Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
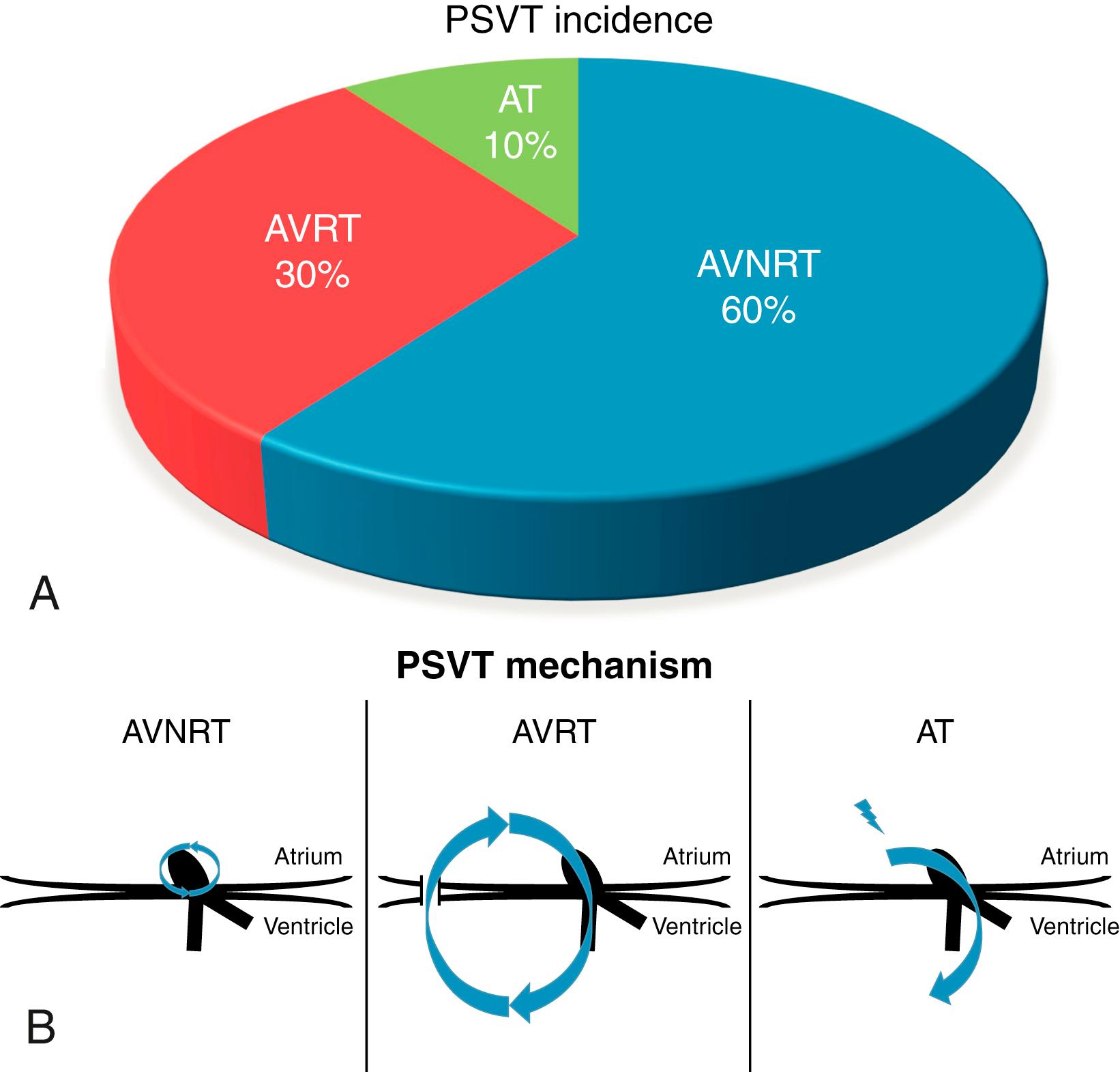
Paroxysmal supraventricular tachycardia (PSVT; Table 70.1 ) refers to a group of heterogenous arrhythmias with different electrophysiologic mechanisms manifesting as a regular narrow complex tachycardia, typically having an abrupt onset and offset. The differential diagnosis for these disorders includes atrioventricular nodal reentrant tachycardia (AVNRT; see Chapter 72 ), atrioventricular reentrant tachycardia (AVRT; see Chapter 74 ), atrial tachycardia (AT; see Chapter 71 ), and junctional ectopic tachycardia (JET; see Chapter 73 ). It does not include atrial fibrillation and atrial flutter. PSVT is relatively common in the general population, with an incidence around 2.5 per 1000 adults. It can be diagnosed at any age, but most commonly presents between the ages of 12 and 30 years. The most common PSVT diagnosed in the electrophysiology (EP) laboratory is AVNRT, accounting for approximately 60% of cases, although this may be higher in adults as there is increasingly earlier diagnosis and ablation of Wolff-Parkinson-White (WPW) syndrome. AV reentrant tachycardia accounts for approximately 30% of PSVT adult cases. The most common form of AVRT is called orthodromic SVT, in which antegrade conduction occurs over the AV node and retrograde conduction occurs over a bypass accessory pathway (see Chapter 74 ). The least commonly encountered PSVT is AT, accounting for approximately 10% of cases and, unlike the former two diagnoses, is AV nodal independent. It is very rare to encounter JET in the EP lab, as it occurs most commonly in children and after cardiac surgery (see Chapter 73 ). Having a baseline understanding of the underlying mechanisms of SVT is essential to better diagnose these in the lab ( Fig. 70.1A–B ). During a typical EP study, the mechanism and origin of PSVT is determined by analyzing the following during tachycardia: (1) the mode of initiation, (2) the relationship of the P wave to QRS, (3) effects of bundle branch block (BBB), (4) the effect of AV dissociation, and (5) the effect of atrial or ventricular stimulation during tachycardia. This chapter discusses the various arrhythmia mechanisms and the tools needed to differentiate them in the EP laboratory.
| AOP | Atrial overdrive pacing |
| AP | Accessory pathway |
| AT | Atrial tachycardia |
| AVNRT | Atrioventricular nodal reentry tachycardia |
| AVRT | AV reentry tachycardia using an accessory pathway |
| BBB | Bundle branch block |
| HB | His bundle |
| HRA | High right atrium |
| HRPAC | His refractory premature atrial beat |
| JET | Junctional ectopic tachycardia |
| LB | Left bundle |
| NPV | Negative predictive value |
| ORT | Orthodromic atrioventricular reentry tachycardia |
| PH | Para-Hisian |
| PPV | Positive predictive value |
| RB | Right bundle |
| RAAS | Retrograde atrial activation sequence |
| SVT | Supraventricular tachycardia |
| TZ | Transition zone during ventricular overdrive pacing |
| VA | Ventriculoatrial (retrograde) conduction or VA conduction interval |
| VOP | Ventricular overdrive pacing |
Planning for an EP study should begin prior to arrival in the lab, starting with a detailed history and physical exam. A patient’s age, gender, and comorbidities provide insight into the likely type of SVT encountered. In a study of 1754 patients with PSVT, most patients with AVRT were men, whereas the majority with AVNRT were women. Patients with AVRT presented much earlier in life (60% during the first decade of life) compared with AT patients, of whom 23% presented after the age of 70 years. In patients with known AVRT, females more frequently have a right annular accessory pathway (AP) compared with men. In adult patients who present with AT, the majority have organic heart disease.
An electrocardiogram (ECG) in sinus rhythm and tachycardia can be useful to make some baseline observations. A sinus rhythm ECG should be assessed for any degree of manifest preexcitation, which would strongly predict a PSVT mechanism involving an AP, with a specificity and positive predictive value (PPV) reported as high as 97% and 98%, respectively.
An ECG or telemetry strip in tachycardia should be assessed for the P-QRS relationship, P wave morphology, and RP interval. If P waves are discernable during tachycardia, a superior or inferior P wave axis can be suggestive of AVNRT (superior axis) or AT/AVRT (inferior axis). A tachycardia that does not have a 1:1 AV relationship (i.e., more than one P wave for each QRS) essentially rules out AVRT, which requires ventricular depolarization for tachycardia maintenance. The RP interval should also be analyzed to classify a tachycardia as short RP, with an RP/PR interval ratio less than 1, or long RP, having an RP/PR interval ratio of 1 or greater. A short RP tachycardia has the differential diagnosis of typical AVNRT, AVRT, and AT, whereas a long RP tachycardia may represent atypical AVNRT, AVRT, or AT. If no P waves are discernable during tachycardia, the terminal portions of the QRS should be inspected in the inferior leads (II, III, aVF) and lead V 1 . A pseudo R wave in lead V 1 or a pseudo S wave in the inferior leads present during tachycardia but not during sinus rhythm is highly suggestive of AVNRT.
When available, an ECG or telemetry strip showing the initiation or termination of tachycardia can also be quite useful. A premature atrial complex (PAC), followed by a relatively long PR interval, suggesting conduction antegrade over a slow pathway, with subsequent initiation of a narrow complex tachycardia would strongly favor AVNRT. Termination of a sustained 1:1 tachycardia with AV block, represented by termination with a P wave that is not premature, is evidence of an AV nodal–dependent tachycardia and essentially excludes AT. When looking for ECG clues for diagnosis, one should not rely completely on these criteria, although their validity increases when the findings are consistent and reproducible.
Prior to the procedure, informed consent is obtained and any blood work done. Moderate sedation with intravenous (IV) fentanyl and midazolam is used for most patients undergoing an EP study and is generally administered by the nursing staff under the direction of the EP attending physician. Some centers routinely use anesthesiology staff, but monitored anesthesia care or general anesthesia should be avoided, if possible, as these modes of deeper sedation may make tachycardia induction difficult. The majority of EP procedures can be done using three catheters and the right femoral vein. If a fourth catheter is needed, the left femoral vein can be used for access. After the patient is prepped and draped, access to the femoral vein can be obtained using the modified Seldinger technique under vascular ultrasound guidance.
A standard EP study is performed using a soft-tip quadripolar catheter in the right ventricle (RV), a multipolar or ablation catheter in the His position, and a steerable quadripolar catheter in the high right atrium (HRA). If the suspicion for AVNRT is high, a long guiding sheath can be placed initially, through which a standard 4 mm electrode tip deflectable ablation catheter can be advanced through to the His position. If it is necessary to assess the retrograde atrial activation sequence (RAAS) or the pattern of preexcitation in a WPW patient, the HRA or ablation catheter can be moved to the coronary sinus (CS) position.
After catheters are placed, the patient should receive an IV bolus of heparin (3000 U), followed by an additional 1000 U/hr to prevent thrombus formation on the catheters or sheaths. An advanced three-dimensional mapping system is now commonly used for most cases of PSVT ablation and can be helpful, but it is not necessary unless the procedure is intended to be done without the use of fluoroscopy.
Prior to induction of tachycardia, a few baseline observations can be made to assist in making a proper diagnosis and provide insight to the tachycardia mechanism. These observations include (1) manifest preexcitation, (2) dual AV nodal physiology, (3) ventriculoatrial (VA) block cycle length (CL), and (4) para-Hisian (PH) pacing response.
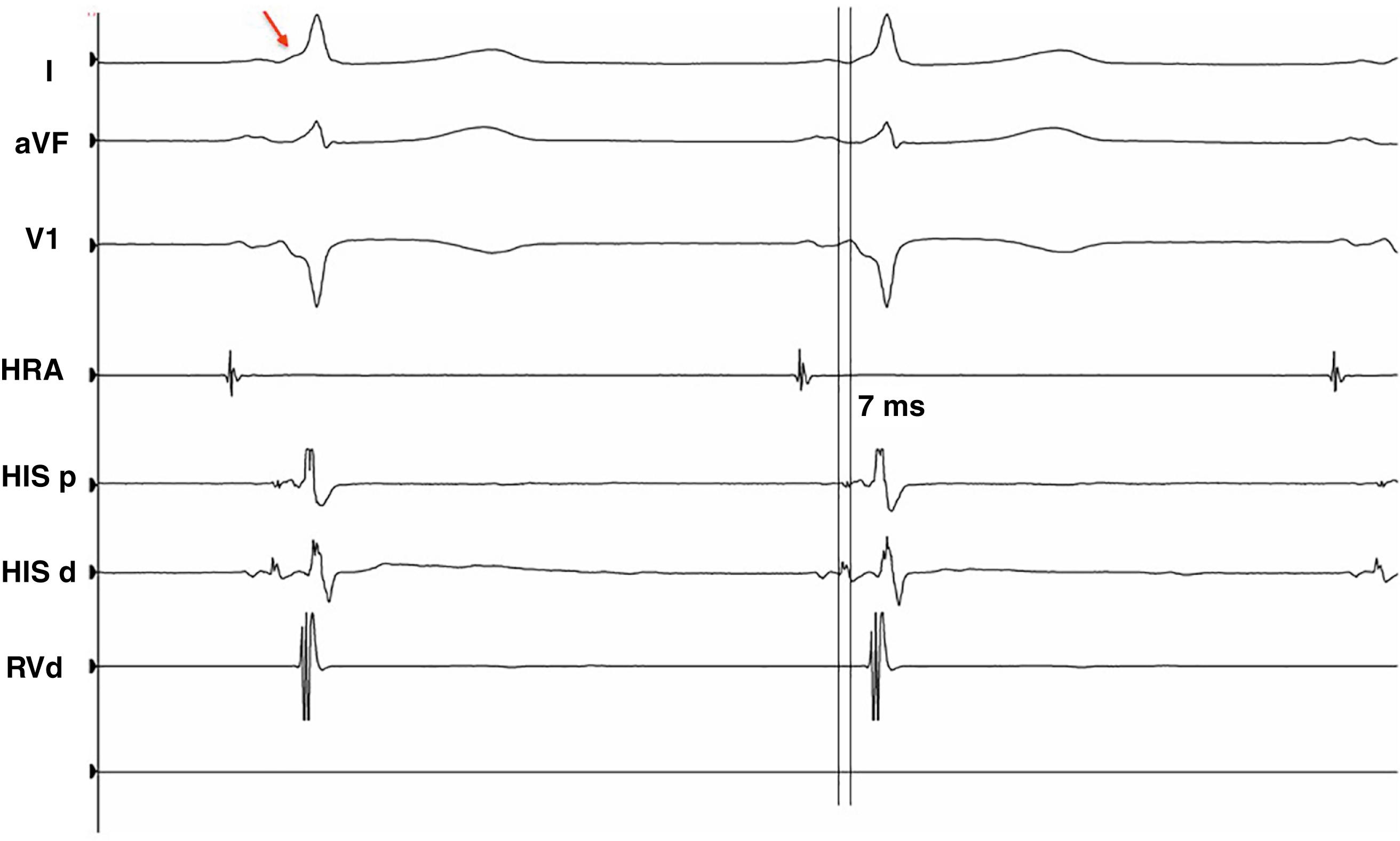
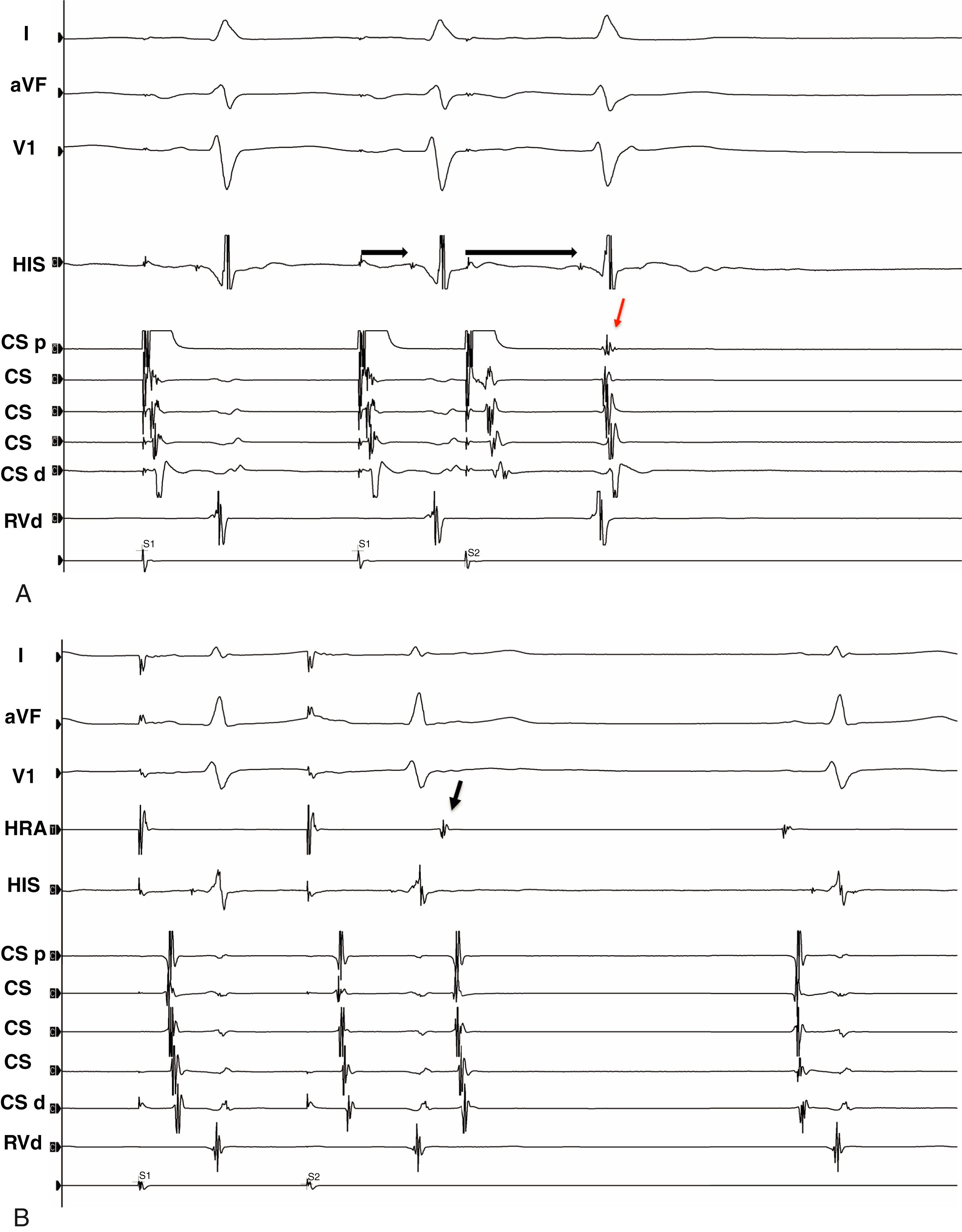
Prior to any pacing maneuvers, baseline intervals should be measured, including the HV interval. Any evidence of ventricular preexcitation on the surface ECG, or an HV interval of less than 35 ms ( Fig. 70.2 ), has a high specificity and PPV for detecting AVRT in a patient with PSVT. Atrial extrastimulus pacing is used to define AV nodal physiology. Dual AV nodal physiology is diagnosed by observing an increase by at least 50 ms in the AH interval (A2H2) with a 10 to 20 ms decrease in the coupling interval (A1A2) of the atrial extrastimulus ( Fig. 70.3A –B). The presence of dual AV nodal physiology has a sensitivity and specificity of 86% and 83%, respectively, for detecting AVNRT in patients presenting with PSVT. However, 25% of patients without SVT also demonstrate dual AV nodal physiology with atrial extrastimulus pacing. It should be remembered that dual AV nodal pathways and APs can be incidental findings.
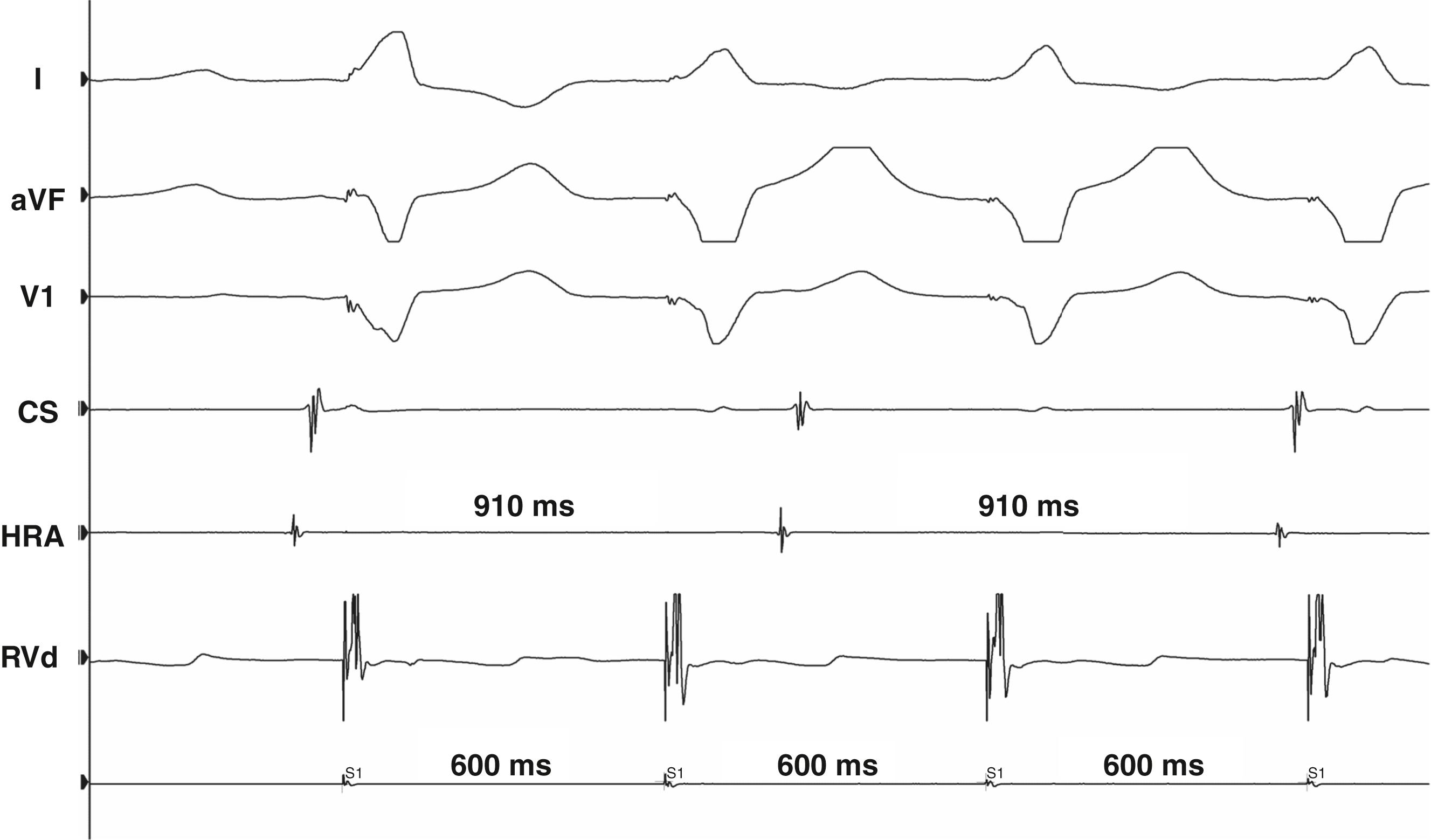
Ventricular pacing at baseline should be done to assess for retrograde conduction and to demonstrate decremental versus fixed retrograde conduction. If a CS catheter is present, an eccentric pattern of atrial activation during ventricular pacing can indicate the presence of an AP and increases the likelihood of AVRT as the culprit SVT. If there is no VA conduction present at a CL of 600 ms or greater ( Fig. 70.4 ), the presence of an AP is very unlikely, although not impossible, as approximately 5% of these patients may have retrograde conduction with catecholamine stimulation. , In a patient without an AP, ventricular pacing at shorter CLs will increase VA conduction time because of decremental conduction retrograde through the AV node. However, in a patient with an AP, the VA interval may remain fixed if conduction time retrograde through the AP is shorter than transit time through the AV node. Evidence for decremental conduction by ventricular pacing makes the presence of an AP unlikely, although accessory pathways can exhibit decremental properties.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here