aortic stenosis, coronary artery anomalies, cardiomyopathies, and myocarditis. Cardiac arrhythmias associated with sudden death include Wolff-Parkinson-White syndrome and prolonged QT syndrome. A less common cause is commotio cordis resulting from nonpenetrating blunt trauma to the chest. Warning events or symptoms may not always be evident prior to sudden cardiac death; if it presents, patients may complain of episodes of dizziness, lightheadedness, presyncope, syncope, dyspnea, or palpitations. Other relevant history may include fatigue, unexplained seizure, or chest pain. It is important for the physician to perform a detailed history and physical examination to look for warning signs of cardiovascular disease in the patient and family ( Table 7.12 ). Key elements of the physical examination should include measurement of blood pressure and a complete cardiovascular exam with attention to heart rate, rhythm, murmurs, pulses, and features of possible hereditary disorders with recognizable phenotypes such as Marfan syndrome.
| Patient History Questions: |
| Tell Me About Any of These in Your Child … Yes or No |
|
| Family History Questions: |
| Tell Me About Any of These in Your Family… |
|
| Please Explain More About Any “Yes” Answers. |
∗ Ask these questions (or have parents complete for your review) at periodic times during well-child visits (neonatal, preschool, before or during middle school, and before or during high school).
Predictors of a cardiac etiology of syncope versus a more benign etiology such as neurocardiogenic syncope include:
Syncope associated with activity or while sitting or supine
Family history of cardiac disease or sudden/unexplained cardiac death
Physical examination consistent with cardiac disease
Abnormal ECG
Palpitations
Primary neurologic causes of syncope are more unusual in otherwise healthy children and adolescents than in adults. Seizures must be considered if there is a history of an aural prodrome, focal or generalized tonic-clonic activity, and a prolonged postictal phase of lethargy or confusion (see Tables 7.4 and 7.5 ). Prolonged postevent lethargy is unusual with more common causes of syncope if the vital signs have returned to normal. Seizures are a common cause of loss of consciousness in the recumbent patient. Seizures are often accompanied by tachycardia and normal or elevated blood pressure. A premonitory aura may herald vertebrobasilar vascular spasm, which appears to occur when syncope is with basilar type migraines . There may be a history of unilateral visual changes; the loss of consciousness usually has a somewhat longer onset and duration. The patient frequently complains of headache after regaining consciousness. Basilar type migraine or migraine affecting the vertebrobasilar circulation can cause dizziness, vertigo, ataxia, confusion, and headache. There is often a positive family history of migraines.
Hypoglycemia should always be included as a cause of syncope, but it is rare in children and adolescents except in patients with insulin-dependent diabetes or inborn errors of glucose, glycogen, fatty acid metabolism, or adrenal insufficiency (see Chapter 57 ). With hypoglycemia, the patient feels weak, hungry, sweaty, agitated, and confused and eventually experiences altered mental status. Onset is gradual, and the patient remains hemodynamically stable, although tachycardia may be evident. Ingestion of oral hypoglycemic agents may exceed the body’s normal glucose homeostasis, resulting in hypoglycemia.
Reflex asystolic syncope, also known as “pallid breath-holding spells,” is often initiated in a toddler-aged child with a minor stimulus (bump to the head). This is not true breath holding; the child becomes pale, loses tone, and may have asystole and on awakening red color returns to the child’s face. This may be an early predictor of vasovagal syncope in an older child.
Cyanotic breath-holding spells are triggered by pain or frustration in a toddler-aged infant. The child experiences a prolonged expiratory apnea and loses tone. Treatment is reassurance and iron supplementation if the serum ferritin level is low.
Infant hyperekplexia manifests with hypertonia, apnea, exaggerated startle response to unexpected stimuli (noise), and poststartle rigidity. Associated gene variants include GLRA1 , SLC6A5 , GLRB , GPHN , and ARHGEF9 (X-linked). Most are autosomal dominant, but autosomal recessive and X-linked inheritance is possible. Treatment includes clonazepam and placing the patient in a curled-up position during an episode.
Paroxysmal extreme pain disorder may manifest in the neonate and infant and is often triggered by defecation or by changes in temperature, emotional distress, eating spicy foods, or drinking cold fluids in an older child (see Chapter 39 ). The manifestations include flushing (occasionally Harlequin change), apnea, stiffening, and paroxysmal localized pain (jaw, perianal area). Gene variants in SCN9A cause this autosomal dominant disorder. The differential diagnosis includes erythromelalgia and hyperekplexia. Carbamazepine has been one effective medication to manage the neuropathic pain.
Patients with a history of panic attacks may become syncopal secondary to hyperventilation. The mechanism is not completely understood but may involve the reaction of cerebral blood flow in response to hypocapnia and respiratory alkalosis. Tetany or paresthesias may be present in some patients. The history of the episode is critical, and witnesses are especially helpful. The patient frequently relates a feeling of suffocation, smothering, shortness of breath, or chest tightness. In retrospect, the patient may also admit to numbness and tingling of the extremities and visual changes. Hyperventilation and hypocapnia may be detected during a tilt-table test by measuring end-tidal co 2 .
A psychiatric cause of syncope (pseudosyncope) is a diagnosis of exclusion. The patient is usually an adolescent and frequently has episodes in the presence of others. The patient is unusually calm in describing the episodes and relates details that may indicate no loss of consciousness. During the episode, there are no associated hemodynamic changes and no pallor, sweating, or respiratory changes. Typically, the patient falls without injury. The key is to define what secondary gain the patient attains through the disorder.
The history of the event is the critical information for most patients (see Table 7.4 ). A detailed account of what the patient felt immediately before losing consciousness, what the patient was doing, what the posture or position was, how the patient looked, how long the episode lasted, and associated signs or symptoms direct the diagnostic work-up. A thorough and detailed family history is necessary to discover risk for sudden death, dysrhythmia, heart disease, seizures, and metabolic disorders. The medication history, including over-the-counter, prescribed, and illicit drugs, as well as any accessible medication of other family members should be gathered.
Any person who has a syncopal episode should undergo a thorough physical examination, with special attention to the cardiovascular and neurologic systems. The examination should include obtaining vital signs with the patient supine and after standing for 5–10 minutes. Upon careful auscultation, the presence of an outflow tract murmur radiating to the neck, an abnormally loud second heart sound, or the presence of a long decrescendo diastolic murmur at the apex leads to more involved diagnostic testing. A complete neurologic exam should be performed. In most cases, patients with a history of syncope have normal physical findings at the time of the examination.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here