Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cavernous malformations (CMs) have long been recognized as one of the major clinicopathologic categories of vascular malformations of the nervous system. CMs have been included in the descriptions of cryptic or occult vascular malformations , a term that has been used to describe any vascular malformation that cannot be seen on angiography. The term cavernous angioma was used by Russell and Rubinstein in their description of the pathology of these lesions. CMs have also been called cavernous hemangiomas or cavernomas , but the term cavernous malformation has become more widely accepted, explicitly distinguishing these lesions from true vascular neoplasms as suggested by the term angioma.
Before computed tomography (CT), the diagnosis of CMs was rarely made before operation or autopsy. CT suggested the diagnosis in some patients; however, when high-field magnetic resonance imaging (MRI) became available, a picture characteristic of CMs was defined, allowing the diagnosis to be established in many cases. Furthermore, the advances in imaging not only have improved diagnosis of symptomatic lesions but also have resulted in increasing reports of incidental CMs.
The management of patients with CMs usually includes a consideration of surgical treatment or of observation. Rarely, radiosurgery is considered, but high complication rates and poor definition of end points for therapy have discouraged the use of this technique. With emerging knowledge of the natural history of CMs, the indications and guidelines for management decisions continue to evolve. This chapter reviews the surgical management of 121 cases of CMs at the Massachusetts General Hospital (MGH). From this information and from a review of the literature, recommendations are made for treating patients with this disorder.
CMs can occur throughout the brain or spinal cord parenchyma, as well as on cranial and spinal nerves. , The lesions, which may be multiple, can range in size from a few millimeters to several centimeters. Often, an associated venous malformation of the brain may be present; rarely, similar lesions may be found in other parts of the body. ,
The molecular and cellular processes involved in CM development are not clear. In some patients, the lesions are clearly acquired, appearing in areas of the brain that were normal on prior MRI studies. These include patients with familial lesions and those in whom the CM has developed in an area of previously irradiated brain tissue or has even developed sporadically. Wilson has proposed a possible pathogenesis for the development of acquired lesions.
The lesion is well defined and usually has a lobulated appearance. There is often a characteristic gross appearance that has been likened to a mulberry, dark red or purple in color. Inside the lesion is a honeycomb of thin-walled vascular spaces. Small hemorrhages adjacent to or within the lesion may occur, but large hemorrhages are rare. A variable number of small blood vessels enter the lesion. Gliotic tissue surrounds the mass, yellow in color due to hemosiderin staining resulting from hemoglobin degradation. In some patients, the lesion may gradually enlarge as a result of small hemorrhages, progressive hyalinization, thickening of the vascular walls, or gradual thrombosis. ,
Irregular sinusoidal spaces are visible on microscopic examination and many contain areas of thrombosis and organization with thin walls devoid of elastic tissue and muscle. These walls consist of a single layer of endothelium with varying amounts of extraluminal connective tissue. No intervening or neural tissue is present except that at the periphery, which is a layer of gliotic tissue that contains hemosiderin-packed macrophages adjacent to the lesion. Small hematomas of varying ages may also be seen with extensive calcification, as well as collections of capillaries on the surface of the lesion.
High-quality CT scans suggest the diagnosis of CM in some patients. The characteristic findings are a roughly circular or irregularly shaped lesion located in the brain parenchyma; this lesion shows high density on the noncontrast scan and slight or no contrast enhancement. In some patients, extensive calcification is noted. Other types of occult vascular malformations, and some tumors associated with hemorrhage, also have the same CT appearance.
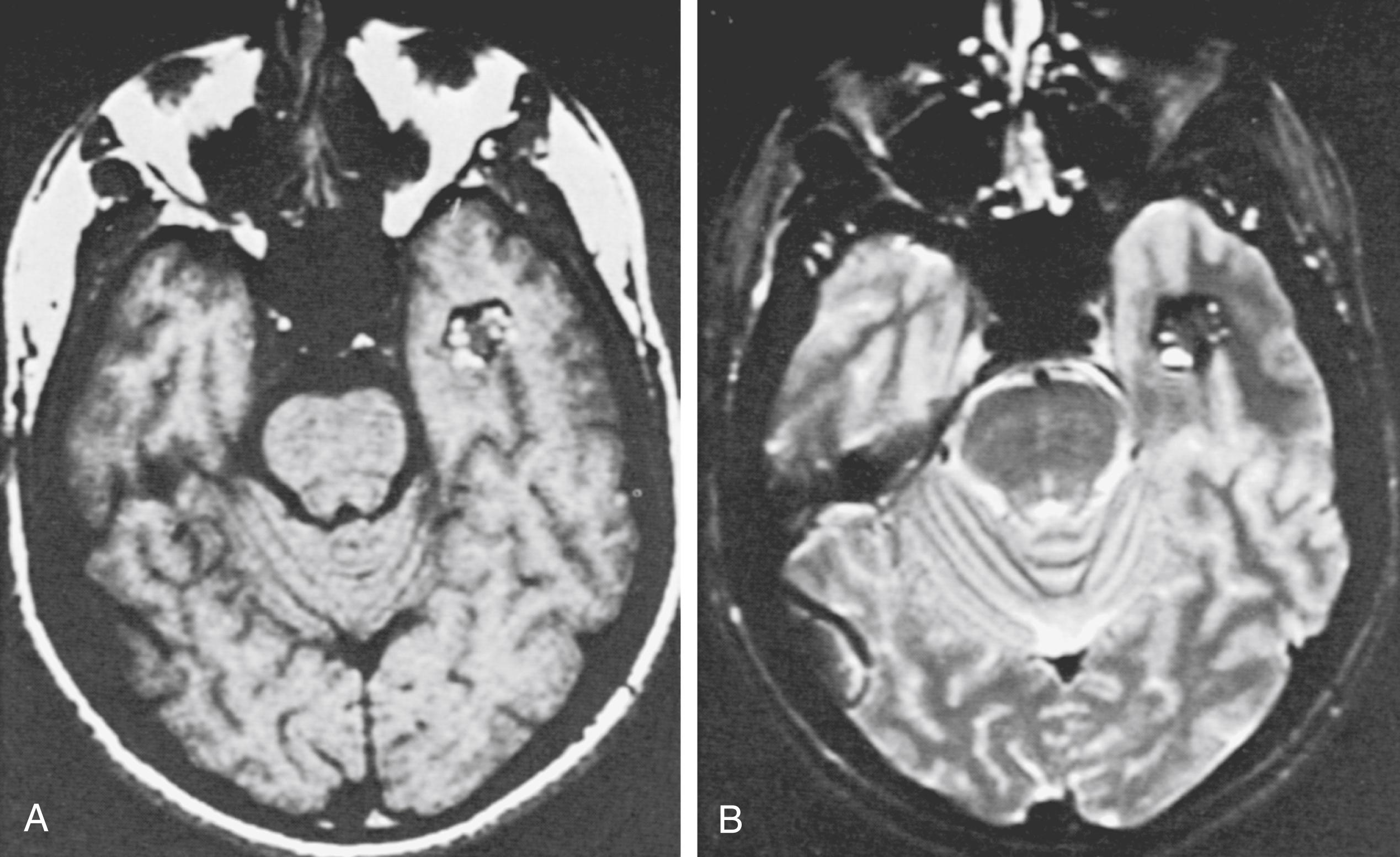
MRI accurately establishes the diagnosis in most cases and often is the only study needed. The criteria for MRI diagnosis is a well-circumscribed lesion with a combination of a reticulated or mottled core of mixed signal intensity and a prominent surrounding rim of decreased signal intensity ( Fig. 55.1 ). Hemorrhages of different ages may be seen within or around the lesion, causing a T2 hypointense “hemosiderin ring,” and an associated venous anomaly may be seen. T2 hyperintensity may be present beyond the “hemosiderin ring” in the adjacent brain as a result of edema. Usually little or no enhancement follows the administration of gadolinium. Although appearance on MRI has a high correlation with the diagnosis of CM, occasionally an occult arteriovenous malformation or a tumor can have a similar appearance. , , Significant enhancement suggests the possibility of a tumor. Advances in MRI techniques have resulted in the use of susceptibility-weighted imaging as the gold standard for diagnosis of CMs. Head-to-head comparisons of susceptibility weighted imaging (SWI) against T2 gradient echo and other T2-weighted sequences have shown a significantly higher sensitivity for relatively small lesions that would have classically been considered occult. This is particularly relevant in familial cases where multiple CMs are present and for locating otherwise-cryptogenic seizure foci in these patients.
The angiographic results are almost always normal because the lesion has small blood vessels with low flow and no hypertrophied feeding arteries or early draining veins. Rarely, an avascular mass or capillary blush can be identified. , Since the development of MRI, angiography is rarely indicated. Occasionally, angiography is needed to obtain information regarding the vascular anatomy to help plan a surgical approach. If the MRI scan suggests an association with another vascular malformation, or if the diagnosis is in doubt, angiography should be done.
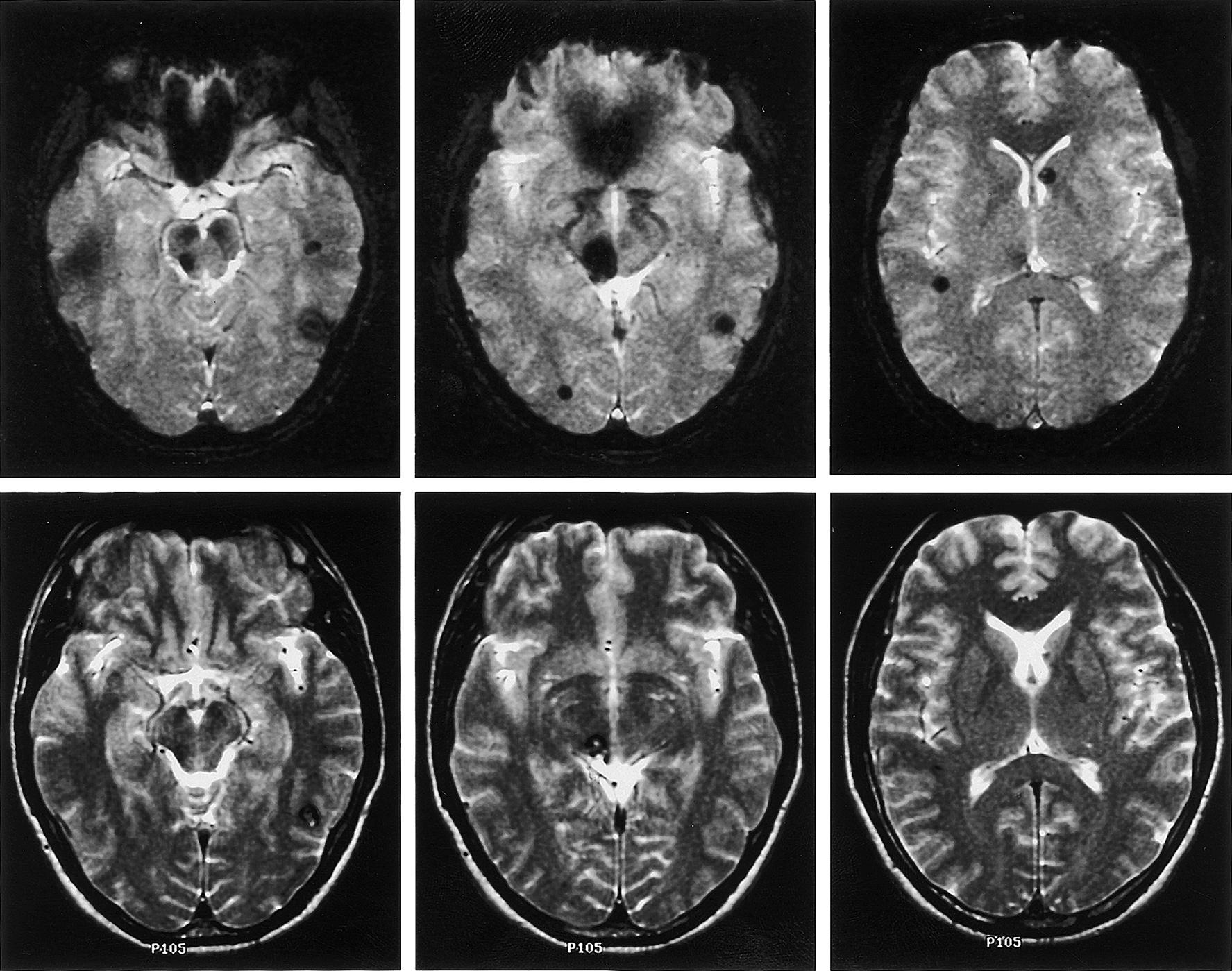
CMs are known to be present in both sporadic and familial forms. , , The familial form of the disease affects up to 30% to 50% of patients harboring a CM , and seems most common among Hispanic Americans. Studies have shown that familial CMs are more prevalent than previously believed, and there is a greater incidence of multiple lesions ( Fig. 55.2 ). Rigamonti et al. estimated a 73% familial incidence of multiple CMs of the brain, compared with a 10% to 15% incidence in the sporadic form. Further reports have indicated that familial CMs can be found in diverse ethnic groups, including the Japanese and French. , Familial and sporadic forms of the disease appear to be similar clinically ; however, as many as 75% of patients who present with multiple CMs likely harbor the hereditary form of the disease.
An autosomal dominant pattern of inheritance with variable penetrance was first described in a 122-member Hispanic lineage, of whom 5 harbored symptomatic lesions. This autosomal pattern of inheritance was confirmed by a subsequent description of six unrelated Hispanic families. Subsequent study of other families utilizing MRI to detect silent lesions revealed a more complete expression than previously suspected. The location of the responsible gene was mapped to the long arm of chromosome 7, to a locus named cerebral cavernous malformation 1 (CCM1). , CCM1 locus homogeneity was identified in an analysis of 14 Hispanic families with CMs but did not extend to kindreds of different ethnicity. Investigation of 20 non-Hispanic Caucasian families revealed linkage to two additional loci: CCM2 at chromosome 7p and CCM3 at chromosome 3q. The clinical, radiographic, and pathologic characteristics of the disease in kindreds mapping to these other loci does not appear to differ from those seen in kindreds mapping to the CCM1 locus. Linkage to one of these three loci (i.e., 7q, 7p, or 3q) accounted for inheritance in all 20 Caucasian kindreds studied. CCM1 was considered to be the locus involved in only 40% of non-Hispanic kindreds, with the remaining lineages linked to CCM2 (20%) or CCM3 (40%). Subsequent analysis of further kindreds seems to confirm that about 40% of familial CMs are attributable to CCM1 mutations. The discovery of genetic heterogeneity in familial CMs has important implications both for the ability to provide reliable genetic testing in presymptomatic diagnosis and for understanding the pathogenesis of the disease. It has been suggested that there may be locus-specific differences in the penetrance of the disease, although such differences may also be attributable to the particular mutation involved.
Given that the clinical phenotypes of mutations at all three loci are essentially identical, the presumption is that the involved proteins likely converge on a conserved pathway that is required for the regulation of endothelial development. This has been borne out in a series of detailed molecular studies aimed at identifying the molecular pathogenesis of the disease. The responsible gene associated with CCM1, at the chromosome 7q locus, has been identified as human Krev interaction trapped 1 (KRIT1). Mutations in KRIT1 were first identified in a study of French kindreds with CMs; 12 different mutations were discovered. Further KRIT1 mutations have been described in families of different ethnicities. , Although the exact function of KRIT1 remains unknown, its interaction with Krev/rap 1a (a RAS family guanosine triphosphatase) and with integrin cytoplasmic domain-associated protein-1 α and evidence that KRIT1 is a microtubule-associated protein suggest a role in endothelial cell matrix interactions that in turn could play a role in abnormal vascular development. Gene products associated with CCM2 have been recently reported as proteins with potential involvement in integrin signaling encoded by the gene MGC4607 (malcavernin, osmosensing scaffold for MEKK3). , Subsequent molecular studies have identified this gene as a key regulator of the Rho family of guanosine triphosphatases involved in endothelial proliferation and migration through effects on microtubule stability and expression of cell adhesion molecules. The most recent breakthrough was the identification of the gene product of the CCM3 locus, a protein known as programmed cell death 10 (PDC10). , While the exact mechanism has not been determined, preliminary studies have shown that the CCM3 gene functions in the same Rho signaling pathway as its family members. In a striking example of how the study of human disease has resulted in the advancement of our understanding of cellular biology, investigations into the CCM proteins have uncovered a signaling pathway that is fundamental to vascular biology.
Based on the identified genetic abnormalities, it could be proposed that familial CMs result from inherited mutations and that sporadic CMs result from either a germline mutation in an individual or a somatic mutation in a single cell. There are reports both for de novo germline mutations and for somatic cell mutations in KRIT1 leading to sporadic CMs. Support for the notion of somatic mutations may be found in the development of CMs following radiation therapy, where cerebral lesions have been described within the irradiated field and were not present prior to treatment. The possibility of radiation-induced mutagenesis resulting in CM formation is one explanation for this observation.
In 1976, Voigt and Yasargil analyzed 163 cases reported up to 1974. They found that these lesions occurred in every age group and that the gender incidence was equal. In 1988, Simard et al. reviewed 126 cases published since 1960 and added 12 of their own. The male-to-female ratio was 0.9:1, and the ages ranged from neonate to 75 years. In 1991, two publications were based on the analysis of consecutive MRI scans performed over several years. , In the report by Robinson et al. of 66 patients, the male-to-female ratio was 1.2:1, and the ages ranged from 4 months to 84 years (mean 34.6 years). In the report of 32 patients by Curling et al., the male-to-female ratio was 1.1:1, the ages ranged from 16 to 72 years (mean 37.6 years), and multiple lesions were present in 6 patients (19%). Scott et al. reported a series of 19 children ranging in age from 7 months to 17 years. In the MGH series of 116 patients, the ages ranged from 4 to 69 years (mean 35.5 years), with a male-to-female ratio of 1:1.2. Multiple lesions were present in 12 patients (10.3%) in this series, and associated venous malformations were present in 9 patients (7.8%).
Most CMs that come to attention are supratentorial in location ; the distribution of CMs within the central nervous system seems to reflect the volume of tissue, without specific predilection for any particular location. The locations of the 121 operated CMs in the MGH series of 116 patients are listed in Table 55.1 .
| Location | Cavernous Malformations | Percentage of Total Cavernous Malformations |
|---|---|---|
| Cerebrum | 84 | 69.4 |
| Frontal | 36 | |
| Parietal | 16 | |
| Temporal | 28 | |
| Occipital | 4 | |
| Brain stem | 17 | 14.0 |
| Mesencephalon | 2 | |
| Pontomesencephalon | 4 | |
| Pons | 8 | |
| Pontomedullary | 2 | |
| Medulla | 1 | |
| Cerebellum | 8 | 6.6 |
| Cranial nerves | 4 | 3.3 |
| Spinal cord | 8 | 6.6 |
| Cervicomedullary | 2 | |
| Cervical | 3 | |
| Thoracic | 2 | |
| Lumbar | 1 | |
| Total cavernous malformations | 121 | 99.9 |
The four general categories of clinical presentation are seizures, headache, neurologic deficit, and asymptomatic presentation. Seizure is the most common presenting symptom, affecting 35% to 55% of patients. , , , In many patients, more than one symptom is present. Within each of the symptomatic categories, some patients have had a hemorrhage into the adjacent brain parenchyma. The hemorrhages are usually small but on rare occasion can be large, with the patient having rapid deterioration. In some patients, the CM gradually enlarges, and the lesion can act as a mass that causes a progressive neurologic deficit. The clinical symptoms arising from the 121 CMs in the MGH surgical series are presented in Table 55.2 ; among the intracranial lesions, seizures were the presenting symptom in 45%, followed by neurologic deficits (38%) and headaches (17%).
| Location | Cavernous Malformations | Presenting Symptoms | Cavernous Malformations by Presenting Symptom | Overt Hemorrhage a |
|---|---|---|---|---|
| Cerebrum | 84 | Seizure | 51 | 28 (54.9%) |
| Neurologic deficit | 15 | 13 (86.6%) | ||
| Headache | 18 | 16 (88.9%) | ||
| Brain stem | 17 | Neurologic deficit | 17 | 12 (70.6%) |
| Cerebellum | 8 | Neurologic deficit | 7 | 7 (100%) |
| Headache | 1 | 0 (0%) | ||
| Cranial nerves | 4 | Neurologic deficit | 4 | 1 (25%) |
| Spinal cord | 8 | Neurologic deficit | 8 | 6 (75%) |
a Percentage of patients with a particular clinical presentation who experienced overt hemorrhage.
In 1985, Wilkins reviewed the natural history of vascular malformations. He concluded that not enough information was present in the literature to describe the natural history of cavernous angiomas. In 1991, two reports of CMs diagnosed in large consecutive series of MRI scans gave some information about the short-term natural history, , and data from familial cases have contributed to our knowledge.
Most hemorrhages are not catastrophic, but there are occasional exceptions. Zimmerman et al. reported one patient who died from rehemorrhage of a tectal CM. There are neurologic consequences, however, even of repeated small hemorrhages. Progressive deterioration with successive hemorrhages has been described, and Robinson et al. found a strong association between hemorrhage and neurologic disability in patients with CMs. Knowledge regarding the long-term risk of hemorrhage is of importance in management decisions, especially for CMs presenting incidentally or with minimal symptoms.
Overall, available estimates of the risks of initial hemorrhage from CMs have indicated low hemorrhage rates. In a retrospective study, Curling et al. reported a 0.25% per person-year and 0.1% per lesion-year hemorrhage rate among 32 patients with 76 lesions. Robinson et al. followed symptomatic patients with 66 lesions for a mean of 26 months and observed only 1 hemorrhage in 143 lesion-years, resulting in a 0.7% per lesion-year hemorrhage rate. Porter et al. reported a 1.6% per person-year hemorrhage rate among 110 patients followed for a mean of 46 months. For 68 prospectively followed patients, Moriarity et al. reported an overall 3.1% per person-year hemorrhage rate. The risk of bleeding may be higher in deep or brain stem CMs. In their cohort of 110 prospectively followed patients, Porter et al. found a 10-fold higher hemorrhage rate among infratentorial lesions at 3.8% per year compared with supratentorial lesions at 0.4% per year. This may reflect the eloquence of the surrounding tissue, with even small brain stem hemorrhages being more likely than lesions to be clinically manifest in the cerebral hemispheres.
The risk of hemorrhage in familial CMs appears to be similar to that in nonfamilial CMs, when considering the increased frequency of lesion multiplicity. In their follow-up of six families with familial CMs, Zabramski et al. found a 1.1% per lesion-year (6.5% per person-year) rate of bleeding over a follow-up period of 26 months. In 40 patients with familial CMs, Labauge et al. reported a 2.5% per lesion-year hemorrhage risk.
Several reports suggest a higher risk of bleeding after a first hemorrhage. Kondziolka et al. followed 122 patients for 34 months and noted a low 0.6% per person-year hemorrhage rate among those without a history of prior hemorrhage but a higher 4.5% per person-year rate among those with a previous hemorrhage. Kim et al. also reported a slightly higher recurrent hemorrhage rate of 3.8% per person-year compared with 2.3% per person-year for first hemorrhage. For brain stem lesions, Kupersmith et al. reported a bleeding rate of 2.5% per person-year, with a rebleeding rate of 5.1% per person-year. Tung et al. reported recurrent hemorrhage occurring in seven patients whose diagnosis of CM was confirmed at surgery. The median interval from the initial hemorrhage to the recurrent hemorrhage was 12 months, with only 2 months until a second rebleed. Aiba et al. also found a much higher incidence of hemorrhage in those with prior bleeds at 22.9% per lesion-year versus 0.4% per lesion-year in those without prior bleeds. There is also evidence for temporal clustering of hemorrhages, with rates of rehemorrhage initially as high as 2% per month in a selected population but decreasing to less than 1% per month after 2 to 3 years.
Information regarding the long-term risk of seizure development is scarce. Kondziolka et al. reported that 4 of 94 patients without seizures developed seizures over the mean 34-month follow-up. Curling et al. estimated the risk of seizure development to be 1.5% per person-year based on 32 patients. In Zabramski et al.’s group of patients with familial CMs followed over a mean period of 2.2 years, one of six asymptomatic individuals developed seizures. The rate of new seizures in the 68 patients reported by Moriarity et al. was 2.4% per person-year.
The natural history of familial CMs has been addressed in several reports. Zabramski et al. reported six families with familial CMs; 31 patients among these families harbored CMs, 21 of whom were followed clinically and with serial imaging. A total of 128 CMs were identified radiographically in these patients. During the mean follow-up of 2.2 years, 5 lesions were found to change in size, 13 lesions showed changes in signal characteristics, and 17 new lesions were identified in six patients. Given the dynamic nature of the CMs, the report’s authors recommended serial MRI at 12-month intervals for symptomatic individuals, in addition to screening of family members. This approach can clarify the risk of morbidity in these patients and the need for close radiographic and clinical follow-up while providing data regarding the natural history. Labauge et al. noted 23 new lesions in 11 patients (27.5%) during follow-up of 40 patients with familial CM harboring 232 CMs over a mean follow-up of 3.2 years. Nine lesions (3.9%) changed in size, and signal change was observed in 14 lesions (6%) over the same follow-up period.
De novo lesions have been described in nonfamilial cases of CMs as well. The primary risk factor identified has been radiation therapy, with reports of de novo development of CMs in the spinal cord and the brain , years following irradiation. However, cases without an identifiable risk factor have also been documented. ,
Little information is available about asymptomatic patients and their risks for developing symptoms. In the report by Robinson et al., four of nine asymptomatic patients developed symptoms related to the CM over a relatively short follow-up period of 6 months to 2 years (mean 18 months).
Treatment for patients with CMs is based on careful comparison of the benefits and risks associated with the treatment options, usually either surgery or observation. Occasionally, radiosurgery has been used. The age and medical condition of the patient are considered in this decision. Because knowledge and experience are still in the cumulative stage, only guidelines can be offered.
Some patients with CMs should be followed conservatively. Almost all asymptomatic lesions are observed, because they can remain asymptomatic indefinitely and if a hemorrhage occurs, it is usually small and lacks a major neurologic deficit. Another group that may be observed consists of those with symptomatic lesions in a deep or critical area when the risks of surgery are judged to be significant and neither a recurrent hemorrhage nor an increasing neurologic deficit is present. Some patients with seizures or headache, in whom no hemorrhage has occurred, have been observed, but subsets of these patients are also candidates for surgery, as discussed in the following sections. The decision about which treatment is appropriate depends on a detailed evaluation of the clinical problem and on discussion with the patient.
No clear guidelines exist on how often the MRI scan should be repeated. A general recommendation is to perform MRI on the patient at 6-month intervals for 2 years; then, if the lesion is stable, the scan is repeated once a year. This regimen may be modified based on surgeon preference and individual patient considerations.
The current, well-established indications for surgical resection of CMs are recurrent hemorrhage, progressive neurologic deterioration, and epilepsy, unless the location is associated with an unacceptably high surgical risk. , , When the surgical risk is high, observation or radiosurgery should be considered. Because the risk of surgery is low for lesions in many locations, there are groups of patients (e.g., those with CMs of the cerebrum or cerebellum with a single overt hemorrhage, those with the onset of a seizure disorder, and those who are worried about the presence of the lesion) in whom surgery should be considered. In children, Scott et al. have a “policy to recommend surgery for patients with cavernous angiomas if the lesion is safely accessible, is currently symptomatic either by mass effect and/or hemorrhage or seizure, or shows evidence of having bled in the past.”
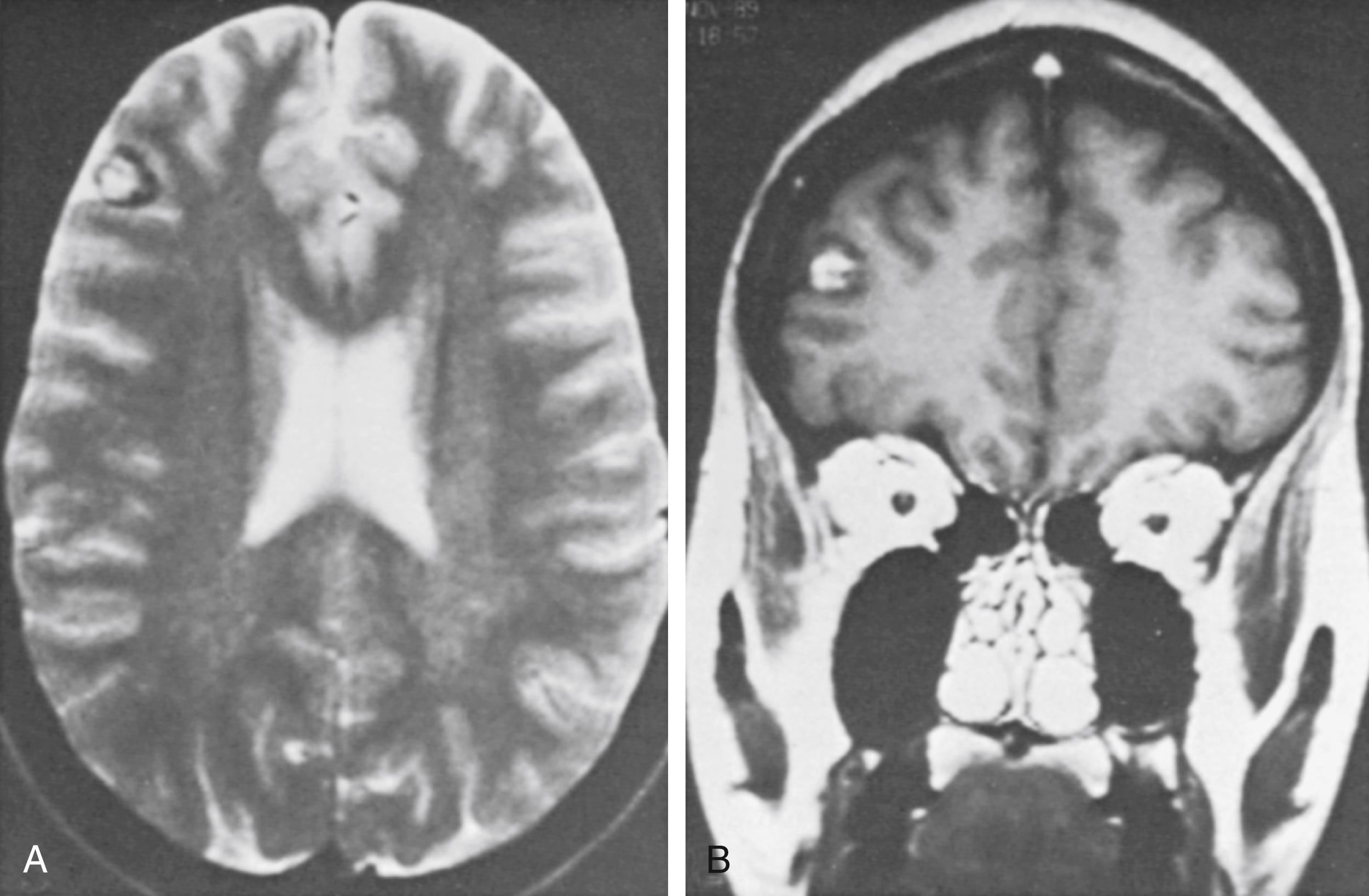
In a special category is the young woman who wants to become pregnant ( Fig. 55.3 ). Robinson et al. noted that two of their six patients with acute hemorrhage were in the first trimester of pregnancy. They suggested that in women contemplating pregnancy, one of the indications for surgical excision was an accessible lesion. Other authors have also commented on the possible role of hormonal influences as a contributing factor. , Aiba et al. reported that women predominated in the group of patients presenting with hemorrhage and that young women had a higher rate of subsequent hemorrhage.
When surgical excision of a CM is indicated, the lesion can usually be removed entirely with low morbidity. This procedure is facilitated by microsurgical dissection in the gliotic tissue that surrounds the lesion, allowing a distinct plane of cleavage to be developed through microsurgical techniques, bipolar coagulation, and the use of fine-regulated suction. When the lesion is exposed, internally decompressing the mass and retracting the capsule into the area of the decompression may help avoid pressure on the surrounding normal parenchyma. When the lesion is densely calcified, an ultrasonic surgical aspirator may be used for debulking. Bleeding is usually not a significant problem.
In some patients, splitting a cortical fissure may be possible rather than performing a full corticectomy to approach the lesion. For lesions in critical areas, cortical mapping and stimulation may be used. When removal of a CM in the deep portions of the cerebral hemispheres is indicated, the lesion is localized with stereotactic techniques and intraoperative ultrasound. , , A comparison of microsurgical resection with or without neuronavigation demonstrated that the size of resection was significantly smaller when stereotaxy was used. While this study did not show a difference in outcome, it clearly demonstrated that neuronavigation can result in a safe, better-defined resection. This is particularly important for deeply seated lesions in the basal ganglia, thalamus, or brain stem. For brain stem lesions, special monitoring with evoked potential responses may be helpful, and arrangements for temporary cardiac pacing may be prudent.
Stereotactic radiosurgery has been used to treat patients with CMs thought to be inoperable and associated with progressive worsening of neurologic symptoms because of mass effect or recurrent hemorrhage. There is difficulty, however, in establishing valid end points for therapeutic success because the natural history is poorly understood, because complications can be related to either minor rebleeding or delayed radiation-induced injury, and because MRI results may not change significantly during the follow-up period.
Kondziolka et al. reported on gamma knife use in the treatment of 47 patients with surgically inaccessible lesions with at least one prior hemorrhage. Over the mean follow-up of 3.6 years, they found a significant decline in the hemorrhage rate, from 32% per lesion-year pretreatment to 1.1% per lesion-year at 2 years after treatment. There was a high incidence of radiation-induced complications after treatment, with mean center doses of 32 Gy (range 20 to 40 Gy): 12 of the 42 patients (27%) were affected, although only 2 patients (4%) were reported to suffer permanent deficits. In a subsequent report from the same institution, 82 patients were analyzed. Again, a reduction in hemorrhage risk was reported from 33.9% to 12.3% during the first 2 years post-treatment and by 0.76% per patient-year thereafter. Overall incidence of radiosurgical morbidity was 13.4%. Karlsson et al. also reported experience with gamma knife, treating 22 patients with symptomatic CMs using maximum doses of 11 to 60 Gy (mean and median 33 Gy) and minimum doses of 9 to 35 Gy (mean and median 18 Gy). Over the mean follow-up of 6.5 years, they noted a decreasing trend in hemorrhages 4 years after treatment. However, they also found a high rate of morbidity, with six patients (27%) suffering radiation-related complications; in five of them (23%), these led to permanent deficits. Pollock et al. also noted a high incidence of radiation-related complications, occurring in 41% of their 17 patients with deep lesions, although hemorrhage rates did decline from 40.1% pretreatment to 2.9% more than 2 years after treatment. Another series of gamma knife radiosurgery noted a reduced frequency of seizures following treatment, with 18 of 28 patients (64%) who had a chief complaint of seizure experiencing this benefit.
More recent studies have shown similar results. Lunsford et al. recently published their results of a retrospective cohort of 103 patients who demonstrated a propensity to bleed (more than two bleeds) and had CMs in locations deemed too risky for microsurgical resection. Their analysis again demonstrated a reduction in hemorrhage risk from 32.5% to 4.6%. Most of the risk of hemorrhage was in the first 2 years after surgery (10.8%), because the rate of hemorrhage after this initial latency period dropped to 1.06%. The studies’ authors commented that this latency period likely reflects the time period over which the endothelium undergoes progressive hyalinization and luminal obliteration, reminiscent of the mechanism of action on arteriovenous malformations. One report of histopathologic analysis of a CM that was microsurgically resected 1 year after receiving 40 Gy of radiation supports this hypothesis. Despite the use of a slightly lower mean dose (30.2 Gy, range 21.7 to 40 Gy) and confining the target volume to the hemosiderin ring as defined by high-resolution T2 images, the incidence of postradiation T2 signal change surrounding the CM was 18.4%. New neurologic deficit was noted in 13.5% of patients, though the report’s authors commented that these deficits were all transient, with only one patient demonstrating persistent deficits. Similar results were found by the same group looking at a cohort of 68 patients with hemorrhagic brain stem CMs that were also deemed surgically inaccessible. Moreover, the authors bring up the point that previous studies demonstrating much higher and more permanent adverse radiation effects likely reflected treatment of CMs with associated developmental venous anomaly (DVA), which are at intrinsically high risk for venous congestion and ischemic events if treated with stereotactic radiosurgery. As such, the authors advocate for better patient selection rather than abandonment of stereotactic radiosurgery for CMs in surgically high-risk areas.
Stereotactic charged-particle radiosurgery, both helium-ion radiosurgery and proton beam therapy, has also been used to treat CMs. Fabrikant et al. noted that the clinical results after helium-ion radiosurgery for CMs were not as good as those for arteriovenous malformations. Radiosurgery using a linear accelerator has also been reported but with small numbers of patients treated and a lack of long-term data. Chang et al. summarized the results of patients treated using helium ion (47 patients) or linear accelerator (10 patients). All patients harbored CMs that had bled previously and were treated with mean doses of 18 GyE. Hemorrhage rates decreased 3 years after treatment to 1.6% per patient-year. In this study, five patients (9%) suffered radiation-related edema or necrosis, resulting in permanent deficits in two patients (4%). Analysis of Kjellberg’s experience at the Harvard Cyclotron Laboratory using proton beam therapy revealed a decline in hemorrhage rates from 17.3% per lesion-year before treatment to 4.5% per lesion-year after a latency period of 2 years. Among the 98 lesions treated with a median center dose of 18 Gy, 26 (26.5%) were associated with radiation-related complications, 16 of which were permanent and 3 of which resulted in mortality.
Because the long-term natural history of CMs is not well defined, current evidence favors expectant management, given the high rates of complications with radiosurgery. The risk of radiation-related complications appears to be significantly higher than that found for arteriovenous malformations of similar size and location ; although the basis for this is unknown, a role for the potential radiosensitizing properties of the hemosiderin ring around CMs has been proposed. The decline in hemorrhage rates observed in most studies cannot definitively be ascribed to the treatment, because it may reflect the poorly characterized natural history of bleeding in these lesions.
Temporal clustering of hemorrhages, with a spontaneous 2.4-fold decline in hemorrhage rates after 2 years, has been observed and may affect the interpretation of hemorrhage risk reduction in radiosurgical series. This modality is presently considered only rarely for deep, inaccessible lesions associated with repeated hemorrhage and progressive neurologic deficit.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here